Abstract
Coronary heart disease (CHD) is one of the most serious public health problems. However, few studies have focused on the effects of exposure to particulate matter and gaseous air pollutants on CHD. This study aimed to explore the relationship between air pollutants and the number of hospitalized patients with CHD in Lanzhou, and we collected daily data on the number of hospitalized patients with CHD, daily air pollutants, and meteorological factors from 2013 to 2020. A distributed lag nonlinear model (DLNM) combined with a quasi-Poisson regression model was applied to evaluate the relationship between air pollutants and the number of hospitalized patients with CHD. The results indicated that the hysteresis effect of all pollutants except O38h reached its maximum at lag3, and the relative risk of coronary heart disease admission was 1.0014 (95%CI: 1.0004, 1.0023), 1.0003 (95%CI: 1.0000, 1.0006), 1.0020 (95%CI: 1.0004, 1.0035), and 1.0053 (95%CI: 1.0026, 1.0080) when PM2.5, PM10, NO2, and SO2 concentrations were increased by 10 μg/m3, respectively. Each 1 mg/m3 increase in CO concentration was associated with a relative risk of coronary heart disease; hospitalization risk was 1.1076 (95%CI: 1.0530, 1.1650). We observed a relative risk of 0.9991 (95%CI: 0.9986, 0.9999) for each 10 μg/m3 increase in O38h for coronary heart disease admission at lag1. Women and elderly were more susceptible to the impact of air pollution, and the impact was greater during cold seasons. Our results indicate that air pollution increased the risk of hospitalization for CHD in a short term. The research findings can provide strategic insights into the impact of current and future air pollution on CHD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary heart disease (CHD) is a heart disease caused by stenosis or occlusion of coronary artery lumen. According to the American Heart Association, coronary heart disease is the leading cause of death globally [1], and the cases of coronary heart disease would increase nearly 100% by 2030 [2]. According to the data released by the World Health Organization in 2019, the number of people who die from cardiovascular diseases each year accounts for 31% of the total number of deaths worldwide, more than any other cause of death [3]. According to the Health China Action (2019–2030), there are currently 11 million patients with coronary heart disease in China, and more than 700,000 patients die of coronary heart disease. Coronary heart disease, with its high incidence rate, high mortality, and high treatment costs, has seriously restricted the further improvement of people’s living standards.
Lanzhou was one of the cities with the most serious air pollution in China and even in the world. Sand and dust weather was common in Lanzhou in spring, but after decades of treatment, the frequency of sand and dust occurrence has been greatly reduced, and the level of particulate pollution has been greatly reduced. At the same time, Lanzhou is a famous chemical city, and the car ownership is high. By the end of 2021, the car ownership in Lanzhou has exceeded 1.03 million, which also makes the air condition in Lanzhou not optimistic. To sum up, Lanzhou is a city with characteristic air pollution. Therefore, we conducted a study on the relationship between air pollutants and coronary heart disease in Lanzhou.
The prevalence of coronary heart disease in 2019 was 24 times that in 1980 [4]. Facing the high burden and high pollution level of coronary heart disease, it is urgent to clarify the relationship between air pollution and coronary heart disease.
Many evidences show that air pollutants may have delayed effects on health outcomes, and the exposure-response relationship is usually nonlinear [5]. Distributed lag nonlinear model (DLNM) is more feasible and flexible among the various methods that have been proposed to deal with delays. It has been widely used to analyze the impact of air pollution on various healthy tissues in recent years [6, 7]. But few studies have applied this model to evaluate the relationship between exposure to six air pollutants (PM2.5, PM10, NO2, SO2, O38h, CO) and the risk of coronary heart disease.
In this study, DLNM was used to estimate the exposure-lag response relationship between the concentration of air pollutants and the risk of coronary heart disease; we also aim to provide strategic insights into the current and future impact of air pollution on CHD.
Material and Methods
Study Area and Period
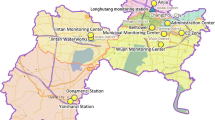
We conducted this study in Lanzhou (102°35′-104°34′E, 35°34′-37°07′N), Gansu Province, from 1 Jan 2013 to 31 Dec 2020 (2922 days). Lanzhou has five districts and three counties under its jurisdiction (Figure S1). In 2021, Lanzhou has a permanent population of 4.3843 million. Lanzhou is located in the geometric center of northwest China and Chinese Mainland, in the middle of Gansu Province. The Yellow River flows from the southwest to the northeast, crosses the whole territory, cuts through mountains, and forms a beaded valley with valleys and basins. Lanzhou has a temperate continental climate. There is no extreme heat in summer and no severe cold in winter. It is a famous summer resort.
The Data of Coronary Heart Disease
The inpatient data of coronary heart disease from January 1, 2013, to December 31, 2020 came from the admission and discharge data of Lanzhou local residents diagnosed as coronary heart disease in seven class III class A hospitals in Lanzhou, and these data include gender, age, home address, hospitalization date, discharge date, hospitalization diagnosis, and other information. According to the International Classification of Disease, 10th revision (ICD-10), all cases coded as coronary heart disease (I20–I25) were included in this study. The SPSS 27.0.0 was used to logically correct the inpatient data and eliminate the missing and duplicate data such as gender, age, date of visit, ICD code. Screening is carried out according to the registered residential address information of patients, and patients whose residential address is not Lanzhou City will be eliminated. Non-residents will be eliminated through the registered home address information of patients, so as to ensure that the research objects are from the local permanent residents of Lanzhou City.
Air Pollutants and Meteorology
The data of air pollutants (PM2.5, PM10, NO2, SO2, O38h, CO) were collected from National Environmental Monitoring Station. There are four national air-quality monitoring stations in Lanzhou (Biological Products Institute, Railway Design Institute, Worker Hospital, and LanLian Hotel). These monitoring stations were far away from major roads, industrial sources, and pollutants, ensuring that the monitoring results reflect the overall air pollution level in Lanzhou. The measured data included 24-h average concentrations of PM2.5, PM10, NO2, SO2, CO, and 8-h maximum average concentrations of O3, and then the average of the four monitoring stations was used as the daily concentrations for each air pollutant, and all measurements of the ambient air pollutants were operated according to the China National Quality Control.
The type of all data was the daily municipal average. Ozone data was the maximum continuous 8-h average ozone concentration in a day
Statistical Analysis
The daily number of inpatients with coronary heart disease was classified by sex and age, and the air pollutants and meteorological factors were expressed by maximum (Max), minimum (Min), median, mean, standard deviation (SD), and inter quartile range (IQR). Spearman’s rank correlation analysis was used to estimate the relationship between air pollution and meteorological factors. The harmful effects of air pollutants on health were delayed, and the relationship was often nonlinear [8]. Therefore, DLNM was used to analyze the correlation between the daily count of coronary heart disease and the concentration of air pollutants. Both the exposure-response relationship and the hysteresis-response relationship were explained in one model [9, 10]. The event of hospitalization for coronary heart disease was a low-probability event, consistent with the occurrence of Poisson [9]. Therefore, DLNM combined with quasi-Poisson regression model was applied to the time series analysis of the impact of environmental air pollution [11]. Therefore, the specific formula is as follows:
where t is the lag day; Yt means the number of inpatients for CHD on day t; E(Yt) means the expected count of CHDs at day t; α is the intercept; β represents the regression coefficient; ns is natural spline function; ns(Time) is natural cubic spline function used to control the long-term trend and seasonality of time; ns(Temp) is natural cubic spline function to control the average temperature; ns(Rh) is natural spline function to control the daily relative humidity; Holiday was utilized to control for the effect of holidays; DOW represents the indicator variable for the “day of the week effect”; df is the degree of freedom. Using ns fitted time functions, the choice of degrees of freedom is more critical, combining previous studies to choose df = 7, controlling for long-term trends and seasonality. In our study, we choose the degrees of freedom based on the minimum value of Quasi Akaike Information Criterion (Q-AIC), and a smaller value of Q-AIC indicates a better model.
The model calculated the relative risk (RR) and 95% confidence interval (CI) for each 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, and O38h and 1 mg/m3 increase in CO under different conditions from 2013 to 2020. First, we used the single-pollution model to study the impact of different air pollutants on coronary heart disease. We set the maximum lag time to 7 days, fully study the short-term effect of air pollutants on coronary heart disease, and observe the impact of different lag days, including single-day lag (lag0–lag7) and cumulative lag (lag0-1~lag0-7). After that, we conducted subgroup analysis and divided hospitalized patients with coronary heart disease into different subgroups according to sex and age. Finally, in order to explore the impact of seasonal factors, we divided the year into cold seasons (January, February, March, October, November, and December) and warm seasons (April, May, June, July, August, and September) for analysis.
The R statistic software (version 4.2.1) and the “dlnm” package were adopted for all statistical analyses, and it is considered statistically significant when P < 0.05.
Results
Table 1 shows that from 2013 to 2020, 88,805 in-patients with coronary heart disease were included in this study, including 59,507 males (67.01%), 29,298 females (23.99%), 46,562 patients younger than 65 years old (52.43%), and 42,243 patients older than 65 years old (47.57%). And during the study, the average daily concentration of air pollutants from 2013 to 2020 was 49.70 μg/m3 (PM2.5), 114.45 μg/m3 (PM10), 21.64 μg/m3 (SO2), 45.94 μg/m3 (NO2), 1.16 mg/m3 (CO), and 83.80 μg/m3 (O38h). The average daily temperature and relative humidity were 11.13 °C and 51.19%.
Figure 1 shows the daily concentrations of different air pollutants in Lanzhou from 2013 to 2020, which showed a stable fluctuation, and the daily concentrations of O38h and NO2 showed an upward trend. The daily concentration of air pollutants had obvious seasonality. The daily concentrations of PM2.5, SO2, and CO showed a downward trend; the daily concentrations of PM10 showed an upward trend. The concentration of NO2, PM2.5, PM10, SO2, and CO was the highest in winter and the lowest in winter. However, O38h showed the opposite trend and reached its peak in summer.
We also performed Spearman’s correlation analysis for different air pollutants and meteorological factors, and the results show that the concentration of PM2.5, PM10, SO2, and O38h was positively correlated with each other, PM10 and PM2.5 were highly correlated (r = 0.850), followed by PM2.5 and SO2 (r = 0.681), and NO2 was lowly correlated with PM10, PM2.5, and SO2. The concentration of CO was negatively correlated with other air pollutants. Except for O3-8h, all pollutants were negatively correlated with temperature, and the correlation coefficients ranged from − 0.578 to − 0.0358 (Table S1).
Figure 2 shows the exposure-response relationship between the daily concentration of pollutants and the number of inpatients with coronary heart disease. The relationship between the two shows a linear curve without threshold. The risk of hospitalization for coronary heart disease increases with the increase of the concentration of air pollutants (PM2.5, PM10, SO2, NO2, CO), while the trend of O38h is opposite.
Figure 3a shows the effect of 10 μg/m3 increase in air pollutant (PM2.5, PM10, SO2, NO2, and O38h) concentration and each 1 mg/m3 increase in CO increment in single-pollutant exposure at different lag day; except for O38h, all air pollutants contributed to the increase of the number of inpatients due to coronary heart disease. Among the five pollutants, NO2 showed the strongest effect on the third day of delay, namely, CO (RR = 1.1076, 95% CI 1.0530–1.1500), SO2 (RR = 1.0053, 95% CI 1.0026–1.0080), PM2.5 (RR = 1.0014, 95% CI 1.053–1.165), PM10 (RR = 1.0003, 95% CI 1.0001–1.0006), and NO2 showed the strongest effect on the fourth day (RR = 1.0020, 95% CI 1.0004–1.0035), while O38h showed the strongest effect on the 7th day, specifically (RR = 0.9999, 95% CI 0.9992–1.0006) (Table S3). Among all six pollutants, CO shows the strongest effect, while NO2 and PM10 have a weak effect. (The specific values can be seen in the supplementary table)
a Relative risk of single-day lag of CHD admissions in different gender and age for each 10 μg/m3 increase in air pollutant (PM2.5, PM10, SO2, NO2, and O38h) concentration and each 1 mg/m3 increase in CO. b Relative risk of cumulative-day lag of CHD admissions for each 10 μg/m3 increase in air pollutant (PM2.5, PM10, NO2, SO2, and O38h) concentration and each 1 mg/m3 increase in CO
Figure 3 b shows the relationship between cumulative lag day and relative risk of CHD admissions for each 10 μg/m3 increase in air pollutant (PM2.5, PM10, SO2, NO2, and O3-8h) concentration and each 1 mg/m3 increase in CO. Except for O38h, other pollutants will increase the number of inpatients with coronary heart disease, and all pollutants except NO2 will reach a higher risk on the third day, namely, PM2.5 (RR = 1.0019, 95% CI 1.0007–1.0020), PM10 (RR = 1.0003, 95% CI 0.9999–1.0006), SO2 (RR = 1.0046, 95% CI 1.0015–1.0078), and CO (RR = 1.1397, 95% CI 1.0774–1.2055), and the relative risk of NO2 will reach the maximum on the fourth day (RR = 1.0047, 95% CI 1.0029–1.0064). However, O38h showed the strongest effect on the 4th day, specifically (RR = 0.9984, 95% CI 0.9974–0.9994) (Table S4). Among all six pollutants, CO has the strongest effect. NO2, SO2, and PM2.5 have significant cumulative effects on the risk of coronary heart disease, while PM10 has a weak effect. (The specific values can be seen in the supplementary table)
We grouped the hospitalized patients with coronary heart disease according to sex and age and carried out subgroup analysis. The details can be seen in Fig. 4a and b. We find that when the concentration of five air pollutants increases by 10 μg/m3 and the concentration of CO increases by 1 mg/m3, the risk of hospitalization due to coronary heart disease is higher in men than in women, and the risk of elderly people older than 65 years old is higher than that of adults younger than 65 years old. At the same time, we also divided the year into cold season and warm season and analyzed the number of inpatients due to coronary heart disease in these two periods. We found that the risk of hospitalization in cold season was higher than that in warm season. On this basis, we divided the risk of hospitalization due to coronary heart disease by sex and age and found that the risk of hospitalization due to coronary heart disease was higher for men than for women, and the risk of elderly people older than 65 years old was higher than that of adults younger than 65 years old, which was the same as the results of the above subgroup analysis. (See the supplementary Figure S2-S3)
a Relative risk of single-day lag of CHD admissions in different gender and age for each 10 μg/m3 increase in air pollutant (PM2.5, PM10, SO2, NO2, and O38h) concentration and each 1 mg/m3 increase in CO. b Relative risk of cumulative-day lag of CHD admissions in different gender and age for each 10 μg/m3 increase in air pollutant (PM2.5, PM10, SO2, NO2, and O38h) concentration and each 1 mg/m3 increase in CO
The contour map of the relative risk (RR) of coronary heart disease and the concentration of air pollutants and the delayed days is shown in Fig. 5. As the concentration of pollutants increases, the risk of coronary heart disease increases. However, the change trend of each pollutant is different.
We added additional pollutants to construct the double-pollutant model (Table S2). Except for CO, all other multi-pollutant models had a higher effect on CHD admissions.
The detailed results of the sensitivity analysis are shown in the supplementary documents. (Tables S3). In the range of 6–10, the change of df has no significant effect on the connection between air pollutions with CHD.
Discussion
This study used the DLNM to study the short-term correlation between air pollutant exposure and coronary heart disease admission rate in Lanzhou City, Gansu Province, from 2013 to 2020. The results indicated that short-term exposure to PM2.5, PM10, SO2, NO2, and CO are positively correlated with an increase in hospitalization rates for coronary heart disease, and there is a significant lag effect of air pollutants on the onset of coronary heart disease. Among them, except for O3, all pollutants have a slightly greater impact on women than men, and elderly people aged ≥ 65 are more susceptible to the impact of air pollutants. There are differences between cold and warm seasons. In cold seasons, people are more affected by air pollutants. There is a significant correlation between the increase in air pollutant concentration and the incidence of CHD in the entire population.
The concentrations of six air pollutants are 49.70 μg/m3 (PM2.5), 114.45 μg/m3 (PM10), 21.64 μg/m3 (SO2), 45.94 μg/m3 (NO2), 1.16 mg/m3 (CO), and 83.80 μg/m3 (O38h), respectively, with concentrations of PM2.5, PM10, and NO2 higher than the World Health Organization’s air quality guidelines (15 μg/m3, 45 μg/m3, 25 μg/m3), while SO2, CO, and O38h comply with the World Health Organization’s air quality standards. PM2.5 and PM10 exceed the standard by 3–4 times, making them the main pollutants in Lanzhou.
In our study, we found that PM2.5 has short-term effects and affects coronary heart disease admission. In the single-pollutant model, the impact is greatest at lag 2(RR = 1.0014, 95% CI 1.0002, 1.0019). Elderly people are more susceptible to the impact of PM2.5 (RR = 1.0019, 95% CI: 1.0000, 1.0008). Meanwhile, in warm seasons, women are more susceptible to the influence of particulate matter such as PM2.5. Studies have also confirmed that when PM2.5 increases by 10 μg/m3, female is associated with an increased risks in coronary heart disease, which coincides with our research findings [12]. Elevated PM2.5 levels may lead to coronary heart disease, as PM2.5 pollution is associated with changes in hemodynamics [13], it may cause an increase in plasma viscosity, heart rate acceleration, and so on [14]. In addition, the impact of particulate matter pollution on health varies with different particle sizes, with different physical properties, chemical components, and biological activities [15, 16]. In our study, an increase in PM10 concentration had a greater impact on women. Because women have smaller coronary arteries, microvascular dysfunction seems to be more common [17]. These results are consistent with some previous studies [18, 19].
This study found that the concentration of NO2 was increasing year by year. In the single pollution model, every 10% increase of NO2 μg/m3, the impact is greatest at lag 2 (RR = 1.0020, 95% CI 1.0004, 1.0035). The risk for women is higher than that for men, and the risk for old people (RR = 1.0021, 95% CI = 1.0003, 1.0038) is higher than adult. At the same time, the incidence risk in cold season is significantly higher than that in warm season. At present, it is unclear why there is gender difference in the impact of NO2 on cardiovascular disease mortality. Elderly people are more susceptible to the impact of NO2, mainly due to their low immune system and high incidence of related basic diseases such as heart and lung [20]. Our research results are also consistent with other previous studies [21, 22].
For SO2, our conclusion is that in a single pollution model, we observed a relative risk of 1.0053 (95%Cl 1.0026,1.0080) for each 10μg/m3 increase in SO2 for coronary heart disease admission at lag2, and it has a greater impact on the elderly and men, which is consistent with most previous studies. In Beijing, the relative risk (95% CI) of admission to cardiovascular emergency rooms for every 10 mg/m3 of SO2 is 1.008 (95%CI: 0.999, 1.018) [23]. In the atmosphere of six cities in China, the acute impact of sulfur dioxide on population mortality can be observed. We can observe that the impact of SO2 on CHD mortality varies, but there is a clear correlation [24]. At the same time, research has found that inhalation of SO2 in mice leads to an increase in lipid peroxidation levels in organs, and a significant decrease in SOD, GSH-Px enzyme activity, and GSH content, leading to oxidative stress and significant changes in antioxidant activity in nine organs of mice. In addition, studies have found that SO2 derivatives can cause changes in Ca2+, K+, and Na+ and channels in myocardial cells, which have adverse effects on the cardiovascular system.
Ozone has shown a short-term protective effect in our research. The underlying mechanism needs further study. Some previous studies have proved that ozone can play the role of “protector” in some cases. Inject high-pressure ozone into the patient’s blood and then inject it back into the patient’s body. It can effectively improve the level of blood lipids and myocardial markers and improve exercise tolerance and cardiac ejection function. High-pressure ozone can also reduce the inflammatory reaction of vascular wall and the damage to vascular endothelium [25,26,27]. However, low concentration of ozone can inhibit enzyme activity, affect lipoprotein metabolism, induce systemic inflammatory reaction, and cause cardiovascular related diseases [28]. Therefore, ozone is a relatively contradictory air pollutant.
Our study found that CO was positively correlated with respiratory admission rate, and the relationship was the strongest in the cumulative lag model. When CO increases by 1 mg/m3, the impact is greatest when the lag is 0–3 days (RR = 1.1397, 95% CI= 1.0774, 1.2055). At the same time, in the cumulative lag model, the effect of CO on women (RR = 1.1797, 95% CI = 1.1044, 1.2601) is higher than that of men, and the effect on older people older than 65 years old (RR = 1.1547, 95% CI = 1.0862, 1.2276) is higher than that of adults younger than 65 years old (RR = 1.1266, 95% CI = 1.0593, 1.1982) (see supplementary table). Many previous studies have shown that low exposure to carbon monoxide can increase blood carboxyhemoglobin concentration and aggravate myocardial ischemia [29]. Because the affinity of hemoglobin to carbon monoxide is more than 200 times that of oxygen, exposure to carbon monoxide will combine with hemoglobin, thus reducing the delivery of oxygen, leading to adverse health reactions [30]. Bell and his colleagues reported a positive and significant correlation between the day’s exposure to carbon monoxide and the increased risk of hospitalization for cerebrovascular disease in the USA [31].
This study has the following advantages: First, this study was carried out in the whole city of Lanzhou, based on the total number of patients with coronary heart disease in seven tertiary hospitals in Lanzhou within 8 years, with a large sample size and complete data. Compared with some sample surveys, this study has no deviation and the results are stable. Secondly, DLNM was adopted in this study. DLNM can flexibly and conveniently analyze the lag effect between air pollution and disease, so as to conduct in-depth quantitative analysis of the relationship between the two. At the same time, quasi-Poisson regression is adopted, which has relatively loose requirements for variables. However, there are still some shortcomings in this study: First, coronary heart disease is a kind of disease caused by coronary atherosclerosis, and there are many subtypes. In our study, we only studied this kind of disease and did not further explore the relationship between air pollution and its subtypes; Secondly, our research had only explored the overall relationship between air pollution and the number of inpatients with coronary heart disease in Lanzhou. However, many people are exposed to more serious air pollution due to their occupational particularity, and our research has not taken this into account.
Conclusion
The results of this study show that exposure to PM2.5, PM10, NO2, SO2, and CO is positively correlated with the risk of CHD, while exposure to O3 is associated with a reduced risk of CHD. Elderly people have a higher risk of developing diseases than adults. Except for O3, women exposed to other pollutants have a higher risk of developing the disease than men. The interaction between air pollutants and CHD and its potential mechanisms needs further research. At the same time, more attention should be paid to the dangers brought by air pollution. Active measures should be taken to reduce the concentration of environmental air pollutants, thereby reducing the occurrence of CHD.
Data Availability
Air pollution data for this study are available at the China Environmental Monitoring General Station http://www.cnemc.cn/. Meteorological data can be accessed at http://data.cma.cn, which is managed by the National Meteorological Information Centre of China. Clinical hospital admission data are not available to the public. All analyses in this study were performed using R version 4.2.1 software, and licensing and other information are available at https://www.r-project.org. The package used to construct the distributed lag nonlinear model (DLNM) is publicly available at https://cran.r-project.
Abbreviations
- CHD:
-
Coronary heart disease
- DLNM:
-
Distributed lag non-linear models
- RR:
-
Relative risk
- SD:
-
Standard deviation
- IQR:
-
Inter quartile range
- Q-AIC:
-
Quasi Akaike information criterion
- CI:
-
Confidence intervals
- WHO:
-
World Health Organization
References
Lozano R, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Benjamin EJ, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528.
Li W, et al. Prediction of coronary heart disease based on combined reinforcement multitask progressive time-series networks. Methods. 2022;198:96–106.
Xu J, et al. Study on the association between ambient air pollution and daily cardiovascular death in Hefei, China. Environ Sci Pollut Res Int. 2020;27(1):547–61.
Zhu G, et al. The association between ambient temperature and mortality of the coronavirus disease 2019 (COVID-19) in Wuhan, China: a time-series analysis. BMC Public Health. 2021;21(1):117.
Allen MJ, Sheridan SC. Mortality risks during extreme temperature events (ETEs) using a distributed lag non-linear model. Int J Biometeorol. 2018;62(1):57–67.
Yu H, et al. Influence of coarse particulate matter on chickenpox in Jiading District, Shanghai, 2009-2018: a distributed lag non-linear time series analysis. Environ Res. 2020;190:110039.
Zhu S, et al. Ambient air pollutants are associated with newly diagnosed tuberculosis: A time-series study in Chengdu, China. Sci Total Environ. 2018;631-632:47–55.
Zhang Q, et al. Associations between weekly air pollution exposure and congenital heart disease. Sci Total Environ. 2021;757:143821.
Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med. 2010;29(21):2224–34.
Warner P. Poisson regression. J Fam Plann Reprod Health Care. 2015;41(3):223–4.
Leiva GM, et al. A five-year study of particulate matter (PM2.5) and cerebrovascular diseases. Environ Pollut. 2013;181:1–6.
Peters A, et al. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103(23):2810–5.
Gold DR, et al. Ambient pollution and heart rate variability. Circulation. 2000;101(11):1267–73.
Huang YC, et al. Comparison of gene expression profiles induced by coarse, fine, and ultrafine particulate matter. J Toxicol Environ Health A. 2011;74(5):296–312.
Faiz Y, et al. Occurrence and profile of organophosphorus compounds in fine and coarse particulate matter from two urban areas of China and Pakistan. Environ Pollut. 2018;233:26–34.
Dockery DW, Stone PH. Cardiovascular risks from fine particulate air pollution. N Engl J Med. 2007;356(5):511–3.
Zhang Y, et al. Association between ambient air pollution and hospital emergency admissions for respiratory and cardiovascular diseases in Beijing: a time series study. Biomed Environ Sci. 2015;28(5):352–63.
Rodopoulou S, et al. Air pollution and hospital emergency room and admissions for cardiovascular and respiratory diseases in Doña Ana County, New Mexico. Environ Res. 2014;129:39–46.
Guo Y, et al. Time series analysis of ambient air pollution effects on daily mortality. Environ Sci Pollut Res Int. 2017;24(25):20261–72.
Yang Y, et al. Long term exposure to air pollution and mortality in an elderly cohort in Hong Kong. Environ Int. 2018;117:99–106.
Huang J, et al. The burden of ischemic heart disease related to ambient air pollution exposure in a coastal city in South China. Environ Res. 2018;164:255–61.
Ma Y, et al. Short-term effects of ambient air pollution on emergency room admissions due to cardiovascular causes in Beijing, , China. Environ Pollut. 2017;230:974–80.
Zeng Q, et al. Acute effects of SO2 and NO2 on mortality in the six cities of China. Zhonghua Yu Fang Yi Xue Za Zhi. 2015;49(12):1085–91.
Bocci V, et al. The ozone paradox: ozone is a strong oxidant as well as a medical drug. Med Res Rev. 2009;29(4):646–82.
Chuang GC, et al. Pulmonary ozone exposure induces vascular dysfunction, mitochondrial damage, and atherogenesis. Am J Phys Lung Cell Mol Phys. 2009;297(2):L209–16.
Xia Y, et al. Effects of personal short-term exposure to ambient ozone on blood pressure and vascular endothelial function: a mechanistic study based on DNA methylation and metabolomics. Environ Sci Technol. 2018;52(21):12774–82.
Faridi S, et al. Long-term trends and health impact of PM(2.5) and O(3) in Tehran, Iran, 2006-2015. Environ Int. 2018;114:37–49.
Liu C, et al. Ambient carbon monoxide and cardiovascular mortality: a nationwide time-series analysis in 272 cities in China. Lancet Planet Health. 2018;2(1):e12–8.
Prockop LD, Chichkova RI. Carbon monoxide intoxication: an updated review. J Neurol Sci. 2007;262(1-2):122–30.
Bell ML, et al. Emergency hospital admissions for cardiovascular diseases and ambient levels of carbon monoxide: results for 126 United States urban counties, 1999-2005. Circulation. 2009;120(11):949–55.
Funding
Supported by the Fundamental Research Funds for the Central Universities (lzujbky-2020-9).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
We declare that we have no known competing interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 3.94 mb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, M., Yu, J., Zhu, A. et al. Association Between Air Pollution and Coronary Heart Disease Hospitalizations in Lanzhou City, 2013–2020: a Time Series Analysis. J Urban Health 100, 1246–1257 (2023). https://doi.org/10.1007/s11524-023-00797-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-023-00797-w