Abstract
Background
Revisional surgery has become a widely accepted alternative for weight loss failure/regain after bariatric surgery. However, it is associated to higher morbi-mortality and lesser weight loss than primary bariatric procedure. Our aims are to present a novel technique for weight loss treatment after failed laparoscopic Roux-en-Y gastric bypass (LRYGB) and to report its short-term results.
Methods
This is a retrospective analysis of patients submitted to a revisional hand-sewn double-layer gastrojejunal plication (GJP) for treatment of weight loss failure/regain after LRYGB. Analysis of demographics, body mass index (BMI), and percentage of excess weight loss (%EWL) at the 6th month complications, and financial costs involved was included.
Results
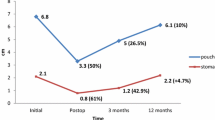
Four patients were submitted to revisional GJP. Three patients were female and the mean age at revision was 30 ± 9 years (21–44). The median time interval between LRYGB and GJP was 51 months (24–120). The median BMI at the moment of GJP and the 3rd and 6th month was 35.6 kg/m2 (32.0–37.8), 32.2 kg/m2 (29.7–34.1), and 30.7 kg/m2 (28.1–32.1), respectively. The median %EWL at the 3rd and 6th month was 35.4 % (13.6–38.9) and 46.2 % (45.1–55.5), respectively, reaching a cumulative (combined surgeries) %EWL of 62.9 % (16.5–67.9) and 71.7 % (65.1–77.6), respectively. There were no complications or mortality. Financial costs were significantly lower compared to revisional gastrojejunal stapled reduction (US$1400 cheaper).
Conclusion
Revisional GJP is a feasible, safe, and cost-effective novel procedure for treatment of weight loss failure/regain after LRYGB. Mid- and long-term results are necessary in order to establish its real effectiveness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic Roux-en-Y gastric bypass (LRYGB) is considered the “gold standard” procedure of bariatric surgery (BS). However, it fails to produce adequate and durable weight loss in 15 to 25 % of patients [1, 2]. Thus, it is estimated that up to 25 % of patients require a revisional surgery (RS) after the primary bariatric procedure [3].
Revisional procedures are indicated when an anatomical factor is implicated in weight loss failure/regain after LRYGB, such as a big gastric pouch, gastro–gastric fistula, long common limb, short alimentary limb, or a dilated gastrojejunostomy [4, 5]. In these cases, there are many alternatives for revision, including endoscopic and surgical procedures. Surgical options include the conversion of LRYGB into a more malabsorptive bariatric procedure through enlarging the alimentary or biliopancreatic limb, reducing the diameter of the gastrojejunostomy, placing an adjustable band on the gastric pouch, narrowing the gastrojejunal complex, among others [6].
The gastrojejunal sleeve reduction (GSR) is a surgical option to revise a dilated gastric pouch [6]. It consists in trimming the excess of the gastric pouch and proximal jejunum, which effectively restores satiety [6]. It has the advantage of being a simpler procedure than those that involve only reducing the diameter of the gastrojejunal anastomosis, avoiding the risk of anastomotic leak and stricture. In previous reports, it has being described by removing the excess of the gastric pouch and jejunum through a mechanical stapled resection, with the theoretical risk of leak in the stapled line and the financial costs related to the stapling devices.
In our institution, we have performed a revisional laparoscopic hand-sewn gastrojejunal plication (GJP) in a small cohort of patients, by plicating the gastric pouch and proximal jejunum, without resection. Our aims are to report our short-term results and to present this novel technique for the treatment of weight loss failure/regain after LRYGB.
Materials and Methods
This is a retrospective analysis of the electronic database of the Bariatric Program at the Digestive Surgery Department of the Pontificia Universidad Católica de Chile. Data from patients who underwent laparoscopic hand-sewn revisional GJP for weight loss failure/regain (percentage of excess weight loss, %EWL <50 %) after LRYGB were included.
Patients were submitted to RS because all of them had significant weight regain after LRYGB, refractory to medical treatment. All cases were discussed in a multidisciplinary committee including psychiatric evaluation and the decision was made in agreement with patients. Written informed consent was obtained from all patients.
Data analyzed included age, gender, body mass index (BMI), %EWL, comorbid conditions, intraoperative data, early and late complications, and mortality. BMI and %EWL evolution after the primary bariatric surgery are reported as well.
Preoperative work-up consisted in an upper gastrointestinal (GI) endoscopy and upper GI radiological series (Fig. 1) in order to evaluate anatomic abnormalities and gastric pouch dilation (>120 cc). Patients with evidence of pouch dilation on preoperative work-up were considered for surgery.
All patients were operated by a single bariatric surgeon (C.B.) using a standard novel technique described below.
Surgical Technique (Fig. 2)
Pneumoperitoneum is established using a direct view optical trocar and five trocars are placed as for a primary LRYGB. Adhesions between the gastric pouch and liver or remnant distal stomach are divided and complete anatomy of the gastric pouch, gastrojejunal anastomosis, and the alimentary limb is recognized. A 34-French orogastric bougie is inserted by the anesthesiologist and laparoscopically guided to the alimentary limb. Next, a hand-sewn running suture is performed from the upper part of the gastric pouch down to 7 cm downstream in the alimentary limb, including the gastrojejunal anastomosis. The GJP is performed with 3-0 monofilament absorbable sutures, in two sero-serosal layers, by plicating the excess of the gastric wall of the dilated pouch, with no resection. Then, the anesthesiologist removes the bougie. We do not perform methylene blue test looking for leaks and no drains are placed.
Statistical and Costs Analysis
Statistical analysis was descriptive, using non-parametric tests. Also, we present the financial costs of the revisional GJP compared to a revisional stapled GSR.
Results
In our institution, we have performed this novel technique in four patients. Basal demographic characteristics of the cohort are showed in Table 1.
Three patients were female and the mean age at the time of revision was 30 ± 9 years old (range, 21–44). All patients had a prior LRYGB, with a 150-cm alimentary limb. In addition, one patient had a prior gastric banding 2 years before the LRYGB. The median time interval between the primary LRYGB and GJP was 51 months (range, 24–120).
Two patients had medical comorbidities at the time of GJP; one had a fatty liver disease and the other had insulin resistance and arterial hypertension. Three patients had psychiatric disorders, two had an anxiety disorder and one had depression.
All patients had evidence of a dilated gastric pouch, with no other anatomic abnormalities (Fig. 1).
Pre-revision surgery anthropometrics (BMI, weight, and %EWL) of the cohort are presented in Table 2. All patients had weight regain after LRYGB.
Surgical Results
The median operative time was 68 min (range, 65–70). All patients were operated according to the technique described above, and in one patient, a cholecystectomy was performed due to a gallbladder polyp larger than 1 cm. Also, in the same patient, a stapled resection of the jejunal blind limb was performed due to significant enlargement diagnosed intraoperatively. There were no conversions to open surgery.
All patients were refed with clear liquids on the first postoperative day (POD) and were discharged on POD 2, except for the patient with the blind limb jejunal resection, who was discharged on POD 3.
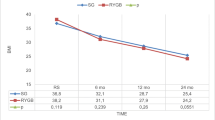
All patients were followed-up for 6 months, except for one who lost control on month 3. The median BMI was 30.7 kg/m2 (range, 28.1–32.1) and the median weight was 82.7 kg (range, 72–105), reaching a BMI loss and median %EWL of 4.9 kg/m2 (range, 3.9–5.7) and 46.2 % (range, 45.1–55.5), respectively. The combined surgery (cumulative LRYGB + GJP) median BMI loss was 11.2 kg/m2 and the median %EWL was 71.7 % (range, 65.1–77.6) at the 6th month (Table 3, Fig. 3).
There were no complications, readmissions, nor mortality in this series.
Financial Costs
Compared with the most similar revisional procedure (stapled GSR), the only difference in costs for the patient is the suture itself. Considering that a stapled GSR implies using at least two 3.5 linear 60-mm-long stapler and eventually reinforcing material (as SEAMGUARD® Bioabsorbable, W. L. Gore & Associates, Flagstaff, AZ), the cost of stapled resection is near to US$1,400, while revisional GJP has an estimated cost of US$12, which is the cost of the sutures.
Discussion
Currently, LRYGB is the most effective treatment for class II–III obesity and associated comorbidities [7–9]. However, BS is not always successful and weight regain can occur. In fact, it has been estimated that 20.4 % of morbid obese and 39.4 % of super obese patients undergoing LRYGB fails to effectively reduce their weight or may regain it within 10 years [10], requiring additional procedures.
BS failure can be attributed to anatomical factors, non-anatomical, or a combination of both. This data and the type of primary surgery performed usually determine the revision procedure that must be done, when indicated.
In the case of weight regain after LRYGB, alternatives range from endoscopic procedures such as injection of inert substances, suturing, and clipping to surgical procedures such as alimentary (Roux) limb or biliopancreatic enlargement. Each one of these approaches has its own advantages and dropouts. Endoscopic procedures, while associated with lower morbidity, have not shown to be effective in weight regain management in the long-term follow-up [11]. In contrast, surgery implies higher risk of complications but at the same time offers a more definitive alternative [12].
One of the most reported anatomical factors involved in LRYGB failure is the gastric pouch and gastrojejunostomy (stoma) enlargement [13], which reduces the restrictive component of the LRYGB and makes the alimentary limb to act as reservoir, thus diminishing satiety and causing lower weight loss or regain [14–16]. On the other hand, non-anatomical factors involved in LRYGB failure include irregular dietary behaviors, psychiatric disorders, and endocrinological dysfunction [17, 18]. In our series, the high rate of related psychiatric disorders (three of four patients)is striking, which makes us think that probably behavioral factors (as dietary transgressions) contributed to gastric pouch and stoma dilation, causing weight regain or inadequate weight loss after the primary bariatric procedure. Multidisciplinary team evaluation is essential previous to RS, in order to adequately treat psychiatric or medical disorders related and prevent future weight regain.
As described above, it is important to evaluate upper GI anatomy of patients undergoing RS, since it helps to identify potential causes of failure and rule out an anatomical complication, guiding the procedure that must be done [12]. In our series, all patients had an upper GI endoscopy and upper GI radiological series in order to evaluate anatomical abnormalities and to diagnose gastric pouch or stoma dilation (Fig. 1). Also, the preoperative work-up was useful to rule out other anatomical factors of BS failure such as gastro–gastric fistulas.
It has been reported that weight loss after RS is usually lesser than that reached after the primary bariatric surgery and depends mainly on factors mentioned above [1]. Despite of that, a significant proportion of patients achieve %EWL ≥50 % after RS. Consistent with this data, in our series, all patients achieved successfully ≥50 % of cumulative %EWL at the 6th month compared with the pre-LRYGB weight (median of 71.7 %; range, 65.1–77.6 %). Results between the first and second postoperative years (nadir %EWL) are necessary in order to reach valid conclusions at mid- and long-term follow-up.
One of the main concerns about RS is the higher morbidity and mortality due to higher frequency of wound infections, anastomotic leaks, gastrointestinal fistulas, venous thromboembolisms, and trocar site hernias compared with primary BS. The incidence of major complications after RS reaches 13–50 % and mortality rate increases to 1–2 % in some series [1, 19]. Fortunately, in our initial experience with this technique, we had no complications, readmissions, nor mortality after 6 months of follow-up. We think that abolition of gastric or jejunal resection is an advantage of the GJP compared with other revisional surgeries and this could explain the lower morbidity reported in our study.
The main limitation of our report is indeed the short-term follow-up and low number of patients included since this is a novel procedure. In prior experiences with other techniques of gastric volume reduction such as StomaphyX™ endoscopic plication (EndoGastric Solutions Inc., Redmond, WA, USA), the results in weight loss were not sustained at long term, due to dilation of the pouch and stoma over time [16]. In the case of stapled GSR [6], no significant differences were found between preoperative and postoperative BMI and %EWL at the mean follow-up of 12 months. Thus, it is necessary to evaluate our technique in a larger number of patients and for a longer period of time in order to evaluate potential risks and the true effect on weight loss. Despite these issues, we think that at least in short-term follow-up, the results of GJP seem promissory.
In conclusion, here we present a novel procedure consisting in a revisional GJP that implies less financial costs and eventually less morbidity for patients, especially leaks, since it does not involve gastric or jejunal resection, making this technique feasible and safe. Furthermore, this technique not only reduces the dilated gastric reservoir but also reaches a gastrojejunal stoma narrowing, with eventually consequent benefits on delayed gastric emptying, higher satiety, and consequently weight control. Mid- and long-term results are necessary in order to establish real effectiveness of this novel technique.
References
Radtka 3rd JF, Puleo FJ, Wang L, et al. Revisional bariatric surgery: who, what, where, and when? Surg Obes Relat Dis. 2010;6(6):635–42.
Zingg U, McQuinn A, DiValentino D, et al. Revisional vs. primary Roux-en-Y gastric bypass—a case-matched analysis: less weight loss in revisions. Obes Surg. 2010;20(12):1627–32.
Gagner M, Gentileschi P, de Csepel J, et al. Laparoscopic reoperative bariatric surgery: experience from 27 consecutive patients. Obes Surg. 2002;12(2):254–60.
Mullady DK, Lautz DB, Thompson CC. Treatment of weight regain after gastric bypass surgery when using a new endoscopic platform: initial experience and early outcomes (with video). Gastrointest Endosc. 2009;70(3):440–4.
Carrodeguas L, Szomstein S, Soto F, et al. Management of gastrogastric fistulas after divided Roux-en-Y gastric bypass surgery for morbid obesity: analysis of 1,292 consecutive patients and review of literature. Surg Obes Relat Dis. 2005;1(5):467–74.
Parikh M, Heacock L, Gagner M. Laparoscopic “gastro-jejunal sleeve reduction” as a revision procedure for weight loss failure after roux-en-y gastric bypass. Obes Surg. 2011;21(5):650–4.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309(21):2240–9.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244(5):734–40.
Dakin GF, Eid G, Mikami D, et al. Endoluminal revision of gastric bypass for weight regain—a systematic review. Surg Obes Relat Dis. 2013;9(3):335–42.
Kellogg TA. Revisional bariatric surgery. Surg Clin N Am. 2011;91(6):1353–71.
Muller MK, Wildi S, Scholz T, et al. Laparoscopic pouch resizing and redo of gastro-jejunal anastomosis for pouch dilation following gastric bypass. Obes Surg. 2005;15(8):1089–95.
Heneghan HM, Yimcharoen P, Brethauer SA, et al. Influence of pouch and stoma size on weight loss after gastric bypass. Surg Obes Relat Dis. 2012;8(4):408–15.
Abu Dayyeh BK, Lautz DB, Thompson CC. Gastro-jejunal stoma diameter predicts weight regain after Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol. 2011;9(3):228–33.
Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of reoperative bariatric surgery for failed and complicated procedures (excluding adjustable gastric banding). Obes Surg. 2011;21(8):1209–19.
Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13(4):639–48.
Sallet PC, Sallet JA, Dixon JB, et al. Eating behavior as a prognostic factor for weight loss after gastric bypass. Obes Surg. 2007;17(4):445–51.
Goyal V, Holover S, Garber S. Gastric pouch reduction using StomaphyX in post Roux-en-Y gastric bypass patients does not result in sustained weight loss: a retrospective analysis. Surg Endosc. 2013;27(9):3417–20.
Conflicts of Interest
Drs. Felipe León, Cristóbal Maiz, David Daroch, Nicolás Quezada, Mauricio Gabrielli, César Muñoz, and Camilo Boza have no conflicts of interest or financial ties to disclose.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Funding
There are no funding sources involved.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
León, F., Maiz, C., Daroch, D. et al. Laparoscopic Hand-Sewn Revisional Gastrojejunal Plication for Weight Loss Failure After Roux-en-Y Gastric Bypass. OBES SURG 25, 744–749 (2015). https://doi.org/10.1007/s11695-014-1463-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1463-z