Abstract
Summary
Five-year fracture risk prediction from the Fracture Risk Brussels Epidemiological Enquiry (FRISBEE) models was externally tested in 9716 Canadian women and demonstrated good discrimination but consistently overestimated risk.
Introduction
Five-year risk prediction models for all fractures, major osteoporotic fractures (MOFs) and central fractures (proximal to forearm and ankle) from the FRISBEE cohort demonstrated good performance in the original derivation cohort. Our aim was to externally validate the FRISBEE-based 5-year prediction models in routine practice.
Methods
Using the population-based Manitoba Bone Mineral Density (BMD) registry, we identified women aged 60–85 years undergoing baseline BMD assessment from September 1, 2012 to March 31, 2018. Five-year probabilities of all fractures, MOFs and central fractures were calculated using the FRISBEE prediction models. We identified incident non-traumatic fractures up to 5 years from population-based healthcare data sources. Performance characteristics included area under the receiver operating characteristic curve (AUROC), gradient of risk (hazard ratio [HR] per SD increase and across risk tertiles) from Cox regression analysis, and calibration (ratio 5-year observed cumulative incidence to predicted fracture probability).
Results
We included 9716 women (mean age 70.7 + / − SD 5.3 years). During a mean observation time of 2.5 years, all fractures, MOFs and central fractures were identified in 377 (3.9%), 264 (2.7%) and 259 (2.7%) of the women. AUROC showed significant fracture risk stratification with the FRISBEE models (all fractures 0.69 [95%CI 0.67–0.72], MOFs 0.71 [95%CI 0.68–0.74], central fractures 0.72 [95%CI 0.69–0.75]). There was a strong gradient of risk for predicting fracture outcomes per SD increase (HRs from 1.98 to 2.26) and across risk tertiles (HRs for middle vs lowest from 2.25 to 2.41, HRs for highest vs lowest from 4.70 to 6.50). However, risk was overestimated for all fractures (calibration-in-the-large 0.63, calibration slope 0.63), MOF (calibration-in-the-large 0.51, calibration slope 0.57) and central fractures (calibration-in-the-large 0.55, calibration slope 0.60).
Conclusions
FRISBEE 5-year prediction models were externally validated to stratify fracture risk similar to the derivation cohort, but would need recalibration for Canada as risk was overestimated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by decreased bone strength and increased fracture risk resulting from low bone mass and deterioration of bone microarchitecture [1]. Sequelae of osteoporosis-related fractures result in significant individual-level health and quality of life-related impairment, and represent a significant system-level financial burden [2].
Low bone mineral density has been associated with an increased risk of osteoporotic fractures; however, algorithms combining clinical risk factors (CRFs) and bone mineral density (BMD) may estimate individual-level fracture risk more accurately, and guide the identification of high-risk individuals who may benefit most from treatment [3]. Prior fractures, falls, advanced age, bone loss, smoking and high alcohol intake represent some of the CRFs that have been associated with increased fracture risk [4, 5]. Individualized estimation of absolute fracture risk to guide decision-making regarding treatment initiation is recommended internationally.
The Fracture Risk Brussels Epidemiological Enquiry (FRISBEE) study is an ongoing population-based cohort study involving 3560 post-menopausal women aged 60 to 85 years from Brussels, Belgium, recruited between July 2007 and June 2013. Three models for fracture risk prediction were recently developed using data from the FRISBEE study: one, for major osteoporotic fracture (MOF) prediction (similar to FRAX); two, for all fracture prediction (similar to the Garvan FRC); and three, for central fracture prediction. Models were developed using a sub-distribution regression method, accounting for competing risk of mortality. In addition to total hip BMD and spine BMD, the MOF prediction model retained three CRFs from FRAX (age, history of fracture, high alcohol intake), and the all fracture prediction model retained all Garvan FRC CRFs (age, total hip BMD, history of fracture, history of recent fall). Central fractures have been associated with higher fracture risk relative to MOFs [6, 7]; the original prediction model that was developed included five CRFs (age, total hip BMD, history of fracture, spine BMD, rheumatoid arthritis). All three nomograms demonstrated good discrimination with AUROCs of 0.72 to 0.73, well-performing calibration curves, and concordance analyses showing moderate to good reliability when compared against FRAX and the Garvan FRC [8].
No prior studies have externally validated the three FRISBEE-based prediction models. The FRISBEE cohort was limited to post-menopausal women and recruited participants exclusively from Brussels; validation in other population-based samples internationally is warranted [8]. To further assess the generalizability of FRISBEE prediction models and their performance in the clinical setting, we examined their predictive performance in a large clinical registry from Manitoba, Canada.
Methods
Study design and population
We conducted a retrospective analysis using the Manitoba Bone Mineral Density (BMD) registry. The database is a well-validated province-wide integrated repository of all dual-energy X-ray absorptiometry-bone mineral density (DXA-BMD) scans since 1997, and facilitates anonymized patient-level record linkage with other population-level computerized healthcare data.
We identified all women aged 60 to 85 years with DXA-BMD scans completed from September 1, 2012 (date when the intake questionnaire included self-reported frequency of falls in the prior 12 months) to March 31, 2018. Women were excluded if they were not registered for health care in Manitoba or had missing baseline measurements required for the FRISBEE prediction models. For those with more than one qualifying examination, only the first was included. The study was approved by the Health Research Ethics Board for the University of Manitoba.
Fracture risk prediction calculation
Five-year probabilities of all fractures, MOFs and central fractures were calculated using the FRISBEE prediction models [8]. Hip and lumbar spine DXA scans were performed and analysed in accordance with manufacturer recommendations (Lunar iDXA, GE HealthCare); total hip and lumbar spine BMD measurements were converted to equivalent Hologic units using previously published formulae for fan-beam DXA systems [9]. Height and weight were recorded at the time of the BMD test.
All included women received an intake questionnaire by mail approximately two to 4 weeks prior to their BMD appointment. Self-reported history of falls in the prior year, alcohol use (3 or more per day designated as high alcohol intake), and diagnosis of rheumatoid arthritis were collected. All data were reviewed for completeness and accuracy by the BMD technologist at the time of BMD testing and by the physician at the time of BMD reporting; there were no missing data. History of prior fractures without major trauma and other comorbidities (hyperthyroidism, ankylosing spondylitis, celiac disease, chronic liver disease, inflammatory bowel disease, cerebrovascular disease, multiple sclerosis, muscular dystrophy, chronic pancreatitis, Parkinson disease, aromatase inhibitor use, solid organ transplantation) was obtained from linkage with population-based healthcare data (hospital discharge abstracts and medical claims diagnoses since 1984), as previously described [10,11,12].
Fractures outcome definition
Provincial population-based health records were assessed for the presence of fracture diagnostic codes following the BMD assessment, up to March 31, 2018. Fractures that were not associated with trauma codes were assessed through a combination of hospital discharge abstracts (diagnoses and procedures coded using the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] prior to 2004 and International Classification of Diseases, Tenth Revision, Canadian Enhancements [ICD-10-CA] thereafter) and physician billing claims (coded using ICD-9-CM). We previously validated these data sources for fracture detection compared with x-ray review; diagnostic algorithms were tested and adopted for national osteoporosis surveillance [13,14,15].
For the current analysis, we identified incident non-traumatic fractures, MOFs, and central fractures. Incident fractures were defined as fractures that occurred after the index BMD measurement with site-specific fracture codes, derived from hospitalizations or physician visits. All fractures were defined as any fracture (excluding craniofacial, hand and foot). MOFs were defined as clinical fractures involving the vertebrae, hip, distal forearm, and humerus. Central fractures were defined as fractures occurring proximal to the forearm and ankle, and included clinical fractures of vertebrae, hip, humerus, pelvis, ribs, scapula, clavicles, and sternum [16].
To minimize potential misclassification of prior fractures as incident fractures, we conservatively required that there be no hospitalization or physician visits with the same fracture type in the 6 months preceding an incident fracture diagnosis.
Statistical analysis
Descriptive statistics for demographic and baseline characteristics are presented as mean ± standard deviation (SD) for continuous variables, and frequency (%) for categorical variables, unless otherwise stated. The primary analysis examined the performance characteristics of the FRISBEE predictive models in stratifying incident fracture, MOF and central fracture risk [8], using area under the receiver operating characteristic curve (AUROC). Cox proportional hazards regression models for incident fractures were used to estimate gradient of risk as hazard ratios (HR) with 95% confidence intervals (CI) for each SD increase in risk (log-transformed due to a skewed distribution) and across tertiles of fracture risk (referent was lowest risk). The proportional hazards assumption was confirmed by testing log-scaled Schoenfeld residuals (all p > 0.2). Ratios of 5-year observed versus predicted all fractures, MOFs and central fractures were used to assess calibration overall (calibration-in-the-large) and for risk tertiles (calibration slope), where unity indicates perfect calibration. Observed risk was estimated from the cumulative incidence function and included the effect of competing mortality [17]. Statistical analyses were performed with Statistica (Version 13.0, StatSoft Inc, Tulsa, OK, USA) and AUROCs were generated using IBM SPSS for Windows (version 27, IBM Corporation).
Results
The Manitoba registry cohort included a total of 10,592 women aged 60 to 85 years with baseline DXA-BMDs conducted between September 1, 2012 and March 31 2018. Of this cohort, 138 women were excluded as non-Manitoba residents, and 738 were excluded because total hip and lumbar spine BMD data was not available. The final analysis therefore included 9716 women. Of this cohort, 9265 (95.4%) women were alive at final follow-up; 339 (3.5%) had died, and 112 (1.2%) had moved.
Mean age was 70.7 (SD 5.3) years. A minority of participating individuals had self-reported previous fractures (21.7%), recent falls (19.3%), high alcohol use (0.3%), rheumatoid arthritis (4.0%) and other comorbidities (14.1%) (Table 1). Mean 5-year risks of all fractures, MOFs and central fractures based on FRISBEE prediction models were 12.5% (SD 7.2), 9.5% (SD 6.9) and 9.2% (SD 7.5), respectively.
During a mean follow-up period of 2.5 (SD 1.6) years, 377 (3.9%) individuals sustained fractures, 264 (2.7%) sustained MOFs, and 259 (2.7%) sustained central fractures. Pairwise comparisons for individual FRISBEE prediction model components and their association with incident fractures, MOFs and central fractures are presented in Table 2. Hip and lumbar spine BMD, age, and history of previous fractures and previous falls were associated with increased risks of all fractures, MOFs and central fractures (p < 0.001); high alcohol use, rheumatoid arthritis and other comorbidities were not significantly associated (p > 0.05). Mean FRISBEE risk predictions were significantly higher in those with versus without incident fractures, MOFs and central fractures (p < 0.001).
AUROCs for 5-year fracture risk stratification for incident fractures, MOFs and central fractures are presented in Table 3. The FRISBEE prediction model for all fractures performed well in stratifying risk for all incident fractures (AUROC 0.69, 95% CI 0.67 to 0.72), MOFs and central fractures (for both: 0.68, 95% CI 0.65 to 0.71). The prediction model for MOFs similarly stratified risk well for all incident fractures (0.72, 95% CI 0.69 to 0.75), MOFs and central fractures (for both: 0.71, 95% CI 0.68 to 0.74). Similar results were obtained with the prediction model for central fractures (all fractures: 0.73, 95% CI 0.70 to 0.76), MOFs and central fractures (0.72, 95% CI 0.69 to 0.75).
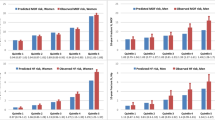
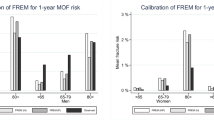
HRs per SD increase in FRISBEE risk predictions from Cox proportional hazards models are summarized in Table 4. There was a significant gradient of risk for all fractures (HR 1.98, 95% CI 1.80 to 2.19), MOFs (2.07, 95% CI 1.84 to 2.33) and central fractures (2.26, 95% CI 2.00 to 2.55) (p < 0.001 for all three outcomes). Cumulative fracture incidence plots showed clear separation according to risk tertiles (all log-rank p < 0.001) as shown in Fig. 1. Compared to the lowest risk tertile, middle and highest tertiles were associated with significantly increased risk for all fractures (middle: HR 2.25, 95% CI 1.61 to 3.16; highest: HR 4.70, 95% CI 3.45 to 6.41), MOF (middle: 2.36, 95% CI 1.53 to 3.65; highest 5.78, 95% CI 3.90 to 8.57) and central fractures (middle: 2.41, 95% CI 1.54 to 3.79; highest: 6.50, 95% CI 4.33 to 9.75).
Calibration (observed versus predicted 5-year fracture risk) with the FRISBEE models is summarized in Table 4 and Fig. 1. There was overestimation in risk of all fractures (calibration-in-the-large 0.63, calibration slope 0.63), MOF (calibration-in-the-large 0.51, calibration slope 0.57) and central fractures (calibration-in-the-large 0.55, calibration slope 0.60).
Discussion
We found that the FRISBEE prediction models performed well for risk stratification for all fractures, MOF and central fractures. However, evaluation of calibration showed that the models overestimated risk for all three fracture outcomes. To our knowledge, this is the first external validation study for FRISBEE 5-year prediction models.
Several externally validated tools, including FRAX, Garvan fracture risk calculator (FRC) and QFracture, are available for use in clinical practice. The tools use different combinations of risk factors and BMD to estimate fracture risk. No robust head-to-head comparisons exist comparing the available tools against one another or against FRISBEE 5-year models [18, 19]. FRISBEE 5-year prediction models include risk associated with history of falls and previous fractures, hip and spine BMD, and a number of other established risk factors (age, high alcohol intake, rheumatoid arthritis, other comorbidities), but several other risk factors were not included based on multivariate analyses (parental hip fracture, glucocorticoid use, current smoking, high or low body mass index, sedentary lifestyle, sleep disturbances, education level, early non-substituted menopause).
The source of the observed FRISBEE miscalibration in our cohort of women from Canada is unclear, especially since the FRAX tool for Belgium generates similar probabilities to the Canadian FRAX tool. Several possibilities may contribute to the observed differences. First, miscalibration is not uncommon when prediction tools are externally validated in other populations, even when risk stratification is similar. Both overestimation and underestimation of fracture risk with Garvan FRC, and overestimation of hip fracture risk with the Fracture Risk Evaluation Model (FREM), have recently been demonstrated when applied to our cohort [20, 21]. Second, marked variation in fracture risk exists between countries. These differences are poorly understood but are likely multifactorial, reflecting unmeasured lifestyle, environmental and genetic factors [22]. Third, differences between modelled and observed fracture may reflect differences in the relative proportion of MOF to hip fractures. While the Canadian FRAX model demonstrated good calibration for MOF prediction [23, 24], the Belgian FRAX model severely underestimated risk in the FRISBEE cohort (calibration slope 2.12, p < 0.001) [25]. This discrepancy may reflect the 1.7 to 1.8-fold higher MOF to hip ratios in the FRISBEE cohort compared to the ratios used to estimate non-hip fractures for calibrating the Belgian FRAX tool [26, 27].
A major strength of our study is that our sample was representative of older women seen in routine clinical practice for assessment of bone health [28]. Our results are therefore broadly generalizable to clinical practice. There are several limitations to consider. First, our analysis was limited to those referred for BMD testing; there may therefore be a selection bias for individuals at intrinsically higher risk of all fractures. However, this would actually produce higher observed/predicted ratios (i.e., risk underestimation, not overestimation) if there are strong risk factors in the referral population not captured by the risk prediction tool. Conversely, elderly individuals living in congregate settings (e.g., nursing homes) and those with severe function-impairing disabilities or higher short-term mortality may be less likely to be referred for such testing [29]. The same limitations apply to the FRISBEE cohort. Second, fracture rates vary between countries and populations, which may limit application to settings with much higher or lower risk than in Canada [22]. Finally, mean follow-up duration was short at 2.5 years. However, this would not affect assessment of calibration which estimates 5-year fracture probability from the cumulative incidence function.
In summary, we found that recently published FRISBEE 5-year prediction models are able to risk stratify all fractures, MOFs and central fractures in Canadian women, but overestimated fracture risk, emphasizing the need for re-calibration before application in the Canadian context. Further efforts are warranted to externally validate the prediction models in other international cohorts, and should ideally include head-to-head comparisons against other available fracture risk assessment tools. Where miscalibration is identified, high-quality data (ideally population-based and representative of the population’s demographics and clinical risk factors) could be used to obtain satisfactory calibration.
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. The Lancet 393(10169):364–376
Hansen D, Bazell C, Pelizarri P, Pyenson B (2019) Medicare cost of osteoporotic fractures. Report Commissioned by the National Osteoporosis Foundation. URL: https://assets.milliman.com/ektron/Medicare_cost_of_osteoporotic_fractures.pdf. Accessed 23 Dec 2022
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV et al (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25
Kanis JA, McCloskey EV (1998) Risk factors in osteoporosis. Maturitas 30(3):229–233
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18(8):1033–1046
Kinnard V, Baleanu F, Iconaru L, Moreau M, Paesmans M, Body JJ et al (2020) Postfracture risk assessment: target the centrally sited fractures first! A substudy of NoFRACT. J Bone Miner Res 35(4):827–828
Borgen TT, Bjørnerem Å, Solberg LB, Andreasen C, Brunborg C, Stenbro MB et al (2019) Post-fracture risk assessment: target the centrally sited fractures first! A substudy of NoFRACT. J Bone Miner Res 34(11):2036–2044
Baleanu F, Moreau M, Charles A, Iconaru L, Karmali R, Surquin M et al (2022) Fragility fractures in postmenopausal women: development of 5-year prediction models using the FRISBEE study. J Clin Endocrinol Metab 107(6):e2438–e2448
Fan B, Lu Y, Genant H, Fuerst T, Shepherd J (2010) Does standardized BMD still remove differences between Hologic and GE-Lunar state-of-the-art DXA systems? Osteoporos Int 21(7):1227–1236
Leslie WD, Morin SN, Lix LM, Niraula S, McCloskey EV, Johansson H et al (2019) Performance of FRAX in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. J Bone Miner Res 34(8):1428–1435
Peschken CA, Hitchon CA, Garland A, Bernstein CN, Chen H, Fransoo R et al (2016) A population-based study of intensive care unit admissions in rheumatoid arthritis. J Rheumatol 43(1):26–33
Yang S, Leslie WD, Yan L, Walld R, Roos LL, Morin SN et al (2016) Objectively verified parental hip fracture is an independent risk factor for fracture: a linkage analysis of 478,792 parents and 261,705 offspring. J Bone Miner Res 31(9):1753–1759
O’Donnell S, Group CCDSSCOW (2013) Use of administrative data for national surveillance of osteoporosis and related fractures in Canada: results from a feasibility study. Arch Osteoporos 8:143
Lix LM, Azimaee M, Osman BA, Caetano P, Morin S, Metge C et al (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12:301
Leslie WD, Epp R, Morin SN, Lix LM (2021) Assessment of site-specific X-ray procedure codes for fracture ascertainment: a registry-based cohort study. Arch Osteoporos 16(1):107
Iconaru L, Charles A, Baleanu F, Surquin M, Benoit F, Mugisha A et al (2022) Prediction of an imminent fracture after an index fracture - models derived from the Frisbee cohort. J Bone Miner Res 37(1):59–67
Leslie WD, Lix LM, Wu X, Program MBD (2013) Competing mortality and fracture risk assessment. Osteoporos Int 24(2):681–688
Rubin KH, Friis-Holmberg T, Hermann AP, Abrahamsen B, Brixen K (2013) Risk assessment tools to identify women with increased risk of osteoporotic fracture: complexity or simplicity? A systematic review. J Bone Miner Res 28(8):1701–1717
Beaudoin C, Moore L, Gagne M, Bessette L, Ste-Marie LG, Brown JP et al (2019) Performance of predictive tools to identify individuals at risk of non-traumatic fracture: a systematic review, meta-analysis, and meta-regression. Osteoporos Int 30(4):721–740
Agarwal A, Leslie WD, Nguyen TV, Morin SN, Lix LM, Eisman JA (2022) Predictive performance of the Garvan Fracture Risk Calculator: a registry-based cohort study. Osteoporos Int 33(3):541–548
Moller S, Skjodt MK, Yan L, Abrahamsen B, Lix LM, McCloskey EV et al (2022) Prediction of imminent fracture risk in Canadian women and men aged 45 years or older: external validation of the Fracture Risk Evaluation Model (FREM). Osteoporos Int 33(1):57–66
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C et al (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA et al (2010) Independent clinical validation of a Canadian FRAX tool: fracture prediction and model calibration. J Bone Miner Res 25(11):2350–2358
Fraser LA, Langsetmo L, Berger C, Ioannidis G, Goltzman D, Adachi JD et al (2011) Fracture prediction and calibration of a Canadian FRAX® tool: a population-based report from CaMos. Osteoporos Int 22(3):829–837
Baleanu F, Iconaru L, Charles A, Kinnard V, Fils JF, Moreau M et al (2021) Independent external validation of FRAX and Garvan fracture risk calculators: a sub-study of the FRISBEE cohort. JBMR Plus 5(9):e10532
Mugisha A, Bergmann P, Kinnard V, Iconaru L, Baleanu F, Charles A et al (2021) MOF/hip fracture ratio in a Belgian cohort of post-menopausal women (FRISBEE): potential impact on the FRAX® score. Calcif Tissue Int 109(6):600–604
Leslie WD, Kanis JA (2021) Calibration of FRAX: a journey, not a destination. Calcif Tissue Int 109(6):597–599
Leslie WD, Caetano PA, Macwilliam LR, Finlayson GS (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8(1):25–30
Leslie WD, Tsang JF, Lix LM (2008) Validation of ten-year fracture risk prediction: a clinical cohort study from the Manitoba Bone Density Program. Bone 43(4):667–671
Acknowledgements
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC 2016/2017-29). The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, Seniors and Active Living, or other data providers is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee.
Author information
Authors and Affiliations
Contributions
Authors’ roles: conception, design, analysis, drafting the article (AA, WDL), interpretation of data (all authors); critically revising the article for important intellectual content (all authors); final approval of the version to be published (all authors); and agreement to be accountable for all aspects of the work (all authors). WDL had full access to all the data in the study and takes the responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agarwal, A., Baleanu, F., Moreau, M. et al. External validation of FRISBEE 5-year fracture prediction models: a registry-based cohort study. Arch Osteoporos 18, 13 (2023). https://doi.org/10.1007/s11657-022-01205-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01205-7