Abstract
The purpose of this study is to demonstrate and discuss the radiological features of four patients with muscular hydatid disease and to evaluate the results of percutaneous treatment in these patients. Four patients (three female and one male) with six muscular hydatid cysts underwent percutaneous treatment and were followed up. The mean age of patients was 35 years (range: 12–60 years). Type I (n = 2), type II (n = 1), and type III (n = 3) hydatid cysts were observed in the thigh (n = 3) and gluteal (n = 1) region on radiologic examination. All interventions were performed under sonographic and fluoroscopic guidance. According to the type of the cyst, the procedure was carried out by either a “catheterization technique with hypertonic saline and alcohol” or a “modified catheterization technique.” The mean cathaterization time was 13.7 days, ranging from 1 to 54 days. The dimensions of the residual cavity were noted at every sonographic control, and an average of 96.1% volume reduction was obtained in six cysts of four patients. No sign of viability was observed during the follow-up period. Cavity infection and cellulitis were observed as complications, which resolved after medical therapy. Percutaneous treatment is a safe and effective procedure in patients with soft-tissue hydatid cysts and should be considered as a serious alternative to surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hydatid cyst might appear anywhere in the body, although the liver and lungs are the primary sites affected in the disease as a result of their role as capillary filter station [1–5]. The liver is the most frequently involved organ (50–77%), whereas the pulmonary involvement ranges between 8.5% and 43%. In 10–15% of the cases, hydatid cysts might occur in other regions of the body, including bone, kidney, heart, and brain [1, 3–5].
Muscular involvement in hydatid disease is extremely rare and muscle is accepted as an unfavorable site for infection because of high lactic acid levels. Muscular hydatid disease is reported between 0.5% and 4.7% in different series [6–9]. The great majority of cases involve the trunk muscles and those proximal to it [8]. Most of the muscular involvement has been reported as the primary disease [7–9].
The traditional treatment of soft-tissue hydatid disease has been surgery, which has major disadvantages, such as the necessity of extensive surgical resection in some cases and the need of general anesthesia [8, 9]. Adjuvant administration of benzimidazole derivates are widely used in treatment protocols (10). However, the efficacy of benzimidazole derivates in the treatment of soft-tissue hydatid disease is very limited [7–9].
Percutaneous treatment is widely employed in most of liver hydatid cysts with successful results [11–14]. The percutaneous approach has also been reported as a safe and effective alternative treatment in patients with pulmonary, renal hydatid cysts as well as atypically located cysts in the orbita and parotid gland [15–18].
The aim of this study is to demonstrate and discuss the radiological features of muscular hydatid disease and to evaluate the results of percutaneous treatment in four patients. To our knowledge, this is the first study in the literature presenting the results of percutaneous treatment in patients with muscular hydatid cysts.
Materials and Methods
Patients
From January 1998 to March 2002, four patients (three female and one male) with six muscular hydatid cysts underwent percutaneous treatment and were followed up until January 2006. The age of the patients ranged from 12 to 60 years (mean: 35 years).
Clinical data and radiological findings of the patients are summarized in Table 1. A nontender palpable mass was the presenting symptom in three patients (patients 1, 2, and 4) and patient 3 had severe pain and swelling of the left thigh. The masses were in the left thigh in patients 2, 3, and 4 and in the left gluteal region in patient 1. The mass over the left gluteal region had been drained surgically. After the drainage, she had remained symptom-free for 15 months. The mass reappeared 3 months later and progressively increased in size over this period. Local examination showed a palpable nontender mass about 4 cm in diameter over the gluteus maximus muscle subcutaneously.
Radiological workup included ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) and were performed for all patients. US was accepted as the primary imaging modality for the classification of the cysts according to Gharbi’s classification [19]. US and MRI were used for the follow-up. Radiological examinations demonstrated a type II hydatid cyst over the gluteus maximus muscle in the subcutaneous fat in patient 1, a type I hydatid cyst in the left lateral vastus muscle in patient 2, and a type III hydatid cyst in semimembranosus and semitendinosus muscles in patient 4. Three hydatid cysts, one type I and two type III, were detected in patient 3, with destruction of the iliac wing and the head of the femur.
Chest X-ray and abdominopelvic CT were alos obtained in search of any possible hydatid cysts located in the body. Muscular involvement of the disease was the primary site in three of the patients, and only one patient had a pulmonary cyst at the right anterior costophrenic sinus (patient 1).
Procedure and Techniques
Informed consent was obtained from all patients before the procedure. One week before and 2 weeks after the percutaneous procedure, the patients were given albendazole orally (10 mg/kg/day) to prevent dissemination from leakage of cyst fluid. Complete blood count, Prothrombin Time (PT), Partial Thromboplastin Time (PTT), International Normalized Ratio (INR), and platelet counts were checked. The patients fasted overnight. All of the patients were sedatized and monitored by an anesthesiologist in the interventional suite for the possible risk of anaphylaxis.
All interventions were performed under sonographic and fluoroscopic guidance. The location of the cyst was defined in two planes by sonography. After the puncture site was chosen and under standard sterile conditions, initial puncture was carried out by US guidance under local anesthesia. The course of the punctured tract was followed on an US monitor.
According to the type of the cyst, the procedure was carried out by either a “catheterization technique with hypertonic saline and alcohol” or a “modified catheterization technique”that we named MoCaT, which is a similar technique to percutaneous evacuation (PEVAC) [11, 20].
One cyst (patient 2) was treated by catheterization technique with hypertonic saline and alcohol. A Seldinger needle was employed for the puncture of the cyst. After entering the cystic cavity, cystic fluid was aspirated up to 35–50% of the estimated volume. The cavity was filled with hypertonic saline (20–30% NaCl), 5–10% less than the aspirated volume. Cyst aspiration and refilling with hypertonic saline was repeated until the complete separation of the endocyst (germinative and laminated membranes) from the pericyst at least for 10 min. Cyst puncturing, aspiration and refilling of the cystic cavity, and separation of the endocyst were monitored continuously by sonography. The next step, a 6F pigtail drainage catheter was placed into the cavity under fluoroscopic guidance and all of the fluid in the cavity was evacuated via the catheter. After flushing the cavity with hypertonic saline, the catheter was fixed on the skin and left for gravity drainage for 24 h. If the daily drainage was less than 10 cc, a cystography was achieved for confirming that there was no leakage outside of the cavity. After that, 95% of absolute alcohol (approximately 50% of the estimated volume) was put into the cavity and left there for 10 min for sclerozing of the cyst wall. Later, all of the fluid was reaspirated and the catheter was withdrawn. No repeat irrigation was performed before withdrawal of the catheter.
Five cysts (patients 1, 3, and 4) in three patients were treated by MoCaT. Until the next day after catheterization, the steps of MoCaT are similar with the steps of the catheterization technique with hypertonic saline and alcohol. In MoCaT, a 14F pigtail catheter was placed instead of 6F catheter to better evacuate the degenerative membranes and daughter cysts (Figs. 1c and 4b). We irrigated these cavities vigorously with hypertonic and normal saline for half an hour twice every day to evacuate the content of these types of hydatid cyst. After ensuring total emptying of the cavity by cystography, 95% of absolute alcohol (approximately 50% of the estimated volume) was put into the cavity for 10 min for sclerosis of the cyst wall. After that, all of the fluid was reaspirated and the catheter was withdrawn.
Follow-up
Follow-up of the patients were performed every 3 months of the first year. In the following years, follow-up was carried out twice a year. In every examination, sonography was performed to assess the changes in size, content, and wall of the cyst. Reduction in size and volume, thickening and irregularity of the wall, decreased fluid content, and solid appearance of the remnant on US examination were accepted as positive criteria of healing [11–13]. Patients were also examined once a year by MRI for the assessment of the changes. Follow-up time ranged between 6 months and 57 months (mean: 34.8 months).
Results
Features of the Imaging Modalities
Pulmonary involvement was found in one patient (patient 1). Hepatic lesion was not observed in any of the four patients. In all of the patients, cystic lesions were demonstrated by US, CT, and MRI. We preferred US and MRI for evaluation of inner structure of the cavities and CT was useful for demonstration of osseous and extraosseous extension of the disease [7–9]. US was the primary modality in determining the viability.
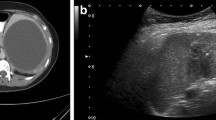
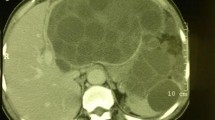
Ultrasound examination demonstrated a type II hydatid cyst with a relatively thick wall in patient 1 over the gluteus maximus muscle in the subcutaneous fat layer. Thorax and abdominopelvic CT examination revealed another hydatid cyst at the right costophrenic sinus. A type I hydatid cyst with a partially split membrane in the left lateral vastus muscle in patient 2 was detected by US (Fig. 2c). In patient 3, US demonstrated a type I cyst and two type III cysts in the left thigh and hip. Floating daughter vesicles were observed in these type III cysts. CT demonstrated the destruction of the ilac wing and the head of the femur with a large soft-tissue component (Fig. 3b). US revealed a type III hydatid cyst with daughter vesicles within the semimembranoous and semitendinous muscles in patient 4.
A 12-year-old boy with a type I hydatid cyst in left lateral vastus muscle. Coronal T1W images before (A) and after (B) gadolinium administration demonstrate hydatid cyst with rim enhancement. US image (C) shows type I hydatid cyst. MR (D) and US (E) images 2 years after the procedure demonstrate residual pseudotumor appearance.
A 60-year-old woman with hydatid cysts in her left thigh and hip. (A) Axial gadolinium enhanced T1-weighted MR image shows the largest cyst with daughter cysts (type III). (B) CT image shows intraosseos extension. (C) Six months after the procedure, two cysts totally disappeared and the T1-weighted MR image shows almost complete resolution of the largest cyst.
Magnetic resonance imaging revealed unilocular and multilocular cystic masses and helped to clarify the extent of the soft-tissue involvement in each patient (Figs. 1a, 2a, 2b, 3a, and 4a). Gadolinium-enhanced T1-weighted MR images demonstrated an enhancing rim representing the pericyst in patients 1, 2, and 4 (Figs. 2a and 2b). No enhancing rim was demonstrated around any of the cysts of patient 3 (Fig. 3a).
A 45-year-old woman with a type III hydatid cyst in her left thigh. Axial T2-weighted MR image (A) and cystogram (B) during the procedure show type III hydatid cysts lesion with multiple daughter cysts. A 14F catheter is in the cystic cavity (C). (D) MR image shows complete resolution of the cysts 3 years after the procedure
Changes in the Cavities After Percutaneous Procedures
The dimensions of the residual cavity were recorded at every sonographic control and an average of 96.1% volume reduction was obtained in six cysts of the four patients. No sign of viability was observed during the follow-up period.
In patient 1, at the first month control, the cystic cavity reduced in size containing only a small amount of fluid. Its dimensions were 22 × 7 × 29 mm at the first month control, 15 × 9 × 10 mm at the third month control, and 10 × 2.5 × 2.3 mm at the six month control. Nine months after the percutaneous treatment, sonography and MR demonstrated only a 5 × 4 × 5 mm simple cystic fluid collection. At the fifth year control, no fluid collection and no hydatid cyst were detected (Fig. 1d).
In patient 2, two cystic compartments connected with each other were detected at the first month control. The first and second compartments measured 15 × 9 × 14 mm and 13 × 8 × 13 mm, respectively. US and MRI examination was repeated at the third month control with no change in the dimensions of cystic compartments. At the fortieth month control, a 11 × 6 × 24 mm pseudotumor with no sign of viability was detected on US and MRI (Figs. 2d and 2e).
In patient 3, follow-up examinations including US and MR were performed at the third and sixth months after the removal of the catheter. Initial volume of the cysts were 1200 cc, 120 cc, and 60 cc. Duration of drainage was 54, 12, and 1 day, respectively. Two cysts disappeared completely and the volume reduction to 5% of the initial volume in the largest cyst was obtained at the third month control MR examination. At the end of the treatment, the patient was completely symptom-free. At the end of the sixth month, no recurrence was detected (Fig. 3c).
In patient 4, granulation tissue measuring 33 × 27 × 17 mm with a small amount of fluid collection was detected on MRI at the first month control.No daughter cyst was noted that was present before treatment. At the third month, the patient was admitted to our institute because of the tenderness and the limitation of motion in the same region. MR and US examinations documented stable changes. Clinical diagnosis was cellulitis and clinical improvement was obtained following a conservative medical therapy. At the third year control, no lesion was detected by US and MRI (Fig. 4d).
Complications, Catheterization Time, and Hospital Stay
Neither mortality nor recurrence was encountered in any patient during or after percutaneous treatment.The mean cathaterization time was 13.7 days, ranging from 1 to 54 days. The mean hospitalization time was 17.8 days, ranging from 1 to 54 days.
The duration of catheterization was 54 days in patient 3. The reason for the prolonged catheterization time was infection of the largest cyst at the 14th day of catheterization. The patient received antibiotics. After 10 days, the drainage material became clear and the patient’s fever subsided. When the drainage volume was less than 5 mL daily, we removed the catheter. That was the only major complication that we observed during the catheterization and hospitalization period. The catheterization time was less than 9 days for all of the other patients.
Patient 4 was admitted to our institute at the third month following the intervention because of the tenderness and the limitation of motion in the same region. A diagnostic puncture was performed but no fluid was obtained by aspiration. Symptoms were attributed to cellulitis and patient was free of symptoms following an oral antimicrobial therapy. This was the only minor complication that we observed during the follow-up period. No additional intervention was required.
Ultrasound and MRI were preferred as the imaging modalities during the follow-up period. The mean follow-up period was 34.8 months, ranging from 6 months to 57 months.
Discussion
Muscles are accepted as a rare and unfavorable site for infective diseases because of the high lactic acid levels. This might be the real reason for the rarity of primary echinococcosis within muscle. US, CT, and MRI can be performed for the diagnosis of soft-tissue hydatid cysts. US and MRI are mainly used to evaluate the inside of the cavity, whereas CT is helpful in demonstrating the osseous and extraosseous extension of the disease [7–9].
Ultrasound is widely used and accepted as a screening imaging modality in the diagnosis of hydatid cysts [1, 3, 4, 6, 7, 19, 21]. We used US as a primary modality in the assessment of viability, during the interventional procedures, and in the follow-up period. The type of the cyst was determined by the US findings according the Gharbi classification. Daughter cysts are the most characteristic feature of echinococcosis and the presence of daughter cysts reveal viability. We detected daughter cysts in three cysts out of six (two cysts of patient 3 and in the cyst in patient 4). Because the double-layered wall is an important-specific feature for the diagnosis of type I hydatid cysts, we used US as the primary modality in the evaluation of the capsule. Therefore, unilocular hydatid cysts can easily be differentiated from simple cysts, as we did in two cysts (type I) (Fig. 2c). A cyst with a detached membrane is also a pathognomonic feature for a hydatid cyst, which we observed in one cyst.
Computed tomography reveals hydatid cysts as sharply defined cysts. The CT appearance of the disease is not pathognomonic and might mimic benign or malignant diseases such as single or multiple metastases, congenital cysts or pseudocysts, hematomas, and other lesions [1, 3–7]. The presence of daughter cysts, germinal membrane detachment, and calcification allows diagnosis. The lesions are usually spherical or oval in shape, with inner attenuation value similar to that of cerebrospinal fluid. There is no rim enhancement unless the cyst is superinfected. CT is superior to MRI in demonstrating wall calcifications. We detected no wall calcification in our patients. CT can also be helpful in the detection of osseous extension of the disease, as in our study (patient 3) (Fig. 3b). We did not modify the treatment in one patient with osseos involvement. Catheterization of the only soft-tissue component was adequate because communication was present between the soft-tissue and osseos components. We believe that screening of the osseous invasion of the disease for soft-tissue hydatid disease is critical for the course of the treatment, so CT should be performed as a part of screening and treatment protocols.
Magnetic resonance imaging features of hydatid disease in soft tissue have rarely been reported [1, 3, 4, 6, 7, 22–27]. MRI can reveal a cystic mass containing daughter cysts and water lilly sign, which are characteristic for hydatid disease [22–27] (Figs. 3a and 4a). We used MRI in the diagnosis and follow-up in monitoring the response to the percutaneous treatment. The cyst wall shows a rim of low signal intensity on both T1- and T2-weighted images. The demonstration of rim is critical in differentiating hydatid cysts from simple epithelial cysts and MRI is superior to CT in the assessment of the wall rim. T2-Weighted images are superior to T1-weighted images in revealing the wall of the hydatid cyst because of the high contrast between the low signal intensity of the wall and the high signal intensity of the fluid content [22, 24]. Although no enhancement was reported in many cases, MR images demonstrated an enhancing rim representing the pericyst on the post-gadolinium T1-weighted images in most of the patients in our study [25]. The daughter cysts were hypointense on T1-weighted and slightly less hyperintense than the mother cysts on T2-weighted images. MRI allowed diagnosis by demonstrating daughter cysts in two of our patients.
The treatment experience of soft-tissue hydatid disease in the literature is limited with surgery [7–9, 22–25]. Adjuvant administration of benzimidazole derivates is widely used in the treatment protocols of surgery. However, the experience with benzimidazole derivates in the treatment of soft-tissue hydatid disease is very limited and results of the medical treatment are far from being curative. Excision of the cystic mass with wide surgical margins is widely accepted as the conventional treatment modality in soft-tissue hydatid disease. Although surgical excision seems to be the main choice of the treatment, it has some major disadvantages, such as the necessity of extensive surgical resection in some cases and the need of general anesthesia [7–9, 22–25].
Percutaneous treatment has become a serious alternative to surgery in patients with hydatid cysts in most of the organs of the body such as the liver, lungs, kidney, orbita, and parotid gland; however, there is no study in the literature describing the results of percutaneous treatment of soft-tissue hydatid cysts [11–13, 15–18]. We percutaneously treated six soft-tissue hydatid cysts in four patients and did not observe any serious major complication or recurrences after a mean follow-up of 34.8 months. Two procedure-related complications were observed, including infection of the cavity and cellulitis, which resolved after antibiotic treatment.
To our knowledge, this is the first study in the literature presenting the results of percutaneous treatment in patients with soft-tissue hydatid cysts. In conclusion, despite small numbers and limited experience, we believe that percutaneous treatment is a safe and effective procedure with successful results in patients with soft-tissue hydatid cysts and should be considered as a serious alternative to surgery.
References
Beggs I (1985) The radiology of hydatid disease. Am J Roentgenol 145:639–648
Bouree P (2001) Hydatidosis: dynamics of transmission. World J Surg 25:4–9
Czermak BV, Unsinn KM, Gotwald T, et al. (2001) Echinococcus granulosus revisited: Radiologic patterns seen in pediatric and adult patients. Am J Roentgenol 177:1051–1056
Haliloglu M, Saatci I, Akhan O, et al. (1997) Spectrum of imaging findings in pediatric hydatid disease. Am J Roentgenol 169:1627–1631
Tuzun M, Hekimoglu B (2001) Various locations of cystic and alveolar hydatid disease: CT appearances. J Comput Assist Tomogr 25:81–87
Dahniya MH, Hana RM, Ashebu S, et al. (2001) The imaging appearances of hydatid disease at some unusual sites. Br J Radiol 74:283–289
Merkle EM, Schulte M, Vogen J, et al. (1997) Musculoskeletal involvement in cystic echinococcosis: Report of eight cases and review of the literature. Am J Roentgenol 168:1531–1534
Ammari FF, Khasawneh Z, Salem MK, et al. (1998) Hydatid disease of the musculoskeletal system. Surgery 124:934–397
Martin J, Marco V, Zidan A, et al. (1993) Hydatid disease of the soft tissues of the lower limb: Findings in three cases. Skeletal Radiol 22:511–514
Mohamed AE, Yasawy MI, Al Karawi MA (1998) Combined albendazole and praziquentel versus albendozole alone in the treatment of hydatid disease. Hepatogastroenterology 45:1690–1694
Akhan O, Dincer A, Gokoz A, et al. (1993) Percutaneous treatment of hydatid cysts with hypertonic saline and alcohol. Invest Radiol 28:121–127
Akhan O, Ozmen MN, Dincer A, et al. (1996) Liver hydatid disease: Long-term results of percutaneous treatment. Radiology 198:259–264
Akhan O, Ozmen MN (1999) Percutaneous treatment of liver hydatid cysts. Eur J Radiol 32:76–85
Battyany I, Herbert ZH, Rostas T, et al. (2006) Successful percutaneous drainage of a giant hydatid cyst in the liver. World J Gastroenterol 12:812–814
Akhan O, Ustunsoz B, Somuncu I, et al. (1998) Percutaneous renal hydatid cyst treatment: Long-term results. Abdom Imaging 23:209–213
Akhan O, Ozmen MN, Dincer A, et al. (1994) Percutaneous treatment of pulmonary hydatid cysts. Cardiovasc Intervent Radiol 17:271–275
Akhan O, Bilgic S, Akata D, et al. (1998) Percutaneous treatment of an orbital hydatid cyst: A new therapeutic approach. Am J Ophtalmol 125:877–879
Akhan O, Ensari S, Ozmen MN (2002) Percutaneous treatment of a parotid gland hydatid cyst: A possible alternative to surgery. Eur Radiol 12:597–599
Gharbi HA, Hassine W, Brauner MW, et al. (1981) Ultrasound examination of hydatid liver. Radiology 139:459–463
Schipper HG, Lameris JS, van Delden OM, et al. (2002) Percutaneous treatment of multivesicular echinococcal cysts with or without cystobiliary fistulas which contain non-drainable material: First results of a modified PAIR method. Gut 50:718–723
Niron EA, Ozer H (1981) Ultrasound appearances of liver hydatid disease. Br J Radiol 54:335–338
Chevalier X, Rhamouni A, Bretagne S, et al. (1994) Hydatid cysts of the subcutaneous tissue without other involvement: MR imaging features. Am J Roentgenol 163:645–646
Cannon CP, Nelson SD, Panosian CB, et al. (2001) Soft tissue echinococcosis: A report of two cases and review of the literature Clin Orthop Relat Res 385:186–191
Guthrie JA, Lawton JO, Chalmers AG (1996) Case report: the MR appearances of primary intramuscular hydatid disease. Clin Radiol 51:377–399
Salai M, Apter S, Dudkiewicz I, et al. (1999) Magnetic resonance imaging of hydatid cyst in skeletal muscle. J Comput Assist Tomogr 23:331–332
Dudkiewicz I, Salai M, Apter S (1999) Hydatid cyst presenting as a soft-tissue thigh mass in a child. Arch Orthoped Trauma Surg 119:474–475
Comert RB, Aydingoz U, Ucaner A, et al. (2003) Water-lilly sign on MR imaging of primary intramuscular hydatidosis of sartorius muscle. Skeletal Radiol 32:420–423
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akhan, O., Gumus, B., Akinci, D. et al. Diagnosis and Percutaneous Treatment of Soft-Tissue Hydatid Cysts. Cardiovasc Intervent Radiol 30, 419–425 (2007). https://doi.org/10.1007/s00270-006-0153-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-006-0153-1