Abstract
Background
Management of failed laparoscopic gastric plication (LGP), defined as weight regain or inadequate weight loss, is a challenging issue.
Methods
This prospective investigation was conducted in individuals with morbid obesity who had undergone LGP from 2000 to 2016. Patients with weight loss failure, weight regain, and regain-prone cases were indicated for reoperation. Re-plication, laparoscopic one anastomosis gastric bypass (LOAGB), and modified jejunoileal bypass were done as revisional surgery.
Results
Revisional surgery was performed in 102 of 124 patients who needed reoperation. Overall, 39 re-plication, 38 LOAGB, and 25 malabsorptive procedures were performed. Re-plication was the shortest surgery and had the shortest length of hospital stay. The percentage of TWL at 6, 12, and 24 months of follow-up was 20.5%, 25%, and 26.8% for re-plication; 20.2%, 27%, and 30.5% for LOAGB; and 22.9%, 28.9%, and 32.6% for the malabsorptive procedure, respectively. In addition, the percentage of EWL at 6, 12, and 24 months of follow-up was 62%, 74.6%, and 79.6% for re-plication; 51.6%, 68.2%, and 75.9% for LOAGB; and 55.4%, 70.1%, and 79.1% for malabsorptive procedure, respectively. In long-term follow-up, according to %TWL, LOAGB and malabsorptive procedure had better outcome compared to re-plication, whereas there was no statistically significant difference in %EWL among the three surgical approaches.
Conclusions
In terms of weight loss, reoperation on failed LGP was completely successful and no treatment failure was reported. All three revisional procedures, including re-plication, LOAGB, and malabsorptive procedure showed promising results and provided substantial weight loss. Since there is little information about the long-term efficacy and safety of revisional surgery on failed LGP, we highly recommend further investigations to confirm our results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a major growing global concern and public health issue that is associated with several medical disorders [1]. Obesity and related complications impose a large economic burden on the health care system [2], of which 35% is related to morbid obesity [3].
Nowadays, bariatric surgery is considered the only effective therapy for treatment of morbid obesity to induce long-standing weight loss and control comorbidities [4]. There are three approaches for the implementation of bariatric surgery: restrictive, malabsorptive, or a combination of both [5]. Laparoscopic gastric plication (LGP) is a restrictive bariatric surgical technique that is similar to laparoscopic sleeve gastrectomy (LSG) [6, 7]. In this procedure, the greater curvature of the stomach is folded inwardly and sutured. LGP is a reversible procedure that requires no partial stomach resection or device insertion, thus complications such as leakage and hemorrhage are less frequent [8]. In addition, LGP is a comparatively inexpensive technique. The main indications of revisional bariatric surgery are inadequate weight loss or weight regain. Our last study on LGP revealed a weight regain rate of 5.5%, 31%, and 42% after 4, 8, and 10 years of follow-up, respectively [9].
The increased prevalence of morbid obesity has led to a growing demand for bariatric surgery; hence, the need for revisional bariatric surgery is becoming more common [10]. Some investigations have tried to find the best therapeutic option after bariatric surgery failure [11, 12], but management of failed LGP, defined as weight regain or inadequate weight loss, is a challenging issue. In the present study, we aimed to report the weight loss outcomes of revisional bariatric surgery in patients with failed LGP.
Patients and Methods
As part of a large prospective study, this bicentral investigation was conducted in individuals with morbid obesity who had undergone LGP from 2000 to 2016. The Institutional Review Board of Tehran University of Medical Sciences approved the study protocol. Accurate medical history and anthropometric measurements were recorded. Patients who met National Institute of Health (NIH) criteria for surgical treatment of morbid obesity and were motivated to modify their lifestyle after the operation underwent LGP. In all patients, the original bariatric procedure was one-row LGP (from 2000 to 2006) and two-row LGP (from 2000 to 2016). The detailed information of the surgical technique used for LGP is described in our previous paper.
Briefly, in one-row LGP, dissection was started from the prepyloric area for up to almost 2 cm to the angle of His, preserving the anatomy of the angle of His and sacrificing the left and right gastroepiploic artery. The gastric greater curvature was invaginated into the stomach and one layer of the gastric greater curvature was plicated from the anterior wall of the stomach to its posterior wall. Continuous suturing was performed from the fundus to the antrum using 2/0 prolene or nylon.
In two-row LGP, dissection of the proximal part was complete and the angle of His was actually destroyed. Anti-reflux suturing was done in the beginning to prevent reflux, and after dissecting and releasing the gastric greater curvature, four separation-points of A and B (anterior), and C and D (posterior), which represented the location of suture bites, were considered to make three sections. In fact, purse string suturing of the folds at proximal part of the esophagus prevents any eversion of folds into it. These points were repeated at many transverse levels from the top in the fundus to the bottom in the prepyloric area of stomach. Three sections of the gastric wall forming the perimeter of the greater curvature were invaginated at different levels. Points A and D in all levels comprised the outer or superficial suture row while points B and C made the deep or inner suture row. The gastric greater curvature was plicated using a two-layer continuous suture with one 2/0 prolene or nylon thread from the fundus at the level of diaphragm preserving the angle of His to just proximal to the pylorus. All sutures were seromuscular or became seromsucular after closure via cutting the mucosal layer to avoid their absorption by gastric acid. Finally, a tube-shaped stomach was formed in which the greater curvature was inverted into the stomach [9].
Inclusion Criteria and Definitions
Patients with weight loss failure or weight regain following LGP were selected from our prospective study for revisional procedures. Weight loss failure was defined as percentage of excess weight loss (%EWL) < 30% during the first 12 postoperative months, and weight regain was diagnosed if %EWL reached < 30% at any time of follow-up postoperatively. We had an extra group of patients named “regain-prone” who experienced satisfactory weight loss after surgery, but experienced weight regain later and volunteered for revisional surgery.
Revisional Surgery
Patients with weight loss failure or weight regain as well as regain-prone cases were indicated for revisional surgery. All operations were done by one surgeon. Weight loss failure cases and those who had weight regain with poor prognostic factors were considered for malabsorptive technique early in the study and laparoscopic one anastomosis gastric bypass (LOAGB) later in the study. Patients with weight regain due to a new temporary condition such as pregnancy were recommended to undergo re-plication or LOAGB if they were not convenient with considering life style modifications such as sticking to a diet and doing regular exercise [13]. Reoperation techniques were as follows:
In the re-plication technique, after releasing adhesions at the site of previous sutures and inserting a number 32 guide, all bubbles at the site of plication are inverted by a new suture line mostly in one row because the size of the stomach does not usually allow to use two-row sutures. However, in some parts where the stomach is dilated like a big diverticula, two- or three-row sutures are used. The technique is easier than the primary technique because the stomach is not very dilated and can be plicated completely by one-row suturing.
LOAGB was performed as described by Rutledge [14]. In brief, a cylindrical gastric tube was created by division of stomach parallel to the lesser curvature from the angle of His to the antrum using a stapler. The site of horizontal staple was checked at about 6 cm below the LES to ensure it was dilated enough to fire the stapler without any problems. If it was plicated, plication was undone to make sure multiple layers were not fired by the stapler. Then, vertical stapling was continued by tri-stapler purple covidien to separate a narrow tall vertical pouch from the remaining of the stomach. If the proximal part of the stomach became ischemic following separation of the pouch, it was cut by continuing the stapler line at the row of horizontal stapling and the proximal part was removed. An anastomosis was created between the distal end of the gastric tube and the jejunum, 200 cm distal to the ligament of Trietz, using continuous 2/0 prolene sutures.
Modified jejunoileal bypass was accomplished as outlined by Fazel et al. [15]. To sum up, the proximal 15 cm of the jejunum was anastomosed to the distal 45 cm of the terminal ileum. The defunctionalized limb was bypassed by anastomosing its ends to the gall bladder and cecum.
Postoperative Follow-Up
Following reoperation, patients had regular visits every 2 weeks during the first 6 months, monthly until the end of the first year, every 2 months during the second year, and annually afterwards. Postoperative complications and weight-related measures were carefully evaluated in each visit. Weight-related measures as outcomes were as follows: BMI (weight (kg)/height (m)2), excess weight (preoperative weight − ideal weight), excess BMI (preoperative BMI − 25), total weight loss percentage (%TWL) ((preoperative weight − weight at each time point)/preoperative weight × 100), and %EWL((preoperative weight − weight at each time point)/excess weight × 100). Treatment failure was defined as %EWL < 30% at 12-month follow-up.
Statistical Analysis
We assessed the distribution of study parameters using the Shapiro-Wilk normality test. Associations between categorical parameters were analyzed using the Chi-square or Fisher’s exact test, whichever appropriate. Student’s t test and Mann-Whitney U test were used to compare continuous parameters between the two groups. For comparisons among more than two groups, analysis of variance or the non-parametric Kruskal–Wallis H test was used, followed by post-hoc analysis for significant results. P values < 0.05 were considered significant.
Results
Study Population
A total of 1840 individuals with morbid obesity were treated with LGP. Among them, 156 patients underwent one-row and 1684 patients underwent two-rows LGP including six cases with failure in one-row (3%) and two cases with failure in two-rows group (0.1%). One hundred twenty-four participants (58 male and 66 female) with a mean age of 31.6 years, including 74 patients with weight regain, 42 regain-prone subjects, and 8 cases with weight loss failure were scheduled for revisional surgery in this study. Of these 124 participants, 69 had undergone one-row LGP and the rest had received two-row LGP (Table 1). At the time of enrolment for the primary LGP, the failure group had the highest BMI and excess weight compared to regain and regain-prone groups. Failure group had the highest one-row to two-row LGP ratio compared to regain and regain-prone cases. Baseline characteristics of the participants and the outcome of primary bariatric surgery are presented in Table 2 (Fig. 1).
Reason of Reoperation
Reoperation was performed on 102 patients (49 male and 53 female) including 55 patients with weight regain, 42 regain-prone cases, and 5 subjects with weight loss failure. On average, the revisional procedures were performed 3.5 years after the primary LGP, and those with weight loss failure had the longest duration between the primary and revisional bariatric surgery. The failure group had a longer operation time (116 min) than regain (83 min, P value = 0.006) and regain-prone cases (80 min, P value = 0.004). The mean excess weight of regain, regain-prone, and failure cases before the reoperation was 46, 38.4, and 59.3 Kg, respectively. In order, failure, regain, and regain-prone cases had a significantly higher BMI before revisional surgery (P value < 0.001).The mean hospital stay after the reoperation was 3.2 days and the length of hospital stay was comparable between three groups.
At 6-, 12-, and 24-month follow-up, the %TWL was 20.7%, 26.8%, and 30.1% in the regain; 20.8%, 26%, and 28.2% in regain-prone, and 26%, 32.1, and 35.2% in failure cases (Fig. 2).The percentage of TWL was comparable between regain cases and regain-prone group. However, the %TWL was significantly higher in failure cases compared to both regain and regain-prone groups.
At 6-, 12-, and 24-month follow-up, the %EWL was 55%, 70.5%, and 79.3% in the regain; 58.7%, 72%, and 76.8% in regain-prone, and 58.5%, 71.9%, and 79.1% in failure cases. The percentage of EWL was comparable at 6 months of follow-up and thereafter among the three groups. Table 3 presents baseline characteristics of patients before reoperation and detailed results of revisional surgery according to the reoperation reason.
Revisional Surgery
Overall, 39 re-plication, 38 LOAGB, and 25 malabsorptive procedures were performed. The patients who received malabsorptive procedures had more excess weight (52.9 kg) than LOAGB (48.2 kg, P value = 0.04) and re-plication (33 kg, P value < 0.001) cases before the reoperation. Moreover, re-plication cases had the lowest baseline BMI but the difference was not significant between LOAGB and malabsorptive groups (P value = 0.1). Re-plication, with a reoperation time of 53.6 min, was the shortest surgery, but the reoperation time was comparable between the LOAGB and malabsorptive group (P value = 0.2). Re-plication and LOAGB had the shortest and longest postoperative hospital stay, respectively.
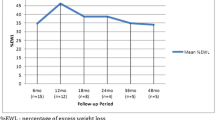
Percentage of patients who reached 6-, 12-, 24-, 36-, and 48-month follow-ups were %94, %88, %68, %41, and %28, respectively. Furthermore, there was no significant difference in terms of baseline characteristics between groups of patients who did versus did not reach ≥ 36-month follow-up visit.
The percentage of TWL at 6, 12, and 24 months of follow-up was 20.5%, 25%, and 26.8% for re-plication; 20.2%, 27%, and 30.5% for LOAGB; and 22.9%, 28.9%, and 32.6% for the malabsorptive procedure, respectively (Fig. 3). At 6 months of follow-up, malabsorptive procedure showed greater %TWL compared to both re-plication and LOAGB. However, at 12 and 24 months of follow-up, LOAGB and malabsorptive procedure had comparable results, and both showed significantly larger %TWL compared to re-plication. On the whole, according to %TWL, LOAGB, and malabsorptive procedure had better outcome compared to re-plication.
The percentage EWL at 6, 12, and 24 months of follow-up was 62%, 74.6%, and 79.6% for re-plication; 51.6%, 68.2%, and75.9% for LOAGB; and 55.4%, 70.1%, and 79.1% for the malabsorptive procedure, respectively. Re-plication had a greater %EWL until 6 months of follow-up compared to the malabsorptive procedure and until 12 months of follow-up compared to LOAGB. The percentage of EWL was comparable for malabsorptive procedure and LOAGB. Generally, in the long term, there was no significant difference in the %EWL among three surgical approaches. Table 4 shows the baseline characteristic of patients before the reoperation and the detailed outcome of reoperation based on the type of revisional surgery.
Discussion
LGP is a restrictive bariatric surgery. The technique needs no gastric resection and/or insertion of any instrument, so the rate of complications is significantly low. In fact, LGP works like LSG, but without gastric resection, which makes it reversible. American Society for Metabolic and Bariatric Surgery (ASMBS) considers LGP an investigational procedure [16] and recommends more complementary studies to clarify its different aspects.
In the current study, we evaluated the weight loss outcome of revisional bariatric operations in patients who had undergone LGP for morbid obesity. We used re-plication, LOAGB, and malabsorptive procedure as reoperation procedures. A total of 102 patients underwent reoperation and were followed for 48 months. The one-row to two-row LGP ratio was higher in the failure group. Weight loss failure cases had a longer operation time and the highest BMI before the reoperation. Patients who received the malabsorptive procedure had the greatest amount of excess weight before reoperation, while patients in the re-plication group had the lowest baseline BMI. All three groups (categorized based on both the reason of reoperation and the type of revisional surgery) showed successful weight loss for up to 24 months. Although, there was no significant different in %EWL between the three groups in the long-term follow-up, LOAGB and malabsorptive procedure demonstrated greater %TWL compared to re-plication.
The rate of complications is higher after reoperation than the primary bariatric surgery [17], so it is critical to apply appropriate patient selection criteria. A recent systematic review of the literature revealed that the majority of published studies have no definition for failure of bariatric surgery. Nevertheless, EWL < 50% at 18-month follow-up and EWL < 30% at a not determined follow-up period have been the more frequently applied criteria [18]. In this study, patients were considered for reoperation if %EWL was below 30% after 12 months of follow-up or %EWL reached < 30% at any time during the follow-up. Lack of a standard definition for bariatric surgery failure can expose patients to unnecessary revisional surgery that might lead to further undesirable complications and decrease their quality of life. Therefore, there is a real need for a standard and generally accepted definition for failure of bariatric surgery.
Besides, surgeons always try to select the best operative choice for their patients. As mentioned above, reoperations are more likely to cause complications [17], so we have to choose the least invasive yet the most effective procedure. The type of reoperation after the primary bariatric surgery is selected based on the cause of reoperation such as weight regain, weight loss failure, or complications. Prior studies have introduced re-plication, laparoscopic gastric bypass (LGBP), and LSG as reoperation techniques after LGP complicated by weight regain or weight loss failure in limited cases.
Weight loss failure indicates that the previous surgical procedure was not effective to induce weight loss. Since LGP is a restrictive approach, inadequate weight loss indicates that a pure restrictive approach might no longer be efficacious in patients with a high BMI. LOAGB is a bariatric surgery technique almost identical to LGBP, which has both restrictive and malabsorptive properties. LOAGB has been demonstrated to induce a similar weight loss as compared to LGBP [21]. Nevertheless, LOAGB is less invasive because only one anastomosis is performed in LOAGB compared to LGBP with two anastomoses. Therefore, the rate of complications is lower in LOAGB. Hence, we preferred to perform a malabsorptive procedure (earlier in this study) or LOAGB (later in this study) in weight loss failure cases.
Shrinkage of the plicated fold and extension of the elastic gastric wall are two main causes of weight regain following LGP [9], indicating that restrictive procedures are effective in weight regain cases although there is a need for refixing. Therefore, LGP is still a treatment option for morbid obesity. Considering all this information, we considered re-plication or LOAGB for patients with weight regain as the least invasive procedures.
Although LGP has been evaluated in several studies [8, 9, 22,23,24], very few studies have provided detailed information about the outcome of revisional surgery following weight regain or weight loss failure in patients with prior LGP. To our knowledge, only two studies have reported the outcome of revisional surgery due to weight loss failure or weight regain [19, 20]. Albanses et al. performed LGP in 56 individuals with morbid obesity of whom 13 underwent reoperation due to unsatisfactory weight loss. Of the 13 patients with reoperation, 10 had LSG and two underwent re-plication. In patients with LSG, the mean BMI and percentage of excess BMI loss (%EBL) was 34 kg/m2 and 20% after 1 month. The first month postoperative BMI and %EBL of two re-plication patients were 39 kg/m2 and 41 kg/m2 and 16.9% and 22.6%, respectively [20]. Zerrweck et al. conducted a study in 100 patients with morbid obesity. Thirty cases with poor weight loss, severe upper gastrointestinal (GI) symptoms, or both were reoperated. Seventeen patients underwent LSG and 13 received LGBP. LSG patients had the shortest hospital stay (2 days vs. 3 days in the LGBP group). After 18 months of follow-up, %EWL was 61.4% and 75.7% in the LSG and LGBP group, respectively [19]. Although these two studies presented the outcome of revisional bariatric surgery in LGP patients, they had some important limitations. Albanese et al. followed the patients for a short time after the reoperation and reported the BMI and %EBL of the patients only in the first month post reoperation [20]. Besides, they only had two patients in re-plication group that hindered conclusion. In the study by Zerrweck et al., the patients underwent revisional surgery due to poor weight loss, upper GI symptoms, or both [19]. They did not stratify the results according to the reoperation reason. Therefore, their results should be interpreted with caution.
We found that the failure group had the highest baseline BMI compared to weight regain cases and regain-prone group. This finding was confirmed by the results of a recent study that showed %EWL was significantly lower, and the percentage of inadequate weight loss was significantly higher in patients with BMI > 45 than those with BMI < 45 [25]. The authors assumed that massive obesity and hepatomegaly might result in impeded proper gastric wall plication and believed inadequate weight loss was due to insufficient gastric volume reduction or failure of gastric wall bonding [25]. LGP seems to be less effective in severely obese individuals, and surgeons should anticipate high rates of failure in patients with a BMI above 45 kg/m2.
Of patients who underwent reoperation, 69 and 55 subjects had received one-row and two-row plication, respectively. The one-row to two-row plication ratio was higher in weight loss failure cases. Previous studies with a short follow-up time have shown no difference in %EWL between one-row, two-row, or multiple row gastric plication [25, 26]. Our previous report showed the same %EWL at first but a higher %EWL in two-row LGP in a longer follow-up [9]. Dilation and outside displacement of the plicated fold are some disadvantages of one-row plication, which could explain the higher rate of failure in this technique. In our series, we had only eight failure cases, which is too small to prove any relationship and therefore further investigations are required.
A recent systematic review revealed that LGP has a %EWL of 32 to 74% from 6 to 24 months of follow-up [27]. In our study, the %EWL of re-plication from 6 to 24 months of follow-up was 62 to 79.6%. In our previous report, the %EWL of the primary LGP in a similar follow-up period was from 60 to 70%, and a decreasing trend was observed in %EWL after 24 months [9]. Re-plication seems to have promising results as compared to the primary LGP and is associated with a lower rate of complications such as shrinkage of plicated fold and gastric wall extension. Therefore, plication should not be left aside after the first failed experience and re-plication can be employed for the second operation.
LOAGB as a primary bariatric surgery is reported to have a 6-month %EWL of 38–58%. The percentage of EWL reaches 64–80% at 24-month follow-up [28], and 70% at 36, and 73% at 60-month follow-up [29, 30]. Bruzzi et al. compared the percentage of excess BMI loss (%EBMIL) between primary LOAGB and revisional LOAGB after failed restrictive procedure. Although %EBML was lower in revisional LOAGB, the difference was not significant in the long term [31]. We observed %EWL of 51.6 to 75.9% from 6 to 24 months of follow-up after revisional LOAGB. Our patients experienced comparable or even better outcomes compared to previous studies and LOAGB after failed plication might be an effective choice.
Jejunoileal bypass is an old malabsorptive procedure whose name is linked to liver failure and cirrhosis [32, 33]. Jejunoileal bypass has been demonstrated to cause permanent weight reduction, but long-term complications are severe. Nowadays, jejunoileal bypass is not frequently used and has become unpopular. We used modified jejunoileal bypass introduced by Fazel et al. that has been claimed to induce effective weight loss without causing hepatic failure [15]. We observed an acceptable %EWL in our series. Nevertheless, we used jejunoileal bypass early in our study, and as we moved forward, jejunoileal bypass was switched to LOAGB.
LGP and LOAGB, as original bariatric surgery, have shown comparable results in terms of %EWL [34]. In long-term follow-up, we observed comparable %EWL between re-plication and LOAGB. However, LOAGB resulted a greater %TWL. In a prospective study, Talebpour et al. demonstrated that single young females who participated in group meetings were more likely to have optimal weight loss following LGP [13]. The main issue in the selection criteria is the patient’s preference; however, we remind the possibility of weight regain in re-plication or sleeve method and emphasize the need for lifestyle modification. LOAGB is recommended for patients with reflux, diabetes, and a weak motivation for exercise or diet modification. To the best of our knowledge, this is the first study comparing re-plication with malabsorptive procedure and LOAGB as revisional surgery on failed LGP.
We observed a shorter operation time and hospital stay in re-plication compared to LOAGB and malabsorptive procedure. Similarly, other studies have showed that LGP is associated with a shorter length of hospital stay and operation duration compared to LOAGB [34]. A shorter surgical time can decrease the risk of postoperative complications, particularly infection [35] and is considered an advantage of LGP. Repetitive changes in the surgical staff due to different reasons and regrowth of bacterial flora after a time period increase the risk of contamination. In addition, infusion of larger amounts of fluids and more CO2 absorption in laparoscopy can lead to more complications. Although the length of hospital stay is related to the complexity of the operation and surgical complications, a longer hospital stay is not necessarily a disadvantage of LOAGB [34].
We had some limitations in our study. As a main limitation, no information was available about complications of revisional surgery. Second, although all the patients who entered the study were available and followed their regular visits until completion of data registry, less than half of the participants reached their follow-up visits to 36 and 48 months, which definitely hampers interpretation of the results at 36- and 48-month follow-up. Nevertheless, there was no significant difference in terms of baseline characteristics between groups of patients who did versus did not reach ≥ 36-month follow-up visit. We also suggest future randomized clinical trial studies with random allocation of patients to different revisional surgery methods following failed LGP that will provide higher level of evidence and more robust results compared to cohort design of current study. Despite these limitations, our work had some strong points. This is the first study reporting the outcome of reoperation on LGP with a long follow-up time. We had a relatively large sample size and our patients were stratified according to the reason of reoperation. Finally, we presented the outcome of three distinct procedures after failure of primary LGP. Beyond time-frame of case recruitment and data analysis in this study, we have recently identified new regain patients who are currently under observation. We are about to report their baseline characteristics as well as the results of probable reoperation in future, in our upcoming studies.
Conclusion
In conclusion, LGP seems to be less effective in severely obese patients with BMI > 45. Two-row LGP was observed to have a lower rate of weight loss failure and weight regain than one-row LGP. In terms of weight loss outcome, reoperation on failed LGP was completely successful and no treatment failure was reported. All three revisional procedures including re-plication, LOAGB, and malabsorptive procedure showed promising results and provided substantial weight loss. Since there is little information about the long-term efficacy and safety of revisional surgery on failed LGP, we highly recommend further investigations to confirm our results.
References
Kopelman P. Health risks associated with overweight and obesity. Obes Rev. 2007;8(s1):13–7.
Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14(4):435.
Tsai AG, Williamson DF, Glick HA. Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obes Rev. 2011;12(1):50–61.
Melissas J. IFSO guidelines for safety, quality, and excellence in bariatric surgery. Obes Surg. 2008;18(5):497–500.
DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356(21):2176–83.
Zeinoddini A, Heidari R, Talebpour M. Laparoscopic gastric plication in morbidly obese adolescents: a prospective study. Surg Obes Relat Dis. 2014;10(6):1135–9.
Zeinoddini A, Heidari R, Talebpour M. Reply to commentary “laparoscopic gastric plication in morbidly obese adolescents: a prospective study”. Surg Obes Relat Dis. 2014;10(6):1235–6.
Atlas H, Yazbek T, Garneau PY, et al. Is there a future for laparoscopic gastric greater curvature plication (LGGCP)? A review of 44 patients. Obes Surg. 2013;23(9):1397–403.
Talebpour M, Motamedi SM, Talebpour A, et al. Twelve year experience of laparoscopic gastric plication in morbid obesity: development of the technique and patient outcomes. Ann Surg Innov Res. 2012;6(1):7.
Gumbs AA, Pomp A, Gagner M. Revisional bariatric surgery for inadequate weight loss. Obes Surg. 2007;17(9):1137–45.
Himpens J, Coromina L, Verbrugghe A, et al. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obes Surg. 2012;22(11):1746–54.
Langer FB, Bohdjalian A, Shakeri-Manesch S, et al. Inadequate weight loss vs secondary weight regain: laparoscopic conversion from gastric banding to Roux-en-Y gastric bypass. Obes Surg. 2008;18(11):1381–6.
Talebpour A, Heidari R, Zeinoddini A, et al. Predictors of weight loss after laparoscopic gastric plication: a prospective study. J Laparoendosc Adv Surg Tech A. 2015;25(3):177–81.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276–80.
Fazel I, Pourshams A, Merat S, et al. Modified jejunoileal bypass surgery with biliary diversion for morbid obesity and changes in liver histology during follow-up. J Gastrointest Surg. 2007;11(8):1033–8.
Clinical Issues Committee. ASMBS policy statement on gastric plication. ASMBS policy statement on gastric plication. Surg Obes Relat Dis. 2011;7(3):262. https://doi.org/10.1016/j.soard.2011.03.004.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10(5):952–72.
Mann JP, Jakes AD, Hayden JD, et al. Systematic review of definitions of failure in revisional bariatric surgery. Obes Surg. 2015;25(3):571–4.
Zerrweck C, Rodriguez JG, Aramburo E, et al. Revisional surgery following laparoscopic gastric plication. Obes Surg. 2017;27(1):38–43.
Albanese A, Prevedello L, Verdi D, et al. Laparoscopic gastric plication: an emerging bariatric procedure with high surgical revision rate. Bariatr Surg Pract Patient Care. 2015;10(3):93–8.
Noun R, Skaff J, Riachi E, et al. One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg. 2012;22(5):697–703.
Brethauer SA, Harris JL, Kroh M, et al. Laparoscopic gastric plication for treatment of severe obesity. Surg Obes Relat Dis. 2011;7(1):15–22.
Niazi M, Maleki AR, Talebpour M. Short-term outcomes of laparoscopic gastric plication in morbidly obese patients: importance of postoperative follow-up. Obes Surg. 2013;23(1):87–92.
Ramos A, Galvao Neto M, Galvao M, et al. Laparoscopic greater curvature plication: initial results of an alternative restrictive bariatric procedure. Obes Surg. 2010;20(7):913–8.
Skrekas G, Antiochos K, Stafyla VK. Laparoscopic gastric greater curvature plication: results and complications in a series of 135 patients. Obes Surg. 2011;21(11):1657–63.
Fried M, Dolezalova K, Buchwald JN, et al. Laparoscopic greater curvature plication (LGCP) for treatment of morbid obesity in a series of 244 patients. Obes Surg. 2012;22(8):1298–307.
Ji Y, Wang Y, Zhu J, et al. A systematic review of gastric plication for the treatment of obesity. Surg Obes Relat Dis. 2014;10(6):1226–32.
Georgiadou D, Sergentanis TN, Nixon A, et al. Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis. 2014;10(5):984–91.
Wang W, Wei PL, Lee YC, et al. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15(5):648–54.
Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22(12):1827–34.
Bruzzi M, Voron T, Zinzindohoue F, et al. Revisional single-anastomosis gastric bypass for a failed restrictive procedure: 5-year results. Surg Obes Relat Dis. 2016;12(2):240–5.
Griffen Jr WO, Bivins BA, Bell RM. The decline and fall of the jejunoileal bypass. Surg Gynecol Obstet. 1983;157(4):301–8.
Buchwald H, Rucker R. The rise and fall of jejunoileal bypass. Surgery of the Small Intestine Appleton Century Crofts, Norwalk, CT. 1987:529–41.
Darabi S, Talebpour M, Zeinoddini A, et al. Laparoscopic gastric plication versus mini-gastric bypass surgery in the treatment of morbid obesity: a randomized clinical trial. Surg Obes Relat Dis. 2013;9(6):914–9.
Daley BJ, Cecil W, Clarke PC, et al. How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee surgical quality collaborative. J Am Coll Surg. 2015;220(4):550–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
The Institutional Review Board of Tehran University of Medical Sciences approved the study protocol.
Rights and permissions
About this article
Cite this article
Heidari, R., Talebpour, M., Soleyman-jahi, S. et al. Outcomes of Reoperation After Laparoscopic Gastric Plication Failure. OBES SURG 29, 376–386 (2019). https://doi.org/10.1007/s11695-018-3522-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3522-3