Abstract
Background
Obesity prevalence increases in elderly population. Bariatric surgery has been underused in patients over 60 because of fears of complications and lower weight loss. We postulated worse outcomes in the elderly in comparison to young and middle-aged population 1 year after gastric bypass.
Methods
We retrospectively analyzed gastric bypass outcomes in young (<40 years), middle-aged (40 to 55 years), and elderly (>60 years) patients between 2007 and 2013. Each subject over 60 (n = 24) was matched with one subject of both the other groups according to gender, preoperative body mass index (BMI), surgical procedure, and history of previous bariatric surgery (n = 72).
Results
Older subjects demonstrated higher prevalence of preoperative metabolic comorbidities (70 vs 30 % in the <40-year-old group, p < 0.0001). Mean duration of the surgical procedure, mean length of stay, and early and late complication rates were similar between age groups. A trend towards fewer early complications and less-severe complications in the younger groups was noted. One-year weight loss results were similar between young, middle-aged, and elderly patients (percentage of excess BMI loss (EBL%), 74.4 ± 3.5; 78.9 ± 4.5, and 73.7 ± 4.5 respectively, p = 0.69). Age was not predictive of weight loss failure 1 year after surgery. Remission and improvement rates of comorbidities were similar between age groups 6 months after surgery.
Conclusions
Our study confirms weight loss efficacy of gastric bypass in the elderly with acceptable risks. Further studies evaluating the benefit-risk balance of bariatric surgery in the elderly population will be required so as to confirm the relevance of increasing age limit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Life expectancy is increasing, with more elderly people identified as obese. Currently, 17 % of the French population over 65 years of age are obese according to the national survey following the epidemiology of obesity (ObEpi), and 35 % of subjects over 60 years old in the USA suffer from obesity including further increase in extreme obesity [1].The prevalence of obesity in the elderly population is anticipated to grow as the baby boomer population continues to age. Rapidly accumulating evidence associates excess body fat with a panel of metabolic, cardiovascular, psychological comorbidities, as well as a direct increase in risk of dementia [2]. As both aging and obesity may have a severe impact on public health, an increasing obese elderly population will undoubtedly cause growing financial problems in health care systems in developed countries [3].
As a consequence, concerns have been raised for years about the treatment of obesity in the elderly [4, 5]. Bariatric surgery in the elderly is still under debate as the risk-benefit balance is questioned. Currently, surgical weight loss in the elderly is indicated on a case-by-case basis [6–8]. One specific feature of obesity in the elderly is sarcopenia, which is a component of the frailty syndrome. Sarcopenia is the degenerative loss of skeletal muscle mass (0.5–1 % loss/year after the age of 25), quality, and strength associated with aging. It could restrict weight loss efficacy of bariatric procedures in the elderly. Thus, risk-benefit balance for bariatric surgery in the >60 years of age population should be questioned not only from a safety perspective but also for efficacy. Indeed, previous studies reported less weight loss in the elderly after bariatric surgery [9–11].
Furthermore, an increased operative risk in elderly patients has been reported due to a greater prevalence of metabolic comorbidities [9, 12–14]. Thus, many bariatric programs use age cut-off partly due to higher perioperative morbidity and mortality risks. Consequently, weight loss surgery has been underused in patients over 60 because of fears of complications and reduced success in achieving weight loss [15]. Moreover, long-term benefits of surgical weight loss concerning morbidity and mortality have not been proven in the elderly population especially as the correlation between body mass index (BMI) and mortality risk is weaker in that population [16, 17].
In the present study, we wanted to determine the influence of age on gastric bypass results at 1 year. We postulated that age classes would have a significant effect on weight loss results with worse outcomes in the elderly. Contrary to most previous studies, we were careful to match age classes groups by gender, preoperative BMI, and previous history of bariatric surgery in order to avoid maximum bias.
Materials and Methods
Population and Study Design
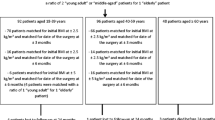
This is a retrospective analysis of gastric bypass outcomes in young (<40 years of age), middle-aged (40 to 55 years of age), and elderly (>60 years of age) patients who underwent gastric bypass between May 2007 and February 2013 in two expert centers of bariatric surgery (Edouard Herriot Hospital, Lyon and Private Hospital of Loire, St Etienne, France). During this period, 366 laparoscopic gastric bypasses were performed by two experienced surgeons. In order to determine reliably the influence of age classes on bariatric surgery outcomes, we divided the whole population into three groups according to age before surgery, as follows: <40 years old, between 40 and 55 years old, and >60 years old. As bariatric surgery is currently not recommended in France for the elderly, only 27 patients (7.4 %) from the whole population operated on were over 60 years of age before surgery. We performed a 1:2 matching considering the >60-year-old group as the reference group. We succeeded in perfectly matching 24 subjects over 60 years of age with one subject from both other groups according to gender, preoperative BMI, and history of previous bariatric surgery. Subjects were also matched according to the type of surgical procedure (omega loop bypass (OLB) or Roux-en-Y gastric bypass (RYGBP)), except for one subject from the >60-year-old age group who benefited from an OLB, whereas its counterparts benefited from a RYGBP. A total of 72 patients were finally included in the study. Forty-two subjects had primary gastric bypass, and no history of previous bariatric surgery: we performed another statistical analysis on this subgroup of patients so as to avoid bias as it was previously reported that revisional surgery impact weight loss outcomes.
Surgical Procedures
Laparoscopic RYGBP was performed in 53 subjects and laparoscopic OLB in 19 subjects.
Laparoscopic Roux-en-Y Gastric Bypass
A five-port technique was used as described by Lonroth et al. [18]. It consisted in a small gastric pouch (30 cm3) by stapling the stomach using a linear stapler. The first jejunal loop was used and moved up into an antecolic position after an omental transection so as to perform the gastro-jejunal anastomosis. An end-to-side gastro-jejunal anastomosis was performed using a linear stapler. Closure of the anterior part of the anastomosis was done using a running suture. The alimentary limb was 150 cm long and the biliopancreatic limb was 30 cm long. A latero-lateral jejuno-jejunal anastomosis was performed with a linear stapler. The closure of the Petersen area was systematic, using a nonresorbable silk suture (2/0).
Laparoscopic Omega Loop Gastric Bypass
A five-port technique was also used as described by Rutledge [19]. A long and narrow gastric tube calibrated with a 37-French bougie was performed using a linear stapler and began at the angle of the lesser curvature until the angle of His. A unique anastomosis was made between the bottom of the gastric tube and a long jejunal OLB of 200 cm. It was an end-to-side gastro-jejunal anastomosis done with a linear stapler and closed on its anterior part with a running suture.
Perioperative Data Collection
Comorbidities including type 2 diabetes (T2D), high blood pressure (HTN), dyslipidemia, liver steatosis, severe obstructive sleep apnea syndrome (OSAS), and degenerative joint disease (joint pain) were evaluated and recorded at baseline and 6 months after surgery. Improvement of dyslipidemia, HTN, and T2D was considered established when medications were reduced. T2D remission was defined as cessation of antidiabetic treatments and HbA1c <6 % and/or fasting blood glucose levels <100 mg/dl, according to the American Diabetes Association (ADA) guidelines. Dyslipidemia and HTN were considered in remission when medications were stopped. Duration of the surgical procedure, operative complications, conversions to laparotomy, and mean length of hospital stay were recorded. Postoperative features at 2 months, 6 months, 1 year, and at the end of the follow-up were prospectively collected using a computerized database devoted to bariatric surgery. The early complications rate (within 30 days after surgery) as well as the late complications rate were recorded. Body weight, BMI, percentage of excess BMI loss (EBL%), and time to weight nadir were recorded or calculated to quantify weight loss. Weight loss failure was defined as BMI >35 kg m−2 or EBL% <50 % 1 year after surgery.
Statistical Analysis
MedCalc 9.0 (MedCalc Software, Belgium) was used for statistical analysis. Data were presented as arithmetic means ± 1 SEM. We performed a 1:2 matching to compare outcomes according to the three age groups: results of each subject of the >60-year-old group were compared with the results of its counterparts of both the other groups. Concerning quantitative variables, differences between the three groups were assessed by one-way ANOVA. A Chi-square test with a Yates’ correction for continuity was applied for comparison of proportions. A multiple logistic regression analysis was performed to identify relevant factors associated with weight loss failure at 1 year. p < 0.05 was considered significant.
Results
Baseline Characteristics of the Population
The anthropometric characteristics of the whole study population and for the subgroup of primary gastric bypass at baseline are presented in Table 1. The population was mostly female (67 % of female), and mean initial BMI was 41.5 kg m−2. Considering the study design, gender and initial BMI were similar between age groups. It is of note that the previous maximal weight was not different between age groups even though obesity history is likely to be longer in older subjects.
Prevalence of comorbidities at baseline is shown in Fig. 1. Prevalence of metabolic comorbidities was obviously related to age classes, older subjects demonstrating a higher operative risk profile. Indeed, despite similar BMI, the rate of metabolic comorbidities was between 15 to 30 % in the <40-year-old group, vs above 70 % in the >60-year-old group (p < 0.0005 for T2D, HTN, OSAS, and dyslipidemia).
Prevalence (%) of baseline comorbidities according to age groups (white bars, <40 years of age group; grey bars, 40–55 years of age group; black bars, >60 years of age group) in the whole population. T2D type 2 diabetes, HTN high blood pressure, OSAS obstructive sleep apnea syndrome. *p < 0.05; ***p < 0.0005
Baseline surgical features are resumed in Table 2 for the whole population. Given the study design, previous bariatric surgery prevalence, mainly gastric banding, was the same between groups (38 % in each age group). Nobody had previous malabsorptive procedure. RYGBP procedure was predominantly performed in comparison to OLB without any imbalance between the 3 age groups.
Operative Data and Complications
Operative data and complication rates according to age groups are presented in Table 3 for the whole population and for the subgroup of primary gastric bypass. Mean duration of the surgical procedure was 132 min for the <40-year-old group, 134 min for the 40-55-year-old group and 154 min for the >60-year-old group (p > 0.05). Neither conversion to laparotomy nor intraoperative complications occurred whatever the age group. The mean length of stay was not longer in the elderly group (4.6 ± 0.1 days), despite more frequent preoperative metabolic comorbidities.
Early Complications
Early complications rate was not significantly different between age groups (p = 0.54), even if early complications were quantitatively more frequent in the >60-year-old group. When considering only primary gastric bypass patients (n = 42) and when excluding revisional procedures, early complication rates were similar between groups.
Three patients from the >60-year-old group (13 %) had early complications. The first patient benefited from a RYGBP after failure of gastric banding and presented with a mesenteric hematoma at the jejuno-jejunal anastomosis responsible for bowel obstruction. This complication required a redo surgery on postoperative day 4 for drainage and adhesiolysis. The redo surgery was complicated by septic shock and a pulmonary embolism. The patient died 14 days after surgery of a multiple organ failure. The second patient presented with hemorrhage on port site requiring drainage at postoperative day 1 after OLB. The third patient had an anastomotic ulcer after OLB. He complained of epigastric pain and food intolerance. He did not take the proton pomp inhibitor (PPI) medication. The upper gastrointestinal endoscopy confirmed the diagnosis at postoperative day 30. The anastomotic ulcer healed after good observance of PPI medication (80 mg/day during 2 months).
Two patients from the 40- to 55-year-old group (8 %) had early complications after RYGBP. The first one had an anastomotic ulcer on postoperative day 3, which required blood transfusions and endoscopic metallic-clip placement. The second patient had pneumonia, successfully treated with antibiotics.
One patient from the <40-year-old group (3.7 %) also had early complications. He presented with anastomotic stenosis, which required instrumental distension, then a stent placement and finally a surgical redo anastomosis 6 months after RYGBP.
Late Complications
Mean postoperative follow-up duration was 21.4 ± 1.4 months without any differences between age groups (p = 0.85).
Two subjects from the >60-year-old group (8 %) exhibited late complications. Two patients presented with anastomotic ulcers after OLB. Both patients were smokers. The first patient had a perforated anastomotic ulcer after cessation of PPI treatment requiring a laparoscopic suture, 11 months after surgery. The second patient had an anastomotic bleeding ulcer 2 months after surgery while he was treated by antiplatelet drug and had stopped his PPI medication. He benefited from emergency surgery with the reversal of the OLB. Two patients from the 40- to 55-year-old group (8 %) had anastomotic ulcers after RYGBP that healed with PPI medication. Two patients from the <40-year-old group (8 %) also had late complications. The first one had a gastric fistula on the remnant stomach after revisional RYGBP requiring redo surgery for drainage 6 months after surgery. The second patient presented with an internal hernia 1 year after RYGBP treated by laparoscopic reduction without bowel resection.
Weight Loss Results
Weight loss results are presented in Table 4 and in Fig. 2. Results are presented for the whole population (n = 72) as well as for the subgroup of primary gastric bypass, excluding revisional procedures (n = 42). For primary gastric bypass procedures, mean BMI at 1 year was between 28.4 and 29.0 kg.m−2 (Table 4) and mean EBL% was between 79.6 and 83.4 % (Table 4; Fig. 2b) without any significant impact of age groups. As expected, weight loss results of the whole population were not as good as in the primary gastric bypass subgroup, but it was not statistically significant. Mean BMI at 1 year was between 29.0 and 29.8 kg.m−2 (Table 4), and mean EBL% was between 73.7 and 78.9 % (Table 4; Fig. 2a). Evolution of BMI and EBL% from baseline to 1 year were not different between age groups. The time to reach weight nadir after surgery was not different between age groups (p = 0.44). Weight loss failure at 1 year in the whole population, defined as BMI >35 kg.m−2 or EBL% <50 %, was observed in 16.6 % of subjects in the >60-year-old group, and it was not significantly different from the other groups (p = 0.37).
When analyzing relevant factors that could explain weight loss failure at 1 year using multiple logistic regressions, we found that female gender, high initial BMI, and previous bariatric surgery were significantly and independently associated with 1-year weight loss failure while age and bypass technique (OLB vs RYGBP) were not.
Resolution of Comorbidities
Improvement and remission rates of main metabolic comorbidities 6 months after gastric bypass are summarized in Table 5. Early metabolic benefits from surgery were similar between groups, with a T2D remission rate from 25 to 50 %, a HTN remission rate from 44 to 71 %, and a dyslipidemia remission rate from 50 to 75 %.
Discussion
Bariatric surgery in the elderly (>60 years old) has been under-used and represented, in 2005, 2.7 % of all bariatric procedures performed at academic centers [13]. Thus, only a few previous studies reported bariatric surgery outcomes in the elderly. In the current study, we determined the influence of age classes on weight loss results 1 year after gastric bypass. Age groups were matched by gender, BMI, bariatric procedure (OLB vs RYGBP), and previous history of bariatric surgery in a way to limit confounding factors. In our study, elderly candidates for bariatric surgery had more metabolic comorbidities than younger candidates despite similar gender and BMI, highlighting a potential role of obesity duration in the genesis of metabolic complications. Another explanation could be that body fat distribution changes overtime, with an increase in visceral abdominal fat and a decrease in subcutaneous abdominal fat. These changes occur even if BMI does not change significantly and have important consequences on metabolic profile and cardiovascular risk factors. It has already been reported that older bariatric candidates had a higher operative risk profile [9, 12–14]. In bariatric candidates over 70, there is an average of four comorbidities preoperatively [20]. Conversely, older adults do not demonstrate any increased psychological risk factors compared with middle-aged or young adults before bariatric surgery [21]. The greater operative risk profile in the >60-year-old surgical candidates is thought to be associated with increased perioperative morbidity and mortality. Flum et al. noted a 4.8 vs 1.7 % mortality rate for patients over 65 years of age compared with younger patients [22]. Livingston et al. used the National Inpatient Survey database for their report showing a three times higher mortality for patients over 55 years of age as compared with younger patients [23], mainly concerning open procedures. In the current study, one patient from the >60-year-old group, who benefited from revisional surgery, died postoperatively, but no death occurred in younger groups. Concerning perioperative morbidity, Varela et al. reported that compared with nonelderly, elderly patients who underwent bariatric surgery had longer lengths of stay, more overall complications, pulmonary complications, hemorrhagic complications, and wound complications [13]. Dorman et al. also reported that the older the patient, the longer the hospital stay, but there were no more major events following bariatric surgery [24]. Unlike these authors, we did not report increased length of stay nor increased operative time in the >60-year-old group. These results are in accordance with some previous studies [12, 25] and the prospective data from the Longitudinal Assessment of Bariatric Surgery Consortium, which did not identify advancing age as a perioperative risk factor for bariatric procedures [26]. This is probably due to the improvement of anesthetic management and surgical technique in recent years. However, even if early complications rate was not statistically different in the >60-year-old group, we observed fewer early complications and fewer severe complications in the younger groups.
One of the main results of the present study is that 1-year weight loss results of gastric bypass were identical between young, middle-aged, and elderly patients independently of history of previous bariatric procedure. Moreover, the elderly were not likely to lose less weight. In addition, time to reach weight nadir, as well as 1-year BMI and EBL% were not different between age groups. Age did not impact bariatric surgery outcomes, and this result was independent of previous history of bariatric surgery. These results are in contradiction with previous studies reporting greater weight loss in younger populations [9–11]: indeed, it has been reported that patients under 45 years lose greater amount of excess BMI than older patients after RYGBP or sleeve gastrectomy [27] and that a greater short-term weight loss was observed in women between 20 and 45 vs 55 and 65 years of age following bariatric surgery [28]. However, in agreement with our results, it was also previously reported that EBL% in gastric bypass patients were not different between the patients >65 years old (n = 100) and those <65 years old at 12 months (74.8 vs 77.8 %) and 24 months (83.4 vs 78.5 %) [12]. Several authors have reported surgical weight loss results in elderly patients without comparing them to younger patients: Trieu et al. reported a mean EWL% 1 year after gastric bypass of 53.8 % in 92 patients >60 years old [29], and Loy et al. reported a mean EWL% 1 year after gastric banding of 36 ± 12.7 % in 55 patients >70 years old associated with moderate resolution of comorbid conditions [20]. In addition, a French study identified that subjects >50 years of age had a 1.8 greater risk of weight loss failure after gastric banding [29]. In our study, weight loss failure was not significantly different between age groups. These results were not expected and go against our initial hypothesis. Aging involves a decrease in muscle mass shifting to more fat mass, which normally peaks around 65 years in men and later in women [30]. High levels of fat mass associated with low muscle mass may lead to decrease mobility as well as metabolic disorders, explaining the high rate of comorbidities observed in the >60-year-old group. These body composition changes associated with obesity in the elderly correspond to a specific phenotype that has been recently defined as sarcopenic obesity. Moreover, obese older subjects may be sarcopenic whatever their amount of fat free mass due to a progressive deterioration of muscle quality with reduction in their functional status, aerobic capacity, strength balance, and walking speed [31]. The decrease in muscle mass and mobility is supposed to reduce total energy expenditure in the elderly population and may lead to limitation of weight loss or weight regain, mainly characterized by the accumulation of abdominal fat [32]. However, while we did not assess sarcopenia, our results clearly demonstrate that weight loss efficiency of gastric bypass procedure is not altered in the elderly population. It is of note that this study has several limitations including a retrospective design, a small sample size, a short mean follow-up, which could underestimate late complications rate. Nevertheless, the challenging design of the study which explains the small sample size, reinforces the reliability of our results. Indeed, elderly patients are carefully selected for bariatric surgery for being considered at higher risk, representing a small sample of the obese population operated on. Moreover, due to the 1:2 matching design, the inclusion of revisional procedures as well as OLB procedures is representative of the gastric bypass population, reinforcing the relevance of our conclusions, rather than being a design flaw. The good weight loss results obtained in this matched case–control study design together with the reasonable complication rate argue for an extension of the age limit for gastric bypass procedures. This is all the more true that despite a higher prevalence of comorbidities in the older age group (>70 vs <30 % in the youngest group), the improvement and remission rates of the main metabolic comorbidities (T2D, HTN, and dyslipidemia) were similar between age groups.
Despite acceptable risks and weight loss efficiency of gastric bypass surgery in all age classes, the expected benefits of bariatric surgery in the elderly are questionable. Benefits in elderly may concern a gain in mobility, autonomy, and quality of life rather than increased life expectancy and decreased cardiovascular morbidity and mortality. Indeed, several epidemiological studies indicate that BMI is inversely related to mortality in the elderly [33–36]: this is called the “obesity paradox”. In addition, because of food restriction and malabsorption, gastric bypass procedures could expose them to undernutrition, which is already more prevalent in the elderly. Thus, long-term nutritional consequences of bariatric surgery in the elderly could lead to the frailty syndrome and have to be evaluated. However, quality of life seems to be improved after bariatric surgery in the elderly, as well as metabolic comorbidities [11, 37–39]. Thus, further studies evaluating the benefit-risk balance of bariatric surgery in the elderly population will be required so as to confirm the relevance of increasing age limit.
References
Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55.
Smith E, Hay P, Campbell L, et al. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obes Rev. 2011;9:740–55.
Roubenoff R. Sarcopenic obesity: the confluence of two epidemics. Obes Res. 2004;12:887–8.
McTigue KM, Hess R, Ziouras J. Obesity in older adults: a systematic review of the evidence for diagnosis and treatment. Obesity (Silver Spring). 2006;14:1485–97.
Andres R, Elahi D, Tobin JD, et al. Impact of age on weight goals. Ann Intern Med. 1985;103:1030–3.
Laville M, Romon M, Chavrier G, et al. Recommendations regarding obesity surgery. Obes Surg. 2005;15:1476–80.
Sauerland S, Angrisani L, Belachew M, et al. Obesity surgery: evidence-based guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2005;19:200–21.
Fried M, Hainer V, Basdevant A, et al. Inter-disciplinary European guidelines on surgery of severe obesity. Int J Obes (Lond). 2007;31:569–77.
Sugerman HJ, DeMaria EJ, Kellum JM, et al. Effects of bariatric surgery in older patients. Ann Surg. 2004;240:243–7.
St Peter SD, Craft RO, Tiede JL, et al. Impact of advanced age on weight loss and health benefits after laparoscopic gastric bypass. Arch Surg. 2005;140:165–8.
Taylor CJ, Layani L. Laparoscopic adjustable gastric banding in patients > or =60 years old: is it worthwhile? Obes Surg. 2006;16:1579–83.
Willkomm CM, Fisher TL, Barnes GS, et al. Surgical weight loss >65 years old: is it worth the risk? Surg Obes Relat Dis. 2010;6:491–6.
Varela JE, Wilson SE, Nguyen NT. Outcomes of bariatric surgery in the elderly. Am Surg. 2006;72:865–9.
Benotti PN, Wood GC, Rodriguez H, et al. Perioperative outcomes and risk factors in gastric surgery for morbid obesity: a 9-year experience. Surgery. 2006;139:340–6.
Sosa JL, Pombo H, Pallavicini H, et al. Laparoscopic gastric bypass beyond age 60. Obes Surg. 2004;14:1398–401.
Chen Z, Yang G, Offer A, et al. Body mass index and mortality in China: a 15-year prospective study of 220 000 men. Int J Epidemiol. 2012;41:472–81.
Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363:2211–9.
Lönroth H, Dalenbäck J, Haglind E, et al. Laparoscopic gastric bypass. Another option in bariatric surgery. Surg Endosc. 1996;10:636–8.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11:276–80.
Loy JJ, Youn HA, Schwack B, et al. Safety and efficacy of laparoscopic adjustable gastric banding in patients aged seventy and older. Surg Obes Relat Dis. Available from http://dx.doi.org/10.1016/j.soard.2013.06.022.
Heinberg LJ, Ashton K, Windover A, et al. Older bariatric surgery candidates: is there greater psychological risk than for young and midlife candidates? Surg Obes Relat Dis. 2012;8:616–22. discussion 622–624.
Flum DR, Salem L, Elrod JAB, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294:1903–8.
Livingston EH, Langert J. The impact of age and Medicare status on bariatric surgical outcomes. Arch Surg. 2006;141:1115–20. discussion 1121.
Dorman RB, Abraham AA, Al-Refaie WB, et al. Bariatric surgery outcomes in the elderly: an ACS NSQIP study. J Gastrointest Surg. 2012;16:35–44. discussion 44.
Wittgrove AC, Martinez T. Laparoscopic gastric bypass in patients 60 years and older: early postoperative morbidity and resolution of comorbidities. Obes Surg. 2009;19:1472–6.
Longitudinal Assessment of Bariatric Surgery (LABS) Consortium, Flum DR, Belle SH, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361:445–54.
Contreras JE, Santander C, Court I, et al. Correlation between age and weight loss after bariatric surgery. Obes Surg. 2013;23:1286–9.
Ochner CN, Teixeira J, Geary N, et al. Greater short-term weight loss in women 20–45 versus 55–65 years of age following bariatric surgery. Obes Surg. 2013;23:1650–4.
Chevallier J-M, Paita M, Rodde-Dunet M-H, et al. Predictive factors of outcome after gastric banding: a nationwide survey on the role of center activity and patients’ behavior. Ann Surg. 2007;246:1034–9.
Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2:141–7.
Villareal DT, Banks M, Siener C, et al. Physical frailty and body composition in obese elderly men and women. Obes Res. 2004;12:913–20.
Nair KS. Aging muscle. Am J Clin Nutr. 2005;81:953–63.
Zekry D, Herrmann FR, Vischer UM. The association between the body mass index and 4-year all-cause mortality in older hospitalized patients. J Gerontol A Biol Sci Med Sci. 2013;68:705–11.
Janssen I, Katzmarzyk PT, Ross R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. J Am Geriatr Soc. 2005;53:2112–8.
Kalmijn S, Curb JD, Rodriguez BL, et al. The association of body weight and anthropometry with mortality in elderly men: the Honolulu Heart Program. Int J Obes Relat Metab Disord. 1999;23:395–402.
Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279:585–92.
Fatima J, Houghton SG, Iqbal CW, et al. Bariatric surgery at the extremes of age. J Gastrointest Surg. 2006;10:1392–6.
Quebbemann B, Engstrom D, Siegfried T, et al. Bariatric surgery in patients older than 65 years is safe and effective. Surg Obes Relat Dis. 2005;1:389–92. discussion 392–393.
Trieu HT, Gonzalvo JP, Szomstein S, et al. Safety and outcomes of laparoscopic gastric bypass surgery in patients 60 years of age and older. Surg Obes Relat Dis. 2007;3:383–6.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robert, M., Pasquer, A., Espalieu, P. et al. Gastric Bypass for Obesity in the Elderly: Is It as Appropriate as for Young and Middle-Aged Populations?. OBES SURG 24, 1662–1669 (2014). https://doi.org/10.1007/s11695-014-1247-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1247-5