Abstract
Background and Aim
Even though health-related quality of life (HRQOL) is considered an important component of bariatric surgery outcome, there is a lack of HRQOL measures relevant for preoperative and postoperative patients. The objective of the current study was to develop a new instrument assessing HRQOL prior to and following bariatric surgery, entitled Quality of Life for Obesity Surgery (QOLOS) Questionnaire.
Methods
Topics for the QOLOS were initially generated via open-ended interviews and focus groups with 19 postoperative bariatric surgery patients. Qualitative analysis resulted in 250 items, which were rated by patients (n = 101) and experts (n = 69) in terms of their importance. A total of 120 items were retained for further evaluation and administered to 220 preoperative patients and 219 postoperative patients. They also completed a battery of other assessments to analyze issues of construct validity.
Results
Analyses resulted in a 36-item section 1 QOLOS form targeting both preoperative and postoperative aspects across seven domains (eating disturbances, physical functioning, body satisfaction, family support, social discrimination, positive activities, partnership) and a 20-item section 2 QOLOS form focusing on postoperative concerns only (domains: excess skin, eating adjustment, dumping, satisfaction with surgery). Subscales of both sections showed acceptable to excellent internal consistency (Cronbach’s α 0.72 to 0.95) and good convergent and discriminant validity.
Conclusion
The QOLOS represents a reliable and valid instrument to assess HRQOL in preoperative and postoperative patients. Future studies should test the questionnaire in larger samples consisting of patients undergoing different types of surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In addition to weight loss and improved physical and mental diseases, health-related quality of life (HRQOL), which is one of the core concepts of “patient-reported outcomes” (PROs) [1, 2], is used to evaluate the success or failure of bariatric surgery [3,4,5,6,7,8,9,10,11]. Numerous studies have suggested an association between surgically induced weight loss and better HRQOL [5,6,7]. Furthermore, depression severity before surgery and changes in depression scores may predict postoperative HRQOL [8]. HRQOL reflects patients’ subjective perception of their health including functioning in physical, emotional, mental, and social life domains, and well-being [1]. Research on bariatric surgery frequently uses questionnaires that measure generic HRQOL (e.g., 36-Item or 12-Item Short Form Health Survey [8,9,10,11,12]) or obesity-specific HRQOL (i.e., Impact of Weight on Quality of Life-Lite [13]).
Even though HRQOL is acknowledged as an important outcome of bariatric surgery beyond changes in weight, somatic comorbidities, and psychiatric disorders [14,15,16], there is a lack of valid instruments that focus on aspects of HRQOL that are particularly relevant post surgery, such as concerns related to hanging skin, eating adjustment, dumping, or other health issues [17,18,19]. This is surprising given the increasing numbers of bariatric surgeries worldwide [20, 21]. Below, we briefly summarize the questionnaires that are currently in use.
Very simple, time-economic instruments to globally assess quality of life in bariatric surgery patients are the 6-item Moorehead-Ardelt Quality of Life Questionnaire (MAQOL) of the Bariatric Analysis and Reporting Outcome System (BAROS) [22, 23] and the 12-item Bariatric Quality of Life (BQL) index [24]. The Bariatric and Obesity-specific survey (BOSS) [25] consists of 42 items across three generic dimensions relevant to bariatric and non-bariatric patients (incapacity, work and well-being, social functioning) and three bariatric-specific domains (appearance and health, eating patterns, and sexual health). These questionnaires are limited by the lack of items concerning crucial postoperative aspects of HRQOL (e.g., excess skin, dumping, non-normative eating behavior).
Recently, researchers from Canada, UK, and USA validated the BODY-Q—an 138-item PRO measure—in weight loss and body contouring patients [26]. This questionnaire was primarily designed to address the potential impact of excess skin after weight loss on appearance and HRQOL using literature review, interviews with bariatric surgery post-weight loss body contouring patients, and input from experts [27, 28]. Applying Rasch Measurement Theory analysis, a subset of items was selected which were distributed on 18 scales across three broad domains: appearance (nine scales; e.g., abdomen, skin, scars, inner thighs), HRQOL (body image, physical, psychological, sexual, and social functioning), and experience of health care (four scales; e.g., medical team, office staff). The BODY-Q is a comprehensive, psychometrically sound instrument. However, it has a strong focus on body contouring and is time-consuming due to the high number of items. Furthermore, the application of its HRQOL domain to bariatric surgery is clearly limited by the absence of any items that relate to eating behavior, which is problematic given the relevance of this topic prior and following surgery [29,30,31].
To address the lack of a comprehensive bariatric-specific HRQOL measure, the purpose of the present study was to develop and validate such an instrument following recommendations for the assessment of HRQOL as a PRO outcome [1, 2, 32]. The subject of item generation was addressed within a previous study [33]. The present article aimed to focus on psychometric analyses to reduce the number of items and to validate the new instrument entitled Quality of Life for Obesity Surgery (QOLOS) Questionnaire in a sample including preoperative and postoperative patients.
In order to evaluate convergent validity of the new instrument, questionnaires assessing generic and obesity specific quality of life were administered. Correlations between these measures and the QOLOS were expected to be high, providing support for the convergent validity of the new instrument. Furthermore, all patients completed questionnaires assessing symptoms of anxiety, depression, and eating disorders. Correlations between these self-ratings and psychological domains of the QOLOS were assumed to be high given previous reports on the link between diminished quality of life and elevated psychopathology among bariatric surgery patients [11, 34,35,36]. Past research showed improvements in HRQOL following surgery [3, 4, 6,7,8,9,10, 16, 37, 38]. Accordingly, postoperative patients in comparison to preoperative patients were expected to exhibit higher HRQOL as measured with the QOLOS, providing support for discriminant validity.
Materials and Methods
Phase 1: Item Generation
As mentioned above, item generation was carried out within an earlier study described in detail elsewhere [33]. The procedure was based on open-ended interviews that took place from October 2013 to December 2014. An interview guideline was designed based on literature research and discussions with experts who are working with bariatric surgery patients (e.g., operating surgeons, mental health professionals, nutritionists, authors of the present article). The open-ended interviews targeted the impact of obesity and bariatric surgery on various aspects of everyday life from the patients’ perspective, including their concerns with regard to somatic complaints and comorbidity, motility, hygiene, body image and appearance, medication, eating, self-esteem, mood, social life, stigmatization, occupational functioning, partnership/family, sexuality, etc. Following the concept of data saturation, interviews were conducted until no new relevant and important information emerged. In total, 10 individual interviews with postoperative patients and focus groups with another nine postoperative patients were conducted. Patients for phase 1 were recruited within routine clinical assessments at the Department of Psychosomatic Medicine of Hannover Medical School and within self-help groups for bariatric surgery. Inclusion criteria were age of 18 years or above and a minimum duration of 6 months since surgery. Exclusion criteria were insufficient German language skills, psychosis, any developmental disorder, severe neurological disorders, cognitive impairments, and dementia. Patients who participated in individual interviews received a reimbursement of 30 €, and participants of the focus groups received 25 €. Participation in the study was completely voluntary, and all participants gave written informed consent. Phase 1 was approved by the ethics committee of Hannover Medical School on April 24, 2013.
Qualitative content analysis of audio verbatim transcripts of the interviews and focus groups was conducted supported by MAXQDA© software resulting in 250 patient items, applying an inductive approach to development of categories that was informed by theoretical considerations [39]. The importance of every item was then rated on a 3-point Likert scale (0 = not important, 1 = important, 2 = very important) by 51 preoperative patients, 50 postoperative patients (not included in item generation), and 69 experts (e.g., operating surgeons, mental health professionals, nutritionists, authors of the present article). A total of 120 items with an average importance rating of ≥ 1 were retained for further evaluation. Of those, 88 items targeted both preoperative and postoperative aspects and were summarized in section 1 of the new measure, while the remaining 32 items focused on postoperative concerns only (section 2) [33].
Phase 2: Item Reduction and Psychometric Analyses
Psychometric analyses to reduce the number of items and the validation of the new instrument were objectives of the present investigation.
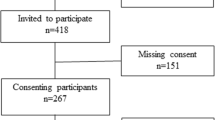
Participants
Data for the present study were collected between September 2015 and March 2016. The total sample included 220 preoperative and 219 postoperative patients (not included in phase 1). Inclusion criteria were 18 years of age or older, scheduled bariatric surgery for the preoperative group, and any kind of past bariatric surgery for the postoperative group. Exclusion criteria were cognitive impairments, psychosis, dementia, and insufficient German language skills.
Preoperative patients were recruited within routine preoperative mental health evaluations at Hannover Medical School, and postoperative patients within routine surgical care at Nordstadt Hospital Hannover (n = 178) or within self-help groups for bariatric surgery (n = 41). A doctoral student (A. O.), who was not involved in the psychiatric or surgical evaluation or in any other kind of clinical care, informed the patients about the study, asked them to participate, and collected the data.
Participation in the study was completely voluntary. All participants received a compensation of 10 €. Written informed consent was obtained from all patients according to procedures approved by the institutional ethics committee of Hannover Medical School on August 27, 2015. The study was registered as a clinical trial in the German Clinical Trials Register (trial registration DRKS00009901).
Assessment
Information on sociodemographic variables, weight, and height was self-reported. Patients further completed a questionnaire package that included the self-rating instruments described below.
First, the generated QOLOS items were administered. The initial 120-item QOLOS version started with the instruction: “Below are several statements referring to your health-related quality of life before and after bariatric surgery. Please read all statements carefully and then choose among the five answer options the one that most applies to you regarding the past 4 weeks.” The following instruction was placed after item 88 (before section 2 of the questionnaire):“Please answer the following questions only if you have already undergone bariatric surgery.” The last three items of section 2 (items 118 to 120) referred to symptoms of dumping and were introduced by the instruction: “The following three questions refer to ‘dumping’ which is the term for various physical symptoms that can appear after eating foods high in sugar. These symptoms include sweating, nausea, vomiting, diarrhea, dizziness, rapid heartbeat, weakness, restlessness, shaking.’”.
The 88 items of section 1 and the 32 items of section 2 were each displayed in a random order and the response format was consistent for each item using a 5-point Likert scale (1 = completely true, 2 = mostly true, 3 = neither true nor not true, 4 = mostly not true, 5 = completely not true). Twelve items were reversed coded. For all other items, higher scores indicated better quality of life.
As mentioned above, the first section of the QOLOS consisted of items referring to aspects that are relevant for both preoperative and postoperative patients, while section 2 contained items only relevant for postoperative patients [33]. Accordingly, section 1 was answered by all patients (preoperative and postoperative patients), while section 2 was filled out by postoperative patients only.
Generic HRQOL was measured using the German version of the 12-Item Short Form Health Survey (SF-12) [40]. Two summary measures were computed based on population norms: the Physical Component Summary (PCS) and the Mental Component Summary (MCS) score. Higher PCS/MCS scores indicate higher self-perceived physical/mental quality of life. Cronbach’s α for the components were not calculated due to the differential weighting of the items.
The 31-item German translation of the Impact of Weight on Quality of Life-Lite (IWQOL) [13, 41,42,43] was administered to assess HRQOL related to obesity. The instrument consists of the following five domains: physical functioning (11 items, α = 0.94 in current study), self-esteem (7 items, α = 0.97), sexual life (4 items, α = 0.94), public distress (5 items, α = 0.95), and work (4 items, α = 0.89). Responses are rated on a 5-point Likert scale (1 = never true, 5 = always true), with higher scores indicating better quality of life.
The Moorehead-Ardelt Quality of Life Questionnaire (MAQOL) of the BAROS [23] was used as an instrument assessing quality of life in patients who have undergone treatment for obesity (see above). Higher scores indicate better quality of life. Cronbach’s α in the current study was α = 0.89).
The mean total score of the German version of the Eating Disorder Examination-Questionnaire (EDE-Q) [44] was used to assess eating disorder symptoms. A mean global score can be calculated including 23 items (α = 0.89 in current study). Higher scores indicate more eating disturbances.
Psychopathology was assessed using the German version of the Hospital Anxiety and Depression Scale (HADS) [45]. This questionnaire does not include items referring to symptoms that may have a physical cause and is therefore considered to be unbiased by somatic conditions. The HADS consists of two 7-item subscales: one for anxiety (α = 0.83 in current study) and one for depressive symptoms (α = 0.88 in current study). Higher HADS scores indicate more psychopathology.
Statistical Analyses
All analyses were conducted using SPSS version 19.0 and Mplus version 7.11. The preoperative and postoperative samples were randomly divided into equal groups and assigned to the Development and Validation subsamples. Scale structure for the section 1 QOLOS was established on the Development subsample using exploratory factor analysis (EFA) with principal axis extraction and ProMax oblique rotation. In principal axis extraction, the diagonal of the correlation matrix among indicator variables contains a communality estimate for each variable which represents the proportion of variance in each variable which is accounted for by other variables in the model. Thus, principal axis extraction in EFA assumes that each indicator variable provides information about a latent dimension, but may also be influenced by other sources of error. Given the assumption that the factors of the QOLOS represent broad latent dimensions and not merely linear combinations of the specific indicator variables, principal axis extraction best matched the measurement model.
As the different dimensions of quality of life were assumed to be correlated at least to some extent, ProMax oblique rotation was used because this method allows for correlations among factors.
An iterative process was used to identify items that loaded strongly (> 0.40) on a primary factor with minimal cross-loadings (< 0.30) on other factors. The number of factors was established using eigenvalues from the SCREE plot, clinical interpretation of the factor content, and Horn’s parallel analysis [46]. The resultant scale structure was evaluated in the Validation sample using confirmatory factor analysis (CFA). Models were estimated with weighted least squares with mean and variance adjustment (WLSMV) for ordered categorical items. The use of WLSMV in confirmatory factor analysis is appropriate for ordered categorical items. This is particularly justified when the number of response choices is limited (5-point scale) and the distributions are not normally distributed. Model fit was evaluated based upon RMSEA ≤ 0.05, CFI ≥ 0.95, and TLI ≥ 0.95. Two models were evaluated: (1) a correlated factors model with items assigned to specific scales (based upon EFA results) and scales allowed to correlate freely; and (2) a higher-order model with items assigned to specific scales and scales contributing to a higher-order factor.
A score for the QOLOS scales was only calculated when a valid response was provided on at least two thirds of the items on that scale. For example, on a scale with six items, a valid response was required on at least four items. QOLOS scale scores represented the average of the valid responses on that scale. The QOLOS Total Score for section 1 was only calculated when a valid response was provided on at least 27 of the 36 items (75%), and for section 2 when the valid response was available on at least 15 of 20 (75%) items. The QOLOS Total Scores for section 1 and 2 represented the average of all valid responses on the questionnaire section 1 and 2.
All scores range from 1 (worst) to 5 (best). The internal consistency of the section 1 QOLOS subscale scores and the total score were evaluated using Cronbach’s alpha. Correlations between section 1 QOLOS scores and collateral measures were used to evaluate validity. Construct validity was further assessed using the known-groups method [47] comparing the section 1 QOLOS scores between preoperative and postoperative patients (t tests).
Given the smaller sample size of the postoperative sample (N = 219), the scale structure of the section 2 QOLOS was evaluated using the full postoperative sample without splitting into Development and Validation subsamples. EFA analyses were conducted following the same procedures described above. CFA was performed using the postoperative sample only to evaluate the use of a higher-order factor. Comparable procedures to those described were used to evaluate the internal consistency and convergent validity of the Post-Operative QOLOS subscale scores and the total score.
The statistical significance level for all tests was set at α of p < .01 in order to correct for family-wise error.
Results
Descriptive Characteristics
Sociodemographic characteristics and BMI, along with scores on collateral measures, are presented in Table 1. Surgeries in the postoperative sample included sleeve gastrectomy (n = 144), gastric bypass (n = 53), gastric band (n = 21), and one other procedure. The average time since bariatric surgery in the postoperative group was 25.23 months (SD = 31.69, range 0.75–200, median = 14.00, IQR = 23), and the mean weight loss was 32.8% (SD = 11.61, range 6.19–61.82, median = 32.60, IQR = 16.21). Thirty-one out of the 219 postoperative patients (14.2%) had previously undergone body contouring surgery. Time since body contouring surgery ranged between 3 weeks and 53 months (mean = 19.75 months, SD = 18.99, median = 20, IQR = 31.25).
Missing Data
Among the items from the section 1 QOLOS, 76 out of the 88 items (86.4%) had missing data rates ≤ 2.0%. Highest missing item responses emerged for two items that referred to patients’ children (10.9% missing: “With regard to my lifestyle, I am not a good model for my children”; 13.9% missing: “Because of my look, my children experience difficulties”). Among the 32 postoperative items, missing data rate for 29 items was ≤ 0.7%, and for the remaining 3 items ≤3.0%.
Section 1 QOLOS
EFA analyses in the Development subsample resulted in the identification of seven factors utilizing 36 items. Neither the pattern of factor loadings nor the results from Horn’s parallel analysis supported a smaller number of factors. Factor loadings are presented in Table 2. Factors were labeled as follows: (1) eating disturbances (nine items); (2) physical functioning (seven items); (3) body satisfaction (six items); (4) family support (three items); (5) social discrimination (four items); (6) positive activities (four items); and (7) partnership (three items). CFA analysis in the Validation subsample indicated good fit for both the correlated factors (RMSEA = 0.05; CFI = 0.97; TLI = 0.97) and the higher-order (RMSEA = 0.04; CFI = 0.97; TLI = 0.97) models.
In the total sample, missing item responses per subscale were ≤ 0.6% for eating disturbances, physical functioning, body satisfaction, family support, and positive activities and 2.5% for social discrimination. The highest missing rate was found for the subscale Partnership with 5.9%. Subsequent analyses revealed differences in response rates between patients with vs. without partner, particularly for the item “I experience enough support in my partnership,” which was not answered by 21.1% of patients without a partner compared to 0.3% of those living in a partnership. The item “It bothers me not to have a steady partner” was not answered by 2.3% of patients without a partner and by 9.7% of those with a partner. No differences were found with respect to the item “Because of my looks, I have difficulty finding a partner” (missing rates 3.1 vs. 3.9% for patients with a partner and those without a partner, respectively).
Internal consistency coefficients for section 1 QOLOS subscale scores and the total score were as follows: eating disturbances α = 0.92; physical functioning α = 0.87; body satisfaction α = 0.90; family support α = 0.84; social discrimination α = 0.80; positive activities α = 0.85; partnership α = 0.78; and general QOLOS total α = 0.95. Correlations between the section 1 QOLOS subscales ranged from 0.20 to 0.70. Section 1 QOLOS subscales and total scores are presented in Table 3 for the preoperative and postoperative groups. As expected, the postoperative group had significantly higher scores (i.e., better HRQOL) on all section 1 QOLOS scales, with the exception of the Partnership subscale. Men and women did not differ in the General QOLOS total score or in subscales scores.
Correlations between the section 1 QOLOS scores and collateral measures are presented in Table 4. All correlations are significant (p < .001). Notable findings are the strong correlations between the section 1 QOLOS Eating Disturbances scale and the EDE-Q Global score (r = −.60), the section 1 QOLOS Physical Functioning and the IWQOL Physical Functioning (r = .85) and the SF-12 PCS (r = .82) scales, between the section 1 QOLOS Body Satisfaction scale and the IWQOL Self-Esteem scale (r = .86), between the section 1 QOLOS Social Discrimination scale and the IWQOL Public Distress (r = .67) and Work (r = .73) scales, and between the section 1 QOLOS Positive Activities scale and the HADS Depression subscale (r = −.74).
Section 2 QOLOS
EFA analyses in the full postoperative sample resulted in the identification of four factors utilizing 20 items. Horn’s parallel analysis supported the four-factor solution. Factor loadings are presented in Table 5. Factors were labeled as follows: (1) excess skin (eight items); (2) eating adjustment (five items); (3) dumping (three items); and (4) satisfaction with surgery (four items). CFA analysis in the same sample indicated good fit for the higher-order model (RMSEA = 0.05; CFI = 0.98; TLI = 0.98).
Missing item responses per subscale were 0.3% for excess skin, 0.1% for eating adjustment, 2.7% for dumping, and 0.1% for satisfaction with surgery. Internal consistency coefficients for the section 2 QOLOS subscales and the total score were as follows: excess skin α = 0.93; eating adjustment α = 0.79; dumping α = 0.89; satisfaction with surgery α = 0.72; and section 2 QOLOS total α = 0.87. Correlations between the section 2 QOLOS subscales ranged from 0.11 to 0.44. Mean (SD) scores on the section 2 QOLOS subscales and the total scale were as follows: excess skin 3.38 (1.15); eating adjustment 4.14 (0.87); dumping 4.19 (1.05); satisfaction with surgery 4.44 (0.68); and total 3.90 (0.67). Dumping subscale scores did not differ by surgery type (F (2, 201) = 0.52, p = .59). Similarly, no differences by surgery type were found for the other subscales (p ≥ .102). No gender differences were found with regard to the section 2 QOLOS total score or subscales.
Correlations of the section 2 QOLOS scales with the section 1 QOLOS scales and collateral measures are presented in Table 6. Notable findings include the strong correlation between the section 2 QOLOS Excess Skin and the section 1 QOLOS Body Satisfaction scales (r = .44), between the section 2 QOLOS Eating Adjustment and the section 1 QOLOS Eating Disturbances scales (r = .46), between the section 1 QOLOS Dumping and the SF-MCS (r = .37), HADS Depression (r = −.36) and HADS Anxiety scales (r = −.38), and the strong correlation between the scores of the total scales of the section 2 QOLOS and the section 1 QOLOS (r = .60). Correlations between the section 2 QOLOS total scale and total scores of other measures assessing HRQOL (i.e., IWQOL, SF-12 PCS, SF-12 MCS, MAQOL; Table 6) were significantly weaker than correlations between the section 1 QOLOS total score and these measures (Table 4) (z ≥ 2.49, p < .01).
Body mass index, percent weight loss, and time since surgery were not related to the section 2 QOLOS total score. Significant (p < .01), albeit weak, correlations were found between the section 2 QOLOS Body Satisfaction scale and BMI (r = −.19), percent weight loss (r = .21), and months since surgery (r = −.19).
Discussion
The present study aimed at developing and evaluating a new instrument to assess HRQOL prior to and following bariatric surgery. Below, the results are discussed with regard to psychometric properties and the additional value of the new bariatric-specific questionnaire.
The findings of the factor analyses revealed a 7-factor solution for the section 1 QOLOS with 36 items loading on the dimensions eating disturbances, physical functioning, body satisfaction, family support, social discrimination, positive activities, and partnership. Internal consistencies of the total scale and the subscales were good to excellent. The high correlations between the total score of the section 1 QOLOS and other HRQOL measures support the convergent validity of this part of the new instrument (.59 ≤ r ≤ .87). With respect to the subscales, the section 1 QOLOS Physical Functioning scale was highly correlated (r ≥ .82) with subscales of other instruments that also target physical functioning, particularly the IWQOL Physical Functioning, and the SF-12 PCS (convergent validity), but showed relatively low correlations (p < .50) with mental health measures such as the SF-12 MCS and the HADS Anxiety (discriminant validity). Convergent validity of the section 1 QOLOS Eating Disturbances scale was supported by the strong correlation with the EDE-Q Global score, which assesses eating disorder symptoms. In contrast, this scale was only weakly correlated with the SF-12 PCS (discriminant validity). Furthermore, the section 1 QOLOS Social Discrimination scale and the IWQOL subscales Public Distress and Work were highly correlated. This speaks for the convergent validity of the section 1 QOLOS Social Discrimination scale that contains items referring to professional development, finding a job, disadvantages in daily life because of the perceived look, and financial problems [48,49,50,51]. The section 1 QOLOS Body Satisfaction scale was positively correlated with the IWQOL Self-Esteem scale. This finding is in accordance with prior studies concerning the link between body dissatisfaction and low self-esteem [52,53,54]. The section 1 QOLOS total scale showed a high inverse correlation with the HADS-Depression subscale. This is in line with past reports on the association between extreme obesity and mood disturbances [55], elevated depression scores among bariatric surgery candidates [11], and the predictive value of changes in depression scores for postoperative HRQOL [8]. In the same vein, convergent validity of the section 1 QOLOS Positive Activities scale was supported by its negative correlation with the HADS Depression subscale, given that loss of interest or reduced pleasure in daily activities is one of the key symptoms of depressive disorder [56]. The postoperative group reported significantly higher scores (i.e., better HRQOL) on most section 1 QOLOS scales than the preoperative group, which is in line with the literature reporting improved HRQOL following surgery [3, 4, 6,7,8,9,10, 16, 37, 38]. In summary, these findings provide strong support for the validity of the section 1 QOLOS.
Noteworthy is the relatively high missing response rate of the section 1 QOLOS Partnership scale (5.9% in the total sample), which was mostly attributable to the item “I experience enough support in my partnership.” A reasonable percentage of patients not currently living in a partnership did not provide any response to this item. This suggests a potential limitation of the Partnership scale in its current form and the need for further evaluation of this scale. With regard to the abovementioned item, future studies may profit from adding a specific instruction to increase the validity of this item (e.g., “Please answer the next question only, if you have a partner. If you do not have a partner, please go to question #X.”). Furthermore, an instrument assessing relationship quality or dyadic functioning should be used to investigate the validity of this subscale considering the known association between relationship functioning and individual well-being [57].
Item response rates for the section 2 QOLOS were relatively high, with missing scale scores highest—albeit acceptably—for the Dumping subscale (2.5%). Factor analyses resulted in a 20-item version with four specific postoperative dimensions labeled as excess skin, eating adjustment, dumping, and satisfaction with surgery. The section 2 QOLOS subscales showed acceptable to excellent reliability. Discriminant validity could be demonstrated by the lower correlations between the section 2 QOLOS total scale and other HRQOL measures (almost all r < .50) compared to the correlations between these measures and the section 1 QOLOS total scale, suggesting that the second part of the new instrument covers specific postoperative aspects that are not directly assessed by other HRQOL measures (i.e., IWQOL, SF-12, MAQOL).
In terms of convergent validity, we found relatively strong correlations between the section 2 QOLOS Dumping scale and instruments assessing mental health or psychopathology. Lower scores on the Dumping scale (indicating more problems with dumping) were notably related to lower generic mental HRQOL (SF-MCS), and to elevated anxiety and depressive symptoms (HADS). It is well known that late dumping symptoms may include mental confusion, decreased consciousness, fatigue, and difficulty to concentrate [58]. These emotionally distressing complications of bariatric surgery can lead to anxiety and dysphoria [59, 60]. Hence, lower postoperative HRQOL related to dumping symptoms may come along with lower self-perceived mental health and more psychopathology.
Dumping syndrome occurs mainly after gastric bypass [61]. Therefore, lower scores on the Dumping subscale may have been expected in gastric bypass patients. However, there were no differences in Dumping subscale scores by surgery type, which questions the construct validity of this subscale. In order to avoid confusion, the three items concerning dumping symptoms were preceded by a short explanation of dumping (see “Assessment” section), which might need revision given that some patients most likely misunderstood the word dumping. Furthermore, the relatively low number of gastric bypass patients in our sample, or the possibility of dumping symptoms in sleeve gastrectomy patients [59], might have contributed to the lack of differences. Future studies using the QOLOS should not only adopt the instruction but also include a dumping-specific questionnaire (e.g., the Sigstad Clinical Diagnostic Index [60]) to further investigate the validity of the section 2 QOLOS Dumping scale.
As assumed, there was a close link between section 1 and section 2 of the QOLOS. Strong correlations were found between scales pertaining to body image (section 2 QOLOS Excess Skin and section 1 QOLOS Body Satisfaction scales) or eating (section 2 QOLOS Eating Adjustment and section 1 QOLOS Eating Disturbances scales).
Interestingly, no significant association was found between the section 2 QOLOS total score and BMI, percent weight loss, and months since surgery. With respect to section 2 QOLOS subscales, the Satisfaction with surgery subscale was negatively related to BMI and months since surgery, and positively related to percent weight loss. However, these correlations were very weak (r ≤ I .21I). The missing association between section 2 QOLOS and weight-related variables as well as time since surgery might be caused by the left-skewed distribution of time since surgery in the current postoperative sample (i.e., most patients received surgery within the past 2 years). Future studies using the QOLOS should include larger cohorts of more strictly defined postsurgical timelines and patients undergoing different types of surgery.
The current study has several notable strengths. First, the QOLOS was developed based upon feedback from patients, as well as experts in the field, following international guidelines [1] for the development of HRQOL measures. The new multidimensional instrument was designed to assess the impact of obesity and bariatric surgery on daily life from the patients’ perspective, covering a wide range of aspects that were rated as highly important by prebariatric and postbariatric surgery patients themselves and by experts in the field of bariatric surgery. The sample size in the current study was sufficiently large to allow confirmation of the factor structure of the section 1 QOLOS in an independent sample, and the initial psychometric properties of the QOLOS appear to be quite strong. The findings indicate that the QOLOS provides additional value beyond other HRQOL questionnaires that are generic (like the SF-12), extremely short (like the MAQOL of the BAROS), not specifically designed for bariatric surgery (like the IWQOL), rather developed for body contouring patients (like the BODY-Q), or that miss important postoperative topics. In summary, the results indicate potential clinical utility of the QOLOS for assessing the course of HRQOL in bariatric surgery patients. Section 1 can be used pre and post surgery and allows for comparisons. Following surgery, it can be supplemented by section 2 that complements the assessment by addressing specific postoperative domains that are of relevance following surgery only (e.g., excess skin, postoperative non-normative eating behavior, dumping syndrome). Clinicians and researchers alike may benefit by having a comprehensive, time-economic questionnaire that is made to assess HRQOL concerns that are relevant prior and following bariatric surgery. The combination of sections 1 and 2 could be useful as an outcome measure in clinical research and as a tool to facilitate healthcare providers’ and patients’ awareness for improvements and possible deteriorations following surgery. Hence, it appears that the QOLOS may fill a gap in the field of bariatric surgery.
Nevertheless, the present findings should be considered in light of several limitations. First, QOLOS data from the current study were based upon the original German version. While the QOLOS has been translated by a professional translator into American English, the psychometric properties of this translated version have yet to be evaluated. The extent to which the wording of some of the instructions and some of the items may need revision remains an important open question which should be considered in future studies. Second, data from the current study are cross-sectional; the sensitivity to change and the test-retest reliability of the QOLOS have not been established. Also, divergent validity has not been thoroughly assessed. Third, due to sample size limitations, the factor structure of the section 2 QOLOS has not yet been confirmed in an independent sample. Fourth, the proportion of bypass patients in the current postoperative sample was relatively small and the majority of patients received surgery within the previous 2 years, raising questions about the use of the QOLOS to assess the long-term impact of bariatric surgery. Finally, patients in the current study were recruited from a single site in Germany, limiting our ability to generalize these findings to other patient populations. These limitations indicate future studies implementing the QOLOS. Cross-cultural research projects using a longitudinal design are needed to test the questionnaire in larger samples consisting of patients undergoing different types of surgery.
Conclusion
Taken together, the QOLOS (which is available for the public domain upon request from the first or last author) represents a reliable and valid instrument that can be applied to assess HRQOL in preoperative and postoperative patients. The assumption that—with respect to bariatric surgery—the QOLOS is superior to existing HRQOL instruments needs further empirical verification.
References
Bullinger M, Quitmann J. Quality of life as patient-reported outcomes: principles of assessment. Dialogues Clin Neurosci. 2014;16(2):137–45.
FDA. Guidance for industry. Patient-reported outcome measures: use in medical product development to suport labeling claims. 2009 [December 16, 2016]; Available from: http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf.
Raaijmakers LC, Pouwels S, Thomassen SE, et al. Quality of life and bariatric surgery: a systematic review of short- and long-term results and comparison with community norms. Eur J Clin Nutr. 2017;71(4):441–9.
Andersen JR, Aasprang A, Karlsen TI, et al. Health-related quality of life after bariatric surgery: a systematic review of prospective long-term studies. Surg Obes Relat Dis. 2015;11(2):466–73.
Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22(4):668–76.
Alvares RS, Beleigoli AM, Cancado AG, et al. Quality of life and weight loss in the long term after gastric bypass. Obes Surg. 2017;27(4):1069–70.
Reynolds CL, Byrne SM, Hamdorf JM. Treatment success: investigating clinically significant change in quality of life following bariatric surgery. Obes Surg. 2017;27(7):1842–8.
Peterhänsel C, Nagl M, Wagner B, et al. Predictors of changes in health-related quality of life 6 and 12 months after a bariatric procedure. Obes Surg. 2017;27(8):2120–8.
Biter LU, van Buuren MMA, Mannaerts GHH, Apers JA, Dunkelgrun M, Vijgen G, 2017. Quality of life 1 year after laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass: a randomized controlled trial focusing on gastroesophageal reflux disease. Obes Surg . doi: 10.1007/s11695-017-2688-4.
Monteiro F, Ponce DA, Silva H, et al. Physical function, quality of life, and energy expenditure during activities of daily living in obese, post-bariatric surgery, and healthy subjects. Obes Surg. 2017;27(8):2138–44.
Osterhues A, von Lengerke T, Mall JW, de Zwaan M, Müller A, 2017. Health-related quality of life, anxiety, and depression in bariatric surgery candidates compared to patients from a psychosomatic inpatient hospital. Obes Surg. doi: 10.1007/s11695-017-2629-2.
Ware JE, Snow K, Kosinski M, et al. SF-36 Health Survey: manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1993.
Kolotkin RL, Crosby RD. Manual for the impact of weight on quality of life measure (IWQOL and IWQOL-Lite). Obesity and Quality of Life Consulting: Durham, NC; 2008.
De Luca M, Angrisani L, Himpens J, et al. Indications for surgery for obesity and weight-related diseases: position statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg. 2016;26(8):1659–96.
Runkel N, Colombo-Benkmann M, Hüttl TP, et al. Evidence-based German guidelines for surgery for obesity. Int J Color Dis. 2011;26(4):397–404.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26(2):395–409.
de Zwaan M, Hilbert A, Swan-Kremeier L, et al. Comprehensive interview assessment of eating behavior 18-35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis. 2010;6(1):79–85.
Gilmartin J, Bath-Hextall F, Maclean J, et al. Quality of life among adults following bariatric and body contouring surgery: a systematic review. JBI Database System Rev Implement Rep. 2016;14(11):240–70.
Coulman KD, Howes N, Hopkins J, et al. A comparison of health professionals’ and patients’ views of the importance of outcomes of bariatric surgery. Obes Surg. 2016;26(11):2738–46.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Stroh C, Weiner R, Benedix F, et al. Adipositas- und metabolische Chirurgie in Deutschland 2012 - Ergebnisse der Qualitatssicherungsstudie zur operativen Therapie der Adipositas (GBSR). [bariatric and metabolic surgery in Germany 2012 - results of the quality assurance study on surgery for obesity (data of the German Bariatric Surgery Registry)]. Zentralbl Chir. 2014;139(2):e1–5.
Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (BAROS). Obes Surg. 1998;8(5):487–99.
Oria HE, Moorehead MK. Updated bariatric analysis and reporting outcome system (BAROS). Surg Obes Relat Dis. 2009;5(1):60–6.
Weiner S, Sauerland S, Fein M, et al. The Bariatric Quality of Life index: a measure of well-being in obesity surgery patients. Obes Surg. 2005;15(4):538–45.
Tayyem RM, Atkinson JM, Martin CR. Development and validation of a new bariatric-specific health-related quality of life instrument “bariatric and obesity-specific survey (BOSS)”. J Postgrad Med. 2014;60(4):357–61.
Klassen AF, Cano SJ, Alderman A, et al. The BODY-Q: a patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open. 2016;4(4):e679.
Klassen AF, Cano SJ, Scott A, et al. Satisfaction and quality-of-life issues in body contouring surgery patients: a qualitative study. Obes Surg. 2012;22(10):1527–34.
Klassen AF, Cano SJ, Scott A, et al. Assessing outcomes in body contouring. Clin Plast Surg. 2014;41(4):645–54.
Ivezaj V, Kessler EE, Lydecker JA, et al. Loss-of-control eating following sleeve gastrectomy surgery. Surg Obes Relat Dis. 2017;13(3):392–8.
Devlin MJ, King WC, Kalarchian MA, et al. Eating pathology and experience and weight loss in a prospective study of bariatric surgery patients: 3-year follow-up. Int J Eat Disord. 2016;49(12):1058–67.
Mitchell JE, Christian NJ, Flum DR, et al. Postoperative behavioral variables and weight change 3 years after bariatric surgery. JAMA Surg. 2016;151(8):752–7.
Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002;11(3):193–205.
Selle J. Entwicklung eines gesundheitsbezogenen Lebensqualitätsfragebogens bei Adipositaschirurgie [development of a HRQOL questionnaire for bariatric surgery]. Doctoral thesis. Hannover Medical School: Hannover; 2017.
Herpertz S, Müller A, Burgmer R, et al. Health-related quality of life and psychological functioning 9 years after restrictive surgical treatment for obesity. Surg Obes Relat Dis. 2015;11(6):1361–70.
Green DD, Engel SG, Mitchell JE. Psychological aspects of bariatric surgery. Curr Opin Psychiatry. 2014;27(6):448–52.
Müller A, Mitchell JE, Sondag C, et al. Psychiatric aspects of bariatric surgery. Curr Psychiatry Rep. 2013;15(10):397.
Driscoll S, Gregory DM, Fardy JM, et al. Long-term health-related quality of life in bariatric surgery patients: a systematic review and meta-analysis. Obesity (Silver Spring). 2016;24(1):60–70.
Aasprang A, Andersen JR, Vage V, et al. Five-year changes in health-related quality of life after biliopancreatic diversion with duodenal switch. Obes Surg. 2013;23(10):1662–8.
Mayring P. Qualitative Inhaltsanalyse. Beltz: Weinheim und Basel; 2010.
Morfeld M, Kirchberger I, Bullinger M. SF-36 Fragebogen zum Gesundheitszustand: Deutsche Version des Short Form-36 Health Survey. Göttingen: Hogrefe; 2011.
Kolotkin RL, Crosby RD, Williams GR. Assessing weight-related quality of life in obese persons with type 2 diabetes. Diabetes Res Clin Pract. 2003;61(2):125–32.
Kolotkin RL, Crosby RD, Kosloski KD, et al. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–11.
Mueller A, Holzapfel C, Hauner H, et al. Psychometric evaluation of the German version of the impact of weight on Quality of Life-Lite (IWQOL-Lite) questionnaire. Exp Clin Endocrinol Diabetes. 2011;119(2):69–74.
Hilbert A, Tuschen-Caffier B. Eating disorder examination—questionnaire. Deutsche Übersetzung. Verlag für Psychotherapie: Münster; 2006.
Herrmann-Lingen C, Buss U, Snaith RP. Hospital anxiety and depression scale: Deutsche version. Bern: Huber; 2011.
Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–85.
Hattie J, Cooksey RW. Procedures for assessing the validities of tests using the “known-groups” method. Appl Psychol Meas. 1984;8(3):295–305.
Giel KE, Thiel A, Teufel M, et al. Weight bias in work settings—a qualitative review. Obes Facts. 2010;3(1):33–40.
Giel KE, Zipfel S, Alizadeh M, et al. Stigmatization of obese individuals by human resource professionals: an experimental study. BMC Public Health. 2012;12:525.
Sarwer DB, Fabricatore AN, Eisenberg MH, et al. Self-reported stigmatization among candidates for bariatric surgery. Obesity (Silver Spring). 2008;16(Suppl 2):S75–9.
Vartanian LR, Fardouly J. The stigma of obesity surgery: negative evaluations based on weight loss history. Obes Surg. 2013;23(10):1545–50.
Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: a prospective analysis. J Abnorm Psychol. 2005;114(1):119–25.
van den Berg PA, Mond J, Eisenberg M, et al. The link between body dissatisfaction and self-esteem in adolescents: similarities across gender, age, weight status, race/ethnicity, and socioeconomic status. J Adolesc Health. 2010;47(3):290–6.
de Zwaan M, Georgiadou E, Stroh CE, et al. Body image and quality of life in patients with and without body contouring surgery following bariatric surgery: a comparison of pre- and post-surgery groups. Front Psychol. 2014;5:1310.
Fabricatore AN, Wadden TA, Sarwer DB, et al. Health-related quality of life and symptoms of depression in extremely obese persons seeking bariatric surgery. Obes Surg. 2005;15(3):304–9.
APA. Diagnostic and Statistical Manual of mental disorders. 5th ed. Washington DC: American Psychiatric Press; 2013.
Whisman MA, Baucom DH. Intimate relationships and psychopathology. Clin Child Fam Psychol Rev. 2012;15(1):4–13.
Tack J, Arts J, Caenepeel P, et al. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol. 2009;6(10):583–90.
van Beek AP, Emous M, Laville M, et al. Dumping syndrome after esophageal, gastric or bariatric surgery: pathophysiology, diagnosis, and management. Obes Rev. 2017;18(1):68–85.
Kalarchian MA, Marcus MD, Courcoulas AP, et al. Self-report of gastrointestinal side effects after bariatric surgery. Surg Obes Relat Dis. 2014;10(6):1202–7.
Ramadan M, Loureiro M, Laughlan K, et al. Risk of dumping syndrome after sleeve gastrectomy and Roux-en-Y gastric bypass: early results of a multicentre prospective study. Gastroenterol Res Pract. 2016;2016:2570237.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
All procedures were in accordance with the ethical standards of the institutional research committee of the Hannover Medical School and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
This work was supported by a grant from the Federal Ministry of Education and Research within the German Obesity Competence Network (01GI1324) and by the Else-Kröner-Fresenius Foundation as part of the structured doctoral program “ClinStrucMed.”
Rights and permissions
About this article
Cite this article
Müller, A., Crosby, R.D., Selle, J. et al. Development and Evaluation of the Quality of Life for Obesity Surgery (QOLOS) Questionnaire. OBES SURG 28, 451–463 (2018). https://doi.org/10.1007/s11695-017-2864-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2864-6