Abstract
Purpose of Review
The purpose of this review is to provide an introduction to quality of life (QOL) outcomes after bariatric surgery and a summary of the current evidence.
Recent Findings
QOL has been emphasized in bariatric surgery since the NIH Consensus Conference statement in 1991. Initial studies were limited to 1- and 2-year follow-up. More recent findings have expanded the follow-up period up to 12 years, providing a better description of the impact on long-term QOL. Overall, there is little to no consensus regarding the definition of QOL or the ideal survey. Bariatric surgery has the greatest impact on physical QOL, and the impact on mental health remains unclear. There are some specific and less frequently reported threats to quality of life after bariatric surgery that are also discussed.
Summary
Obesity has a definite impact on quality of life, even without other comorbidities, and surgery for obesity results in significant and lasting improvements in patient-reported quality of life outcomes. This conclusion is limited by a wide variety of survey instruments and absence of consensus on the definition of QOL after bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, the prevalence of obesity has more than doubled since 1980. Currently, over 600 million adults are obese, and that number will continue to increase. There are more than 41 million children under the age of five who are obese or overweight [1]. Obesity has a significant negative impact on physical, psychological, and social health. While the physical effects of obesity, including metabolic syndrome, hypertension, and diabetes, are well known, the impact of obesity on psychosocial outcomes and quality of life is less well explored [2].
Bariatric surgery has emerged as the most effective and enduring weight loss therapy available, with dramatic weight loss, reduction or resolution of obesity-related comorbidities, and a corresponding decrease in mortality and healthcare costs. These outcomes are objective and quantitative, lending themselves to analysis. Quality of life outcomes are not only more challenging to measure and interpret but also very important when evaluating the impact of bariatric surgery. The NIH Consensus Statement in 1991 called for consideration of quality of life outcomes in all analyses of patients undergoing surgical treatment for obesity [3]. As a result, the Bariatric Analysis and Reporting Outcome System (BAROS) was introduced in 1997; this system identifies three main areas that define success for bariatric surgery: percentage of excess weight loss, changes in medical conditions, and quality of life [4]. Since the late 1990s and early 2000s, after the NIH consensus statement and the development of BAROS, more and more studies have included or exclusively focused on quality of life for patients undergoing bariatric surgery.
This paper seeks to provide an overview of the methods for reporting and analyzing quality of life measures and the recent evidence for the impact of bariatric surgery on quality of life and discuss some implications for clinical practice and research.
Definitions and Measurements of Quality of Life
“Quality of life” (QOL) is a multi-dimensional concept, incorporating physical, psychological, and social aspects [5]. There is no single fully agreed-upon definition for QOL, as evidenced even by the number of interrelated terms that can refer to the same concept, including QOL, health-related quality of life (HRQL), health status, functional assessment, or patient-reported outcomes (PRO) [6, 7]. There are also numerous survey instruments used to measure QOL and its associated concepts. These fall into three broad groups: generic surveys intended for general use, regardless of disease or condition; disease-specific surveys; and aspect-specific surveys, meant to capture a specific domain of interest, such as depression, anxiety, or self-esteem. Table 1 provides examples of these three classes of surveys from the bariatric surgery literature.
The choice of survey instrument matters. First, given the numerous domains that can be encompassed within QOL, including physical, psychological, social, and environmental [21], short-form surveys like the SF-36 or one-page surveys like the Moorehead-Ardelt Quality of Life Questionnaire [4] do not cover all domains equally. Additionally, some authors draw a distinction between health status, which can be measured by external parameters, and quality of life, which is a subjective assessment that can be determined only by the patient [5]. With this distinction, not every patient-reported outcome is truly a measure of quality of life. Two patients with identical health status may have very different subjective assessment of their own QOL. As with all other survey-based metrics, the results reflect the biases of the survey instrument, in this case, the providers’ assumptions of what is important to patients [5].
Many QOL and health status surveys provide population norms, and many of the studies reviewed in this paper compare obese patients to healthy controls, or to specific other disease populations [22]. The validity of these comparisons is unclear. Reference normal populations are usually obtained through voluntary responses to mailed questionnaires and tend to overrepresent well-educated, upper-class women [23, 24]. Direct comparison of patients’ own quality of life is a much more robust metric than comparison of the obese population seeking bariatric surgery with an existing population norm.
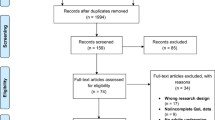
In the sections below, we review several studies that look at quality of life and its affiliated concepts after bariatric surgery. While trends become apparent, it is worth noting that many of these studies do not define QOL or use QOL interchangeably with health status. They also utilize a huge variety of survey metrics, potentially limiting between-study comparisons. One systematic review of patient-reported outcomes in bariatric surgery evaluated 86 studies and found 68 different validated measures to report QOL [7]. The most common measure used was the generic SF-36 Health Questionnaire, and the most common disease-specific measure was the Impact of Weight on Quality of Life-lite (IWQoL-lite) (Table 1).
Changes in Quality of Life After Bariatric Surgery
While a few studies are dedicated specifically to patient-reported outcomes, quality of life, and psychosocial factors [14, 25, 26], the majority report on quality of life as a secondary outcome in studies primarily designed to look at weight loss or resolution of comorbidities [11, 12]. As noted earlier, the available studies utilize a wide range of surveys, resulting in a very diverse collection of outcomes under the heading of “quality of life.”
Impact of Bariatric Surgery on Health-Related Quality of Life
The most commonly used generic measure of quality of life after bariatric, the SF-36, is a measurement of HRQL, or perceived health status, asking respondents to reflect specifically on how their physical or mental health is impacting their life [5]. There are numerous studies that have utilized this instrument. Kolotkin et al. compared 323 patients after gastric bypass with 257 individuals who sought but did not undergo bariatric surgery. At 2 and 6 years of follow-up, the surgery cohort had significantly higher scores on both the SF-36 and the disease-specific IWQOL-Lite [27, 28]. The peak of quality of life improvements was seen at the 2-year time point, and although differences persisted at 6 years, there was some weight regain and an accompanying decline in HRQL [27]. In a comparison of surgery and optimal medical management with type II diabetes, both the adjustable gastric band [29] (AGB) and Roux-en-Y gastric bypass (RNYGB) [30] result in significantly greater weight loss and better glycemic control. Quality of life was again measured with both the generic SF-36 and the disease-specific IWQOL. In this study, when the control group received optimal medical therapy, there was no significant difference in SF-36 scores. The disease-specific metric, however, showed significant improvements in quality of life after the bypass [30].
Adams et al. compared patients undergoing RNYGB with weight-matched controls who received no treatment [31]. All main outcome measures, including weight loss and comorbidities, were improved in the surgical cohort. When looking at quality of life outcomes on the SF-36, patients reported significant improvement in the physical components of the questionnaire, but no improvement on the mental health sections. In a 12-year study of RNYGB, Raoof et al. had similar results, with patients showing significant improvement specifically in the physical components of the SF-36 [32]. In a study comparing preoperative patients, patients 1–2 years from RNYGB, and patients at least 7 years from RNYGB, Neto et al. found that while general health perception and vitality were durably improved postoperatively, there was no difference between the groups in mental health or social functioning [33].
Impact of Bariatric Surgery on Overall Quality of Life
Many of the largest and longest-running studies of bariatric surgery outcomes report on quality of life as a secondary, rather than primary, outcome. The available details on the methodology and results are therefore somewhat limited. Himpens et al., for example, report on 9-year outcomes for 126 patients after the RNYGB [12] and 53 patients after laparoscopic sleeve gastrectomy (LSG) [11]. In both studies, the authors report BAROS scores, which utilize the Moorehead-Ardelt Quality of Life Questionnaire II. In both studies, the authors report long-term positive quality of life outcomes, although the results are limited to a percentage of patients who indicate they are “happy or very happy with the procedure” and would opt to have the operation again.
Impact of Bariatric Surgery on Outcome-Specific Quality of Life
Most outcome-specific quality of life studies focus on depression and anxiety symptoms or eating habits. There are overall mixed results. Buddeberg-Fischer et al. followed 131 patients who applied for bariatric surgery, comparing the surgical cohort (57 patients undergoing gastric band and 12 undergoing RNYGB) with the untreated control group [34]. After four and a half years, the surgical group lost significantly more weight, but did not have significantly higher quality of life, or lower incidences of depression, anxiety, or binge eating. In the long-term follow-up for the Swedish Obese Subjects (SOS) study, patients treated with a variety of bariatric procedures were compared with medically treated patients over 10 years [35]. Depression symptoms were significantly decreased at 10 years post-surgery, but there was no change in overall mood or in anxiety symptoms.
Relationship of Type of Procedure to Quality of Life Outcomes
Numerous studies attempt to compare outcomes between different bariatric procedures. Overall, the LSG, AGB, and RNYGB have all demonstrated significant improvements in quality of life in studies with at least 1-year follow-up [9, 12, 14, 15, 36, 37]. Direct comparisons of quality of life outcomes between two or more procedures are rare. Peterli et al. randomized 217 patients to either sleeve gastrectomy or gastric bypass and found significant and comparable improvements in quality of life at 1 year after either procedure [15]. Other studies have shown significantly greater improvements in quality of life with the bypass in comparison with the gastric band after 1 year [38], 3 years [39], or sleeve gastrectomy after 4 years [40]. Similar results are seen in adolescents, where patients after gastric bypass have a significantly greater improvement in quality of life after 3 years than those undergoing the LSG or AGB [16].
Predictors of Quality of Life Outcomes Postoperatively
A number of potential predictor variables for postoperative quality of life have been explored, including the degree of excess weight loss. The correlation between degree of weight loss and postoperative QOL is not consistent amongst studies. In one study of 459 patients undergoing AGB procedure, percentage of excess weight loss was unrelated to degree of QOL improvement at 4-year follow-up [37]. In another study of 50 patients undergoing AGB, however, degree of QOL improvement was strongly correlated with the degree of excess weight loss at 1 and 5 years as measured by the generic Health-Related Quality of Life Questionnaire [24, 9]. Similarly, studies of patients undergoing gastric bypass show a correlation between degree of weight and improved QOL [25] and show that loss of <50% of excess body weight is a predictor of overall poorer QOL [32, 10, 41]. Strain et al. followed 105 patients undergoing gastric bypass, duodenal switch, or sleeve gastrectomy and found no correlation between degree of weight loss and QOL outcomes measured with SF-36 or depression symptoms measured with the Beck Depression Inventory [17]. In one study, patients who were undergoing gastric bypass as a revision from a prior operation had poorer postoperative quality of life [32] although in a prospective database of patients undergoing LAGB or VBG, the need for reoperation was not a predictor of poorer quality of life [42].
Preoperative depression symptoms have also been identified as a predictor of lower QOL changes after bariatric surgery [10, 43]. Overall, however, the majority of studies looking at psychosocial predictors of outcomes after bariatric surgery focus on weight regain. There are few studies specifically examining predictors of poor quality of life response after surgery.
Specific Threats to Quality of Life After Bariatric Surgery
Overwhelmingly, the available literature demonstrates considerable improvements in multiple quality of life domains after bariatric surgery [44]. There are, however, threats to quality of life after bariatric surgery that warrant specific mention. These are likely rare events, although it is also possible that these outcomes are more common than described in large-scale studies, since they may contribute to the loss of follow-up that is an acknowledged challenge for postoperative bariatric surgery outcomes. Below, we discuss several specific negative QOL outcomes that can occur after bariatric surgery and may warrant specific attention in preoperative planning and postoperative care.
Social Stigma Against Bariatric Surgery
The social stigma against obesity also extends to surgical treatments for obesity [22]. Especially when postoperative complications lead to new health problems, patients may feel that these issues must be kept private. Patients have reported feeling well supported when things are going well and they are losing weight, but a lack of support for postoperative complications, including nutrient deficiencies or chronic pain [45]. Sarwer et al. found that weight-related stigmatization was associated with poorer postoperative quality of life and increased depression symptoms [46].
Excess Skin
One infrequently discussed physical complication of bariatric surgery is the development of skin folds as patients lose significant weight. While not frequently mentioned in large-scale outcome studies, up to 95% of patients undergoing a gastric bypass express dissatisfaction with excess skin, and 74% express a desire for plastic surgery to remove excess skin [47]. Excess skin after massive weight loss can have physical consequences, including dermatitis, ulcers, and chronic pruritis [48]. It can also lead to psychological and quality of life consequences, including social limitations, physical activity, sexual activity, and self-esteem [49]. Furthermore, most patients seek plastic surgery for excess skin specifically to improve quality of life [50] and patients who do undergo body contouring procedures have significantly higher health-related quality of life than patients who undergo gastric bypass without plastic surgery [51].
Depression and Anxiety
The impact of bariatric surgery on depression and anxiety is unclear. There are many studies that demonstrate a decrease in depressive and anxiety symptoms after surgery [26, 18]. There are small studies that have shown an increase in major depression after bariatric surgery, however [52]. Depression either pre- or postoperatively is associated with decreased weight loss and poorer postoperative quality of life [10, 43], emphasizing the importance of understanding the impact of bariatric surgery on depression symptoms.
Alcohol Use Disorder
Alcohol use disorders have been shown to increase after bariatric surgery, particularly when patients are followed beyond the first postoperative year [52, 53]. This may be due to impaired alcohol metabolism after Roux-en-Y gastric bypass; postoperative patients report feelings of mental intoxication with much lower levels of alcohol, and a different constellation of physical symptoms, including lower levels of diaphoresis, flushing, and hyperactivity [54]. This changed metabolism may explain why an increase in alcohol and other addictive disorders is associated with Roux-en-Y gastric bypass, but not with laparoscopic gastric banding or sleeve gastrectomy [55].
Conclusions
Success after bariatric surgery is measured by a number of different factors. The amount of weight loss, the retention of weight loss, and the resolution of obesity-related comorbidities are essential. Improvement in quality of life and psychosocial outcomes is also an important factor though more difficult to measure. Obesity has a definite impact on quality of life, even without other comorbidities [2, 56], and surgery for obesity results in significant and lasting improvements in patient-reported quality of life outcomes. The quality of life improvements after surgery are particularly dramatic in the realm of physical functioning, which is not surprising given the impact of the surgery on comorbidities. Data on the impact on mental and social metrics of quality of life are more mixed. All of these may be useful to assess cost-effectiveness studies which may incorporate Quality-Adjusted Life Years based upon Quality of Life assessment.
Bariatric surgery’s impact on quality of life has been demonstrated in numerous large multi-center trials, but there are two important limitations to the literature that have relevance to clinical practice. First, the existing literature relies heavily on 1-year outcomes. Although some studies have begun to present longer-term outcomes for quality of life [35], these are still in the minority. The vertical banded gastroplasty, which demonstrated excellent short-term weight loss and quality of life outcomes, was shown in 5- and 10-year follow-up to have extremely high rates of weight regain, with associated regression in quality of life outcomes [57, 58]. The story of the vertical banded gastroplasty is a reminder of the need for long-term quality of life outcomes, to ensure that the gains seen in shorter-term studies are enduring. In contrast, the RYGB has demonstrated long-term maintenance of weight loss and QOL studies have demonstrated maintained QOL at 7 to 12 years postop [12]. Second, studies evaluating quality of life after bariatric surgery use a huge variety of survey instruments. The SF-36 is the most common general quality of life instrument, while the Moorehead-Ardelt Quality of Life Questionnaire II is the BAROS-preferred instrument. Dozens of other general, disease- and aspect-specific surveys are used. The variety of instruments limits the ability to compare outcomes across studies, especially when results are not clear-cut. Physical aspects of HRQL are the most dramatically improved after bariatric surgery, while mental health questions on general surveys and outcome-specific questionnaires for anxiety and depression show mixed results.
Finally, there are uncommon but important threats to quality of life after bariatric surgery. These include a perceived lack of support due to a social stigma against the surgery, the consequences of excess skin and the potential need for plastic surgery, depression and anxiety symptoms, and alcohol use disorders. Although these outcomes are a minority of patients, it is essential for a bariatric surgery program to recognize and have plans in place in order to limit their impact on patients’ postoperative quality of life.
Overall, bariatric surgery remains the most effective, durable, and efficient treatment for obesity, and the physical gains are mirrored by significant improvements in quality of life.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Organization WH. Fact sheet: obesity and overweight 2016.
Fontaine KR, Bartlett SJ, Barofsky I. Health-related quality of life among obese persons seeking and not currently seeking treatment. Int J Eat Disord. 2000;27(1):101–5.
Statement NC. Gastrointestinal surgery for severe obesity. 1991;9(1):1–20.
Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (BAROS). Obes Surg. 1998;8(5):487–99.
Hamming JF, De Vries J. Measuring quality of life. Br J Surg. 2007;94(8):923–4.
Fletcher A. Quality-of-life measurements in the evaluation of treatment: proposed guidelines. Br J Clin Pharmacol. 1995;39(3):217–22.
Coulman KD, Abdelrahman T, Owen-Smith A, Andrews RC, Welbourn R, Blazeby JM. Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev. 2013;14(9):707–20.
Jumbe S, Bartlett C, Jumbe SL, Meyrick J. The effectiveness of bariatric surgery on long term psychosocial quality of life—a systematic review. Obes Res Clin Pract. 2016;10(3):225–42.
Mathus-Vliegen EM, de Wit LT. Health-related quality of life after gastric banding. Br J Surg. 2007;94(4):457–65.
Sanchez-Santos R, Del Barrio MJ, Gonzalez C, Madico C, Terrado I, Gordillo ML, et al. Long-term health-related quality of life following gastric bypass: influence of depression. Obes Surg. 2006;16(5):580–5.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
Himpens J, Verbrugghe A, Cadiere GB, Everaerts W, Greve JW. Long-term results of laparoscopic Roux-en-Y gastric bypass: evaluation after 9 years. Obes Surg. 2012;22(10):1586–93.
Myers JA, Clifford JC, Sarker S, Primeau M, Doninger GL, Shayani V. Quality of life after laparoscopic adjustable gastric banding using the Baros and Moorehead-Ardelt Quality of Life Questionnaire II. JSLS. 2006;10(4):414–20.
Amichaud R, Donatini G, Barussaud ML, Charalambous C, Ingrand I, Faure JP. Health-related quality of life after laparoscopic sleeve gastrectomy. A multicentric experience. Minerva Chir. 2016;71(4):245–51.
• Peterli R, Borbely Y, Kern B, Gass M, Peters T, Thurnheer M, et al. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2013;258(5):690–4. discussion 5. This prospective trial demonstrated the weight loss and quality of life differences between the 2 major surgeriesfor weight loss.
Inge TH, Courcoulas AP, Jenkins TM, Michalsky MP, Helmrath MA, Brandt ML, et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374(2):113–23.
Strain GW, Kolotkin RL, Dakin GF, Gagner M, Inabnet WB, Christos P, et al. The effects of weight loss after bariatric surgery on health-related quality of life and depression. Nutr Diabetes. 2014;4:e132.
Burgmer R, Legenbauer T, Muller A, de Zwaan M, Fischer C, Herpertz S. Psychological outcome 4 years after restrictive bariatric surgery. Obes Surg. 2014;24(10):1670–8.
Sarwer DB, Wadden TA, Moore RH, Eisenberg MH, Raper SE, Williams NN. Changes in quality of life and body image after gastric bypass surgery. Surg Obes Relat Dis. 2010;6(6):608–14.
Steffen KJ, Sarwer DB, Thompson JK, Mueller A, Baker AW, Mitchell JE. Predictors of satisfaction with excess skin and desire for body contouring after bariatric surgery. Surg Obes Relat Dis. 2012;8(1):92–7.
The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46(12):1569–85.
Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the importance of obesity-related social stigma and functional status. J Gen Intern Med. 2013;28(2):231–8.
Michelson H, Bolund C, Nilsson B, Brandberg Y. Health-related quality of life measured by the EORTC QLQ-C30—reference values from a large sample of Swedish population. Acta Oncol. 2000;39(4):477–84.
Mathus-Vliegen EM, de Weerd S, de Wit LT. Health-related quality-of-life in patients with morbid obesity after gastric banding for surgically induced weight loss. Surgery. 2004;135(5):489–97.
Batsis JA, Lopez-Jimenez F, Collazo-Clavell ML, Clark MM, Somers VK, Sarr MG. Quality of life after bariatric surgery: a population-based cohort study. Am J Med. 2009;122(11):1055 e1–e10.
Bocchieri LE, Meana M, Fisher BL. A review of psychosocial outcomes of surgery for morbid obesity. J Psychosom Res. 2002;52(3):155–65.
• Kolotkin RL, Davidson LE, Crosby RD, Hunt SC, Adams TD. Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis. 2012;8(5):625–33. This study shows the longest term quality of life improvement for bariatric surgery patients compared to obese controls.
Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Adams TD. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. 2009;5(2):250–6.
Ding SA, Simonson DC, Wewalka M, Halperin F, Foster K, Goebel-Fabbri A, et al. Adjustable gastric band surgery or medical management in patients with type 2 diabetes: a randomized clinical trial. J Clin Endocrinol Metab. 2015;100(7):2546–56.
Halperin F, Ding SA, Simonson DC, Panosian J, Goebel-Fabbri A, Wewalka M, et al. Roux-en-Y gastric bypass surgery or lifestyle with intensive medical management in patients with type 2 diabetes: feasibility and 1-year results of a randomized clinical trial. JAMA Surg. 2014;149(7):716–26.
Adams TD, Davidson LE, Litwin SE, Kolotkin RL, LaMonte MJ, Pendleton RC, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308(11):1122–31.
Raoof M, Naslund I, Rask E, Karlsson J, Sundbom M, Edholm D, et al. Health-related quality-of-life (HRQoL) on an average of 12 years after gastric bypass surgery. Obes Surg. 2015;25(7):1119–27.
Laurino Neto RM, Herbella FA. Changes in quality of life after short and long term follow-up of Roux-en-Y gastric bypass for morbid obesity. Arq Gastroenterol. 2013;50(3):186–90.
Buddeberg-Fischer B, Klaghofer R, Krug L, Buddeberg C, Muller MK, Schoeb O, et al. Physical and psychosocial outcome in morbidly obese patients with and without bariatric surgery: a 4 1/2-year follow-up. Obes Surg. 2006;16(3):321–30.
Karlsson J, Taft C, Ryden A, Sjostrom L, Sullivan M. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes. 2007;31(8):1248–61.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Dixon JB, Dixon ME, O'Brien PE. Quality of life after lap-band placement: influence of time, weight loss, and comorbidities. Obes Res. 2001;9(11):713–21.
Campos GM, Rabl C, Roll GR, Peeva S, Prado K, Smith J, et al. Better weight loss, resolution of diabetes, and quality of life for laparoscopic gastric bypass vs banding: results of a 2-cohort pair-matched study. Arch Surg. 2011;146(2):149–55.
Hell E, Miller KA, Moorehead MK, Norman S. Evaluation of health status and quality of life after bariatric surgery: comparison of standard Roux-en-Y gastric bypass, vertical banded gastroplasty and laparoscopic adjustable silicone gastric banding. Obes Surg. 2000;10(3):214–9.
Romy S, Donadini A, Giusti V, Suter M. Roux-en-Y gastric bypass vs gastric banding for morbid obesity: a case-matched study of 442 patients. Arch Surg. 2012;147(5):460–6.
Rea JD, Yarbrough DE, Leeth RR, Leath TD, Clements RH. Influence of complications and extent of weight loss on quality of life after laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21(7):1095–100.
Schouten R, Wiryasaputra DC, van Dielen FM, van Gemert WG, Greve JW. Influence of reoperations on long-term quality of life after restrictive procedures: a prospective study. Obes Surg. 2011;21(7):871–9.
de Zwaan M, Enderle J, Wagner S, Muhlhans B, Ditzen B, Gefeller O, et al. Anxiety and depression in bariatric surgery patients: a prospective, follow-up study using structured clinical interviews. J Affect Disord. 2011;133(1–2):61–8.
Magallares A, Schomerus G. Mental and physical health-related quality of life in obese patients before and after bariatric surgery: a meta-analysis. Psychol Health Med. 2015;20(2):165–76.
Groven KS, Raheim M, Engelsrud G. “My quality of life is worse compared to my earlier life”: living with chronic problems after weight loss surgery. Int J Qual Stud Health Well-being. 2010;5(4):5553.
Sarwer DB, Fabricatore AN, Eisenberg MH, Sywulak LA, Wadden TA. Self-reported stigmatization among candidates for bariatric surgery. Obesity (Silver Spring). 2008;16(Suppl 2):S75–9.
Kitzinger HB, Abayev S, Pittermann A, Karle B, Kubiena H, Bohdjalian A, et al. The prevalence of body contouring surgery after gastric bypass surgery. Obes Surg. 2012;22(1):8–12.
Kitzinger HB, Abayev S, Pittermann A, Karle B, Bohdjalian A, Langer FB, et al. After massive weight loss: patients’ expectations of body contouring surgery. Obes Surg. 2012;22(4):544–8.
Hurwitz DJ, Ayeni O. Body contouring surgery in the massive weight loss patient. Surg Clin North Am. 2016;96(4):875–85.
Ellison JM, Steffen KJ, Sarwer DB. Body contouring after bariatric surgery. Eur Eat Disord Rev. 2015;23(6):479–87.
Modarressi A, Balague N, Huber O, Chilcott M, Pittet-Cuenod B. Plastic surgery after gastric bypass improves long-term quality of life. Obes Surg. 2013;23(1):24–30.
Mitchell JE, Lancaster KL, Burgard MA, Howell LM, Krahn DD, Crosby RD, et al. Long-term follow-up of patients’ status after gastric bypass. Obes Surg. 2001;11(4):464–8.
King WCCJ, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, Courcoulas AP, Pores WJ, Yanovski SZ. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307(23):2516–25.
Woodard GA, Downey J, Hernandez-Boussard T, Morton JM. Impaired alcohol metabolism after gastric bypass surgery: a case-crossover trial. J Am Coll Surg. 2011;212(2):209–14.
Steffen KJ, Engel SG, Wonderlich JA, Pollert GA, Sondag C. Alcohol and other addictive disorders following bariatric surgery: prevalence, risk factors and possible etiologies. Eur Eat Disord Rev. 2015;23(6):442–50.
Jia H, Lubetkin EI. The impact of obesity on health-related quality-of-life in the general adult US population. J Public Health (Oxf). 2005;27(2):156–64.
Balsiger BM, Poggio JL, Mai J, Kelly KA, Sarr MG. Ten and more years after vertical banded gastroplasty as primary operation for morbid obesity. J Gastrointest Surg. 2000;4(6):598–605.
Wang W, Yu PJ, Lee YC, Wei PL, Lee WJ. Laparoscopic vertical banded gastroplasty: 5-year results. Obes Surg. 2005;15(9):1299–303.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Laura M. Mazer, Dan E. Azagury, and John M. Morton declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Obesity Treatment
Rights and permissions
About this article
Cite this article
Mazer, L.M., Azagury, D.E. & Morton, J.M. Quality of Life After Bariatric Surgery. Curr Obes Rep 6, 204–210 (2017). https://doi.org/10.1007/s13679-017-0266-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-017-0266-7