Abstract
Objectives
This study aimed to evaluate physical function (PF), quality of life (QOL), and energy expenditure (EE) during activities of daily living (ADL) in late outcome post-bariatric surgery (BS) patients and to compare them to severe obese individuals and matched controls.
Methods
Sixty-three subjects were included: 21 patients in post-operative (PO) of BS (3–4 years post-Roux-en-Y gastric bypass) with a stable weight for at least 6 months (16 women, 41 ± 11 years old, BMI = 28 ± 4 kg m−2) (group PO); 21 obese individuals with BS indication (16 women, 44 ± 9 years old, BMI = 44 ± 6 kg m−2) (group OB); and 21 controls matched to PO by gender, age, and BMI (16 women, 42 ± 12 years old, BMI = 27 ± 6 kg m−2) (group MC). PF was objectively assessed by the Glittre and modified Glittre ADL-tests. QOL (SF-36), EE (activity monitoring during ADL), and body composition (bioelectrical impedance) were also assessed.
Results
OB had worse PF (Glittre ADL-test) compared to PO and MC (OB = 224 ± 76 s; PO = 143 ± 39 s; and MC = 118 ± 17 s; p < 0.0001). The same was observed for QOL (p < 0.05 for all SF-36 domains). OB also had higher total EE in the Glittre ADL-test. However, 63% of the activity time was in low-intensity EE. In the Glittre modified protocol, OB had poorer performance than PO and MC when walking up/downstairs, rising/sitting in a chair, and moving objects on a shelf.
Conclusions
Post-BS patients have better PF and QOL and perform activities under lower total EE than obese subjects, very similar to matched controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is strongly associated with type 2 diabetes mellitus, cardiovascular diseases, and decreased musculoskeletal function, resulting in the increased risk of death from all causes [1, 2]. Obese individuals often present marked impairment in their physical function (PF or functionality), and this is closely related to poorer quality of life (QOL) and more pronounced difficulties in performing activities of daily living (ADL) [3, 4]. Many studies have demonstrated the effectiveness of bariatric surgery (BS), mainly the Roux-en-Y gastric bypass (RYGB) technique, in both weight loss and comorbidity control [5, 6]; however, few studies have investigated PF outcomes following weight loss induced by BS [7, 8]. Considering that RYGB is a partial anti-absorptive technique [9], we could speculate whether the physical functionality in performing ADL could be restored and reach the same performance found in individuals matched for body mass index (BMI). In addition to this, we could identify if these patients remain with any degree of physical dysfunctionality despite significant weight loss.
The use of self-reported questionnaires to measure PF in obese individuals has proved to be an inaccurate method due to the common under- or overestimate perception [10]. Nevertheless, in order to fully elucidate one’s functionality, it would be useful to provide a wider perspective. The Glittre ADL-test was developed to address the need for a broader and more representative objective assessment of function, using ADL-like activities.
Another challenge faced by post-BS patients is metabolic changes. Due to large weight loss, patients also have significant loss of lean body mass and decrease in total energy expenditure (EE) [11, 12]. Faria et al. [13] showed that resting EE reduction contributed to weight regain and also found that patients who maintain weight loss after BS had a resting EE of around 260 kcal/day higher than those who failed to maintain their weight loss. Considering that weight maintenance derives from the balance between energy intake and EE, spontaneous and planned physical activities are important variables in this equation [14]. However, to the best of our knowledge, no study has analyzed EE during ADL in post-BS patients.
The aim of this study was to evaluate PF, QOL, and EE during ADL in post-BS patients (3 to 4 years post-BS) and compare them with severely obese individuals not submitted to BS and matched control individuals. We also intended to investigate correlations of PF with EE, QOL, and body composition in these subjects.
Subjects and Methods
Study Participants
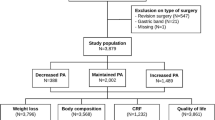
Sixty-five subjects were included in the study: 21 post-BS patients (3 to 4 years after Roux-en-Y gastric bypass) with a stable weight for at least 6 months (PO group: 16 women, 41 ± 11 years old, BMI = 28 ± 4 kg m−2); 23 obese individuals with BS indication according to the World Health Organization’s recommendations [15] (OB group: 16 women, 44 ± 9 years old, BMI = 44 ± 6 kg m−2); and 21 control individuals, matched to the PO group by gender, age, and BMI (MC group: 16 women, 42 ± 12 years old, BMI = 27 ± 6 kg m−2). Post-BS patients were recruited from a list provided by the statistical service of Londrina State University Hospital (HU-UEL) and Londrina Gastro Clínica Hospital. OB group subjects were recruited from the databank of HU-UEL or other obesity projects conducted in the Londrina area, whereas MC group individuals were invited from the community. Exclusion criteria were the presence of uncontrolled high blood pressure or diabetes mellitus, liver or kidney disease, cancer, pulmonary diseases and severe cardiomyopathies, neurologic diseases, wasting syndrome, chronic use of corticosteroids, musculoskeletal diseases, or physical limitations that could hinder the subjects’ performance in the proposed tests. The study was approved by the institutional ethics committee and each participant provided written informed consent to participate.
Assessments
PF, QOL, and EE during ADL and body composition were assessed in a single day. An interview was also performed to obtain personal information about the presence of comorbidities and drug use, pain complaints, educational level, and work-related and physical-related characteristics.
PF was estimated by the Glittre ADL-test [16], a standardized test which includes ADL activities involving rising from a chair, lifting, carrying, and bending. A previous study has confirmed the validity and reproducibility of this test for obese and post-BS individuals [17]. Heart rate (HR), peripheral oxygen saturation (SpO2), blood pressure (BP), and Borg scores (0–10) for dyspnea and fatigue were measured before and after the test. EE was also measured during the test with the activity monitor as described below. The protocol was performed twice with a 30-min interval, and the shortest duration was used for the analysis.
In order to access PF and EE in each circuit activity, subjects were submitted to a modified version of the Glittre ADL-test [18]. It included the same activities performed in the Glittre ADL-test, but performed during 2 min each: walking on the level, walking on the level carrying a backpack (10% of their body weight), rising from a chair and sitting in another chair positioned 1 m across, walking up/downstairs (two steps), and moving an object weighting 1 kg from shelves. Activities were performed in random order, and the time between them was determined by the return of HR, BP, and SpO2 to resting values. HR, SpO2, BP, and Borg scores (0–10) were also measured before and after the test. The protocol was concurrently videotaped by a digital camera as a criterion method for walking distance, in meters or number of repetitions that the activity was performed.
The multisensor SenseWear armband (SAB) activity monitor (BodyMedia Inc., Pittsburgh, PA, USA) was used to evaluate EE during the Glittre ADL-test and the modified Glittre ADL-test. The device estimates EE and also provides the duration of activities performed at different intensities (e.g., time spent in light, moderate, and vigorous intensities) [19]. The SAB has already been used in obese and post-BS patients for measuring EE [4, 20].
Quality of life was assessed by the Portuguese version of the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) [21] and body composition by bioelectrical impedance (BIA) (Biodynamics 310®, Biodynamics Corp., Seattle, WA, USA) [22].
Statistical Analysis
Statistical analysis was performed using the GraphPad Prism 6.0 (GraphPad Software, San Diego, CA, USA) program. The Shapiro-Wilk test was used to check for normal distribution. According to normality in data distribution, comparisons between groups were performed using ANOVA or Kruskal-Wallis tests, followed by a post hoc test (Bonferroni or Dunn, respectively). Similarly, in order to compare changes between pre- and post-BS in PO, the Student paired t or Wilcoxon tests were used. Correlations were studied using the Pearson or Spearman coefficient, also according to the normality in data distribution. A significance level of p ≤ 0.05 was adopted.
Results
Twenty-one individuals were included in the PO (42 ± 3 months post-BS) and MC groups, and 23 individuals were included in the OB group. Two patients from OB were excluded for presenting a marked increase in blood pressure during the protocol. All patients in the PO group succeeded in losing weight after the BS (weight loss equal to or greater than 50% of excess body weight) (Table 1).
All subjects from the OB group had one or more comorbidities: hypertension (81%), musculoskeletal disorders (such as osteoarthritis, osteoarthrosis, and back conditions [e.g., lordosis or kyphosis]) (62%), dyslipidemia (48%), anxiety/depression (33%), and diabetes mellitus (24%), whereas in the PO and MC groups, comorbidities were detected in only 33% of the subjects (p < 0.0001, OB versus PO and MC). The prevalence of comorbidities decreased in the PO group after BS (95% before BS versus 33% after BS, p = 0.0002) as well as BMI reduced in average 15 kg m−2 post-operatively (43 ± 7 to 28 ± 4 kg m−2, p < 0.0001) in comparison with the self-reported pre-surgery BMI. Regarding regular physical activity practice, 33% of the OB, 52% of the PO, and 38% of the MC groups self-reported to perform it regularly (p = 0.43). The majority of patients from the OB and PO groups reported chronic musculoskeletal pain (81 and 62%, respectively), while only 29% in the MC group had that complaint (p = 0.003, OB versus MC).
Glittre ADL-Test
Physical function evaluated by the performance in the Glittre ADL-test was worse in OB when compared to PO and MC (OB = 224 ± 76 s; PO = 143 ± 39 s; and MC = 118 ± 17 s; p < 0.0001). The OB group had higher total EE when compared to PO and MC (24 ± 10, 12 ± 4, and 12 ± 4 cal, respectively, p < 0.05). However, when taking into account the EE by time, the OB spent 63% of the time in light activities (i.e., low energy expenditure), 37% in moderate activities, and no time in vigorous activities. Otherwise, PO spent 51% of the time in light activities, 42% in moderate activities, and 7% in vigorous activities, whereas MC spent 44% in light activities (p = 0.02 versus OB), 52% in moderate activities, and 4% in vigorous activities.
Modified Glittre ADL-Test
When evaluating the Glittre activities separately in the modified protocol, OB had poorer performance than PO and MC in walking up/downstairs (OB = 22 ± 6; PO = 32 ± 9; and MC = 34 ± 7 repetitions), rising and sitting in a chair (OB = 30 ± 7; PO = 40 ± 8; and MC = 43 ± 10 repetitions), and moving objects on shelves (OB = 8 ± 2; PO = 11 ± 3; and MC = 12 ± 1 repetitions) (p < 0.0001 for all activities), therefore showing that in these activities, PO had similar PF in comparison with MC (Fig. 1). Concerning walking activities, MC showed significantly better results (with and without backpack) compared to OB and PO (walking: OB = 140 ± 32; PO = 168 ± 20; MC = 190 ± 24 m; and walking with a backpack: OB = 138 ± 32; PO = 158 ± 24; MC = 182 ± 26 m; p < 0.0001 for both) (Fig. 1). Furthermore, out of the five activities, OB showed a significantly lower average EE in three of them (walking up/downstairs, rising/sitting in a chair, and moving objects up and down in shelves). A statistical trend in the same direction was observed for the walking activities (Table 2).
Quality of Life
OB had lower quality of life according to all aspects of the SF-36 questionnaire (physical and mental domains) when compared to PO and MC, whereas there were no differences between PO and MC (Table 3).
Correlations
As shown in Table 4, better PF was moderately-to-strongly correlated with lower percentage of fat mass, physical functioning (SF-36), and lower EE during ADL in all groups.
Discussion
This study proposed to evaluate the physical functionality in performing ADL in late outcome individuals submitted to RYGB and to compare them to class III obesity patients and control subjects matched for age, gender, and BMI. As expected, 3 to 4 years after BS, individuals had an important decrease in BMI and in the prevalence of comorbidities, reaching similar parameters as the MC subjects. When we analyzed the PF by the Glittre ADL-test, we found that PO and MC groups had similar performances between them, but better than OB individuals. Only a few studies evaluated PF in obese and post-BS patients by an objective method. Some studies have shown that PF, assessed by the 6MWT, significantly improved from 8.8 to 33.3% after BS [23–30]; however, this is a test which assesses only one daily activity (i.e., walking). Three studies evaluated PF (follow-up from 3 to 12 months) by the timed up-and-go test [8, 27, 29], and two other studies evaluated PF by using the Short Physical Performance Battery, which consists of repeated chair stands, balance, and 8 min of walking [26, 30]. All these studies found an increase in PF after BS; however, the maximum time of follow-up in these studies was 12 months not considering that the peak of weight loss after RYGB occurs at 12–16 months and continues up to 18–24 months [31]. We also should highlight that none of these studies included a matched control group, which is important to determine whether post-BS patients reach similar to their controls.
Regarding EE, it is well known that obese patients have a higher EE than individuals with normal body weight [32]. The amount of fat-free mass seems to be the main predictor of a suitable total and resting EE [33]. Das et al. [32] also demonstrated that fat-free mass is able to predict 56% of total EE and 63% of resting EE. Bariatric surgery commonly may lead to important reduction not only of fat but also of fat-free mass [34]. Therefore, some previous studies reported an important EE decrease after this surgical procedure [35]. In the present study, we also found high EE in OB when compared to PO and MC during the Glittre ADL-test. Undoubtedly, this was due to a higher level of work to move their body weight and longer time spent to perform the activities. Nonetheless, in the modified Glittre ADL-test, they showed significantly lower averages for EE. The explanation for this is likely that OB, due to their musculoskeletal limitations, performed the ADL activities at a lower speed and at fewer repetitions than PO and MC. On the other hand, post-BS patients have a similar EE to matched controls. To the authors’ best knowledge, the present study is the first to show that post-BS patients (3 to 4 years post-operatively) have similar EE behavior during ADL in comparison with matched controls, despite lean body mass and energy expenditure reduction.
Several studies have shown that weight loss and reduction of comorbidities after BS were able to improve the quality of life of these patients [3, 36]. In agreement with these findings, the present study showed that PO had statistically better results in all domains of the SF-36 (both physical and mental) when compared to OB. Furthermore, as previously described in the literature, the quality of life of PO and MC was similar, again highlighting the beneficial effects of the surgery [37].
One of the limitations of this study is that EE was assessed by the SAB, which is not the gold standard for this purpose. However, several studies [4, 20, 38] have used this activity monitor in obese and post-BS patients because it is a simpler and less costly tool than indirect calorimetry. We also recognize that a longitudinal design would be ideal to evaluate the effects of surgery. However, the inclusion of an obese group referred for BS and a non-obese group matched by BMI, gender, and age may counteract this limitation by providing a frame for pre-surgical assessment and another frame for a post-surgical “reference,” respectively. Finally, we only studied patients successfully treated by the surgery. Therefore, we cannot extrapolate these conclusions for all individuals submitted to BS.
In summary, post-bariatric surgery patients have better physical function and quality of life and perform activities under lower total EE than obese subjects, very similar to matched controls. In these subjects, better physical function is associated with better body composition and lower EE during activities of daily living.
References
National Task force of Prevention of Obesity. Overweight, obesity, and health risk. National task force on the prevention and treatment of obesity. Arch Intern Med. 2000;160:898–904.
Peltonen M, Lindroos AK, Torgerson JS. Musculoskeletal pain in the obese: a comparison with a general population and long-term changes after conventional and surgical obesity treatment. Pain. 2003;104(3):549–57.
Busetto L, Mozzi E, Schettino AM, et al. Three years durability of the improvements in health-related quality of life observed after gastric banding. Surg Obes Relat Dis. 2015;11(1):110–7.
Josbeno DA, Kalarchian M, Sparto PJ, et al. Physical activity and physical function in individuals post-bariatric surgery. Obes Surg. 2011;21(8):1243–9.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Vogel JA, Franklin BA, Zalesin KC, et al. Reduction in predicted coronary heart disease risk after substantial weight reduction after bariatric surgery. Am J Cardiol. 2007;99(2):222–6.
Belazi D, Goldfarb NI, He H. Measuring health-related quality of life in the clinical setting. Expert Rev Pharmacoecon Outcomes Res. 2002;2(2):109–17.
Iossi MF, Konstantakos EK, Teel DD, et al. Musculoskeletal function following bariatric surgery. Obesity (Silver Spring). 2013;21(6):1104–10.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Pitta F, Troosters T, Probst VS, et al. Quantifying physical activity in daily life with questionnaires and motion sensors in COPD. Eur Respir J. 2006;27(5):1040–55.
Santarpia L, Contaldo F, Pasanisi F. Body composition changes after weight-loss interventions for overweight and obesity. Clin Nutr. 2013;32(2):157–61.
Carrasco F, Papapietro K, Csendes A, et al. Changes in resting energy expenditure and body composition after weight loss following Roux-en-Y gastric bypass. Obes Surg. 2007;17(5):608–16.
Faria SL, Kelly E, Faria OP. Energy expenditure and weight regain in patients submitted to Roux-en-Y gastric bypass. Obes Surg. 2009;19(7):856–9.
LeCheminant JD, Heden T, Smith J, et al. Comparison of energy expenditure, economy, and pedometer counts between normal weight and overweight or obese women during a walking and jogging activity. Eur J Appl Physiol. 2009;106(5):675–82.
SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg Obes Relat Dis. 2009;5(3):387–405.
Skumlien S, Hagelund T, Bjortuft O, et al. A field test of functional status as performance of activities of daily living in COPD patients. Respir Med. 2006;100(2):316–23.
Monteiro F, Ponce DA, Silva H, Carrilho AF, Pitta F. Validity and reproducibility of the Glittre ADL-test in obese and post-bariatric surgery patients. Obes Surg. 2016.
Cavalheri V, Donaria L, Ferreira T, et al. Energy expenditure during daily activities as measured by two motion sensors in patients with COPD. Respir Med. 2011;105(6):922–9.
Monteiro F, Camillo CA, Vitorasso R, et al. Obesity and physical activity in the daily life of patients with COPD. Lung. 2012;190(4):403–10.
Bond DS, Unick JL, Jakicic JM, et al. Objective assessment of time spent being sedentary in bariatric surgery candidates. Obes Surg. 2011;21(6):811–4.
Ciconelli RM, Ferraz MB, Santos W, et al. Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida Medical Outcomes Study 36-item Short Form Health Survey SF-36. (Brasil SF-36). Rev Bras Reumatol. 1999;39(3):143–50.
Lukaski HC, Bolonchuk WW, Hall CB, et al. Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol. 1986;60(4):1327–32.
Maniscalco M, Zedda A, Giardiello C, et al. Effect of bariatric surgery on the six-minute walk test in severe uncomplicated obesity. Obes Surg. 2006;16(7):836–41.
Tompkins J, Bosch PR, Chenowith R, et al. Changes in functional walking distance and health-related quality of life after gastric bypass surgery. Phys Ther. 2008;88(8):928–35.
de Souza SA, Faintuch J, Fabris SM, et al. Six-minute walk test: functional capacity of severely obese before and after bariatric surgery. Surg Obes Relat Dis. 2009;5(5):540–3.
Josbeno DA, Jakicic JM, Hergenroeder A, et al. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis. 2010;6(4):361–6.
Vargas CB, Picolli F, Dani C, et al. Functioning of obese individuals in pre- and postoperative periods of bariatric surgery. Obes Surg. 2013;23(10):1590–5.
da Silva RP, Martinez D, Faria CC, et al. Improvement of exercise capacity and peripheral metaboreflex after bariatric surgery. Obes Surg. 2013;23(11):1835–41.
Lyytinen T, Liikavainio T, Paakkonen M, et al. Physical function and properties of quadriceps femoris muscle after bariatric surgery and subsequent weight loss. J Musculoskelet Neuronal Interact. 2013;13(3):329–38.
Miller GD, Nicklas BJ, You T, et al. Physical function improvements after laparoscopic Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2009;5(5):530–7.
Silver HJ, Torquati A, Jensen GL, et al. Weight, dietary and physical activity behaviors two years after gastric bypass. Obes Surg. 2006;16(7):859–64.
Das SK, Saltzman E, McCrory MA, et al. Energy expenditure is very high in extremely obese women. J Nutr. 2004;134(6):1412–6.
Nelson KM, Weinsier RL, Long CL, et al. Prediction of resting energy expenditure from fat-free mass and fat mass. Am J Clin Nutr. 1992;56:848–56.
Wells J, Miller M, Perry B, et al. Preservation of fat-free mass after bariatric surgery: a comparison of malabsorptive and restrictive procedures. Am Surg. 2015;81:812–5.
Ohrstrom M, Hedenbro J, Ekelund M. Energy expenditure during treadmill walking before and after vertical banded gastroplasty: a one-year follow-up study in 11 obese women. Eur J Surg. 2001;167(11):845–50.
Costa RC, Yamaguchi N, Santo MA, et al. Outcomes on quality of life, weight loss, and comorbidities after Roux-en-Y gastric bypass. Arq Gastroenterol. 2014;51(3):165–70.
de Zwaan M, Lancaster KL, Mitchell JE, et al. Health-related quality of life in morbidly obese patients: effect of gastric bypass surgery. Obes Surg. 2002;12(6):773–80.
Unick JL, Bond DS, Jakicic JM, et al. Comparison of two objective monitors for assessing physical activity and sedentary behaviors in bariatric surgery patients. Obes Surg. 2012;22(3):347–52.
Acknowledgements
FP is a researcher supported by CNPq (National Council for Scientific and Technological Development), Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
The study was approved by the institutional ethics committee.
Rights and permissions
About this article
Cite this article
Monteiro, F., Ponce, D.A.N., Silva, H. et al. Physical Function, Quality of Life, and Energy Expenditure During Activities of Daily Living in Obese, Post-Bariatric Surgery, and Healthy Subjects. OBES SURG 27, 2138–2144 (2017). https://doi.org/10.1007/s11695-017-2619-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2619-4