Abstract
Purpose
The treatment of leishmaniasis, an anthropozoonosis caused by Leishmania protozoa, is limited by factors, such as adverse effects, toxicity, and excessive cost, which has highlighted the importance of novel drugs. In this context, natural products have been considered as sources of antileishmanial agents. This study investigated the leishmanicidal activity of Microgramma vacciniifolia frond lectin (MvFL) on promastigotes and amastigotes of Leishmania amazonensis.
Methods
The effects of MvFL on promastigote proliferation and macrophage infection by amastigotes were evaluated and mean inhibitory concentrations (IC50) were calculated. As a safety assessment, the hemolytic capacity of MvFL (6.25–200 µg/mL) against mouse and human erythrocytes was determined. Additionally, the ability of MvFL (6.25–100 µg/mL) to modulate lysosomal and phagocytic activities and the nitric oxide (NO) production by murine peritoneal macrophages was also investigated.
Results
After 24 h, MvFL inhibited the proliferation of L. amazonensis promastigotes, with an IC50 of 88 µg/mL; however, hemolytic activity was not observed. MvFL also reduced macrophage infection by amastigotes with an IC50 of 52 µg/mL. Furthermore, treatment with MvFL reduced the number of amastigotes internalized by infected murine peritoneal macrophages by up to 68.9% within 48 h. At a concentration of 25 µg/mL, MvFL stimulated lysosomal activity of macrophages within 72 h, but did not alter phagocytic activity or induce NO production at any of the tested concentrations.
Conclusion
MvFL exerts antileishmanial activity and further studies are needed to assess its therapeutic potential in in vivo experimental models of leishmaniasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leishmaniasis is a cosmopolitan public health concern affecting more than 98 countries, with an estimated 900,000 to 1,600,000 new cases occurring annually, mainly in Brazil, Ethiopia, Somalia, South Sudan, and Sudan [1, 2]. Leishmaniasis is a complex of infectious parasitic diseases caused by protozoa of the genus Leishmania (family Trypanosomatidae), which are transmitted through bites of female phlebotomine vectors, and are associated with lesions in different organs [3].
According to the clinical manifestations of the disease, Leishmaniasis is divided into: cutaneous leishmaniasis, with 95% of the cases occurring in the Americas, Mediterranean Basin, Middle East, and Central Asia; mucocutaneous leishmaniasis, with 90% of the cases occurring in Bolivia, Brazil, and Peru; and visceral leishmaniasis, with more than 90% of the cases occurring in seven countries, including Brazil [4, 5]. Leishmania amazonensis is one of the pathogenic species distributed throughout South America, with a high prevalence in Brazil, and is associated with different clinical forms of leishmaniasis. It is also the main causative agent of diffuse cutaneous leishmaniasis in America, a rare clinical form developed by individuals infected with this parasite and that is commonly refractory to currently available treatments [6, 7]. To survive inside host cells and spread into host organs, the parasites trigger mechanisms of immune silencing and evasion to escape oxidative stress induced by hydrolases, lysosomal attack inside macrophage vacuoles, and intracellular calcium, which facilitates alteration of the cytoskeleton [8, 9].
The first prescription option for leishmaniasis is the pentavalent antimonial drugs; N-methyl-glucamine antimoniate is the first-choice drug in Brazil against cutaneous, mucocutaneous, and visceral leishmaniasis whilst amphotericin B (Amp-B) and pentamidine are the alternative options [10, 11]. However, the choice of drug depends on the Leishmania species and factors intrinsic to the patient (comorbidities, pregnancy and aging). Nonetheless, these drugs are potentially toxic, with several kinds of side effects, and low effective, which leads many patients to choose not to undergo treatment [12].
Thus, there is a need to develop novel antileishmanial compounds with pharmacological potential and reduced toxicity using alternative methods that are reliable, have lower cost, and are easily accessible. In this context, plant species have been considered as promising sources of substances with antileishmanial activity as plants in general contain diverse bioactive compounds that made them promising sources for development of novel drugs [13, 14]. Lectins, a heterogeneous group of proteins that can recognize and interact with carbohydrates present on the surface of different cell types, are among these bioactive compounds [15]. These biomolecules possess several biological properties, including antimicrobial [16], anti-inflammatory [17], antitumor [18], immunomodulatory [19], and leishmanicidal [20, 21] properties. The ability of lectins to interact with target glycans on cells plays a significant role in the immunological defense against pathogens [22].
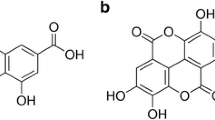
Microgramma vacciniifolia (Langsd. & Fisch) Copel. (family Polypodiaceae) is an epiphyte pteridophyte that has ornamental uses, is used as a medicinal plant for intestinal and respiratory infections, and hemorrhages, and promotes expectoration [23, 24]. Two lectins have been identified and isolated from M. vacciniifolia: one from the rhizome (MvRL) [25] and the other from the frond (MvFL) [26]. MvFL is a multifunctional protein that exhibits lectin activity and has been reported to exert immunomodulatory effects on human lymphocytes, which may be linked to its antitumor properties [18, 26].
There are no reports on the antileishmanial effects of the lectins derived from M. vacciniifolia. Considering the increasing need for alternatives sources of bioactive compounds that can facilitate the development of new drugs, this study aimed to investigate the antileishmanial and immunomodulatory activities of MvFL against promastigotes and internalized amastigote forms of L. amazonensis in vitro. Furthermore, the hemolytic activity of MvFL against mouse and human erythrocytes was evaluated.
Materials and Methods
Plant Material and Isolation of MvFL
Fronds of M. vacciniifolia were collected at the campus of the Universidade Federal de Pernambuco (UFPE) (Recife, Brazil) with authorization (number 36,301) from the Instituto Chico Mendes de Conservação da Biodiversidade. Access was recorded (A9D147B) at the Sistema Nacional de Gestão do Patrimônio Genético e do Conhecimento Tradicional Associado. Taxonomic identification was done at the herbarium Dárdano de Andrade Lima, at the Instituto Agronômico de Pernambuco (Recife, Brazil), where a voucher specimen (number 63,291) was deposited.
MvFL was isolated as described by Patriota et al. [26]. Briefly, fronds of M. vacciniifolia were washed with tap and distilled water and then dried at 28 °C for 7 days before being powdered using a blender. The powder was extracted with 0.15 M NaCl (10%, w/v) for 16 h at 25 °C with constant agitation using a magnetic stirrer. The mixture was filtered and centrifuged at 9000 × g for 15 min at 4 °C, and the supernatant was collected and used as the frond extract in experiments. Frond extract (containing 3.0 mg protein) was loaded onto a Sephadex G-75 (GE Healthcare Life Sciences, Marlborough, MA, USA) column (30.0 cm × 1.5 cm) equilibrated with distilled water. The fractions corresponding to the first absorbance peak at 280 nm were collected, lyophilized, resuspended in 0.1 M Tris–HCl (pH 8.0), and loaded (2.5 mg protein) onto a DEAE-Sephadex (GE Healthcare Life Sciences) ion exchange column (3.0 cm × 2.0 cm) previously equilibrated with the same buffer. The column was washed with Tris buffer and the adsorbed proteins (MvFL) were eluted with 0.1 M Tris–HCl (pH 8.0) containing 1.0 M NaCl, dialyzed with distilled water for 4 h, and lyophilized.
Protein Concentration and Hemagglutination Activity
The concentration of proteins was estimated according to the method described by Lowry et al. [27] using bovine serum albumin (31.25–500 μg/mL) for the standard curve. The sample (0.2 mL) was incubated for 10 min at 25 °C with 1 mL alkaline copper solution (1 mL of 0.5% [w/v] copper sulfate in 1% [w/v] sodium citrate added to 50 mL of 2% [w/v] sodium carbonate solution in 0.1% [w/v] sodium hydroxide). After incubation, 0.1 mL of–Folin-Ciocalteu reagent (Sigma-Aldrich, St. Louis, MO, USA) diluted 1:1 in water was added, and after 30 min incubation at 25 °C, the absorbance was measured at 720 nm.
The carbohydrate-binding ability of MvFL was assessed using a hemagglutination activity (HA) assay according to the protocol described by Patriota et al. [26]. Briefly, 50 μL of the sample was serially diluted twice in 0.15 M NaCl and mixed with 50 μL of 2.5% v/v suspension of rabbit erythrocytes fixed with glutaraldehyde [28] in each well of V-bottomed 96-well microplates. The plates were then incubated at 27 °C for 45 min. Erythrocyte suspension incubated in the absence of a sample was used as the negative control. HA was expressed as the reciprocal (titer−1) of the highest dilution of the sample that was able to promote agglutination. Specific HA was calculated as the ratio of HA to protein concentration (mg/mL). HA inhibitory assay was also performed in the presence of 0.5 mg/mL fetuin as described by Patriota et al. [26]. The Ethics Committee on Animal Use of UFPE approved the method used to collect rabbit erythrocytes (process 23076.033782/2015-70).
Anti-leishmanial Assay in Promastigote Forms of L. amazonensis
For conducting in vitro assays to assess antileishmanial activity, promastigote forms of L. amazonensis (IFLA/BR/67/PH8) maintained at the Laboratório de Atividade Antileishmania, Núcleo de Pesquisas em Plantas Medicinais, Universidade Federal do Piauí were used. Promastigote forms of L. amazonensis were cultured in Schneider media (Sigma-Aldrich) supplemented with 10% bovine fetal serum (BFS) (Sigma-Aldrich) and 10,000 IU/10 mg/mL penicillin–streptomycin (Sigma-Aldrich) at 26 °C in a greenhouse of biological oxygen demand (BOD) [29, 30]. Promastigotes in the logarithmic growth phase (1 × 106 leishmania/100 μL medium) were seeded in 96-well culture plates containing supplemented Schneider’s—medium, and then serial dilutions of MvFL (6.25, 12.5, 25, 50, 100, 200, 400, and 800 μg/mL) were added to the wells and the plates were incubated at 26 °C for 42 h in a BOD incubator.
Next, 20 μL of 1 mM resazurin (Sigma-Aldrich) was added to each well, and the plate was incubated for a further 6 h in the BOD incubator. Therefore, the total incubation time was 48 h. The absorbance was read at 550 nm using a BioTek ELx800 microplate reader (BioTek Instruments, Inc., Winooski, VT, USA). Schneider medium with 0.2% DMSO was used as the negative control and its absorbance value was considered as representing 100% viability of the parasites. Amp-B at a concentration of 2 μg/mL was used as the positive control to validate the experiment. A blank read for each concentration and control was performed to subtract the absorbance resulting from the interaction of the medium with the tested plant materials. All experiments were performed in triplicate.
Hemolysis Assay
The hemolytic activity of MvFL was evaluated using mouse and human erythrocytes, according to the protocol described by Pita et al. [31], with some modifications. Swiss females (25–30 g, 6–8 weeks of age) were obtained from the bioterium of the Laboratório de Imunopatologia Keiso Asami (LIKA-UFPE). The animals were maintained under a 12 h light/dark cycle at a temperature of 23 ± 2 °C), with free access to water and food (Presence Nutrição Animal, São Paulo, Brazil). The mice were anesthetized with an intraperitoneal injection of a mixture of ketamine (150 mg/kg) and xylazine (15 mg/kg) and subjected to brachial blood collection, which was immediately mixed with the anticoagulant ethylenediamine tetraacetic acid (EDTA). Similarly, approximately 4 mL of peripheral venous blood was collected in vials containing EDTA from voluntary donors with blood A+, B+, AB+, and O+ types who signed the free and informed consent form. All experiments performed in this study were approved by the Animal Research Ethics Committee of UFPE (permission No. 0037/2020) and by the Human Research Ethics Committee of UFPE (process 33550320.1.0000.5208).
To isolate erythrocytes, 2 mL of whole blood was diluted with 8 mL of phosphate-buffered saline (PBS, pH 7.4) and centrifuged at 300 g for 5 min. The supernatant and buffy coat were then removed by gentle aspiration, and the above process was repeated twice. Erythrocytes were then resuspended in PBS to make a 1% suspension (v/v) for use in hemolysis assay. Various concentrations of MvFL (6.25, 12.5, 25, 50, 100, and 200 μg/mL) dissolved in PBS was added to 1 mL of the erythrocytes suspension. The MvFL-erythrocyte mixtures were incubated in a mixer for 60 min at 25 °C and then centrifuged at 3000 rpm for 5 min. The absorbance of the supernatants was determined at 540 nm using a microplate reader to measure the extent of red blood cell lysis and determine the concentration that produces 50% hemolysis (HC50). Positive (100% hemolysis) and negative control (0% hemolysis) were also used and were determined by incubating erythrocytes with 1% Triton X-100 in PBS and PBS alone, respectively. All experiments were performed in triplicate.
Antileishmanial Activity of MvFL Against Intramacrophage Amastigotes
Male and female BALB/c mice also obtained from LIKA-UFPE, aged between 4 and 5 weeks, weighing 25–30 g, were used for the present experiment. Mice were intraperitoneally injected with 1.5 mL of 3% thioglycolate medium, and five days later, the mice were sacrificed, and peritoneal macrophages were collected. Animals were treated according to the Guiding Principles (NIH publication #85-23, revised in 1985) for care and use. All experiments performed in this study were approved by the Animal Research Ethics Committee of UFPE (permission No. 0037/2020).
Murine macrophages were cultured in 24-well plates containing sterile 13 mm diameter round coverslips in each well, at a concentration of 1 × 106 cells/mL in RPMI medium (Sigma-Aldrich) supplemented with 10% heat inactivated fetal bovine serum, 100 U/mL penicillin, and 100 µg/mL streptomycin. The culture plates were incubated at 37 °C in a 5% CO2 incubator for 3 h to facilitate cell adhesion. Adhered macrophages were then incubated with fresh medium containing 2 × 106 promastigote forms in stationary growth phase at a ratio of 10 promastigotes to 1 macrophage and incubated at 37 °C in a 5% CO2 incubator for 4 h. The supernatant was subsequently aspirated to remove non-internalized parasites, and the wells were washed with 0.1 M PBS.
Then, the infected macrophages were incubated with MvFL at 22.5, 45 and 90 µg/mL (concentrations non-toxic to cells), or 0.2 μg/mL Amp-B for 48 h. Subsequently, the coverslips were removed and stained using Panoptic fast staining technique (Laborclin, Curitiba, Brazil). The number of infected macrophages (%) and survival index (n) (number of amastigotes recovered per macrophage) were determined by counting the number of parasites in 100 macrophages in a Neubauer chamber. These values were used to calculate the half-maximal inhibitory concentration (IC50) of internalized amastigotes. RPMI containing 0.2% DMSO was used as the negative control. Three independent experiments were performed in triplicate [30].
Evaluation of Macrophage Activation Parameters
Lysosomal activity
Murine macrophages (2 × 105 cells/well) were cultured in 96-well plates and incubated with MvFL (6.25, 12.5, 25, 50, and 100 µg/mL) at 37 °C in a 5% CO2 incubator. After 48 h, 10 μL of 2% neutral red stack solution in DMSO was added to each well and the plates were incubated for 30 min. Next, the supernatant was washed with 0.9% NaCl at 37 °C, and the neutral red trapped in lysosomal vesicles was solubilized by addition of 100 μL of extraction solution (1% [v/v] glacial acetic acid and 50% [v/v] ethanol (v/v) in distilled water). After 30 min at 25 °C on constant agitation, the absorbance was measured on a microplate reader at 550 nm [32].
Phagocytosis Assay
Murine macrophages (2 × 106 cells/well) were incubated with MvFL (6.25, 12.5, 25, 50, or 100 µg/mL) at 37 °C in a 5% CO2 incubator. After 48 h of incubation, 10 µL of neutral red-stained zymosan solution was added per well and the plate was incubated for 30 min at 37 °C. Following incubation, the plates were washed with saline 0.9% (w/v) and 100 μL of Baker's fixative (4% [v/v] formaldehyde, 2% [w/v] sodium chloride, and 1% [w/v] calcium acetate in distilled water) was added to stop phagocytosis of zymosan. Then, 100 μL of extraction solution was added to each well, the plate was incubated for 30 min with constant agitation, and the absorbance was measured on a microplate reader at 550 nm [33].
NO Synthesis
Murine macrophages (2 × 106 cells/well) were plated in a 96-well plate and incubated with MvFL (6.25, 12.5, 25, 50, and 100 µg/mL) in the presence or absence of L. amazonensis promastigote forms (1 × 106 cells/well). After 24 h of incubation at 37 °C in a 5% CO2 incubator, the supernatants were transferred to another 96-well plate for nitrite dosing. A standard curve was prepared with sodium nitrite in RPMI medium at concentrations of 1, 5, 10, 25, 50, 75, 100, and 150 μM. After 24 h of incubation with nitrate, the supernatants were transferred and incubated with equal amount of Griess reagent (Sigma-Aldrich). The absorbance was read on a microplate reader at 550 nm. The results are expressed as the percentage of nitrite production. RPMI medium containing 0.5% DMSO was used as the negative control [34, 35].
Statistical Analyses
All data are presented as the mean ± standard error and all experiments were performed in triplicate. IC50 was calculated with 95% confidence limit using the Probit regression model of SPSS 22.0 software (IBM, Armonk, NY, USA). One-way analysis of variance followed by Tukey’s test was performed using GraphPad Prism 6.0 (GraphPad Software, San Diego, CA, USA) to assess statistical significance. Differences were considered statistically significant at p < 0.05.
Results
Effect of MvFL Against Promastigote Forms of L. amazonensis
M. vacciniifolia frond extract was subjected to chromatography on a Sephadex G-75 column, and MvFL was recovered in the first peak [26] with a specific HA of 12,100. The carbohydrate-binding ability of MvFL was neutralized in the presence of fetuin.
The inhibitory activity of MvFL against promastigote forms of L. amazonensis was also evaluated. Incubation with MvFL for 24 h inhibited the growth of promastigotes in a dose-dependent manner (Fig. 1), and maximum inhibition was observed at 800 µg/mL. After nonlinear regression analysis, at 24 h, an IC50 value at of 88 µg/mL (1.63 µM) was obtained.
Effect of Microgramma vacciniifolia frond lectin (MvFL) on promastigote forms of Leishmania amazonensis after 24 h exposure. The graphs represent the mean ± standard error of mean (SEM) of three independent experiments, considering the control (0.2% DMSO) as 100% viability. One-way ANOVA was used to compare the inhibition observed at different concentrations of MvFL with the control. Different letters (a, b, c and d) indicate significant differences between different concentrations of lectin (p < 0.05)
Hemolytic Activity Assay
The cytotoxic effect of MvFL against mouse and human erythrocytes is shown in Fig. 2. MvFL was found to be safe for mouse and human erythrocytes, owing to its low toxicity against these cells. The maximum hemolytic activity of 200 μg/mL MvFL (the highest concentration evaluated) against mouse erythrocytes was 14.3 ± 0.11%, and 1.66 ± 0.36%, 2.53 ± 0.08%, 1.67 ± 0.08%, and 3.86 ± 0.08% for human erythrocytes isolated from blood types A+, B+, AB+, and O+, respectively.
Cytotoxic effects of MvFL against mouse (A) and human erythrocytes with blood type A + (B), B + (C), AB + (D) and O + (E). Data are expressed as the mean ± SEM of three independent experiments performed in triplicate, considering the control group (1% Triton X-100 in PBS) as 100% hemolysis; (*) p < 0.005 vs control; (**) p < 0.01 vs control; (***) p < 0.001 vs control
Effect of MvFL on Macrophages Infected by L. amazonensis
The effect of treatment with MvFL and the reference drug Amp-B on infected macrophages is shown in Fig. 3. MvFL at concentrations of 22.5, 45, and 90 µg/mL reduced both the number of infected macrophages (Fig. 3A) and internalized amastigotes (Fig. 3B) compared to the negative control. MvFL significant inhibited macrophage infection at 48 h at all three tested concentrations (p < 0.05), with an IC50 of 52 µg/mL. Furthermore, 90 µg/mL MvFL reduced the number of internalized amastigotes by 68.9 ± 0.53%.
Effects of MvFL and reference drug amphotericin B (Amp-B) on infected macrophages (A) and survival index of BALB/c murine macrophages infected with L. amazonensis (B). Cells infected with L. amazonensis were treated with MvFL or Amp-B for 48 h. Data are presented as the mean ± SEM of three independent experiments, considering the control as 100% viability. (***) p < 0.001 vs control
Effect of MvFL on Lysosomal Activity, Phagocytosis, and NO Production in Murine Macrophages
The effect of MvFL on macrophage activation-related parameters, such as lysosomal activity and phagocytic capacity, were assessed based on the retention of neutral red and phagocytosis of neutral red-stained zymosan by murine macrophages. NO production was assessed by nitrite measurement in murine macrophages that were incubated with the sample prior to nitrate treatment. Treatment with 25 µg/mL MvFL significantly (p < 0.05) increased lysosomal activity compared to the control (Fig. 4A). However, MvFL did not affect phagocytic capacity of macrophages at any of the tested concentrations (6.25–100 µg/mL) (Fig. 4B). Additionally, MvFL did not significantly affect NO levels compared to the control, with only a slight reduction in NO levels noted at 6.25 µg/mL (Fig. 5), suggested that MvFL does not directly interfere with nitric oxide synthase (NOS) activity or any other stage of NO synthesis in macrophages.
Effects of MvFL on lysosomal activity (A) and phagocytic capacity (B). Murine peritoneal macrophages were treated at ranging concentrations for 48 h. Lysosomal activity and phagocytic capacity were assessed by quantification of neutral red (NR). Phagocytic capability was determined as the ratio of incorporation of zymosan to NR, solubilized by the extraction solution. (*) p < 0.001 vs control (untreated cells)
Discussion
Parasite resistance and substantial risk of toxicity with drugs used for the treatment of leishmaniasis have increased the need for new antileishmanial drugs [36,37,38]. In recent years, novel bioactive molecules from natural sources that can be obtained in a sustainable manner, are affordable, and have low toxicity, have been the focus of the pharmaceutical industry and researchers [39,40,41]. Several plant species have been reported to be important sources of bioactive compounds that can potentially be used as alternative treatments for various diseases, including leishmaniasis [13, 42, 43]. Among these chemical compounds are lectins, whose specific carbohydrate interactions have been the focus of several studies, mainly in relation to host–pathogen recognition [44], modulation of the host immune system [45], and inhibition of parasitic development [46]. Thus, understanding the nature of these interactions is not only useful for elucidating their biological function, but can also be applied to different areas of research, such as immunology, drug development and delivery, and diagnostics [44].
In the present study, the lectin MvFL, with high HA, was isolated following the protocol described previously. As expected, HA of MvFL was inhibited by fetuin, confirming the presence of lectin molecules with functional carbohydrate-binding sites [26]. Then, we investigated the effect of MvFL on the interaction between L. amazonensis and macrophages. We first evaluated whether MvFL exerts leishmanicidal activity against promastigote forms and observed that MvFL inhibited the growth of promastigote forms at 24 h in a dose-dependent manner. Other natural compounds have also been reported to exert inhibitory effect against promastigote forms of L. amazonensis. Verbascoside, a phenylethanoid glycoside, was reported to have antileishmanial activity and inhibited L. amazonensis promastigotes with an IC50 of 19 μM [47]. Garcinielliptone FC obtained from the seeds of Platonia insignis and bioflavone from the flowers promoted in vitro growth inhibition of promastigotes with IC50 values of 14.06 μM and 47.71 μg/mL, respectively [42, 48].
Promastigotes are the flagellated forms of Leishmania spp., which infect humans through bites of infected sand flies, and are phagocytosed by immune cells, transforming into amastigotes. To prevent infection of host cells by the parasite and subsequent development of leishmaniasis, it is important to inhibit the growth of promastigotes to prevent their proliferation and transformation into intracellular amastigote forms [49, 50].
Lectins have been described in the literature as promising agents against promastigote forms of Leishmania spp. Similarly, a lectin isolated from the venom of Bothrops leucurus (BLL) inhibited L. amazonensis promastigote growth and viability, with an IC50 value of 1.5 µM [20]. Carneiro et al. [21] reported that Parkia pendula lectin (PpeL) significantly inhibited the growth of Leishmania infantum promastigotes with an IC50 value of 4.9 ± 0.05 μM at 48 h, through its carbohydrate recognition domain, suggesting an interaction between PpeL and glycans from L. infantum. Sousa et al. [51] reported that a galectin isolated from the marine sponge Chondrilla caribensis exerted a leishmanicidal effect on L. infantum promastigote forms with an IC50 value of 1.2 ± 0.094 μM at 24 h through its interaction with parasite glycans.
The indiscriminate use of medicinal plants to prevent or cure diseases can cause cytotoxic and genotoxic changes that can potentially lead to the development of other pathologies. Therefore, it is important to understand the action of natural products at the cellular level to ensure their safety and to support further research [52, 53]. In vitro toxicological assays, such as hemolytic activity, are preliminary tests that are especially useful in cytotoxicity assessment of compounds to choose a safe concentration range for use in later stages of drug development [34, 54]. Our study showed that MvFL did not cause significant hemolysis of mouse erythrocytes or human erythrocytes derived from different blood types, suggesting that this lectin can be evaluated in animal models at the concentrations assessed in the present study.
Given the observed inhibitory activity of MvFL on promastigote proliferation, we investigated whether it could also reduce the percentage of macrophages infected by L. amazonensis. Experimental models using macrophages infected with amastigotes of Leishmania are used because these forms in the parasite life cycle are associated with the clinical manifestations of leishmaniasis [48, 55]. Furthermore, models with the intracellular form provide the most efficient method for correlating the in vitro activity of a drug with its effectiveness in an in vitro assay [56]. Based on the results of our experiments, MvFL is an inhibitor of promastigote growth and reduces the number of amastigotes internalized by macrophages.
Afonso-Cardoso et al. [57] evaluated the effect of latex lectin of Synadenium carinatum (ScLL) (100, 50, and 10 µg/mL) against infection of peritoneal macrophages of BALB/c mice by L. amazonensis in vitro, and noted infection rates of 55%, 65%, and 45%, respectively, compared to the control (100% infected cells). Aranda-Souza et al. [20] also analyzed the effect of BLL lectin against macrophages infected with L. amazonensis and Leishmania braziliensis amastigotes and reported that the infection rate in cells treated with 1.6 μM BLL was 28.5 ± 7.91% and 35 ± 8.83% for L. amazonensis and L. braziliensis, respectively.
Afonso-Cardoso et al. [58] analyzed whether association of ScLL with the soluble antigen of L. amazonensis would immunize BALB/c mice against promastigote forms of L. amazonensis. They observed that ScLL (100 µg/animal) promoted a 61.7% reduction in the parasite load inside macrophages compared to the control group, suggesting that the underlying mechanism responsible for the observed protection required further investigation. ArtinM, a lectin isolated from the seeds of Artocarpus heterophyllus, binds to D-mannose and has immunomodulatory properties due to its interaction with N-glycans of immune cells. ArtinM was reported to induce infected human neutrophils infected with Leishmania major promastigotes and reduced parasite viability by 50% when compared to untreated neutrophils [59].
In the present study, MvFL significantly reduced the number of intracellular amastigotes, in addition to reducing infection; however, the underlying mechanism is not clear as it could be due to direct effect on the parasite or activation of macrophage defense mechanisms. Macrophages play a vital role in modulating the immune response against Leishmania parasites through cytokine production and phagocytosis to destroy pathogens or repair lesions associated with inflammation [60]. Macrophages are activated on contact with parasites, which triggers changes in lysosomal activity, phagocytic capacity, and NO production [61]. To understand the mechanism underlying the decrease in the survival rate of intramacrophage amastigotes, the effect of MvFL on parameters associated with macrophage immune response were analyzed to determine whether changes in these parameters stimulated inhibition of parasites.
Phagocytosis and the lysosomal system are essential components that mediate the functions of activated macrophages in innate immune responses through antigen internalization and degradation. In macrophages, parasites are restricted to phagosomes, which fuse with lysosomes to form the parasitic vacuole, an inhospitable compartment with acid hydrolases, reactive oxygen, and NO species, which participate in pathogen degradation [62, 63]. However, our results suggest that the effect of MvFL on the number of amastigotes is not due to an effect of MvFL on phagocytic action; therefore, the observed effect of the lectin could be due to direct action on the parasite or inhibition of infection by promastigotes.
Like the findings of the present study, Afonso-Cardoso et al. [57] observed that ScLL did not induce NO production, suggesting that a NO-independent pathway engages in the decrease of the number of intracellular L. amazonensis. Thomazelli et al. [64] reported that concanavalin A lectin (Con-A) increased the phagocytic capacity of immune cells and promoted L. amazonensis elimination. Pretreatment with Con-A increased the synthesis of reactive oxygen species as well as the expression of iNOS enzyme, but did not affect NO production, perhaps because even though Con-A treatment induced production of pro-inflammatory cytokines, it also promoted the synthesis of anti-inflammatory cytokines. Our results suggest that the leishmanicidal activity of MvFL against promastigote and amastigote forms of L. amazonensis may be related to its proinflammatory potential, as previously described by Patriota et al. [26].
The findings of the present study showed that MvRL, a lectin isolated from the frond of M. vacciniifolia exerts significant in vitro antileishmanial activity against L. amazonensis promastigote replication and macrophage infection. This study also demonstrated that MvFL promoted the activation of macrophages by increasing lysosomal activity but did not affect NO production and phagocytosis. Our study paves the way for further studies to elucidate the immunological mechanisms involved in the leishmanicidal effects of MvFL as well as investigating its effect in in vivo immunization models for leishmaniasis.
Data availability
All data generated or analysed during this study are included in this published article.
References
Pan American Health Organization (2022) Leishmaniasis. Available at: https://www.paho.org/en/topics/leishmaniasis. Accessed 29 Sept 2022
Herrera G, Barragán N, Luna N, Martínez D, De Martino F, Medina J, Niño S, Páez L, Ramírez A, Veja L, Velandia V, Vera M, Zúñiga MF, Bottin MJ, Ramírez JD (2020) An interactive database of Leishmania species distribution in the Americas. Sci Data 7:110. https://doi.org/10.6084/m9.figshare.11993970
Franssen SU, Durrant C, Stark O, Moser B, Downing T, Imamura H et al (2020) Global genome diversity of the Leishmania donovani complex. Elife 9:e51243. https://doi.org/10.7554/eLife.51243
Mitropoulos P, Konidas P, Durkin-Konidas M (2010) New World cutaneous leishmaniasis: updated review of current and future diagnosis and treatment. J Am Acad Dermatol 63:309–322. https://doi.org/10.1016/j.jaad.2009.06.088
World Health Organization (2019) Fact sheet: Leishmaniasis. Available online at. https://www.who.int/leishmaniasis/burden/en/. Accessed 29 Sep 2022
Barroso DH, Falcão SDAC, Motta JDOCD, Santos LS, Takano GHS, Gomes CM, Favali CBF, Lima BD, Sampaio RNR (2018) pD-L1 may mediate T-cell exhaustion in a case of early diffuse leishmaniasis caused by Leishmania (L) amazonensis. Front Immunol 11:1021. https://doi.org/10.3389/fimmu.2018.01021
Christensen SM, Belew AT, El-Sayed NM, Tafuri WL, Silveira FT, Mosser DM (2019) Host and parasite responses in human diffuse cutaneous leishmaniasis caused by L. amazonensis. PLoS Negl Tropl Dis 13:e0007152. https://doi.org/10.1371/journal.pntd.0007152
Araujo PSS, Oliveira SSC, d’Avila-Levy CM, Santos ALS, Branquinha MH (2018) Susceptibility of promastigotes and intracellular amastigotes from distinct Leishmania species to the calpain inhibitor MDL28170. Parasitol Res 117:2085–2094. https://doi.org/10.1007/s00436-018-5894-7
Morais TR, Conserva GAA, Varela MT, Costa-Silva TA, Thevenard F, Ponci V, Fortuna A, Falcão AC, Tempone AG, Fernandes JPS, Lago JHG (2020) Improving the drug-likeness of inspiring natural products—evaluation of the antiparasitic activity against Trypanosoma cruzi through semi-synthetic and simplified analogues of licarin A. Sci Rep 10:5467. https://doi.org/10.1038/s41598-020-62352-w
Croft SL, Olliaro P (2011) Leishmaniasis chemotherapy-challenges and opportunities. Clin Microbiol Infect 17:1478–1483. https://doi.org/10.1111/j.1469-0691.2011.03630.x
Uliana SRV, Trinconi CT, Coelho AC (2016) Chemotherapy of leishmaniasis: present challengs. Parasitology 145:464–480. https://doi.org/10.1017/S0031182016002523
SILVA, AB (2019) Distribuição dos casos de leishmaniose visceral e possíveis fatores que influenciam na sua ocorrência no Estado da Paraíba, Brasil
Brito LM, Alves MMM, Souza AC, Carvalho TP, Campos JHF, Monção NBN, Citó AMGL, Arcanjo DDR, Carvalho FAA (2021) Selective in vitro antileishmanial activity of Mimosa caesalpiniifolia stem barks and its main constituent betulinic acid against Leishmania amazonensis. S Afr J Bot 140:68–75. https://doi.org/10.1016/j.sajb.2021.03.028
Maciel MSP, Reis AS, Fidelis QC (2022) Antileishmanial potential of species from the family Lamiaceae: chemical and biological aspects of non-volatile compounds. Acta Trop 228:106309. https://doi.org/10.1016/j.actatropica.2022.106309
Naithani S, Komath SS, Nonomura A, Govindjee G (2021) Plant lectins and their many roles: carbohydrate-binding and beyond. J Plant Physiol 266:153531. https://doi.org/10.1016/j.jplph.2021.153531
Moura MC, Procópio TF, Ferreira GRS, Alves RRV, Sá RA, Paiva PMG, Ingmer H, Coelho LCBB, Napoleão TH (2021) Anti-staphylococcal effects of Myracrodruon urundeuva lectins on nonresistant and multidrug resistant isolates. J Appl Microbiol 130:745–754. https://doi.org/10.1111/jam.14811
Oladokun BO, Omisore ON, Osukoya OA, Kuku A (2019) Anti-nociceptive and anti-inflammatory activities of Tetracarpidium conophorum seed lectin. Sci Afr 3:e00073. https://doi.org/10.1016/j.sciaf.2019.e00073
Patriota LLS, Ramos DBM, Silva YA, Santos ACLA, Araújo MTMF, Brito JS, Torres DJL, Oliveira AM, Silva DCN, Lorena VMB, Paiva PMG, Mendes RL, Napoleão TH (2021) Microgramma vacciniifolia frond lectin (MvFL) exhibits antitumor activity against sarcoma 180 in mice. Phytomedicine Plus 1:100013. https://doi.org/10.1016/j.phyplu.2020.100013
Santos AJCA, Barros BRS, Aguiar LMS, Patriota LLS, Lima TA, Zingali RB, Paiva PMG, Napoleão TH, Melo CML, Pontual EV (2020) Schinus terebinthifolia leaf lectin (SteLL) is an immunomodulatory agent by altering cytokine release by mice splenocytes. 3 Biotech 10:144. https://doi.org/10.1007/s13205-020-2137-2
Aranda-Souza MA, Lorena VMB, Correia MTS, Figueiredo RCBQ (2018) In vitro effect of Bothrops leucurus lectin (BLL) against Leishmania amazonensis and Leishmania braziliensis infection. Int J Biol Macromol 120:431–439. https://doi.org/10.1016/j.ijbiomac.2018.08.064
Carneiro RF, Aguiar ES, Santos VF, Santos ALE, Santos MHC, Roma RR, Silva RRS, Leal MLMB, Silva LT, Rocha BAM, Silva CGL, Nagano CS, Sampaio AH, Souza ROS, Teixeira CS (2021) Elucidation of the primary structure and molecular modeling of Parkia pendula lectin and in vitro evaluation of the leishmanicidal activity. Process Biochem 101:1–10. https://doi.org/10.1016/j.procbio.2020.11.004
De Schutter K, Van Damme EJM (2015) Protein-carbohydrate interactions as part of plant defense and animal immunity. Molecules 20:9029–9053. https://doi.org/10.3390/molecules20059029
Agra MF, Silva KN, Basílio IJLD, Freitas PF, Barbosa-Filho JM (2008) Survey of medicinal plants used in the region Northeast of Brazil. Rev Bras Farmacogn 18:472–508. https://doi.org/10.1590/S0102-695X2008000300023
Peres MTLP, Simionatto E, Hess SC, Bonani VFL, Candido ACS, Castelli C, Poppi NR, Honda NK, Cardoso CAL, Faccenda O (2009) Estudos químicos e biológicos de Microgramma vacciniifolia (Langsd. & Fisch.) Copel (Polypodiaceae). Quím Nova 32:897–901. https://doi.org/10.1590/S0100-40422009000400013
Santana GMS, Albuquerque LP, Napoleão TH, Souza SR, Coelho LCBB, Paiva PMG (2012) Electrochemical potential of Microgramma vaccinifolia rhizome lectin. Bioelectrochemistry 85:56–60. https://doi.org/10.1016/j.bioelechem.2011.11.006
Patriota LLS, Procópio TF, Brito JS, Sebag V, Oliveira APS, Soares AKA, Moreira LR, Lima TA, Soares T, Silva TD, Paiva PMG, Lorena VMB, Melo CML, Albuquerque LP, Napoleão TH (2017) Microgramma vacciniifolia (Polypodiaceae) fronds contain a multifunctional lectin with immunomodulatory properties on human cells. Int J of Biol Macromol 103:36–46. https://doi.org/10.1016/j.ijbiomac.2017.05.037
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Bing DH, Weyand JGM, Stavitsky AB (1967) Hemagglutination with aldehyde-fixed erythrocytes for assay of antigens and antibodies. Proc Soc Exp Biol Med 124:1166–1170. https://doi.org/10.3181/00379727-124-31953
Valadares DG, Duarte MC, Oliveira JS, Chávez-Fumagalli MA, Martins V, Costa LE, Leite JPV, Santoro MM, Régis WCB, Tavares CAP, Coelho EAP (2011) Leishmanicidal activity of the Agaricus blazei Murill in different Leishmania species. Parasitol Int 60:357–363. https://doi.org/10.1016/j.parint.2011.06.001
Carneiro SM, Carvalho FA, Santana LC, Sousa AP, Neto JM, Chaves MH (2012) The cytotoxic and antileishmanial activity of extracts and fractions of leaves and fruits of Azadirachta indica (A Juss.). Biol Res 45:111–116. https://doi.org/10.4067/S0716-97602012000200002
Pita JCLLR, Xavier AL, Sousa TKG, Mangueira VM, Tavares JF, Júnior RJO, Veras RC, Pessoa HLF, Silva MS, Morelli S, Ávila VMR, Silva TG, Diniz MFFM, Castello-Branco MVS (2012) In vitro and in vivo antitumor effect of trachylobane-360, a diterpene from Xylopia langsdorffiana. Molecules 17:9573–9589. https://doi.org/10.3390/molecules17089573
Bonatto SJR, Folador A, Aikawa J, Yamazaki RK, Pizatto N, Oliveira HHP, Vecchi R, Curi R, Calder PC, Fernandes LC (2004) Lifelong exposure to dietary fish oil alters macrophage responses in Walker 256 tumor-bearing rats. Cell Immunol 231:56–62. https://doi.org/10.1016/j.cellimm.2004.12.001
Grando FCC, Felicio CA, Twardowschy A, Paula FM, Batista VG, Fernandes LC, Curi R, Nishiyama A (2009) Modulation of peritoneal macrophages activity by the saturation state of the fatty acid moiety of phosphatidyl choline. Braz J Med Biol Res 42:599–605. https://doi.org/10.1590/S0100-879X2009005000003
Lustosa AKMF, Arcanjo DDR, Ribeiro RG, Rodrigues KAF, Passos FFB, Piauilino CA, Silva-Filho JC, Araújo BQ, Lima-Neto JS, Costa-Júnior JS, Carvalho FAA, Citó AMGL (2016) Immunomodulatory and toxicological evaluation of the fruit seeds from Platonia insignis, a native species from Brazilian Amazon Rainforest. Rev Bras de Farmacogn 26:77–82. https://doi.org/10.1016/j.bjp.2015.05.014
Alves MMDM, Brito LM, Souza AC, Queiroz BCSH, Carvalho TP, Batista JF, Oliveira JSDSM, Mendonça IL, Lira SRDS, Chaves MH, Gonçalves JCR, Carneiro SMP, Arcanjo DDR, Carvalho FADA (2017) Gallic and ellagic acids: two natural immunomodulator compounds solve infection of macrophages by Leishmania major. Naunyn Schmiedeberg’s Arch Pharmacol 390:893–903. https://doi.org/10.1007/s00210-017-1387-y
Silva BJM, Silva RRP, Rodrigues APD, Farias LHS, Nascimento JLM, Silva EO (2016) Physalis angulata induces death of promastigotes and amastigotes of Leishmania (Leishmania) amazonensis via the generation of reactive oxygen species. Micron 82:25–32. https://doi.org/10.1016/j.micron.2015.12.001
Sundar S, Chakravarty J, Meena LP (2019) Leishmaniasis: treatment, drug resistance and emerging therapies. Exp Opin Orphan Drugs 7:1–10. https://doi.org/10.1080/21678707.2019.1552853
Horácio ECA, Hickson J, Murta SMF, Ruiz JC, Nahum LA (2021) Perspectives from systems biology to improve knowledge of Leishmania drug resistance. Front Cell Infect Microbiol 11:351. https://doi.org/10.3389/fcimb.2021.653670
Nirmala C, Bisht MS, Bajwa HK, Santosh O (2018) Bamboo: a rich source of natural antioxidants and its applications in the food and pharmaceutical industry. Trends Food Sci Technol 77:91–99. https://doi.org/10.1016/j.tifs.2018.05.003
Sharma K, Kaushik G, Thotakura N, Raza K, Sharma N, Nimesh S (2020) Enhancement effects of process optimization technique while elucidating the degradation pathways of drugs present in pharmaceutical industry wastewater using Micrococcus yunnanensis. Chemosphere 238:124689. https://doi.org/10.1016/j.chemosphere.2019.124689
Akdeniz M, Yener I, Yilmaz MA, Kandemir SI, Tekin F, Ertas A (2021) A potential species for cosmetic and pharmaceutical industries: Insight to chemical and biological investigation of naturally grown and cultivated Salvia multicaulis Vahl. Ind Crops Prod 168:113566. https://doi.org/10.1016/j.indcrop.2021.113566
Bezerra EA, Alves MMM, Lima SKR, Pinheiro EEA, Amorim LV, Neto JSL, Carvalho FAA, Citó AMGL, Arcanjo DDR (2021) Biflavones from Platonia insignis Mart. flowers promote in vitro antileishmanial and immunomodulatory effects against internalized amastigote forms of Leishmania amazonensis. Pathogens 10:1166. https://doi.org/10.3390/pathogens10091166
Houël E, Ginouves M, Azas N, Bourreau E, Eparvier V, Hutter S, Knittel-Obrecht A, Jahn-Oyac A, Prévot G, Villa P, Vonthron-Sénécheau C, Odonne G (2022) Treating leishmaniasis in Amazonia, part 2: multi-target evaluation of widely used plants to understand medicinal practices. J Ethnopharmacol 289:115054. https://doi.org/10.1016/j.jep.2022.115054
Mishra A, Behura A, Mawatwal S, Kumar A, Naik L, Mohanty SS, Manna D, Dokania P, Mishra A, Patra SK, Dhiman R (2019) Structure-function and application of plant lectins in disease biology and immunity. Food Chem Toxicol 134:110827. https://doi.org/10.1016/j.fct.2019.110827
Gupta B, Sadaria D, Warrier VU, Kirtonia A, Kant R, Awasthi A, Baligar P, Pal K, Yuba E, Sethi G, Garg M, Gupta RK (2022) Plant lectins and their usage in preparing targeted nanovaccines for cancer immunotherapy. Semin Cancer Biol 80:87–106. https://doi.org/10.1016/j.semcancer.2020.02.005
Ríos-de Álvarez L, Jackson F, Greer A, Bartley Y, Bartley DJ, Grant G, Huntley JF (2012) In vitro screening of plant lectins and tropical plant extracts for anthelmintic properties. Vet Parasitol 186:390–398. https://doi.org/10.1016/j.vetpar.2011.11.004
Maquiaveli CC, Lucon-Jpunior JF, Brogi S, Campiani G, Gemma S, Vieira PC, Silva ER (2016) Verbascoside inhibits promastigote growth and arginase activity of Leishmania amazonensis. J Nat Prod 79:1459–1463. https://doi.org/10.1021/acs.jnatprod.5b00875
Bezerra EA, Alves MMM, Amorim LV, Carvalho RCV, Cruz LPL, Costa-Júnior JS, Oliveira MDA, Neto JSL, Carvalho FAA, Citó AMGL, Arcanjo DDR (2020) Garcinielliptone FC: selective anti-amastigote and immunomodulatory effects on macrophages infected by Leishmania amazonensis. Toxicol in Vitro 63:104750. https://doi.org/10.1016/j.tiv.2019.104750
Sunter J, Gull K (2017) Shape, form, function and Leishmania pathogenicity: from textbook descriptions to biological understanding. Open Biol 7:170165. https://doi.org/10.1098/rsob.170165
Bates PA (2018) Revising Leishmania’s life cycle. Nat Microbiol 3:529–530. https://doi.org/10.1038/s41564-018-0154-2
Sousa ARO, Andrade FRN, Chaves RP, Sousa BL, Lima DB, Souza ROS, Silva CGL, Teixeira CS, Sampaio AH, Nagano CS, Carneiro RF (2021) Structural characterization of a galectin isolated from the marine sponge Chondrilla caribensis with leishmanicidal potential. Biochim Biophys Acta Gen Subj 1865:129992. https://doi.org/10.1016/j.bbagen.2021.129992
Madić V, Stojanović-Radić Z, Jušković M, Jugović D, Popović AZ, Vasiljević P (2019) Genotoxic and antigenotoxic potential of herbal mixture and five medicinal plants used in ethnopharmacology. S Afr J Bot 125:290–297. https://doi.org/10.1016/j.sajb.2019.07.043
Agudelo IJ, Lampropulos VES, Cogoi L, Filip R, Wagner ML, Teves S, Carballo MA, Ricco RA, Nigro MML (2021) Genotoxic evaluation of the infusion of Baccharis spicata (Lam.) Baill (Asteraceae), a substitute of the medicinal plant known as “carqueja” in Argentina. Phytomed Plus 1:100137. https://doi.org/10.1016/j.phyplu.2021.100137
Brandão-Costa RM, Nascimento TP, Bezerra RP, Porto ALF (2020) FDS, a novel saponin isolated from Felicium decipiens: lectin interaction and biological complementary activities. Process Biochem 88:159–169. https://doi.org/10.1016/j.procbio.2019.10.018
Bagirova M, Dinparvar S, Allahverdiyev AM, Unal K, Abamor ES, Novruzova M (2020) Investigation of antileshmanial activities of Cuminum cyminum based green silver nanoparticles on L. tropica promastigotes and amastigotes in vitro. Acta Trop 208:105498. https://doi.org/10.1016/j.actatropica.2020.105498
Assolini JP, Silva TP, Bortoleti BTS, Gonçalves MD, Tomioto-Pellisier F, Sahd CS, Carloto ACM, Feuser PE, Cordeiro AP, Sayer C, Araújo PPH, Costa IN, Conchon-Costa I, Miranda-Sapla MM, Pavanelli WR (2020) 4-nitrochalcone exerts leishmanicidal effect on L. amazonensis promastigotes and intracellular amastigotes, and the 4-nitrochalcone encapsulation in beeswax copaiba oil nanoparticles reduces macrophages cytotoxicity. Eur J Pharmacol 884:173392. https://doi.org/10.1016/j.ejphar.2020.173392
Afonso-Cardoso SR, Silva CV, Ferreira MS, Souza MA (2011) Effect of the Synadenium carinatum latex lectin (ScLL) on Leishmania (Leishmania) amazonensis infection in murine macrophages. Exp Parasitol 128:61–67. https://doi.org/10.1016/j.exppara.2011.02.006
Afonso-Cardoso SR, Rodrigues FH, Gomes MA, Silva AG, Rocha A, Guimarães AH, Candeloro I, Favoreto S Jr, Ferreira MS, Souza MA (2007) Protective effect of lectin from Synadenium carinatum on Leishmania amazonensis infection in BALB/c mice. Korean J Parasitol 45:255–266. https://doi.org/10.3347/kjp.2007.45.4.255
Ricci-Azevedo R, Oliveira AF, Conrado MC, Carvalho FC, Roque-Barreira MC (2016) Neutrophils contribute to the protection conferred by ArtinM against intracellular pathogens: a study on Leishmania major. PLoS Negl Trop Dis 10:e0004609. https://doi.org/10.1371/journal.pntd.0004609
Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili S-A, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A (2018) Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol 233:6424–6440. https://doi.org/10.1002/jcp.26429
Majumder N, Ganguly S, Ghosh AK, Kundu S, Banerjee A, Saha S (2020) Chlorogenic acid acts upon Leishmania donovani arresting cell cycle and modulating cytokines and nitric oxide in vitro. Parasite Immunol 42:e12719. https://doi.org/10.1111/pim.12719
Krishnatry AS, Brazeau DA, Fung HL (2010) Broad regulation of matrix and adhesion molecules in THP-1 human macrophages by nitroglycerin. Nitric Oxide 22:11–17. https://doi.org/10.1016/j.niox.2009.10.004
Reza S, Hasan NA, Maryam NF, Fahimeh B, Ghahremani A, GholamReza HG, Amin HM (2019) Cytokine profile and nitric oxide levels in macrophages exposed to Leishmania infantum FML. Exp Parasitol 203:1–7. https://doi.org/10.1016/j.exppara.2019.05.004
Thomazelli APFDS, Tomiotto-Pellissier F, Miranda-Sapla MM, Silva SS, Alvarenga DS, Panis C, Cataneo AHD, Bordigno J, Silveira GF, Yamauchi LM, Sá JPSR, Felipe I, Pavanelli WR, Conchon-Costa I (2018) Concanavalin—a displays leishmanicidal activity by inducing ROS production in human peripheral blood mononuclear cells. Immunopharmacol Immunotoxicol 40:387–392. https://doi.org/10.1080/08923973.2018.1510960
Acknowledgements
The authors thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for research grants (407192/2018-2) and fellowships (PMGP and THN), and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Finance Code 001) and Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco (FACEPE) for financial support (APQ-0108-2.08/14, APQ-0661-2.08/15). LMSA thanks CAPES for a graduate scholarship.
Funding
Conselho Nacional de Desenvolvimento Científico e Tecnológico, 407192/2018-2, Thiago Henrique Napoleão, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Finance Code 001, Thiago Henrique Napoleão, Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco, APQ-0108-2.08/14, Thiago Henrique Napoleão, APQ-0661-2.08/15, Patricia Paiva.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Souza Aguiar, L.M., de Moraes Alves, M.M., Sobrinho Júnior, E.P.C. et al. Microgramma vacciniifolia Frond Lectin: In Vitro Anti-leishmanial Activity and Immunomodulatory Effects Against Internalized Amastigote Forms of Leishmania amazonensis. Acta Parasit. 68, 869–879 (2023). https://doi.org/10.1007/s11686-023-00717-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11686-023-00717-7