Abstract
Purpose
To evaluate and compare the results of puncture, aspiration, injection and re-aspiration (PAIR) and catheterization techniques for treatment of CE1 and CE3a liver hydatid cysts according to World Health Organization classification.
Materials and Methods
Forty patients (29 females) with 56 liver CE1and CE3a cysts were prospectively randomized and enrolled into 2 groups by sealed envelope method. Procedures were performed under general anesthesia. Several parameters including technical success (completing procedure steps), clinical success (lack of recurrence on follow-up), major and minor complications, long-term changes of cyst cavities and length of hospital stay were compared between two groups.
Results
As in 2 patients with 3 cysts, PAIR technique had to be changed to catheterization technique due to technical reasons. The technical success rates were 91.9% and 100% for PAIR and catheterization groups, respectively. Volume decrease rates were 78.5% and 86.8% in PAIR and catheterization groups, with a mean follow-up of 78.1 and 71 months, respectively. There was no mortality, anaphylactic shock or intraabdominal dissemination. The rate of major complications such as abscess, cysto-biliary fistula and recurrence was 2.94% and 36.84% in PAIR and catheterization groups, respectively (p = 0.002). Median length of hospital stay was shorter in PAIR group (1 vs 4 days) (p = 0.015).
Conclusion
PAIR technique should be preferred to catheterization technique for treatment of liver CE1 and CE3a cysts due to lower rates of major complications and length of hospital stay. Catheterization technique should be employed when cysto-biliary fistula was evident.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystic echinococcosis (CE), traditionally named as hydatid cyst, is a common public health problem in several parts of the globe including Mediterranean basin, Middle East and South America as well as several parts of India, China and Africa [1,2,3,4]. Patients may be diagnosed incidentally or may present with nonspecific symptoms. Clinically severe complications such as; systemically disseminated disease or anaphylaxis after cyst rupture into the peritoneum or biliary tract, albeit rare, may also be encountered in the course of the disease. Viable cysts, even if the patients are asymptomatic, should be treated due to the aforementioned potentially life threatening complications related to the disease [3]. The traditional approach to treatment for liver CE is surgery. However, this approach may be associated with high rates of morbidity, mortality, disease recurrence and a long stay in the hospital with non-negligible burden on health care expenses [5,6,7,8]. Noninvasive approach, with albendazole, has been shown to have limited efficacy in the treatment of this patient group [9, 10]. In modern clinical practice, percutaneous approach to these patients has been shown to be highly effective and with reduced morbidity and mortality [5, 7, 11,12,13,14].
There are three different techniques for the percutaneous treatment of hydatid cysts:
- 1.
PAIR (Puncture, Aspiration of the cyst contents, Injection of hypertonic saline and Reaspiration of all the fluid)
- 2.
Catheterization technique with hypertonic saline and ethanol are widely used for liver CE1and CE3a type hydatid cysts according to world health organization (WHO) classification.
- 3.
Modified catheterization Technique (MoCaT): This approach has been defined for the percutaneous treatment of CE2 and CE3b liver cysts [15,16,17].
Among these three, PAIR emerges as a relatively less technically demanding approach. It is characterized with one needle puncture into the cyst, whereas catheterization technique necessitates more needle and catheter manipulations. The main downside of catheterization technique is the longer patient stay time in the hospital stay [5, 7].
Despite the fact that the results of both techniques have been reported separately in the literature, to the best of our knowledge, there are no data in the literature comparing the effectiveness of PAIR and catheterization techniques in a prospective fashion.
The aim of this study is to compare the long-term results of PAIR and catheterization techniques in the treatment of liver CE1 and CE3a in prospective randomized manner.
Materials and Methods
Forty patients (29 females) with 56 liver CE1and CE3a cysts were prospectively randomized and enrolled into 2 groups within a 5 year period. Randomization was done with sealed envelope technique. The operators, who were blinded to the patient’s radiological data, opened the envelopes the day before to procedure. In two patients with 3 cysts in the PAIR group, the treatment approach had to be changed to catheterization technique due to technical necessities. Finally, 38 patients with 53 liver hydatid cysts who met the inclusion criteria were enrolled into the study (Table 1).
In the first arm of the study (21 patients with 34 cysts), cysts were treated with “PAIR technique”, whereas; 17 patients with 19 cysts were treated with “catheterization technique” in the second arm. The procedures were performed by two senior interventional radiologists who had at least 10 years of experience in percutaneous treatment of the hydatid disease.
After the procedures, we prospectively followed the patients in terms of primary (technical success and complications) and secondary (recurrence rate, length of hospital stay and long-term changes of cyst cavities) outcomes. Our Institutional Review Board approved this study.
Hypothesis of the Study, Inclusion and Exclusion Criteria
The hypothesis of the study was that the complication rates are lower in patients treated with PAIR technique as compared to those treated with the catheterization technique.
Inclusion criteria: Patients with WHO CE1 (pure fluid collection) and WHO CE3a (fluid collection with a split wall) liver hydatid cysts with diameter of at least 4 cm irrespective whether they were symptomatic or asymptomatic were included.
Exclusion criteria: Patients with liver CE2 and CE3b, CE4 or CE5 hydatid cysts according to.
WHO classification with extrahepatic hydatid cysts and liver CE 1 and 3a cysts smaller than 4 cm.
Pre-procedural Preparation
The hydatid cysts were initially diagnosed with ultrasonography and were classified on the basis of US features. After aspiration of the cyst content, the diagnosis was confirmed with microbiological examination.
Written informed consents were obtained from all patients before the procedure. Prophylactic Albendazole (Andazol;Biofarma/Turkey) was given 10–15 mg/kg/per day orally, starting one week before the procedure and continuing 4 weeks after procedure [18]. Due to the potential risk of severe allergic reaction all procedures were performed under general anesthesia.
Patients fasted for at least 8 h before the procedure for preparation to general anesthesia. The coagulation parameters (CBC, PT, INR) of the enrollees were reviewed before the procedure. Any coagulopathy (INR > 1.5, platelet count < 50,000/mm3) was corrected before procedure. All procedures were performed in the interventional radiology suite under US and fluoroscopic guidances.
Techniques
PAIR technique [19]: The cysts were punctured by an 18G Seldinger needle under sonographic guidance. Approximately, 20% of the estimated volume of the cyst was aspirated before contrast agent (Ultravist 300/100 mg/ml; Bayer Schering Pharma, Berlin, Germany) was injected through needle under fluoroscopy to detect any potential communication with the biliary system or the peritoneum.
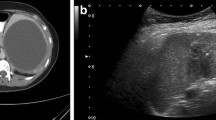
Although in case of communication with biliary tree, scolicidal or sclerosing agents were not injected as they may gave rise to severe sclerosing cholangitis. In these patients, we inserted a catheter (Flexima APDL Boston Scientific, USA) into the cavity for gravity drainage (Fig. 1). When the daily drainage dropped down to less than 10 cc, sclerosis by ethanol (96%) was done under fluoroscopic guidance. If the daily drainage was more than 10 cc, the catheter was left in place until the drainage stopped. After sclerosis with ethanol, the catheter was withdrawn.
A 38-year-old woman was referred to ultrasound for right upper quadrant pain. A CE3a cyst was found in the liver and percutaneous treatment was scheduled. A Cystogram obtained following drainage catheter (arrowhead) insertion revealed biliary communication (arrows). The drainage catheter was kept in the cavity without hypertonic saline injection. On the 7th day after the procedure daily drainage decreased to 20 mL. No further intervention was required for the cysto-biliary fistula. On the 10th day there was no drainage from the cavity. Hypertonic saline injection and sclerosis by ethanol were performed and the catheter was withdrawn. B US obtained after 5 years demonstrated degenerated hydatid cyst cavity (arrows) with no sign of recurrence
If the cyst had no communication with biliary tree confirmed after cystography, the remaining fluid content was aspirated by keeping the tip of the needle within the cavity. At next step hypertonic saline (20–30% in concentration) up to 35–50% of the original cyst volume then was injected. When the separation of the membrane from pericyst occurred (generally happens around 10 min after the injection) the cavity content was re-aspirated through the needle. Finally sclerosis (35–50% of the estimated volume) was done with ethanol (96%) which stayed within the cyst cavity for 5 min. After re-aspiration of previously injected alcohol the needle was withdrawn and the procedure was terminated.
Catheterization technique [1]: After preprocedural preparation similar to PAIR technique, the cyst was punctured with an 18G Seldinger needle under sonographic guidance and a cystogram was obtained as described as above in the PAIR technique. In the absence of any communication between the cyst and the biliary system/peritoneum, the remaining cyst content was aspirated through the needle. Subsequently, hypertonic saline was injected and again we waited for sonographic detachment of the membranes. After the membrane detachment, a 0.035 inch Amplatz guidewire was advanced into cavity, over which an 8F drainage catheter (Flexima APDL Boston Scientific, USA) was advanced. After securing and fixing the catheter, we left it for free gravity drainage. When the daily drainage dropped less than 10 cc, we sclerosed the cavity with ethanol (96%) under fluoroscopic guidance. After sclerosis with ethanol, the catheter was withdrawn.
Follow-Up
All patients were monitored after their procedures in the recovery area and then were transferred to their inpatient floors.
Patients are followed up by US every 3 months in their first year, every 6 months in their second year, and annually thereafter. The primary modality that we use in the follow-up was US [1]. In addition to routine US follow-up, CT studies were also acquired, when US studies were deemed to be suboptimal for optimal evaluation, in 6 cases (five scans in the PAIR group and one scan in the catheterization group).
Definitions and Statistics
Technical success was defined as completion of all steps for PAIR procedure and appropriate placement of the drainage catheter for catheterization technique. Complications were divided into two groups as minor and major based on the CIRSE classification of complications [20].
The healing criteria were reduction in size and volume of cyst, thickening and irregularity of cyst wall, gradual decrease of fluid content and finally solidification of the cyst cavity (pseudotumor appearance). The detection of daughter vesicles or double-layered wall sign during follow-up, was considered as indicators of recurrence. Cyst volumes were calculated by using 3 orthogonal dimensions measured from two-dimensional US images (X × Y × Z × 0.523). Patients who received albendazole were also checked for possible side effects.
Patient characteristics (age, gender), cyst characteristics (single or multiple cysts, volume, CE type), duration of follow-up and length of hospital stay, complications and recurrence rates were statistically analyzed for both groups. For statistical comparisons between two groups, Mann Whitney U, t and chi-square tests were used. For categorical variables frequencies and percentages; for quantitative variables mean, median, standard deviation, minimum and maximum values were used. Statistical analysis was conducted by SPSS 20.0 for Windows (IBM SPSS Statistics, Chicago, IL) and p < 0.05 was considered as statistically significant.
Results
Forty patients (29 females) with 56 liver CE1and CE3a cysts were enrolled into this study. Two patients with 3 cysts from the PAIR arm had to be switched to catheterization arm due to the following two reasons; (1) failure of aspiration of the cystic content due to needle tip occlusion with hydatid membranes seen in 1 cyst, (2) communication of the hydatid cyst with biliary tree revealed on cystogram seen in two cysts. For these reasons, the treatment approach had to be changed to catheterization from PAIR in order to complete the treatment. Therefore, the technical success rates were 91.9% and 100% for PAIR and catheterization arms, respectively.
Twenty-one patients (16 Female) with 34 cysts with a median cyst volume of 110.5 (16–1406) ml were included in PAIR group, whereas 17 patients (11 Female) with 19 cysts with a median cyst volume of 191 (36–1516) ml were included into the catheterization group. In catheterization group, 15 patients had one liver CE cyst; two patients had two liver CE cysts. In PAIR group 15 patients had one liver CE cyst, 4 patients had 2 liver CE cysts, one patient had 3 liver CE cysts and one patient had 8 liver CE cysts. Three of 21 patients in PAIR group and 1 of 17 patients in catheterization group had previous liver surgery due to CE.
The most common presenting symptom was right upper quadrant pain (15.78%). The majority of the patients were asymptomatic (n = 28 patients, 73.68%) at the time of the initial diagnosis. In asymptomatic patients hydatid cysts were detected during ultrasound examination due to various clinical indication including (1) elevated liver enzymes (n = 10), (2) follow-up scan for liver steatosis (n = 13), (3) follow-up scan for renal cysts (n = 5). Four patients (10.52%) had abdominal discomfort, fever and nausea which prompted the diagnosis.
The complications encountered in the study groups are summarized in Table 2. In the PAIR group we saw one patient whose cyst cavity had a bacterial superinfection after treatment and finally presented liver abscess at the previously treated cyst cavity. In the catheterization group abscess formation was detected in 2 cysts, cysto-biliary fistula (CBF) in 1 cyst and both CBF and abscess in 3 cysts. Two out of 3 cysts with CBF and abscess formation were treated with prolonged stay of the drainage catheter within the cyst cavity and intravenous antibiotic therapy. The third cyst, with CBF and abscess combined, was treated by endoscopic papillotomy with prolonged stay of the catheter within the cavity (intravenous antibiotic therapy was also implemented in this patient). Two abscesses without CBF were treated by keeping the catheter in place for a prolonged period of time and appropriate intravenous antibiotic therapy. In one cyst with CBF, catheter dislodgment occurred during follow-up (when the daily drain output was around 20 cc). This patient was put on conservative follow-up without any intervention. Recurrence was detected in this patient on 5-month follow-up and a second intervention was needed for treatment. No other recurrent case was observed in both groups on follow-up imaging. The rate of major complications was statistically significant (p = 0.002) between these two groups (Table 2), whereas the rate of minor complications was statistically insignificant (Table 2). Also there was no statistically significant difference between the groups in terms of pain and fever (48% vs 48%).
The follow-up period was again statistically insignificant between PAIR group (range 12–188 months, mean = 78.1 months) and the catheterization group (range 6–164 months, mean = 71 months) (p > 0.05). On follow-up the liver cysts showed 78.5% and 86.8% volume decrease in PAIR and catheterization groups, respectively (p < 0.05). The median length of hospital stay was significantly shorter in PAIR group (range 1–15 days, median = 1 day) as compared to catheterization group (range 1–52 days, median = 4 days) (p = 0.015). At the time of discharge from the hospital all patients were catheter free.
Discussion
This is a prospective randomized study with the aim of comparing the success rates of PAIR and catheterization techniques in the percutaneous treatment of liver CE 1 and 3a hydatid cysts. We also aimed for comparing the complication rates, the duration of hospital stays and recurrence rates of these two different techniques. Based on our results it appears like the PAIR technique is associated with less major complication rate, shorter duration of hospital stay and lower recurrence rate over catheterization technique. However, two patients with 3 CE cysts were excluded from the PAIR group because of the above-mentioned reasons. Therefore, technical success rates were 91.9% and 100% for PAIR and catheterization groups, respectively, as these two patients with 3 CE cysts had to be treated by catheterization technique.
Some authors have previously advocated that catheterization technique should be the ideal approach for the percutaneous treatment of liver CE1 and 3a cysts which are larger than 6 cm (estimated volume > 100 ml), while PAIR technique may be reserved for the cysts which have less than 6 cm [5, 7, 21]. CE cysts larger than 6 cm were considered to have faster involution of the cavity by utilizing the catheterization technique [5]. Sclerotherapy with ethanol for faster and more efficient involution of the CE cavity may be considered as the percutaneous treatment counterpart of surgical cavity management techniques like omentopexy [5]. Only PAIR with no subsequent sclerotherapy has also been considered optimal approach for CE1 and CE3a liver cyst [12, 22, 23].
We did not encounter any of the previously reported important major complications such as anaphylactic shock, parasite seeding elsewhere in the abdominal cavity or patient death related to percutaneous approach in our study. However, the rates of major complications were 2.94% in PAIR group and 36.84% in catheterization group (p = 0.002). There was no statistically significant difference between 2 groups in terms of pain and fever (48% vs 48%). The frequency of minor complications in our study was in compliance with the results that were previously reported in the literature [24].
There are two retrospective series of giant CE1 and CE3a cysts (at least one size is larger than 10 cm) treated with catheterization technique in the literature [25, 26]. In both series, the rate of major complications such as abscess formation and cysto-biliary fistula were around 30%. Although catheterization technique is proposed as the ideal approach for the percutaneous treatment of giant hydatid cysts, we considered that a prospective randomize study would be relevant to compare the results of two different approaches for the treatment of giant hydatid cysts.
Percutaneous treatment of liver CE1 and CE3a with both PAIR and catheterization techniques was shown to be very effective and safe when compared to the results of medical treatment and surgery [5, 6, 8, 24]. Based on these advantages percutaneous treatment approach has mostly taken over the role of surgery in these patients and became the treatment of choice in CE types [8, 22]. Percutaneous treatment is associated with lower mortality and morbidity rates as well as lower recurrence rates and shorter hospital stays. It is also a less invasive and more cost efficient option to treat multiple liver cysts as well as splenic and other intraabdominal CE cysts as compared to surgical approach [5, 14, 27,28,29,30].
Our study has several limitations. One limitation is the relatively small size of each group. As we could not reach the ideal number of patients (which was considered to be 25 patients in each group) this should be mentioned as another limitation of our study.
In conclusion, we think that PAIR technique may be preferable to catheterization technique whenever percutaneous treatment is considered for liver CE1 and CE3a cysts, due to its statistically significant lower rate of major complications, lower recurrence rate and shorter duration of hospital-stays. Catheterization technique may be more optimal in the presence of cysto-biliary fistulas that were detected during the PAIR procedure. In case of any technical difficulty detected during PAIR approach it may wise to switch to the catheterization technique in order to successfully conclude the procedure.
References
Akhan O, Dincer A, Gokoz A, et al. Percutaneous treatment of abdominal hydatid cysts with hypertonic saline and alcohol. An experimental study in sheep. Invest Radiol. 1993;28:121–7.
da Silva AM. Human echinococcosis: a neglected disease. Gastroenterol Res Pract. 2010;2010:583297. https://doi.org/10.1155/2010/583297
Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13:125–33.
Nunnari G, Pinzone MR, Gruttadauria S, et al. Hepatic echinococcosis: clinical and therapeutic aspects. World J Gastroenterol. 2012;18:1448–58.
Akhan O, Ozmen MN, Dincer A, Sayek I, Gocmen A. Liver hydatid disease: long-term results of percutaneous treatment. Radiology. 1996;198:259–64.
Khuroo MS, Wani NA, Javid G, et al. Percutaneous drainage compared with surgery for hepatic hydatid cysts. N Engl J Med. 1997;337:881–7.
Ustunsoz B, Akhan O, Kamiloglu MA, Somuncu I, Ugurel MS, Cetiner S. Percutaneous treatment of hydatid cysts of the liver: long-term results. AJR Am J Roentgenol. 1999;172:91–6.
Kern P, Menezes da Silva A, Akhan O, et al. The echinococcoses: diagnosis, clinical management and burden of disease. Adv Parasitol. 2017;96:259–369.
Franchi C, Di Vico B, Teggi A. Long-term evaluation of patients with hydatidosis treated with benzimidazole carbamates. Clin Infect Dis. 1999;29:304–9.
Todorov T, Vutova K, Mechkov G, Petkov D, Nedelkov G, Tonchev Z. Evaluation of response to chemotherapy of human cystic echinococcosis. Br J Radiol. 1990;63:523–31.
Brunetti E, Kern P, Vuitton DA. Writing panel for the W-I. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1–16.
Giorgio A, Tarantino L, Francica G, et al. Unilocular hydatid liver cysts: treatment with US-guided, double percutaneous aspiration and alcohol injection. Radiology. 1992;184:705–10.
Khuroo MS, Zargar SA, Mahajan R. Echinococcus granulosus cysts in the liver: management with percutaneous drainage. Radiology. 1991;180:141–5.
Koroglu M, Erol B, Gurses C, et al. Hepatic cystic echinococcosis: percutaneous treatment as an outpatient procedure. Asian Pac J Trop Med. 2014;7:212–5.
Akhan O, Salik AE, Ciftci T, Akinci D, Islim F, Akpinar B. Comparison of long-term results of percutaneous treatment techniques for hepatic cystic echinococcosis types 2 and 3b. AJR Am J Roentgenol. 2017;208:878–84.
Popa AC, Akhan O, Petrutescu MS, et al. New options in the management of cystic echinococcosis—a single centre experience using minimally invasive techniques. Chirurgia (Bucur). 2018;113:486–96.
Akhan O, Gumus B, Akinci D, Karcaaltincaba M, Ozmen M. Diagnosis and percutaneous treatment of soft-tissue hydatid cysts. Cardiovasc Intervent Radiol. 2007;30:419–25.
Akhan O, Yildiz AE, Akinci D, Yildiz BD, Ciftci T. Is the adjuvant albendazole treatment really needed with PAIR in the management of liver hydatid cysts? A prospective, randomized trial with short-term follow-up results. Cardiovasc Intervent Radiol. 2014;37:1568–74.
Ben Amor N, Gargouri M, Gharbi HA, Golvan YJ, Ayachi K. Kchouck H [Trial therapy of inoperable abdominal hydatid cysts by puncture]. Ann Parasitol Hum Comp. 1986;61:689–92.
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017;40:1141–6.
Khuroo MS, Dar MY, Yattoo GN, et al. Percutaneous drainage versus albendazole therapy in hepatic hydatidosis: a prospective, randomized study. Gastroenterology. 1993;104:1452–9.
Group WHOIW. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253–61.
Kabaalioglu A, Ceken K, Alimoglu E, Apaydin A. Percutaneous imaging-guided treatment of hydatid liver cysts: do long-term results make it a first choice? Eur J Radiol. 2006;59:65–73.
Smego RA Jr, Bhatti S, Khaliq AA, Beg MA. Percutaneous aspiration-injection-reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis. 2003;37:1073–83.
Balli O, Balli G, Cakir V, et al. Percutaneous treatment of giant cystic echinococcosis in liver: catheterization technique in patients with CE1 and CE3a. Cardiovasc Intervent Radiol. 2019;42:1153–9.
Men S, Yucesoy C, Edguer TR, Hekimoglu B. Percutaneous treatment of giant abdominal hydatid cysts: long-term results. Surg Endosc. 2006;20:1600–6.
Akhan O, Akkaya S, Dagoglu MG, et al. Percutaneous treatment of splenic cystic echinococcosis: results of 12 cases. Cardiovasc Intervent Radiol. 2016;39:441–6.
Akhan O, Canyigit M, Kaya D, et al. Long-term follow-up of the percutaneous treatment of hydatid cyst in the adrenal gland: a case report and review of the literature. Cardiovasc Intervent Radiol. 2011;34(Suppl 2):S256–S259259.
Akhan O, Ustunsoz B, Somuncu I, et al. Percutaneous renal hydatid cyst treatment: long-term results. Abdom Imaging. 1998;23:209–13.
Yagci G, Ustunsoz B, Kaymakcioglu N, et al. Results of surgical, laparoscopic, and percutaneous treatment for hydatid disease of the liver: 10 years experience with 355 patients. World J Surg. 2005;29:1670–9.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study has obtained IRB approval from Hacettepe University.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akhan, O., Erdoğan, E., Ciftci, T.T. et al. Comparison of the Long-Term Results of Puncture, Aspiration, Injection and Re-aspiration (PAIR) and Catheterization Techniques for the Percutaneous Treatment of CE1 and CE3a Liver Hydatid Cysts: A Prospective Randomized Trial. Cardiovasc Intervent Radiol 43, 1034–1040 (2020). https://doi.org/10.1007/s00270-020-02477-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02477-7