Abstract
Background
Roux-en-Y gastric bypass (RYGB) has recently been authorized for use in older patients. The objective of this single-center study was to evaluate 2-year weight loss in patients ≥60 years compared with younger matched patients undergoing RYGB. Secondary aims were to record complications and the resolution of comorbidities in a 2-year follow-up.
Methods
Of 722 patients with at least 2 years follow-up data, 48 elderly patients were matched with 92 young (<40 years) and 96 middle-aged (40–59 year) patients, according to sex, baseline body mass index, and date of surgery. Weight loss, remission of comorbidities, death, and early (30-day) and 2-year complication rates were compared.
Results
There were three deaths in the elderly group and none in the other groups. The early complication rate was not significantly different in the elderly group (17.8 %) compared with the young (11.5 %, p = 0.637) and middle-aged (13.7 %, p = 1.000) groups. The 2-year complication rates were not significantly different in the elderly group (9.3 %) compared with the young (23.5 %, p = 0.107) and middle-aged (13.2 %, p = 1.000) groups. The 2-year weight loss was lower in the elderly group (31.8 ± 7.2 %; p < 0.001) than in the young group (38.3 ± 6.9 %) but was not significantly different from that in the middle-aged group (34.4 ± 8.0 %; p = 0.145). Remission rates for diabetes and obstructive sleep apnea were lower in the elderly than in the two younger groups.
Conclusion
After bariatric surgery, major weight loss was observed in patients older than 60, but remission of metabolic comorbidities was less marked than in younger subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefit/risk ratio of bariatric surgery in the elderly still needs to be evaluated, despite mounting evidence that it is probably as safe a procedure as in younger subjects [1–13]. Performing bariatric surgery in a person older than 60 can lead to short-term improvements in weight and obesity-related comorbidities, but may also result in immediate complications and increase frailty with regard to chronic diseases that are more prevalent as age increases. Despite older patients showing a higher perioperative risk profile, related to a higher number of obesity-associated comorbidities than in younger patients, the death rate and early complication rate are not increased [10]. This situation has evolved since initial alarming reports [14, 15]. However, there is a need for more studies because most of those reported are short-term, non-case-controlled, and suffer methodological biases. The need for long-term evaluation was recently recommended [16].
In addition to immediate safety issues, the prevention of disabilities and the remission or improvement in obesity-associated comorbidities need to be evaluated. Even if the remission rates are the same across age groups, there would be a massive leverage effect of bariatric surgery in the elderly because of the large number of patients suffering the associated comorbidities. Obesity is also considered a risk factor for future disability [17] and a faster loss of autonomy. Therefore, data with results beyond 1 year after surgery are required in this age group, for which there are only a few reports [10, 12].
The primary aim of this observational study was to evaluate weight loss at 2 years in elderly patients (≥60 years old) compared with younger matched patients aged less than 40 and 40–59 years. The secondary aims were to evaluate early and 2-year complications and resolution of comorbidities at 2 years.
Methods
Patient Selection
This was a retrospective study of the database of a surgery referral center, which included all patients undergoing bariatric surgery since March 2003 (N = 1346). Data such as age, sex, date of surgery, body weight, body mass index (BMI), change in weight, comorbidities, changes in comorbidities, and complications were recorded prospectively. For the present study, only patients with at least 2 years follow-up data (in July 2014) were considered for inclusion in the study, as well as any patients who died during the period (N = 722).
Study Groups
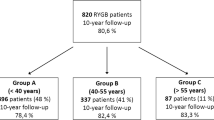
The database search identified patients ≥60 years old at the time of surgery. These “elderly” index cases were matched with two younger groups of patients selected from the database: a “young adult” group of patients aged 18–39 years at the time of surgery; and a “middle-aged” group of patients aged 40–59 years at the time of surgery. The ratio of “non-elderly” to “elderly” patients was 2:1. Patients were matched according to sex, initial BMI, and date of surgery (Fig. 1). Three patients were excluded after the matching process because of death occurring before the end of year 2 (see Results section and Discussion). Five patients were lost to follow-up at 2 years and one patient had missing data on weight at 2 years and was excluded from the analysis. This represents a 96 % follow-up rate of the eligible patients.
All patients were included in a standardized bariatric protocol consisting of preoperative surgical and dietary consultations and complete psychological and endocrine profile evaluations [18]. All patients underwent a complete blood analysis and a preoperative endoscopy to check for Helicobacter pylori, with preoperative eradication when indicated. Additional specialist consultations and tests were asked for if necessary. Informed consent was obtained from all individual participants included in the study. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Surgery
The Roux-en-Y gastric bypass (RYGB) was performed as previously described [19], with the same laparoscopic technique performed throughout by two surgeons. A similar proportion in each patient group was operated on by each surgeon (data not shown).
Body Weight (BW) Changes
The primary outcome of the study was BW loss at 2 years, expressed as the difference relative to BW pre-surgery, as a percentage of the initial value. BW changes were also expressed as excess weight loss (EWL%; i.e., the ratio of the lost weight at a given time to the excess weight before surgery, that being calculated with a reference BMI of 25 kg/m2 [20]. BW was also recorded at 1 year, and change in BW was determined between 1 and 2 years.
Comorbidities
In the present study, only diabetes, hypertension, and obstructive sleep apnea (OSA) were considered. The remission of the comorbidities at 2 years were defined as follows: for diabetes, glycosylated hemoglobin (HbA1c) lower than 6 %, and plasma glucose lower than 100 mg/dL, without any medication [21]; for hypertension, blood pressure lower than 140/90 mmHg without any medication; for OSA, cessation of use of the nighttime positive pressure device. Only complete remissions were considered: there were no attempts to quantify reductions after treatment or improvement in metabolic control or blood pressure.
Complications of Surgery
The complications before day 30 after surgery, and from 2 months to 2 years were recorded prospectively in the database using the Clavien classification [22].
Statistical Analysis
Statistical analysis was performed using STATA statistical software, release 11.2 (STATA Corp., College Station, TX, USA). We describe patient characteristics using number and frequency for qualitative data and mean (± standard deviation) or median (interquartile range) when the normality assumption was not met for quantitative data. Qualitative variables were compared between groups (elderly versus young adult and elderly versus middle-aged) using the χ 2 test (or Fisher’s exact test for small expected numbers). The Student t test was used to compare the distribution of quantitative data (or Mann–Whitney U test when distribution departed from normality or when homoscedasticity was rejected). The Bonferroni correction was used to counteract the problem of multiple comparisons (elderly versus young adult and elderly versus middle-aged). Linear regression was used to compare BW changes at 2 years between groups after adjustment for pre-surgery comorbidities (diabetes, hypertension, and OSA) whose frequencies were imbalanced between groups. All reported p values were two-sided and the significance threshold was <0.05.
Results
The baseline characteristics of the patients are shown in Table 1. Median age was 32.8, 48.5, and 61.9 years in the young, middle-aged, and elderly groups, respectively. Patients in the elderly group ranged from 60.0 to 70.8 years of age. As expected, the characteristics of the three groups did not differ significantly and were well matched regarding date of surgery, sex, initial BW, BMI, and excess weight. They differed in their comorbidity rates (see below). The flow chart of the study is presented in Fig. 1. Six patients had missing data at 2 years and three died before 2 years.
Complications
There were three deaths in the elderly group (Clavien grade 4). One occurred on day 4 post-surgery of pulmonary embolism, one at month 11 of misdiagnosed occlusion while the patient was far from the surgical center, and one of cirrhosis (without further information) close to 2 years. There were no deaths in the other groups.
Early complications (before day 30) occurred in 14 % of patients (1, 6, and 7 with Clavien grade 1, 2, and 3, respectively), half of which required surgery. The early complication rates were not significantly different in the elderly group (17.8 %) compared with the young group (11.5 %, p = 0.637) or middle-aged group (13.7 %, p = 1.000). Table 2 shows a breakdown of the Clavien grades of complications, and there were no significant differences between groups. Between 2 months and 2 years, 16.3 % of elderly patients developed complications, 13.7 % requiring surgery. The complications were not significantly different from those in the young group (23.5 %, p = 0.107) or in the middle-aged group (13.2 %, p = 1.000).
Primary Outcome: BW Loss at 2 Years
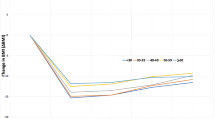
Figure 2 shows the weight trajectories in the three groups. At 2 years, percentage weight loss was significantly greater in young adults (38.3 ± 6.9 %) than in the elderly (31.8 ± 7.2 %; p < 0.001), while weight loss in the middle-aged did not differ from that in the elderly (34.4 ± 8.0 %; p = 0.145). After adjustment for the initial imbalance in the prevalence of diabetes, hypertension, and OSA between groups, weight loss at 2 years remained higher in the young group (p = 0.002) compared with the elderly group and was similar in the middle-aged group compared with the elderly group (p = 0.214). Table 3 presents the results as %EWL, with similar results. In general, there was no regain in weight between 1 and 2 years, and further weight loss was more significant in the young group (−2.7 ± 6.4 kg) than in the elderly group (−0.1 ± 5.2 kg; p = 0.018). In the middle-aged, the mean weight loss between 1 and 2 years was not significantly different from that observed in the elderly (−0.4 ± 5.4 kg, p = 1.000).
Remission of Comorbidities
Table 4 shows the prevalence of diabetes, hypertension, and OSA before surgery and at 2 years. Before surgery, the prevalences of diabetes, hypertension, and OSA were higher in the elderly group than in the young group (all p < 0.001). The prevalences of diabetes and of OSA were higher in the elderly group than in the middle-aged group (p = 0.028 and 0.020, respectively) while that of hypertension was similar in the elderly and middle-aged groups. At 2 years, the remission rates (number of patients in remission at 2 years after surgery divided by the number of patients that had the comorbidity before surgery) were significantly different between groups (all p < 0.001; Table 4). The χ 2 test showed that remissions rates were higher in the young group than in the two other groups for diabetes, hypertension, and OSA and lower in the elderly than in the middle-aged group for diabetes and OSA.
Discussion
This study indicated that elderly subjects lose a similar amount of weight compared with middle-aged patients, have lower remission rates for diabetes and OSA, and do not show significantly more non-lethal surgical complications. The young group of patients lost more weight and had higher remission rates for diabetes, hypertension, and OSA than the elderly group. Non-lethal complications rates were not significantly different between the young and elderly subjects. There were three deaths in the elderly group and none in the other two groups.
The magnitude of desirable weight loss in elderly subjects is debated. On one hand, fear of a significant loss of lean body mass has led to prudent approaches to food restriction. Non-surgical trials have shown a lower weight loss among elderly than with younger patients [23]. However, recent randomized controlled trials have shown that, when associated with proper endurance and resistance training, weight loss of up to 10 % can induce beneficial effects [24–27]. Data from surgical registries have produced heterogeneous results. In a French registry, as in the present study, weight loss was of the same magnitude in people aged 40–60 years as in those older than 60, but lower than that observed in younger patients [28]. This was valid only for RYGB. This suggests that stratification into three age groups is necessary, because pooling the patients aged <60 could mask differences. Robert et al. [29] used this strategy on a smaller cohort (24 patients in each of three groups) with both Roux en Y and omega loops and found a similar weight loss between age groups. Sugerman et al. showed that younger subjects lost more excess weight at 1 year but a similar amount at 5 years as subjects aged 65 and older [10]. Willkomm et al. showed a similar weight loss between patients aged younger than or older than 60 at 12 and 24 months [12]. These two studies did not identify a younger group within those under 60 years [10, 12]. The other publications on RYGB in patients older than 60 were not case–control studies. Altogether, this suggests that RYGB can induce major weight losses of about 30 % and of a similar magnitude in the elderly as in middle-aged patients (note: the mean age for bariatric surgery in most publications is between 40 and 45 years). None of the trials of non-surgical methods has reported such a magnitude of weight loss.
Elderly obese patients are challenged by a higher rate of obesity-associated comorbidities (for example see Sugerman et al. and Busetto et al. [10, 30]) and a threat to their autonomy [17]. The concept of remission of diabetes, hypertension, or OSA has been raised in the surgical literature [31, 32], but very few non-surgical trials have paid attention to this topic. In the Look-Ahead trial involving 59-year-old patients, and intense lifestyle intervention resulting in an 8.6 % weight loss, the rate of complete remission of diabetes was 1.3 % at 1 year and 0.7 % at 4 years [33]. In the present study, the prevalence of diabetes before surgery was significantly higher in elderly subjects, and the complete remission rate after 2 years was lower in the elderly than in the two younger groups. It is not possible to elaborate on the reasons for this because the treatments and duration of disease were not recorded in the database. It is however likely that insulin-requiring diabetes is more prevalent in the elderly and less prone to remission. The absolute number of patients concerned by the complete remission of type 2 diabetes could be higher in the elderly group (and middle-aged group) as compared with younger adults, but the sample size is too small to demonstrate. However, this study does suggest that RYGB has a powerful leverage effect on one of the most frequent and life-threatening complications of obesity even in elderly subjects, with close to 60 % of the patients in remission from diabetes at 2 years. It is difficult to compare our data with that of other trials because of the variety of criteria used to address remission [10, 29, 34] despite clear recommendations [21], or because of the lack of younger groups for comparison. Robert et al. [29] found similar results in study.
Another point to bear in mind when considering RYGB for subjects aged over 60 years is the issue of the safety of the procedure. Flum et al. [14] and Livingston et al. [15] found an increased risk of complications and deaths in patients >65 years. However, in these studies, many patients had open surgery or a laparoscopic procedure performed when RYGB was first introduced 10–15 years ago and surgeons had little experience of the procedure. In addition, the patients were probably frail (under the Medicaid scheme). Sugerman et al. were the first to report the 5-year outcomes of 52 patients with RYGB and noted an acceptable surgical complication rate [10]. Recent studies have highlighted the safety of bariatric surgery in this age category. Improvements in intra-operative surgical management and optimization of perioperative care have decreased the complication rate. Table 2 shows that, when broken down into Clavien scores, the complication rates were the same in the three age groups in the current study. This is in agreement with results from the literature [8, 9, 11–13, 29, 34]. However, there were three deaths in the present study in a small cohort of patients, and at least two were surgery related. The number of deaths in other studies varied from 0 [13] to a few patients (N = 1 to 6 [20, 29, 34, 35]) to 11 patients at 10 years [10]. In Table 2, the Clavien grade 4 complications (here deaths) were not pooled with the other three grades. The risk of death after surgery increases with age. Among the three deaths, one was clearly surgically related, i.e., pulmonary embolism. This risk increases with age but use of preventive strategies can reduce this risk. The death from cirrhosis could not be specifically linked to the surgery because we did not have adequate clinical information for the patient. The third death was from closed loop obstruction. This could be a risk in any patient taken in charge by a less experienced practitioner, but bariatric surgery is becoming commonplace, and the dissemination of training and experience should decrease the risk over time.
This study suggests that more data are needed to estimate the benefit/risk ratio of RYGB in older patients. There is obviously a major weight loss, leading to a substantial proportion gaining remission from diabetes or OSA. Studies of longer duration are needed to evaluate the benefits of such a weight loss on physical and cognitive autonomy, muscle mass and function, and comorbidity. However, three patients died in the 2 years after surgery.
The strengths of this study are that it was a matched study that enabled comparisons between age groups using prospectively collected data. Because bariatric surgery has only recently been authorized in elderly patients >60 years, the matching strategy involved the date of the operation. Indeed, to avoid different stages in the learning curves of the team, we matched the groups for an operation date within 3 months for 136 subjects (70 in the “young group” and 66 in the “middle-aged” group), then within 6 months for the others. We used accurate definitions for remissions as recommended by Buse et al. [21], and this is not always the case in publications on bariatric surgery in the elderly [10, 29, 34]. This was also a single bariatric surgery center, and the same multidisciplinary preoperative procedures were used for all age groups. Finally, this study determined 2-year outcomes, when most of the studies in this age category evaluated outcomes earlier [8, 11, 13, 29, 34, 35] except that of Willkomm et al. at 2 years and that of Sugerman et al. at 5 years [10, 12]. We provide a composite assessment of weight changes, comorbidity changes, and complications.
This study has some limitations. There was a small cohort of patients reflecting the recent use of RYGB in elderly patients in France. The number of patients is further limited by the choice of a 2-year outcome. We also chose 60 years and older to define elderly patients, as this age is used in the French recommendations for surgery, while the World Health Organization uses 65 years and older to denote the elderly. We also limited the comorbidities to OSA, diabetes, and hypertension. In older people, other comorbidities such as degenerative joint diseases should be studied, as they influence the physical activity capacity. However, this was not captured in the database. Future studies should also address the issue of quality of life.
In conclusion, this study showed that bariatric surgery in patients aged 60 years and older resulted in major weight loss and can lead to remission of diabetes or OSA. Morbidity was high although not significantly different compared with younger age groups. Furthermore, there were three deaths within 2 years. Further long-term studies will be necessary to compare outcomes between obese patients receiving surgery or medical intervention.
References
Dorman RB, Abraham AA, Al-Refaie WB, et al. Bariatric surgery outcomes in the elderly: an ACS NSQIP study. J Gastrointest Surg. 2012;16:35–44.
Dunkle-Blatter SE, St Jean MR, Whitehead C, et al. Outcomes among elderly bariatric patients at a high-volume center. Surg Obes Relat Dis. 2007;3:163–9.
Hallowell PT, Stellato TA, Schuster M, et al. Avoidance of complications in older patients and Medicare recipients undergoing gastric bypass. Arch Surg. 2007;142:506–10.
O’Keefe KL, Kemmeter PR, Kemmeter KD. Bariatric surgery outcomes in patients aged 65 years and older at an American Society for Metabolic and Bariatric Surgery Center of Excellence. Obes Surg. 2010;20:1199–205.
Papasavas PK, Gagne DJ, Kelly J, et al. Laparoscopic Roux-En-Y gastric bypass is a safe and effective operation for the treatment of morbid obesity in patients older than 55 years. Obes Surg. 2004;14:1056–61.
Printen KJ, Mason EE. Gastric bypass for morbid obesity in patients more than fifty years of age. Surg Gynecol Obst. 1977;144:192–4.
Quebbemann B, Engstrom D, Siegfried T, et al. Bariatric surgery in patients older than 65 years is safe and effective. Surg Obes Relat Dis. 2005;1:389–92.
Sosa JL, Pombo H, Pallavicini H, et al. Laparoscopic gastric bypass beyond age 60. Obes Surg. 2004;14:1398–401.
Spaniolas K, Trus TL, Adrales GL, et al. Early morbidity and mortality of laparoscopic sleeve gastrectomy and gastric bypass in the elderly: a NSQIP analysis. Surg Obes Relat Dis. 2014;10(4):584–8.
Sugerman HJ, DeMaria EJ, Kellum JM, et al. Effects of bariatric surgery in older patients. Ann Surg. 2004;240:243–7.
Trieu HT, Gonzalvo JP, Szomstein S, et al. Safety and outcomes of laparoscopic gastric bypass surgery in patients 60 years of age and older. Surg Obes Relat Dis. 2007;3:383–6.
Willkomm CM, Fisher TL, Barnes GS, et al. Surgical weight loss >65 years old: is it worth the risk? Surg Obes Relat Dis. 2010;6:491–6.
Wittgrove AC, Martinez T. Laparoscopic gastric bypass in patients 60 years and older: early postoperative morbidity and resolution of comorbidities. Obes Surg. 2009;19:1472–6.
Flum DR, Salem L, Elrod JA, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294:1903–8.
Livingston EH, Langert J. The impact of age and Medicare status on bariatric surgical outcomes. Arch Surg. 2006;141:1115–20.
Puzziferri N, Roshek 3rd TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312:934–42.
Backholer K, Wong E, Freak-Poli R, et al. Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev. 2012;13:456–68.
HAS. Obésité: prise encharge chirurgicale de l’adulte. In: Haute Autorité de Santé; 2011.
Topart P, Becouarn G, Ritz P. Comparative early outcomes of three laparoscopic bariatric procedures: sleeve gastrectomy, Roux-en-Y gastric bypass, and biliopancreatic diversion with duodenal switch. Surg Obes Relat Dis. 2012;8:250–4.
Ritz P, Caiazzo R, Becouarn G, et al. Early prediction of failure to lose weight after obesity surgery. Surg Obes Relat Dis. 2013;9:118–21.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32:2133–5.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Witham MD, Avenell A. Interventions to achieve long-term weight loss in obese older people: a systematic review and meta-analysis. Age Ageing. 2010;39:176–84.
Messier SP, Legault C, Loeser RF, et al. Does high weight loss in older adults with knee osteoarthritis affect bone-on-bone joint loads and muscle forces during walking? Osteoarthritis Cartilage. 2011;19:272–80.
Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50:1501–10.
Villareal DT, Banks M, Sinacore DR, et al. Effect of weight loss and exercise on frailty in obese older adults. Arch Intern Med. 2006;166:860–6.
Villareal DT, Chode S, Parimi N, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–29.
Ritz P, Topart P, Benchetrit S, et al. Benefits and risks of bariatric surgery in patients aged more than 60 years. Surg Obes Relat Dis 2014. doi:10.1016/j.soard.2013.12.012.
Robert M, Pasquer A, Espalieu P, et al. Gastric bypass for obesity in the elderly: is it as appropriate as for young and middle-aged populations? Obes Surg. 2014;24:1662–9.
Busetto L, Angrisani L, Basso N, et al. Safety and efficacy of laparoscopic adjustable gastric banding in the elderly. Obesity (Silver Spring). 2008;16:334–8.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339–50.
Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA. 2012;308:2489–96.
Vanommeslaeghe H, Deylgat B, Van Cauwenberge S, et al. Laparoscbopic Roux-en-Y gastric bypass in the elderly: feasibility, short-term safety, and impact on comorbidity and weight in 250 cases. Surg Endos. 2014. doi:10.1007/s00464-014-3751-zdoi.
Gebhart A, Young MT, Nguyen NT. Bariatric surgery in the elderly: 2009–2013. Surg Obes Relat Dis 2014. doi:10.1016/j.soard.2014.04.014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
EM, EB, SG, and PR have no conflicts of interest related to this work. PT received an honorarium for consultancy and teaching from Baxter, Medtronic, Ethicon, and Olympus unrelated to bariatric surgery in the elderly. GB receives an honorarium for consultancy and teaching from Covidien, Ethicon, and Olympus unrelated to bariatric surgery in the elderly.
Ethical Approval
For this type of study formal consent is not required.
Informed Consent
Does not apply.
Funding
None
Rights and permissions
About this article
Cite this article
Montastier, E., Becouarn, G., Bérard, E. et al. Gastric Bypass in Older Patients: Complications, Weight Loss, and Resolution of Comorbidities at 2 Years in a Matched Controlled Study. OBES SURG 26, 1806–1813 (2016). https://doi.org/10.1007/s11695-015-2024-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-2024-9