Abstract
Purpose
To demonstrate the successful percutaneous treatment of extrahepatic cystic echinococcosis as an alternative to surgical procedures.
Materials and methods
A total of 27 extrahepatic hydatid cysts in 12 patients, the spleen in 8 patients, muscles and soft tissues in 3 patients each and right adrenal gland in 1 patient were treated with PAIR (puncture, aspiration, injection, respiration) or single puncture catheterization methods. As a scolicidal and sclerosing agent, alcohol was used in all patients.
Results
Of 27 extrahepatic lesions of hydatid cysts, 24 (88.9%) were Gharbi type 1 (WHO CE 1), and 3 (11.1%) were Gharbi type 2 (WHO CE 3A). Of hydatid cystic lesions, 20 with PAIR and 7 with single puncture catheterization methods were treated. No major complications developed in any patients. Abscesses were detected in two patients (16.6%). Mean total hospital stay was calculated between 1 and 14 days (mean 2.3 days). Follow-up periods ranged between 10 and 62 months (mean 22.3 months).
Conclusion
Percutaneous treatment for extrahepatic hydatid cystic lesions is an important alternative to surgical procedures because of the high therapeutic success rate, lower rate of complications and shorter hospital stays.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cystic echinococcosis (CE) is a zoonosis caused by the larvae of Echinococcus granulosus. CE is common in areas where sheep and cattle are raised and endemic to the regions including the Mediterranean, the Middle East, Central Asia, South America, Africa, Australia, New Zealand and Turkey [1,2,3,4].
The most frequent site of hydatid cysts is the liver, ranging between 50 and 70%, followed by the lungs at 15 to 20% and, less frequently, other organs, such as the spleen, kidney, bones and brain [3, 5]. The involvement of muscular and adrenal glands in hydatid disease is extremely rare. Muscular hydatid disease is reported to vary between 0.5 and 4.7%, while the adrenal gland is reported as 0.06% in different series [6, 7].
Medications are ineffective to treat hydatid cysts, and surgery is associated with serious mortality and morbidity, high recurrence rates and long hospital stays [8, 9]. For years, surgical treatments have been the only modalities used in organs such as the spleen because of the risk of rupture [10]. However, percutaneous treatment of hydatid cysts has recently emerged as a potential alternative to other surgical options because of the low morbidity and mortality rates, efficiency and reliability [8, 11].
In this study, our aim is to demonstrate the success rate, effectiveness and reliability of percutaneous treatment of extrahepatic CE lesions with PAIR (puncture, aspiration, injection, respiration) or single puncture catheterization (SPC) techniques.
Materials and methods
Patients
After approval had been obtained from the local ethical board, a total of 27 CE lesions in 12 patients diagnosed with extrahepatic hydatid cysts and percutaneously treated in our institute between March 2008 and April 2015 were retrospectively investigated. Twelve patients with mean age 43.9 ± 24.3, ranging between 12 and 79 years and consisting of two males and ten females, were percutaneously treated. The hydatid cystic lesions in the patients were localized in the spleen in eight patients, in the left psoas muscle and gluteal region in one patient, in the fatty tissue of the right supraclavicular region in one patient and in the right adrenal gland in another patient. Multiple lesions were also determined in the bilateral gluteus maximus muscles, right piriformis muscle and perirectal fatty tissue in the last patient.
Radiological workup was performed via ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI). US was performed in all patients, and CT and MRI were conducted in six and three patients, respectively. All cysts were classified under the criteria described by the World Health Organization and Gharbi’s classifications [12, 13]. The classifications are presented in Table 1. The diagnosis of CE was proven with the cytological examination of specimens acquired by aspiration after the percutaneous treatment.
Procedure
Written informed consent was obtained from all patients before the treatment. To prevent dissemination, oral albendazole (10 mg/kg/day) was commenced in all patients by starting 10 days before and continuing for 3 weeks after the treatment. Complete blood count, prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR) and platelet counts were evaluated.
All of the patients were sedated and monitored by an anesthesiologist in the interventional suite because of the possible risks of anaphylaxis. Under the guidance of US and C-arm fluoroscopy, all percutaneous procedures were carried out by two radiologists with 8 years experience in the field of interventional radiology. The lesions were depicted with US. After obtaining sterilization, local anesthesia (prilocaine hydrochloride) was administered prior to the puncture of the cyst. Then, the lesions were punctured with US guidance. PAIR was used for lesions smaller than 6 cm in size and the SPC technique for those larger than 6 cm. Although larger than 6 cm, the hydatid cystic lesion localized in the right adrenal gland was treated with the PAIR technique because we considered that enough parenchymal support would not be obtained during the catheterization.
With PAIR, the CE lesion was punctured with an 18-gauge needle with US guidance. Nearly 50% of the fluid volume in the cyst calculated according to US measurements was aspirated. Then, by injecting a contrast agent (sodium amidotrizoate, Urografin, Bayer) into the cystic cavity at the rate of 10–20% initial fluid volume (calculated from US measurements) under fluoroscopy guidance until the cyst contours became definite, the completeness of the cyst and its association with adjacent structures were evaluated. Almost the full fluid volume of the cavity was re-aspirated, and a combination of absolute alcohol (98% alcohol and approximately 30–50% of the aspirated cavity volume) and contrast agent (approximately 10–20% of the aspirated cavity volume) was injected into the cavity. After waiting for 7–10 min, and seeing the detachment of the endocyst from the pericyst, the injected alcohol was re-aspirated.
In performing the SPC technique, the cyst was catheterized through an 8-F catheter (Bioteq, Taipei, Taiwan) using the trocar method. In the trocar technique, a catheter mounted on a metal stiffening cannula and a sharp trocar needle was inserted into the lesion under US guidance. After seeing the catheter in the lesion on US, the metal stiffening cannula and needle were pulled away, and the pigtail was formed. The content of the cyst was completely aspirated, and a mixture of 0.09% NaCl and contrast agent equal to the amount aspirated was injected into the cyst. Based on cavitographic images, the completeness of the cyst and its association with adjacent structures were evaluated. The diluted contrast agent in the cavity of the cyst was aspirated again, and a mixture of absolute alcohol (98% alcohol, approximately 30–50% of the aspirated cavity volume) and contrast agent at the rate of 10% of cystic volume was then injected into the cavity. After waiting for nearly 20 min, the cystic cavity was re-aspirated, and the catheter was fixed onto the skin.
After the procedures, all patients were observed and monitored in the interventional radiology unit to monitor possible early complications. The patients treated with PAIR were hospitalized on the same day and were discharged the next day after US. When the amount of fluid drained from the cavity decreased below 10 ml per day in patients undergoing catheterization, these patients were discharged after the removal of the catheters. The duration of patients' hospital stay is presented in Table 2.
Follow-ups
The follow-ups of all patients were performed with US at months 1, 3, 6, 9 and 12 following the first procedure and only once a year during the following years. CT and MRI were added to US when the US investigation was insufficient in some tissues or because of complications. In follow-ups, the size, volume, content and wall changes of the treated hydatid cysts were evaluated with US. The healing criteria consisted of considerable reduction in the size and volume of the cyst, irregularity and thickening of the cystic wall, a decrease in the fluid component of the cavity and solidification of the cyst in time by the disappearance of the fluid component [14].
Results
Of 27 hydatid cysts detected, 24 (88.9%) were Gharbi type 1 (WHO CE 1), and 3 (11.1%) were Gharbi type 2 (WHO CE 3A). The data collected from the patients are summarized in Table 2. Of 27 CE lesions, 20 and 7 were treated with the PAIR and SPC techniques, respectively. The PAIR and SPC techniques both were applied successfully in all cysts. The volumes of treated cysts initially ranged between 3 and 792 ml (mean 121.8 ml). A reduction of 83% was observed between initial cystic volumes and residual cystic volumes measured after the follow-ups (Fig. 1). In patients treated with catheterization, the residual cystic volume was measured as mean 59.8 ml after treatment, while the volume was measured as mean 7.7 ml in those treated with the PAIR technique. While mean loss of volume was 85% in patients undergoing catheterization, the loss was measured as 71% in those treated with the PAIR technique.
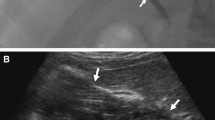
After the follow-ups, it was observed that nine cysts (33.3%) had totally disappeared; nine cyts (33.3%) showed contour irregularities, membrane detachment and a decrease of more than 50% in cystic volume; irregularities of contours, elevations in the solid component and appearance of pseudotumors were present in nine cysts (33.3%) (Fig. 2). No recurrence was determined in any patients after the follow-ups.
No major complications, such as anaphylactic shock or abdominal dissemination, were encountered in any patients. In two patients (16.6%), minor complications developed. In one of these patients for whom SPC had been performed because of a spleen hydatid cyst, pain in the left upper quadrant and fever were observed. Using US and CT, an abscess was determined at the level of the spleen. The abscess was treated with a 14F pigtail catheter (Bioteq, Taipei, Taiwan) and proper antibiotics. In another patient for whom SPC had been performed because of hydatid cysts in the left lumbar and gluteal region, high fever and left-sided pain developed 1 month later. An abscess was detected at the level of the left kidney lower pole on US and CT, and the abscess was treated with proper antibiotics following 14-F pigtail drainage catheterization.
Patient follow-up periods were between 10 and 62 months (median 14.5 months, mean 22.3 months). During the follow-up periods, US was performed in all patients, and CT and MRI were performed in four patients and one patient, respectively.
The times of hospital stay ranged between 1 and 14 days (median 1 day, mean 2.3 days) in all patients. The times were found between 1 and 2 days in those treated with catheterization, while they were calculated as 1 day in all but one patient treated with PAIR. In the patient treated with PAIR and staying at the hospital for 14 days, the treated hydatid cystic lesions in the gluteal region were infected, and the findings of osteomyelitis due to infection were detected in the right sacroiliac region. After percutaneous intervention, the patient was treated with proper antibiotics, and the symptoms of osteomyelitis were seen to regress.
Discussion
Percutaneous treatments can be performed not only in CE lesions localized in the liver, but also in the treatment of CE lesions localized in other extrahepatic solid organs and soft tissues. As a more noninvasive and reliable method with lower rates of postoperative complications and recurrences and shorter periods of hospital stay, percutaneous treatment modalities are of important advantages [11]. However, surgical procedures have longer hospital stay periods and higher rates of complications as well as higher morbidity and mortality rates [5, 8, 15].
The complication rates of post-splenectomy were reported as 36% in a study conducted by Arikanoglu et al. and 29% in another study by Atmatzidis et al. [5, 15]. In another study, recurrence rates were reported to range between 12 and 14% in patients treated with splenectomy and spleen-preserving surgery [5]. In our study, minor complications developed only in two patients (16.6%), and no recurrence was observed during the follow-ups.
Surgical treatments of soft tissue and adrenal gland hydatic cysts are reported to have some major disadvantages, including the requirement for extensive surgical resection, surgical scarring and risk of anesthesia [16, 17]. Percutaneous treatments are of a vital importance in preserving organ functions without requiring the total removal of organs, such as the spleen and adrenal gland. Additionally, percutaneous interventions led to no large excision areas in soft tissues and are less risky in terms of postoperative complications [17]. In extrahepatic hydatid cystic lesions treated with percutaneous modalities in our study, the functions of organs were protected and no complications such as an extensive excision area in soft tissues or surgical scars were encountered.
To the best of our knowledge, the number of studies related to the percutaneous treatment of extrahepatic CE lesions is restricted in the literature. In a study conducted by Akhan et al., 12 hydatid cystic lesions detected in the spleen were successfully treated. Abscesses developed in four patients, and splenectomy was performed in two patients because of infection following the treatment. Mean hospital stay was found to be 9 days [8]. In other studies performed by Akhan et al., the lesion identified in the adrenal gland was treated successfully with percutaneous methods, and no recurrences were encountered within long-term follow-ups. Another study also demonstrated that CE lesions determined in soft tissues were successfully treated, and minor complications were detected only in two patients. The duration of hospital stay was calculated as mean 17.8 days [6, 17]. In our study, all hydatid cysts in soft tissues, adrenal glands and spleens were successfully treated via percutaneous methods. No major complications developed in any patients, abscesses were detected only in two patients (16.6%), and mean hospital stay time was found as 2.3 days. In follow-ups, no recurrences were observed in any of the patients.
Different from other catheterization methods reported in the literature, we use the trocar technique of direct catheterization into the cyst. Therefore, we consider that the trocar method reduces the risk of fluid leakage and spillage into the adjacent tissues or abdomen. We also use alcohol as a scolicidal and sclerosing agent while performing percutaneous interventions. So, we obtain a scolicidal and sclerosing effect by performing a single procedure on the same day.
In the medical treatment of CE lesions, agents such as benzimidazole, albendazole and mebendazole are used [18]. Unfortunately, using these agents alone is insufficient in the treatment process. Before and after percutaneous treatments, these agents are administered prophylactically to prevent abdominal dissemination and recurrences [3]. In our study, albendozole was given to all patients by starting 10 days before and continuing for 3 weeks after the procedure.
US is a widely used imaging technique to screen and diagnose hydatid cystic lesions [2, 7, 19]. As well as its use in screening hydatid cysts, US is also used during percutaneous treatments and in the follow-ups of patients as an important noninvasive method compared to other imaging techniques [17]. The type of cyst is defined through US findings based on the Gharbi and WHO classifications. The appearance of the disease on CT is not pathognomonic and might be confused with benign or malignant disorders, such as single or multiple metastases, congenital cysts or pseudocysts, hematomas and other lesions [7, 17]. However, CT is helpful in demonstrating the osseous and extraosseous extension of the disease and superior to MRI in demonstrating wall calcifications [17]. CT is also known to be more influential in the incidental identification of hydatid cysts in asymptomatic organs, such as especially the adrenal gland [19]. MRI is, however, an effective screening method used to demonstrate soft tissue hydatid cysts, and the detachment of the pericyst from endocyst can be demonstrated better via MRI [20]. In addition, MRI can reveal cystic masses containing daughter cysts and waterlily signs, characteristics of hydatid cystic disease. The cyst wall shows a rim of low signal intensity on both T1- and T2-weighted images [17, 20]. In our study, US was primarily used in the diagnosis and follow-ups of CE lesions. MRI and CT were also included in our investigations, the former into the imaging of soft tissue CE lesions and the latter for hydatid cystic lesions of adrenal glands.
In conclusion, percutaneous treatments are safe and effective procedures with successful results in patients with extrahepatic hydatid cysts and should be assessed as important alternatives to surgical interventions. We consider that further studies including larger populations are needed to support the percutaneous treatments of extrahepatic hydatid cysts.
References
Eris C, Akbulut S, Yildiz MK, Abuoglu H, Odabasi M, Ozkan E, et al. Surgical approach to splenic hydatid cyst: single center experience. Int Surg. 2013;98:346–53.
Giorgio A, Di Sarno A, de Stefano G, Liorre G, Farella N, et al. Sonography and clinical outcome of viable hydatid liver cysts treated with double percutaneous aspiration and ethanol injection as first-line therapy: efficacy and long-term follow-up. AJR Am J Roentgenol. 2009;193:W186–92.
Nayman A, Guler I, Keskin S, Erdem TB, Borazan H, Kucukapan A, et al. A novel modified PAIR technique using a trocar catheter for percutaneous treatment of liver hydatid cysts: a six-year experience. Diagn Interv Radiol. 2016;22:47–51.
Sozuer E, Akyuz M, Akbulut S. Open surgery for hepatic hydatid disease. Int Surg. 2014;99:764–9.
Atmatzidis K, Papaziogas B, Mirelis C, Pavlidis T, Papaziogas T. Splenectomy versus spleen-preserving surgery for splenic echinococcosis. Dig Surg. 2003;20:527–31.
Akhan O, Canyigit M, Kaya D, Koksal A, Akgoz A, Yucesoy C, et al. Long-term follow-up of the percutaneous treatment of hydatid cyst in the adrenal gland: a case report and review of the literature. Cardiovasc Intervent Radiol. 2011;34(Suppl 2):S256–9.
Merkle EM, Schulte M, Vogel J, Tomczak R, Rieber A, Kern P, et al. Musculoskeletal involvement in cystic echinococcosis: report of eight cases and review of the literature. AJR Am J Roentgenol. 1997;168:1531–4.
Akhan O, Akkaya S, Dagoglu MG, Akpinar B, Erbahceci A, Ciftci T, et al. Percutaneous treatment of splenic cystic echinococcosis: results of 12 cases. Cardiovasc Intervent Radiol. 2016;39:441–6.
Akhan O, Ozmen MN. Percutaneous treatment of liver hydatid cysts. Eur J Radiol. 1999;32:76–85.
Khoury G, Abiad F, Geagea T, Nabout G, Jabbour S. Laparoscopic treatment of hydatid cysts of the liver and spleen. Surg Endosc. 2000;14:243–5.
Kabaalioglu A, Ceken K, Alimoglu E, Apaydin A. Percutaneous imaging-guided treatment of hydatid liver cysts: do long-term results make it a first choice? Eur J Radiol. 2006;59:65–73.
Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459–63.
WHO: Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253–61.
Akhan O, Dincer A, Gokoz A, Sayek I, Havlioglu S, Abbasoglu O, et al. Percutaneous treatment of abdominal hydatid cysts with hypertonic saline and alcohol. An experimental study in sheep. Invest Radiol. 1993;28:121–7.
Arikanoglu Z, Taskesen F, Gumus H, Onder A, Aliosmanoglu I, Gul M, et al. Selecting a surgical modality to treat a splenic hydatid cyst: total splenectomy or spleen-saving surgery? J Gastrointest Surg. 2012;16:1189–93.
Akcay MN, Akcay G, Balik AA, Boyuk A. Hydatid cysts of the adrenal gland: review of nine patients. World J Surg. 2004;28:97–9.
Akhan O, Gumus B, Akinci D, Karcaaltincaba M, Ozmen M. Diagnosis and percutaneous treatment of soft-tissue hydatid cysts. Cardiovasc Intervent Radiol. 2007;30:419–25.
Gomez IGC, Lopez-Andujar R, Belda Ibanez T, Ramia Angel JM, Moya Herraiz A, Orbis Castellanos F, et al. Review of the treatment of liver hydatid cysts. World J Gastroenterol. 2015;21:124–31.
Tuzun M, Hekimoglu B. Pictorial essay. Various locations of cystic and alveolar hydatid disease: CT appearances. J Comput Assist Tomogr. 2001;25:81–7.
Chevalier X, Rhamouni A, Bretagne S, Martigny J, Larget-Piet B. Hydatid cyst of the subcutaneous tissue without other involvement: MR imaging features. AJR Am J Roentgenol. 1994;163:645–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest, and no grants or funds were received. The study was reviewed by the ethics committee and performed in accordance with the ethical standards laid down in an appropriate version of the 1964 Declaration of Helsinki and its later amendments as revised in Brazil 2013.
About this article
Cite this article
Arslan, S., Bakdik, S., Oncu, F. et al. Successful percutaneous treatment of extrahepatic cystic echinococcosis through PAIR and single puncture catheter techniques. Jpn J Radiol 35, 296–302 (2017). https://doi.org/10.1007/s11604-017-0633-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-017-0633-z