Abstract
Balneotherapy (BT) is one of the most commonly used non-pharmacologic complementary therapies for different rheumatic diseases. Its beneficial properties probably derived from a combination of mechanical, thermal, and chemical effects, but the exact mechanism of action is not elucidated. This review aimed at summarizing the current knowledge about the effects of BT, and identifying its possible mechanism of action in different rheumatic diseases. Pubmed and Scopus were used to perform a search of the literature to extract articles including terms related to BT and rheumatic diseases published in the period from 2010 to 2021. We selected pre-clinical studies, randomized controlled trials, and clinical trials. The results of clinical studies confirmed the beneficial properties on different mediators and factors of inflammation, oxidative stress, cartilage metabolism, and humoral and cellular immune responses in patients affected by chronic degenerative musculoskeletal disorders. The data derived from OA and RA-induced murine models revealed the efficacy of different BT treatments in decreasing pain, inflammation, and improving mobility, as well as in reducing the expression of matrix-degrading enzymes and markers of oxidative stress damage. Different in vitro studies analyzed the potential effect of a mineral water, as a whole, or of a mineral element, demonstrating their anti-inflammatory, antioxidant, and chondroprotective properties in OA cartilage, synoviocytes and chondrocytes, and osteoblast and osteoclast cultures. The presented data are promising and confirm BT as an effective complementary approach in the management of several low-grade inflammation, degenerative, and stress-related pathologies, as rheumatic diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Balneotherapy (BT) comprises a broad spectrum of therapeutic modalities including hydrotherapy, bath in mineral water, mud pack therapy, or the use of edaphic remedies usually practiced in health resorts (Fioravanti et al. 2017).
In the recent years, BT has been widely used as non-pharmacological intervention, in addition to other options (i.e., physiotherapy and exercise), for the treatment of different rheumatic diseases for its beneficial effect on pain, function, quality of life, and its favorable economic profile (Katz et al. 2012; Ciani et al. 2017; Antonelli et al. 2018; Maccarone et al. 2021a).
The major rheumatic conditions that are frequently treated by BT with a high rate of success are osteoarthritis (OA), fibromyalgia syndrome (FS), low back pain, and spondyloarthritis (Fioravanti et al. 2015a, 2018a; Karagülle and Karagülle 2015; Forestier et al. 2017, 2021; Király et al 2020).
The mechanism of action of BT is still not fully understood and it is difficult to distinguish the efficacy of the thermal method from the benefits that could be derived from a stay in the spa environment (Fioravanti et al. 2011a). The therapeutic activities are probably the results of a combination of mechanical, thermal, chemical, and microbiological factors. A distinction can be made between non-specific and specific mechanisms. Non-specific or hydrotherapic mechanisms are ascribable to the physical properties of the water and are commonly related to the simple baths in hot tap water, while specific or hydromineral effects depending on the organic and inorganic compounds as well as on the community of microorganisms present in mineral water, in mud, or in other peloids with therapeutic properties (Morer et al. 2017; Szabó and Varga 2020; Carretero 2020a, b). Physical properties are well known, while specific effects are difficult to identify and to assess and, therefore, not completely elucidated. Finally, another partially unsolved question concerns the absorption of mineral elements into the skin and subsequently their concentration into the circulation (Shani et al. 1985; Carbajo and Maraver 2017).
The body of evidence substantiating the effectiveness of BT has been increasing progressively during the last decade with a number of preclinical and clinical studies which can allow us to better understand the mechanisms of action of BT in rheumatic disorders.
The purpose of this narrative review was to summarize the highest scientific evidence investigating the possible mechanism of action of BT in rheumatic diseases from 2010 to 2021.
Methods
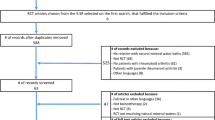
A research from the literature about clinical and pre-clinical studies investigating the role of BT in rheumatic disease conditions has been performed examining the period from January 2010 to September 2021. The strategy used to select the papers consisted in a search in scientific databases Pubmed, Scopus, and Google Scholar.
The keywords selected for the research were “balneotherapy,” “spa therapy,” “mud,” “mud-bath therapy,” “peloidotherapy” in combination with “rheumatic diseases,” “osteoarthritis,” “rheumatoid arthritis,” “fibromyalgia,” “low-back pain,” and “clinical trial,” “clinical studies,” “animal models,” “cell cultures,” and “in vitro studies.”
Studies were considered eligible if were published from 2010 to the present totally written in English language, and classified as original articles whose main objectives were to analyze the effects of BT.
On the contrary, we excluded all article published prior 2010, presented as review, and written in other languages than English.
Results
BT and systemic pro-inflammatory mediators
In the past, different studies have shown the reduction induced by a cycle of mud-bath therapy in circulating levels of Prostaglandin E2 (PGE2), Leukotriene B4 (LTB4), Interleukin (IL)-1β, Tumor Necrosis Factor (TNF)-α, and IL-6, involved in inflammation and chondrolysis occurring in different rheumatic diseases (Bellometti et al. 1997; Basili et al. 2001; Ardiҫ et al. 2007). Likewise, specific TNF receptor serum values decrease after mud therapy, indicating a modulation of the TNF-mediated inflammatory response (Bellometti et al. 2002). In the context of BT, TNF and IL-1β seem to be the most relevant cytokines responsible for its effectiveness (Tenti et al. 2015; Gálvez et al. 2018a).
In a recent experience, Ortega et al. (Ortega et al. 2017) demonstrated the anti-inflammatory and inflammatory/stress responses regulatory effects of 10-day course of BT with mineral-medicinal water, together with mud applications, in patients with OA, showing a significant reduction of serum levels of a panel of cytokines, IL-1β, TNF-α, IL-6, IL-8, and TGF-β, after the treatment. In the same paper, they evaluated some stress biomarkers, such as cortisol and extracellular 72-kDa heat shock protein (eHsp72) (Table 1). The authors reported an increase of cortisol after BT, probably due to the thermal stimulus, that can contribute to reduce the release of cytokines and pro-inflammatory mediators, together with an unexpected reduction in the systemic concentration of eHsp72 that, also, can justify the decrease in inflammatory cytokines (Ortega et al. 2017). Although thermal stress can induce the “heat shock response” and, therefore, the potential synthesis and release of Hsp, a possible reason for the decrease in the circulating eHsp72 after mud therapy could be the physiological adaptation to stress by repeated hyperthermia sessions (Gálvez et al. 2018a; Uzunoğlu et al. 2017; Ortega et al. 2018). This phenomenon can contribute to the beneficial effects of BT through hormetic mechanisms (Gálvez et al. 2018a).
Analyzing the effects of mud-bath therapy on the IL-8/TGF-β ratio as an inflammatory index, it has been found that this ratio presents a reduction, revealing a further decrease in the concentrations of the potent pro-inflammatory chemokine IL-8 (Gálvez et al. 2018b). Indeed, reduced systemic IL-8 and TGF-β concentrations correlated with decreased pain and improved knee flexion, respectively, suggesting that the cytokine-mediated anti-inflammatory effects of BT contributed to clinical improvement in OA patients, especially in pain and joint function (Kapoor et al. 2011; Gálvez et al. 2018b). Changes in the cellular immune response have also been observed. At baseline, OA patients presented diminished neutrophil phagocytic capacity. This capacity increased after BT, reflecting an improvement in the innate defensive capacity against pathogens together with an optimal bioregulatory effect on the inflammatory and innate response (Gálvez et al. 2018b). These results confirmed, for the first time, that systemic anti-inflammatory effects and neuroimmunoendocrine stabilization underline, at least partially, the clinical benefits of BT.
In 2017, Ustyol et al. (2017) studied the potential anti-inflammatory and analgesics effects of Bolu thermal mineral water (Turkey) in 40 patients suffering from OA. The patients were fully immersed in warm thermo-mineral water for 20 min at a temperature of 38 to 40 °C, for a total of 15 immersions in 15 days, and the analysis of serum cyclooxygenase (COX)-2, metalloproteinase (MMP)-3, Hsp70, and sphingosine-1-phosphate (an important mediator of inflammation) was assessed after completion of the BT period. The treatment caused a significant reduction in circulating levels of sphingosine which also resulted positively associated with serum levels of Hsp70, COX-2, and MMP-3, suggesting that BT modulated inflammatory parameters and stress markers through the regulation of sphingosine.
A recent single-blind randomized controlled trial analyzed the anti-inflammatory effects of saline thermal mineral water of Tuzla Spa resort (Istanbul), rich in sodium chloride, magnesium, and calcium, on oxidative status parameters in 29 patients with chronic low back pain (Yücesoy et al. 2021). A total of 10 balneological treatment sessions were planned for the patients over a period of 2 weeks, consisting in tap water full baths up to shoulder level in the hydrotherapy pool (20 min at temperature of 38 °C), followed by mud packs applied on low back region about 15-mm thickness at 42 °C temperature. BT induced a significant increase of IL-10 serum levels and a slight reduction of IL-6 compared to baseline, suggesting a therapeutic role of the treatment in this kind of patients. The authors suggested that balneological treatments may contribute to pain reduction by acting on cytokines. In fact, it has been demonstrated that IL-10 is able to downregulate pro-inflammatory cytokine receptors, and it is considered a key regulator of chronic pain (Uçeyler et al. 2006); thus, the reduction of pro-inflammatory cytokine’s levels after BT can be associated with the analgesic effects of the treatment, as demonstrated by the decrease in perceived pain (Gálvez et al. 2018a; Ortega et al. 2017).
Growing evidence supports the key role of adipokines in the pathophysiology of inflammatory and degenerative rheumatic diseases. Adipokines, such as adiponectin, leptin, resistin, chemerin, omentin, and visfatin, are released primarily by white adipose tissue and have pleiotropic effects modulating immune response and affecting bone and cartilage metabolism (Fantuzzi 2005; Neumann et al. 2016; Fioravanti et al. 2018b, 2019). Considering their role in rheumatic conditions and that BT could regulate their serum levels through the influence of temperature (Zeyl et al. 2004; Imbeault et al. 2009), the modifications of catecholamines (Trayhurn et al. 1998), corticosteroids (Miell et al. 1996), and cytokines (Delaigle et al. 2004), various authors evaluated the possible adipokines modifications after BT.
In a first study, Fioravanti et al. (2011b) measured the serum levels of leptin and adiponectin in patients with knee OA before and after a cycle of mud-bath therapy. At the end of the treatment, serum leptin showed a slight but not significant increase, while a significant decrease in circulating adiponectin was found. In a second prospective randomized, single-blind controlled study in patients with gonarthrosis, the same authors confirmed the decrease of serum adiponectin and showed a similar trend for resistin (Fioravanti et al. 2015b). In view of the recent evidence about the involvement of adiponectin and resistin in the pathogenesis and progression of OA, the decrease of these adipokines partially explains the efficacy of BT in the course of the disease.
However, contrasting data were published by Shimodozono et al. (2012) evaluating the acute effects of a single warm-water bath (30 min) on serum leptin and adiponectin in a small sample of 7 healthy men. The authors showed a significant increase of leptin and a slight, but not significant, increase of adiponectin at the end of the treatment.
Recently, Ionescu et al. (2017) demonstrated the increased serum adiponectin in 23 patients with knee OA after 10 days of cold mud applications and baths combined with physical therapy.
The differences observed by these authors might be related to the subjects studied and the treatment modalities. Furthermore, it remains to be clarified which of the mechanisms of action of BT could modify the changes in serum levels of adipokines. One possible hypothesis is that local application of heat, causing an increase in the internal temperature of the knee, may determine changing in serum adipokine levels, probably due to localized production thereof (Fioravanti et al. 2011b, 2015b; Shimodozono et al. 2012). Nevertheless, currently available data do not allow to identify any specific mechanism of action.
BT and oxidative stress
In the past decades, the involvement of oxidative stress in the pathogenesis of many rheumatic diseases has been widely recognized (Smallwood et al. 2018; Wójcik et al. 2021). The production of endogenous reactive oxygen species (ROS) is physiologically balanced by the antioxidant defense system, and plays a pivotal role in many cellular functions (Wójcik et al. 2021). Conversely, the failure of the antioxidant scavenging system, which occurs in pathological conditions, induces a status of oxidative damage to DNA, proteins, or lipids and promotes alterations in signaling and transcription, contributing to exacerbate inflammation, activate immune cells and apoptosis, and tissue damage (Smallwood et al. 2018; Wójcik et al. 2021).
Recent studies demonstrated the beneficial effects of BT in the regulation of oxidant/antioxidant balance in patients suffering from degenerative and autoimmune rheumatic diseases (Table 2).
The protective antioxidant effect of BT was investigated in a group of patients with symptomatic OA in multiple sites treated with a cycle of mud-bath therapy in combination or not with hydropinotherapy in comparison to a group of control patients (Benedetti et al. 2010). BT, consisting on daily mature thermal mud application followed by a thermal bath in sulfurous water, significantly reduced serum/plasma levels of malondialdehyde while increased total antioxidant capacity, at the end of therapy and 1 month later; this treatment also reduced serum TNF-α and cartilage oligomeric matrix protein (COMP). The authors attributed the positive biochemical effects observed after BT to the high quantity of hydrogen sulfide (H2S), equal to 14.5 mg/L, in their mud-bath composition; it protects cells from oxidative damage thanks to its ability to counteract ROS production, and diminishes, at the joint level, oxidative damage to cartilage components, leading to a reduction of inflammatory and catabolic processes.
In 2017, Karagülle et al. (2017), in a single-blind randomized controlled trial, investigated the influence of 2-week course of saline thermal mineral water of Tuzla Spa (Istanbul), rich in sodium chloride, magnesium, and calcium, on oxidative status parameters in patients with rheumatoid arthritis (RA). They observed a significant increase of non-enzymatic superoxide radical scavenger activity in patients after 12 BT sessions in a thermal mineral water pool in comparison to controls. More recently, the serum levels of paraoxonase, a protein with antioxidant function, were measured and found increased in 45 female patients affected to FS engaged in a cycle of BT (Karadağ and Doğan 2020). Similarly, the serum concentrations of total oxidant status and the measurement of oxidative stress index were detected in 35 females with FS and resulted decreased after receiving 15 sessions of bath treatment for 5 days a week for 3 weeks (Çetinkaya et al. 2020).
These studies suggest that BT has antioxidant activity by decreasing oxidant status and changing the balance in the direction of reduction in oxidative stress.
Furthermore, Gálvez et al. (2020) examined the effects of a cycle of mud-bath therapy on the oxidative burst of circulating monocytes isolated from elderly patients with knee OA, observing that the production of superoxide anion resulted significantly reduced in patients after 10 consecutive days of a daily session of mud-bath therapy. Finally, an increase of total antioxidant status was found by Kuciel-Lewandowska (2020) in patients with OA receiving different spa treatment modalities such as sulfide-radon baths including whole body or only upper and/or lower extremities (temperature of 37–38 °C for 20 min), partial peloid compresses (20 min at 40–42 °C), or cryotherapy (ventilation for 2–3 min at − 80 °C and − 110 °C). However, the paper contains a lot of bias due to the complexity of the spa therapy which make difficult any conclusion.
In the last decade, a group of investigators, through pre-clinical studies, assessed the potential antioxidant effects of a thermal mineral water tested as whole or a specific component which constitute a mineral water, such as H2S (Cheleschi et al. 2020). Among the inorganic molecules which constitute mineral waters, sulfur, especially in the form of H2S, has currently been recognized as a crucial element with a wide range of functions, and its exogenous and endogenous donors were generally employed in in vitro research to reproduce physiological functions of H2S at cellular level (Carbajo and Maraver 2017; Viegas et al. 2019) (Table 3).
In 2020, the effects of the thermal sulfurous water from Spa of Carballo (Spain) were evaluated in an experimental model of Wistar OA rats subjected to meniscectomy (Vaamonde-Garcia et al. 2020). The animals were treated with BT using rich-sulfurous water or were bathed in tap water or not treated (controls). At day 40 after rats sacrifice, the immunohystochemical analysis on cartilage tissue showed a reduced number of cells positive to markers of DNA damage and lipid peroxidation, related to ROS overproduction, as well as a reduction of MMP-13, in BT group compared to controls. The authors suggested a protective effect of BT on cartilage since sulfur-rich water may attenuate oxidative stress-activated signaling upregulating MMP-13 expression, in turn protecting cartilage against degradation.
Several in vitro studies have been conducted aimed at investigating the antioxidant function of a thermal mineral water or exogenous sources of H2S on cartilage or bone-derived cells.
A study by Fioravanti et al. (2013) tested the potential beneficial effects of Vetriolo thermal water (Trentino Alto Adige, Italy), a highly mineralized water, strongly acidic sulfate, rich in calcium, magnesium, and iron, evaluating different concentrations of the thermal water (100%, 50%, 25%), directly dissolved in the culture medium of human OA chondrocytes in presence of IL-1β (5 ng/mL). A significant reduction of nitric oxide (NO) levels and inducible nitric oxide synthase (iNOS) expression was observed in chondrocytes treated with 50% and 25% concentrations of Vetriolo thermal water.
A recent paper analyzed the potential anti-inflammatory effects of a group of 14 Portuguese thermal waters, different for mineralization, belonging to the Central Region of Portugal, in mouse monocyte macrophage cell lines exposed to lipopolysaccharide (LPS) (Silva et al. 2020). The results of the study demonstrated the ability of 11 of the studied waters to reduce NO production activated by LPS, downregulate iNOS expression, and ROS scavenge activity, confirming the anti-inflammatory properties of these waters, supporting their therapeutic use for inflammation-related diseases, including rheumatic diseases.
In 2012, Fox et al. (2012) studied the response of human primary chondrocytes to the incubation with exogenous slow-releasing H2S source, GYY4137. The treatment of the cells with different concentrations of GYY4137 (50–500 mol/L for 18 h) significantly reduced cell death and oxidant-induced mitochondrial dysfunction, via Akt/PI3K-dependent signaling. The effect of GYY4137 (0.1–0.5 mM) was also assessed in a study of human arthritis synoviocytes and articular chondrocytes stimulated with LPS (Li et al. 2013), demonstrating a decrease in COX-2, PGE2, TNF-α, IL-6, and nitrite (NO2−) production, the catalytic activity of iNOS, and nuclear factor (NF)-κB activation, after GYY4137 treatment.
The potential antioxidant and anti-catabolic role of NaHS and GYY4137 (0.05–1 mM, for 24 or 48 h) was also examined in human OA chondrocytes stimulated with IL-1β (5 ng/mL) (Burguera et al. 2014); the results of the study demonstrated the ability of both compounds to significantly decreased nitric oxide NO, PGE2, and IL-6, NOS2, COX-2, PGE synthase, and NF-κB nuclear translocation activated by IL-1β. These data were confirmed 1 year later by Ha et al. (2015) in a study on human OA chondrocytes treated with NaHS (0.06–1.5 mM), in presence of IL-1β (10 ng/mL) for 24 h.
Lately, the production of mitochondrial ROS, the related apoptosis rate, and superoxide dismutase (SOD) activity were measured in a study on primary rat chondrocytes incubated with GYY4137 (100 μM, 24 h) (Wu et al. 2021); GYY4137 significantly decreased ROS generation and apoptosis, while increased SOD activity, confirming the antioxidant function of H2S sources.
A study on murine osteoblast-like cell lines stimulated with hydrogen peroxide (H2O2) (400 μM) showed the antioxidant effect of NaHS (100 μM, 4 h), by increasing SOD activity and reducing ROS production, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase activity, and NO release, probably via p38 and extracellular ERK/MAPK (Xu et al. 2011). Some years later, analogous experimental studies have been performed in MC3T3-E1 osteoblast-like cell lines incubated for 4 h with GYY4137 (100 μM) or with a new synthetic H2S-releasing SDSS (25 μM, 60 min) in presence of H2O2 (400 μM) (Lv et al. 2017; Yan et al. 2017), demonstrating the ability of the studied compounds to reduce SOD activity, ROS, and NO production induced by H2O2.
Finally, a study carried out on human differentiated osteoclasts incubated with NaHS (50–300 μM), for a period ranging from 72 h to 6 days, showed a dose-dependent reduction of intracellular ROS levels and an increase of nuclear factor erythroid 2-related factor 2 (NRF2) activity and antioxidant genes peroxiredoxin-1 and NADPH dehydrogenase (Gambari et al. 2014).
The number of evidence about the beneficial effects of BT on oxidative stress is growing; however, the mechanism by which BT could modulate redox balance is not fully understood. A possible explanation may be related to the high temperature of balneotherapeutic local applications which induces vasodilatation thus increasing blood flow, contributing to remove metabolic products, including excessive free radical species, and ameliorate tissue oxygenation supporting fast cell repair (Jokić et al. 2010). Therefore, it is known that BT high temperature is responsible to the increase of Hsp production, which partially increased SOD and catalase activities, promoting its antioxidant effects (Jokić et al. 2010). Finally, water and mud compositions can represent important factors for the favorable effect of BT on redox balance. Indeed, it has been established that sulfur interacts with antioxidant protection enzymes potentiating their activity and capacity, through the regulation of different signaling pathways (Viegas et al. 2019).
BT and cartilage and bone metabolism
The progressive damage of articular cartilage has been thought to be one of the primary changes associated to arthritic disease, together with moderate inflammatory changes in tissues joints, and formation of osteophytes and bone cysts (Man et al. 2014). The loss of articular cartilage mainly occurs as a consequence of an aberrant chondrocyte metabolism in response to changes in the microenvironment. The established imbalance between chondrocyte catabolic and anabolic activities, in favor of catabolism, induces cell death and progressive depletion of extracellular matrix components, mainly proteoglycans and type II collagen (Zheng et al. 2021).
Accumulating evidence suggests a beneficial impact of mineral waters and components in the regulation of cartilage matrix and tissue remodeling during pathological processes of degenerative and inflammatory rheumatic diseases.
In 2012, Güngen et al. (2012), in a prospective randomized controlled study, evaluated the efficacy of 12 sessions of mud packs on serum levels of YKL-40 and high-sensitivity C-reactive protein (hsCRP), two biological markers for OA articular damage and inflammation, in patients with knee OA. After 3 months of treatment, decreased serum levels of YKL-40 were observed, while no modifications in circulating hsCRP were found. Considering that high levels of YKL-40 seem to be related to cartilage degradation, fibrillation, and osteophyte formation, the maintenance of YKL-40 low levels in mud therapy appears to slow down the progression of knee OA (Table 4). Some years later, the same authors showed no changes in urine levels of C telopeptide fragment of collagen type-II (uCTX-II), a breakdown product of type II collagen and a marker of cartilage destruction, in patients with knee OA treated with an analogous mud pack schedule (Güngen et al. 2016).
Serum levels of CTX-II, hsCRP, COMP, and myeloperoxidase (MPO) were also assessed in a study comprising 103 patients with primary symptomatic bilateral knee OA, randomly assigned to receive a cycle of mud-bath therapy at Chianciano Spa Resort (Siena, Italy) or to continue their standard therapy (Pascarelli et al. 2016). After treatment, a significant increase of CTX-II levels was reported, whereas no changes for COMP, MPO, and hsCRP were observed. The authors affirmed that the significant increase of CTX-II, found to be predictive of joint degeneration in OA, could be due to an increase of cartilage turnover induced by thermal stress. One year later, the same group of investigators evaluated the expression profile of microRNA (miR)-155, 223, 181a, 146a, and let-7e, from whole blood of patients with knee OA, demonstrating a significant reduction of their gene levels after the same BT schedules (Giannitti et al. 2017). The studied miRNA are known to be involved in OA pathogenesis, mainly acting as mediators of cartilage degradation, oxidative stress, and inflammation occurring during the disease (De Palma et al. 2017). The changes in miRNA expression levels observed after BT may be linked to the well-known immunosuppressive effect of this treatment, as well as to the temperature which could regulate miRNA synthesis, since this process is influenced by the thermodynamic stability of the miRNA precursors.
In a recent experience, Cucu et al. (2017) evaluated the serum levels of markers related to bone and cartilage metabolism, as CTX-I, COMP, receptor activator of NFκB ligand, osteoprotegerin, and visfatin, in patients suffering from chronic degenerative musculoskeletal disorders, demonstrating a reduction of serum CTX-I and visfatin after low-dose radon therapy. The authors hypothesized a reduction of bone degradation induced by radon therapy presumably related to an attenuation of inflammation mediated by visfatin.
Lately, a cohort of 66 patients with chronic back pain, secondary to axial OA, were enrolled and randomly treated with daily mud packs and bicarbonate-alkaline mineral water baths, or with a thermal hydrotherapy rehabilitation scheme for 2 weeks (Angioni et al. 2019). An increase of serum fibroblast growth factors, oxidized low-density lipoprotein receptor 1, and MMP-13 were observed after BT in comparison to control group, demonstrating that chemical properties of mineral waters, together with mechanical and thermal effects, may explain, at least in part, the changes in proteins involved in differentiation, angiogenesis, and tissue repair.
The anti-inflammatory and analgesic effects of Hévíz thermal water and mud (Hungary) were tested in OA and RA-induced murine models (Tékus et al. 2018) (Table 5). Hévíz medicinal water and mud significantly decreased the mechanical hyperalgesia and knee edema in induced-OA model, while seemed ineffective in relieving the main symptoms of RA mice. The authors supposed that H2S, present in Hévíz water and mud, can lead to the release of the hormone somatostatin from the nerve fibers and affect neurotransmission exerting anti-nociceptive and anti-inflammatory effects, acting on its receptor, in the late phase of arthritis.
In 2020, Kim et al (2020) demonstrated the beneficial effects of Jeju magma-seawater, with high contents of Na, Mg, Ca, K, zinc, and manganese, in rats with partial meniscectomy-induced OA. Following 8 weeks of bathing in thermal Jeju magma-seawater, an increased joint thickness and bone mineral density, as well as an improvement of mobility, were observed. The protective effects of this water can be related to the activity of its component involved in reducing serum inflammatory cytokines, enhancing the proliferating and anti-apoptotic activities, thus contributing to preserve cartilage tissue.
Fibroblast-like synoviocyte cultures, derived from RA and OA patients, and chondrocyte cell line C-28/I2 were employed to study the molecular mechanism of action of H2S, by using its exogenous source, NaHS (Kloesch et al. 2012a, b). The treatment of the cells with different concentrations of NaHS (0.030–1 mM, for a maximum of 12 h) transiently reduced the expression of IL-6, IL-8, and COX-2, and the activation of MAPK/ERK and NF-κB signaling, induced by IL-1β (5 ng/mL, 1 h); conversely, high concentrations of NaHS (above 0.5 mM) demonstrated opposite effects on the analyzed parameters. The effect of different concentrations of NaHS (0.06–1 mmol/L) was also assessed in OA fibroblast-like synoviocytes stimulated with 10 ng/mL of IL-1β (Sieghart et al. 2015); the results of the study showed that 1 h of NaHS treatment reduced IL-1β-induced secretion of IL-6, IL-8, and RANTES, the expression of MMP-2 and MMP-14, and the phosphorylation of several MAPK proteins, suggesting the ability of H2S to partially antagonize IL-1β stimulation via MAPK and the PI3K/Akt pathways.
NaHS and GYY4137 were tested at concentrations of 200 or 1000 μM, for 21 days, in OA cartilage extracts co-cultured with IL-1β (5 ng/mL) (Vela-Anero et al. 2017). The histological and immunohistochemical analysis of the samples demonstrated a decrease of glycosaminoglycan destruction and MMP-3 and MMP-13 production induced by IL-1β, and an increased synthesis of collagen type II and aggrecans, after long-term treatment of chondrocytes with NaHS or GYY4137.
Later, the protective effects of different concentrations of NaHS (0.01–1 mM) were observed by Wang et al. (2021) in a study on human OA chondrocytes stimulated with IL-1β (10 ng/mL), showing the ability of H2S donor to attenuate IL‐1β‐induced overproduction of IL-6, IL-8, and TNF-α, and to improve the balance between anabolic and catabolic chondrocyte capacities. Furthermore, NaHS significantly reversed mitochondrial dysfunction‐related apoptosis and phosphorylation of MAPK cascades, suggesting that H2S may antagonize IL‐1β‐induced inflammation and mitochondrial dysfunction‐related apoptosis via suppression of the PI3K/Akt/NF‐κB and MAPK signaling pathways.
Finally, Liu et al. (2017) analyzed the potential benefit of NaHS treatment (400 μmol/L, for 30 min) on primary rat osteoablasts, followed by 12-h incubation in DMEM, with high glucose concentration (HG); the authors revealed that NaHS significantly prevented osteoblast injury induced by HG, decreasing the rate of cell proliferation, increasing the number of apoptotic cells, and blocking the HG-induced osteoblast mineralization inhibition, via activating ATP-sensitive potassium channels.
Balneotherapy and immune system: a model of immunoneuroendocrine interaction
Regarding the effects of BT and mud-bath therapy on the immune system, the physiological mechanisms underlying the beneficial anti-inflammatory, chondroprotective, and immunomodulatory effects in rheumatic pathologies are not clearly known yet. However, among these physiological mechanisms, currently immunoneuroendocrine interactions should be included, particularly taking into account well-being aspects linked to the BT interventions, i.e., the environmental enrichment that can improve psychological parameters of the patients (Gàlvez et al. 2018a; Scanu et al. 2021).
It has already been mentioned in previous sections of this review that the anti-inflammatory action may arise from the reduction of pro-inflammatory and chondrolytic activity by inhibition of pro-inflammatory cytokines and adipokines, inhibition of prostaglandins and leukotrienes, and an improvement in the oxidative balance and anabolic metabolism of chondrocytes. This immune response occurs in part due to various neuroendocrine and neurovegetative stimuli, which are caused, at least partially according to the current state of evidence, by heat stress. In general, based on the decrease in inflammatory mediators and reduced adaptive response, heat stress appears to have an immunosuppressive effect. With moderate increases in local skin temperature, a stimulatory effect of the immune response seems to prevail, whereas higher temperatures (40–41 °C), such as those used in BT, apparently have a suppressive effect on immunity (Fioravanti et al. 2011a; Tenti et al. 2015). The immunosuppressive action of heat in both BT and muds is reflected by a significant reduction in T lymphocyte concentrations in the peripheral blood. This reduction could result in lower production of pro-inflammatory cytokines by this cell type (Sukenik et al 1999; Mooventhan et al. 2014).
However, it is known that the influence of stress on the adaptive immune response differs from that in the innate response, and hyperthermia also plays an important role in the function of the innate immune system. Importantly, when analyzing the innate response, it is necessary to consider both the inflammatory humoral response and the innate cellular response (Ortega 2016). Hyperthermia seems to increase the motility, phagocytic and bactericidal properties, and enzymatic activity of circulating granulocytes, as suggested in recent reviews (Fioravanti et al. 2011a; Tenti et al. 2015), although a decrease in the number of neutrophils has also been described (Basili et al. 2001).
Regarding the phagocytic process of circulating monocytes, it has been observed that the chemotactic capacity of these cells increases after BT. As for the phagocytic capacity (percentage of monocytes with phagocytic capacity, and their phagocytic activity), it was not modified, while the production of superoxide anion decreased after treatment. This could potentially reflect a shift towards an anti-inflammatory profile of monocytes (patrolling monocytes) with a greater capacity for infiltration and repair of tissue damage (Gálvez et al. 2020). Moreover, the percentage of CD4 + CD25 + FOXP3 + regulatory T lymphocytes decreased and that of CD8 + CD28 − regulatory T lymphocytes increased after the BT intervention, possibly being also involved in the anti-inflammatory effects of this strategy (Gálvez et al. 2018b). The induction of increased CD8 + regulatory T lymphocytes in rheumatic pathologies has been shown to have beneficial anti-inflammatory effects, as these cells contribute to decrease excessive inflammatory activity (Konya et al. 2009), while the decrease in CD4 + found after mud-bath therapy could be a reflection of the reduced need to counteract the excessive immune response, as it has been observed in other OA treatments (Guo et al. 2015). The novelty of these results lies particularly in the focus on the influence of BT on the systemic cellular immune response.
Since the inflammatory response is part of the innate immune response to pathogens, it could be speculated that a reduction in the inflammatory response could further compromise the cellular immune response in patients with rheumatic pathologies. However, when analyzing all aspects of the innate/inflammatory response together, results have shown that BT interventions can stimulate granulocyte innate activity against pathogens, helping to improve the impaired defensive capacity of granulocytes in OA patients. This anti-inflammatory effect accompanied by an optimal immune response against pathogens is defined (in the context of other non-pharmacological anti-inflammatory strategies such as physical exercise) as the “bioregulatory effect” of the inflammatory/innate immune response (Ortega 2016), and has been proposed in the field of BT as the “bioregulatory effect of balneotherapy” (Gálvez et al. 2018b).
In any case, it is plausible to think that the mechanism of effectiveness of these therapies probably results from a complex synergistic combination of several factors (Morer et al. 2017). Whatever the mechanism involved, to a greater or lesser extent, the physiological responses derived from balneotherapy consist mainly of neuroendocrine and immune effects, which are particularly important in rheumatic pathologies (Gálvez et al. 2018a). These findings corroborate the clinical efficacy of balneotherapy and represent yet another relevant step forward in the field of Medical Hydrology by providing with objective immunophysiological mechanisms of effectiveness to the scientific evidence of the clinical benefits of these therapies.
Discussion
The objective of this narrative review was to summarize the latest available information about the beneficial effects of BT on different mediators and factors of inflammation, oxidative stress, cartilage and bone metabolism, and humoral and cellular immune response (including immunoneuroendocrine interactions), and to identify its possible mechanism of action in different rheumatic diseases.
In the last decade, the growing body of evidence derived both from clinical and pre-clinical studies corroborated the anti-inflammatory, antioxidant, chondroprotective, and immunomodulatory role of different mineral waters or mud applications (Gálvez et al. 2018a; Cheleschi et al. 2020; Maccarone et al. 2021b).
The results of clinical studies, using various BT modalities, confirmed the beneficial properties and the positive effects of BT in limiting the production of the main pro-inflammatory cytokines, prostaglandins, heat shock proteins, and adipokines in patients with OA (Fioravanti et al. 2011a; Shimodozono et al. 2012; Gálvez et al. 2017; Ionescu et al. 2017; Ortega et al. 2017). The ability of BT in regulating oxidant/antioxidant balance and reducing oxidative status parameters was observed in patients suffering from RA, fibromyalgia, and OA (Karagülle et al. 2017; Karadağ and Doğan 2020; Kruciel-Lewandowska et al. 2020). Furthermore, the main markers of bone and cartilage damage and metabolism, and a pattern of miRNA were positively modulated by BT in patients with OA and affected by chronic degenerative musculoskeletal disorders (Güngen et al. 2012, 2016; Pascarelli et al. 2016; Cucu et al. 2017; Giannitti et al. 2017; Angioni et al. 2019).
The data derived from OA and RA-induced murine models revealed the efficacy of different balneological treatments in decreasing pain, inflammation, and improving mobility, as well as in reducing the expression of matrix-degrading enzymes and markers of oxidative stress damage (Tékus et al. 2018; Vaamonde-García et al. 2020; Kim et al. 2020).
Different in vitro studies analyzed the potential effect of mineral elements of mineral waters, especially H2S, demonstrating their anti-inflammatory, antioxidant, and chondroprotective properties in arthritic fibroblast-like synoviocytes and chondrocytes, and in OA chondrocytes and cartilage (Fox et al. 2012; Kloesch et al. 2012a, b; Li et al. 2013; Burguera et al. 2014; Ha et al. 2015; Wu et al. 2021; Sieghart et al. 2015; Vela-Anero et al. 2017; Maccarone et al. 2021b). The ability of H2S donors to reduce oxidative stress damage was confirmed in human and rat primary or transformed cell lines of osteoblasts and osteoclasts (Xu et al. 2011; Gambari et al. 2014; Lv et al. 2017; Yan et al. 2017).
Finally, only two studies on cell cultures attested the beneficial effect of different thermal mineral waters, tested as a whole, in reducing oxidative stress and degrading processes of articular cartilage (Fioravanti et al. 2013; Silva et al. 2020).
Taken together, the presented data are promising and stimulating and confirm BT as an effective complementary approach in the management of several low-grade inflammation, degenerative, and stress-related pathologies, in particular rheumatic diseases. However, although the documented clinical and pre-clinical benefits of BT, the exact role of this therapy in modern medicine and its consensus for scientific community remains still controversial. Indeed, some aspects of these studies are questionable and could represent a source of bias. The presented clinical data only refer to the short-term effects of balneotherapic treatments on modifications of the studied mediators and factors, until the end of the treatment cycle, while no information about the possible long-term effects are available. Comparisons between studies are difficult since the variety and heterogeneity of different compositions of mineral waters and peloids used and treatment schedule; this makes difficult to determine the exact intervention for obtaining optimal biological and clinical outcomes for each pathology. It also remains to be clarified which waters are the most suitable for each pathological condition, which elements are fundamental, and what is their appropriate concentrations for the best response to treatment. Furthermore, there is no enough evidence concerning the absorption of mineral elements composing mineral waters into the systemic circulation through the skin (Fioravanti et al. 2011a).
In vitro testing allows to partially overcome this aspect since they represent an essential approach to understand the specific effect of a mineral water or a particular element, in terms of mechanisms of action, toxicity, and biological response, as well as to identify the best concentrations necessary for obtaining optimal biological benefits. However, the validity of in vitro studies is conditioned by several factors, including the isolation procedures of the cells from different donors, the identification of the most suitable cell model for such pathological condition, and the standardization of the experimental procedures (Cheleschi et al. 2020). Additionally, the maintenance of the optimal culture conditions, such as the physiological temperature preserved at 37 °C, and the sterilizations of mineral waters or single components, to avoid interference with cell viability and metabolism, could alter water composition and maybe remove chemical or organic components, including the natural spring water microbiome, recently considered to be responsible for some positive effects of BT in different diseases (Carretero 2020b; Pedron et al. 2019; Varga 2019). Indeed, the organic compounds, organic matter content, and microbial communities present in thermal mineral waters or mud are specifics for each one and, in some cases, very heterogeneous one to each other. A number of studies have been performed aimed at investigating mud and spring water microbiome biodiversity, identifying different native non-pathogenic microflora communities with specific characteristics (Tett et al. 2017; Pedron et al. 2019; Doulgeraki et al. 2020; Gris et al. 2020). Recent evidence has shown anti-inflammatory, immunomodulatory, and regenerative properties of some spring waters and muds associated with active metabolites produced by the spring microbiome (Pedron et al. 2019; Varga 2019; De Natale et al. 2020; Fernández-González et al. 2021). One of the first report analyzed the microbial composition of the spring water of La Roche-Posay (France), a selenium-rich water known for its anti-inflammatory properties, and principally used for the treatment of chronic inflammatory diseases as atopic dermatitis and psoriasis; the lysate of Vitreoscilla filiformis, a bacterium within the Neisseriaceae family, was isolated from this spring water and has been recognized to induced enhancement of skin defense mechanisms through activation of cutaneous regulatory T cells (Martin et al. 2015). Besides, lysates of Proteobacteria and Actinobacteria were found in Comano spring water (Trento, Italy), a hypotonic, bicarbonate calcium–magnesium mineral water specifically employed for treating various inflammatory-based cutaneous disorders, and cultured with human skin fibroblasts; the study demonstrated a regenerative effects of Comano spring water microbiome by inducing cell proliferation (Nicoletti et al. 2019). A recent study of Eliasse et al. (2020) showed the anti-inflammatory effects of Avéne spring water (France), a water rich in bicarbonate, calcium, and magnesium, extensively used to treat atopic dermatitis and psoriasis; this property was mainly attributed to a biological extract from Aquaphilus dolomiae, a bacterium belonging to Neisseriaceae family, revealing the ability to regulate the innate cutaneous immune response by activation of Toll-like receptors and modulation of mast cell and dendritic cells function (Aries et al. 2014; Eliasse et al. 2020).
Despite the growing body of evidence, the microbiome biodiversity of thermal waters and muds is, however, complex and not fully characterized so far.
In conclusion, the latest and available evidence confirm the role of BT as complementary therapy for the treatment of different rheumatic diseases. However, more researches should be conducted to further evaluate the long-term efficacy of BT, as well as to implement the methodological quality of clinical trials standardizing treatment modalities, intervention periods and frequencies, water temperature, and composition. Nowadays, a general improvement of pre-clinical studies is imperative, both to limit the high heterogeneity existing among the available scientific sources and to allow a standardization of the experimental procedures. Furthermore, the analysis of the effects of the only inorganic composition of thermal waters is not enough, but it is necessary to perform a complex chemical analysis which should also consider their organic fraction and microbial communities that may play a role in the therapeutic efficacy or in other biological mechanisms. All these adjustments could contribute to increase the knowledge about the biological mechanisms underlying the beneficial effects of BT.
Data availability
Not applicable
References
Angioni MM, Denotti A, Pinna S, Sanna C, Montisci F, Dessole G, Loi A, Cauli A (2019) Spa therapy induces clinical improvement and protein changes in patients with chronic back pain. Reumatismo 71:119–131. https://doi.org/10.4081/reumatismo.2019.1200
Antonelli M, Donelli D, Fioravanti A (2018) Effects of balneotherapy and spa therapy on quality of life of patients with knee osteoarthritis: a systematic review and meta-analysis. Rheumatol Int 38:1807–1824. https://doi.org/10.1007/s00296-018-4081-6
Ardiç F, Ozgen M, Aybek H, Rota S, Cubukçu D, Gökgöz A (2007) Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446. https://doi.org/10.1007/s00296-006-0237-x
Aries MF, Fabre P, Duplan H, et al (2014) I-modulia, an Aquaphilus dolomiae extract, stimulates innate immune response through Toll-like receptor activation. J Am Acad Dermatol 70: AB63.
Basili S, Martini F, Ferroni P, Grassi M, Sili Scavalli A, Streva P, Cusumano G, Musca A, Battista Rini G (2001) Effects of mud-pack treatment on plasma cytokine and soluble adhesion molecule levels in healthy volunteers. Clin Chim Acta 314:209–214. https://doi.org/10.1016/s0009-8981(01)00697-0
Bellometti S, Cecchettin M, Galzigna L (1997) Mud pack therapy in osteoarthrosis. Changes in serum levels of chondrocyte markers. Clin Chim Acta 268:101–106. https://doi.org/10.1016/s0009-8981(97)00171-x
Bellometti S, Galzigna L, Richelmi P, Gregotti C, Bertè F (2002) Both serum receptors of tumor necrosis factor are influenced by mud pack treatment in osteoarthrotic patients. Int J Tissue React 24:57–64
Benedetti S, Canino C, Tonti G, Medda V, Calcaterra P, Nappi G, Salaffi F, Canestrari F (2010) Biomarkers of oxidation, inflammation and cartilage degradation in osteoarthritis patients undergoing sulfur-based spa therapies. Clin Biochem 43:973–978. https://doi.org/10.1016/j.clinbiochem.2010.05.004
Burguera EF, Vela-Anero A, Magalhães J, Meijide-Faílde R, Blanco FJ (2014) Effect of hydrogen sulfide sources on inflammation and catabolic markers on interleukin 1β-stimulated human articular chondrocytes. Osteoarthritis Cartilage 22:1026–1035. https://doi.org/10.1016/j.joca.2014.04.031
Carbajo JM, Maraver F (2017) Sulphurous mineral waters: new applications for health. Evid Based Complement Alternat Med 2017:8034084. https://doi.org/10.1155/2017/8034084
Carretero MI (2020a) Clays in pelotherapy. A review. Part I: Mineralogy, chemistry, physical and physicochemical properties. Applied Clay Science 189:105526
Carretero MI (2020b) Clays in pelotherapy. A review. Part II: Organic compounds, microbiology and medical applications. Applied Clay Science 189:105526
Çetinkaya FN, Koçak FA, Kurt EE, Güçlü K, Tuncay F, Şaş S, Erdem HR (2020) The effects of balneotherapy on oxidant/antioxidant status in patients with fibromyalgia: an observational study. Arch Rheumatol 35:506–514. https://doi.org/10.46497/ArchRheumatol.2020.7857
Ciani O, Pascarelli NA, Giannitti C, Galeazzi M, Meregaglia M, Fattore G, Fioravanti A (2017) Mud-bath therapy in addition to usual care in bilateral knee osteoarthritis: an economic evaluation alongside a randomized controlled trial. Arthritis Care Res (hoboken) 69:966–972. https://doi.org/10.1002/acr.23116
Cheleschi S, Gallo I, Tenti S (2020) A comprehensive analysis to understand the mechanism of action of balneotherapy: why, how, and where they can be used? Evidence from in vitro studies performed on human and animal samples. Int J Biometeorol 64:1247–1261. https://doi.org/10.1007/s00484-020-01890-4
Cucu A, Shreder K, Kraft D, Rühle PF, Klein G, Thiel G, Frey B, Gaipl US, Fournier C (2017) Decrease of markers related to bone erosion in serum of patients with musculoskeletal disorders after serial low-dose radon spa therapy. Front Immunol 8:882. https://doi.org/10.3389/fimmu.2017.00882
De Natale A, Mele BH, Cennamo P, Del Mondo A, Petraretti M, Pollio A (2020) Microbial biofilm community structure and composition on the lithic substrates of Herculaneum Suburban Baths. PLoS ONE 15:e0232512. https://doi.org/10.1371/journal.pone.0232512
De Palma A, Cheleschi S, Pascarelli NA, Tenti S, Galeazzi M, Fioravanti A (2017) Do MicroRNAs have a key epigenetic role in osteoarthritis and in mechanotransduction? Clin Exp Rheumatol 35:518–526
Delaigle AM, Jonas JC, Bauche IB, Cornu O, Brichard SM (2004) Induction of adiponectin in skeletal muscle by inflammatory cytokines: in vivo and in vitro studies. Endocrinology 145:5589–5597. https://doi.org/10.1210/en.2004-0503
Doulgeraki AI, Bikouli V, Argyri AA, Chorianopoulos N, Mitre E, Charvourou G, Sourri P, Tassou CC, Oikonomou A (2020) Exploring the bacterial communities of the Kaiafas Thermal Spring Anigrides Nymphes in Greece prior to rehabilitation actions. Int J Environ Res Public Health 17:9133. https://doi.org/10.3390/ijerph17239133
Eliasse Y, Redoules D, Espinosa E (2020) Impact of Avène Thermal Spring Water on immune cells. J Eur Acad Dermatol Venereol 34:21–26. https://doi.org/10.1111/jdv.16335
Fantuzzi G (2005) Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol 115:911–919. https://doi.org/10.1016/j.jaci.2005.02.023
Fernández-González MV, Carretero MI, Martín-García JM, Molinero-García, A, Delgado R (2021) Peloids prepared with three mineral-medicinal waters from spas in Granada. Their suitability for use in pelotherapy. Applied Clay Science 202:105969
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011a) a) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int 31:1–8. https://doi.org/10.1007/s00296-010-1628-6
Fioravanti A, Cantarini L, Bacarelli MR, de Lalla A, Ceccatelli L, Blardi P (2011b) b) Effects of spa therapy on serum leptin and adiponectin levels in patients with knee osteoarthritis. Rheumatol Int 31:879–882. https://doi.org/10.1007/s00296-010-1401-x
Fioravanti A, Lamboglia A, Pascarelli NA, Cheleschi S, Manica P, Galeazzi M, Collodel G (2013) Thermal water of Vetriolo, Trentino, inhibits the negative effect of interleukin-1β on nitric oxide production and apoptosis in human osteoarthritic chondrocyte. J Biol Regul Homeost Agents 27:891–902
Fioravanti A, Bacaro G, Giannitti C, Tenti S, Cheleschi S, Gui Delli GM, Pascarelli NA, Galeazzi M (2015a) a) One-year follow-up of mud-bath therapy in patients with bilateral knee osteoarthritis: a randomized, single-blind controlled trial. Int J Biometeorol 59:1333–1343. https://doi.org/10.1007/s00484-014-0943-0.Erratum.In:IntJBiometeorol59:1345
Fioravanti A, Giannitti C, Cheleschi S, Simpatico A, Pascarelli NA, Galeazzi M (2015b) b) Circulating levels of adiponectin, resistin, and visfatin after mud-bath therapy in patients with bilateral knee osteoarthritis. Int J Biometeorol 59:1691–1700. https://doi.org/10.1007/s00484-015-0977-y
Fioravanti A, Karagülle M, Bender T, Karagülle MZ (2017) Balneotherapy in osteoarthritis: facts, fiction and gaps in knowledge. European Journal of Integrative Medicine 9:148–150
Fioravanti A, Manica P, Bortolotti R, Cevenini G, Tenti S, Paolazzi G (2018a) a) Is balneotherapy effective for fibromyalgia? Results from a 6-month double-blind randomized clinical trial. Clin Rheumatol 37:2203–2212. https://doi.org/10.1007/s10067-018-4117-z
Fioravanti A, Cheleschi S, De Palma A, Addimanda O, Mancarella L, Pignotti E, Pulsatelli L, Galeazzi M, Meliconi R (2018b) b) Can adipokines serum levels be used as biomarkers of hand osteoarthritis? Biomarkers 23:265–270. https://doi.org/10.1080/1354750X.2017.1401665
Fioravanti A, Tenti S, Bacarelli MR, Damiani A, Li Gobbi F, Bandinelli F, Cheleschi S, Galeazzi M, Benucci M (2019) Tocilizumab modulates serum levels of adiponectin and chemerin in patients with rheumatoid arthritis: potential cardiovascular protective role of IL-6 inhibition. Clin Exp Rheumatol 37:293–300
Forestier R, Erol-Forestier FB, Francon A (2017) Current role for spa therapy in rheumatology. Joint Bone Spine 84:9–13. https://doi.org/10.1016/j.jbspin.2016.05.003
Forestier R, Fioravanti A, Bender T, Santos I, Erol Forestier FB, Muela Garcia A, Françon A (2021) Crenobalneotherapy for low back pain: systematic review of clinical trials. Int J Biometeorol. https://doi.org/10.1007/s00484-021-02188-9.
Fox B, Schantz JT, Haigh R, Wood ME, Moore PK, Viner N, Spencer JP, Winyard PG, Whiteman M (2012) Inducible hydrogen sulfide synthesis in chondrocytes and mesenchymal progenitor cells: is H2S a novel cytoprotective mediator in the inflamed joint? J Cell Mol Med 16:896–910. https://doi.org/10.1111/j.1582-4934.2011.01357.x
Gálvez I, Torres-Piles S, Hinchado MD, Alvarez-Barrientos A, Torralbo-Jimenez P, Guerrero J, Martin-Cordero L, Ortega E (2017) Immune-neuroendocrine dysregulation in patients with osteoarthritis: a revision and a pilot study. Endocr Metab Immune Disord Drug Targets 17:78–85. https://doi.org/10.2174/1871530317666170320113613
Gálvez I, Torres-Piles S, Ortega-Rincón E (2018a) Balneotherapy, immune system, and stress response: a hormetic strategy? Int J Mol Sci 19:1687. https//:doi.org/https://doi.org/10.3390/ijms19061687
Gálvez I, Torres-Piles S, Ortega E (2018b) b) Innate/inflammatory bioregulation and clinical effectiveness of whole-body hyperthermia (balneotherapy) in elderly patients with osteoarthritis. Int J Hyperthermia 35:340–347. https://doi.org/10.1080/02656736.2018.1502896
Gálvez I, Torres-Piles S, Ortega E (2020) Effect of mud-bath therapy on the innate/inflammatory responses in elderly patients with osteoarthritis: a discussion of recent results and a pilot study on the role of the innate function of monocytes. Int J Biometeorol 64:927–935. https://doi.org/10.1007/s00484-019-01748-4
Gambari L, Lisignoli G, Cattini L, Manferdini C, Facchini A, Grassi F (2014) Sodium hydrosulfide inhibits the differentiation of osteoclast progenitor cells via NRF2-dependent mechanism. Pharmacol Res 87:99–112. https://doi.org/10.1016/j.phrs.2014.06.014
Giannitti C, De Palma A, Pascarelli NA, Cheleschi S, Giordano N, Galeazzi M, Fioravanti A (2017) Can balneotherapy modify microRNA expression levels in osteoarthritis? A comparative study in patients with knee osteoarthritis. Int J Biometeorol 61:2153–2158. https://doi.org/10.1007/s00484-017-1420-3
Gris B, Treu L, Zampieri RM, Caldara F, Romualdi C, Campanaro S, La Rocca N (2020) Microbiota of the therapeutic Euganean thermal muds with a focus on the main Cyanobacteria species. Microorganisms 8:1590. https://doi.org/10.3390/microorganisms8101590
Güngen G, Ardic F, Fındıkoğlu G, Rota S (2012) The effect of mud pack therapy on serum YKL-40 and hsCRP levels in patients with knee osteoarthritis. Rheumatol Int 32:1235–1244. https://doi.org/10.1007/s00296-010-1727-4
Güngen GO, Ardic F, Findikoglu G, Rota S (2016) Effect of mud compress therapy on cartilage destruction detected by CTX-II in patients with knee osteoarthritis. J Back Musculoskelet Rehabil 29:429–438. https://doi.org/10.3233/BMR-150629
Guo SY, Ding YJ, Li L et al (2015) Correlation of CD4+ CD25+ Foxp3+ Treg with the recovery of joint function after total knee replacement in rats with osteoarthritis. Genet Mol Res 14:7290–7296
Ha C, Tian S, Sun K, Wang D, Lv J, Wang Y (2015) Hydrogen sulfide attenuates IL-1β-induced inflammatory signaling and dysfunction of osteoarthritic chondrocytes. Int J Mol Med 35:1657–1666. https://doi.org/10.3892/ijmm.2015.2183
Imbeault P, Dépault I, Haman F (2009) Cold exposure increases adiponectin levels in men. Metabolism 58:552–559. https://doi.org/10.1016/j.metabol.2008.11.017
Ionescu EV, Tica I, Oprea C, Iliescu DM, Petcu LC, Iliescu MG (2017) Adiponectn correlation with bioclinical benefits of using netural therapeutic factors in knee osteoarthritis. Acta Endocrinol (buchar) 13:308–313. https://doi.org/10.4183/aeb.2017.308
Jokić A, Sremcević N, Karagülle Z, Pekmezović T, Davidović V (2010) Oxidative stress, hemoglobin content, superoxide dismutase and catalase activity influenced by sulphur baths and mud packs in patients with osteoarthritis. Vojnosanit Pregl 67:573–578. https://doi.org/10.2298/vsp1007573j
Kapoor M, Martel-Pelletier J, Lajeunesse D et al (2011) Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 7:33–42
Karadağ A, Doğan HO (2020) Serum paraoxonase enzyme activity after balneotherapy in patients with fibromyalgia. Medical Science and Discovery 7:429–432. https://doi.org/10.36472/msd.v7i3.350
Karagülle M, Karagülle MZ (2015) Effectiveness of balneotherapy and spa therapy for the treatment of chronic low back pain: a review on latest evidence. Clin Rheumatol 34:207–214. https://doi.org/10.1007/s10067-014-2845-2
Karagülle M, Kardeş S, Karagülle O, Dişçi R, Avcı A, Durak İ, Karagülle MZ (2017) Effect of spa therapy with saline balneotherapy on oxidant/antioxidant status in patients with rheumatoid arthritis: a single-blind randomized controlled trial. Int J Biometeorol 61:169–180. https://doi.org/10.1007/s00484-016-1201-4
Katz U, Shoenfeld Y, Zakin V, Sherer Y, Sukenik S (2012) Scientific evidence of the therapeutic effects of dead sea treatments: a systematic review. Semin Arthritis Rheum 42:186–200. https://doi.org/10.1016/j.semarthrit.2012.02.006
Kim CG, Lee DG, Oh J, Lee YH, Lee YJ, Song PH, Song CH, Ku SK (2020) Effects of balneotherapy in Jeju magma-seawater on knee osteoarthritis model. Sci Rep 10:6620. https://doi.org/10.1038/s41598-020-62867-2
Király M, Kővári E, Hodosi K, Bálint PV, Bender T (2020) The effects of Tiszasüly and Kolop mud pack therapy on knee osteoarthritis: a double-blind, randomised, non-inferiority controlled study. Int J Biometeorol 64:943–950. https://doi.org/10.1007/s00484-019-01764-4
Kloesch B, Liszt M, Krehan D, Broell J, Kiener H, Steiner G (2012a) a) High concentrations of hydrogen sulphide elevate the expression of a series of pro-inflammatory genes in fibroblast-like synoviocytes derived from rheumatoid and osteoarthritis patients. Immunol Lett 141:197–203. https://doi.org/10.1016/j.imlet.2011.10.004
Kloesch B, Liszt M, Steiner G, Bröll J (2012b) b) Inhibitors of p38 and ERK1/2 MAPkinase and hydrogen sulphide block constitutive and IL-1β-induced IL-6 and IL-8 expression in the human chondrocyte cell line C-28/I2. Rheumatol Int 32:729–736. https://doi.org/10.1007/s00296-010-1682-0
Konya C, Goronzy JJ, Weyand CM (2009) Treating autoimmune disease by targeting CD8+ T suppressor cells. Expert Opin Biol Ther 9:951–965
Kuciel-Lewandowska J, Kasperczak M, Paprocka-Borowicz M (2020) Assessment of changes in the hemoglobin level under the influence of comprehensive spa therapy using therapeutic radon-sulfur waters and its correlation with free radical reactions. Evid Based Complement Alternat Med 2020:4637129. https://doi.org/10.1155/2020/4637129
Li L, Fox B, Keeble J, Salto-Tellez M, Winyard PG, Wood ME, Moore PK, Whiteman M (2013) The complex effects of the slow-releasing hydrogen sulfide donor GYY4137 in a model of acute joint inflammation and in human cartilage cells. J Cell Mol Med 17:365–376. https://doi.org/10.1111/jcmm.12016
Liu Y, Liu J, Li X, Wang F, Xu X, Wang C (2017) Exogenous H2S prevents high glucose-induced damage to osteoblasts through regulation of KATP channels. Biochimie 137:151–157. https://doi.org/10.1016/j.biochi.2017.03.009
Lv M, Liu Y, Xiao TH, Jiang W, Lin BW, Zhang XM, Lin YM, Xu ZS (2017) GYY4137 stimulates osteoblastic cell proliferation and differentiation via an ERK1/2-dependent anti-oxidant mechanism. Am J Transl Res 9:1183–1192
Maccarone MC, Kamioka H, Cheleschi S, Tenti S, Masiero S, Kardeş S (2021) Italian and Japanese public attention toward balneotherapy in the COVID-19 era. Environ Sci Pollut Res Int 29:1–9. https://doi.org/10.1007/s11356-021-15058-z
Maccarone MC, Magro G, Solimene U, Scanu A, Masiero S (2021b) From in vitro research to real life studies: an extensive narrative review of the effects of balneotherapy on human immune response. Sport Sci Health. 2021:1–19. https://doi.org/10.1007/s11332-021-00778-z. Epub ahead of print.
Man GS, Mologhianu G (2014) Osteoarthritis pathogenesis - a complex process that involves the entire joint. J Med Life 7:37–41
Martin R, Henley JB, Sarrazin P, Seité S (2015) Skin microbiome in patients with psoriasis before and after balneotherapy at the thermal care center of La Roche-Posay. J Drugs Dermatol 14:1400–1405
Miell JP, Englaro P, Blum WF (1996) Dexamethasone induces an acute and sustained rise in circulating leptin levels in normal human subjects. Horm Metab Res 28:704–707. https://doi.org/10.1055/s-2007-979882
Mooventhan A, Nivethitha L (2014) Scientific evidence-based effects of hydrotherapy on various systems of the body. N Am J Med Sci 6:199–209. https://doi.org/10.4103/1947-2714.132935
Morer C, Roques CF, Françon A, Forestier R, Maraver F (2017) The role of mineral elements and other chemical compounds used in balneology: data from double-blind randomized clinical trials. Int J Biometeorol 61:2159–2173. https://doi.org/10.1007/s00484-017-1421-2
Neumann E, Junker S, Schett G, Frommer K, Müller-Ladner U (2016) Adipokines in bone disease. Nat Rev Rheumatol 12:296–302. https://doi.org/10.1038/nrrheum.2016.49
Nicoletti G, Saler M, Tresoldi MM, Faga A, Benedet M, Cristofolini M (2019) Regenerative effects of spring water-derived bacterial lysates on human skin fibroblast in in vitro culture: preliminary results. J Int Med Res 47:5777–5786. https://doi.org/10.1177/0300060519880371
Ortega E, Hinchado MD, Martín-Cordero L, Asea A (2009) The effect of stress-inducible extracellular Hsp72 on human neutrophil chemotaxis: a role during acute intense exercise. Stress 12:240–249. https://doi.org/10.1080/10253890802309853
Ortega E (2016) The “bioregulatory effect of exercise” on the innate/inflammatory responses. J Physiol Biochem 72:361–369. https://doi.org/10.1007/s13105-016-0478-4
Ortega E, Gálvez I, Hinchado MD, Guerrero J, Martín-Cordero L, Torres-Piles S (2017) Anti-inflammatory effect as a mechanism of effectiveness underlying the clinical benefits of pelotherapy in osteoarthritis patients: regulation of the altered inflammatory and stress feedback response. Int J Biometeorol 61:1777–1785. https://doi.org/10.1007/s00484-017-1361-x
Ortega E, Gálvez I, Martín-Cordero L (2018) Extracellular Hsp70 and low-grade inflammation- and stress-related pathologies. In: Asea A, Kaur P (eds) Heat shock proteins and stress. Heat Shock Proteins 15:13–38
Pascarelli NA, Cheleschi S, Bacaro G, Guidelli GM, Galeazzi M, Fioravanti A (2016) Effect of mud-bath therapy on serum biomarkers in patients with knee osteoarthritis: results from a randomized controlled trial. Isr Med Assoc J 18:232–237
Pedron R, Esposito A, Bianconi I, Pasolli E, Tett A, Asnicar F, Cristofolini M, Segata N, Jousson O (2019) Genomic and metagenomic insights into the microbial community of a thermal spring. Microbiome 7:8. https://doi.org/10.1186/s40168-019-0625-6
Scanu A, Tognolo L, Maccarone MC, Masiero S (2021) Immunological events, emerging pharmaceutical treatments and therapeutic potential of balneotherapy on osteoarthritis. Front Pharmacol 12:681871. https://doi.org/10.3389/fphar.2021.681871
Shani J, Barak S, Levi D, Ram M, Schachner ER, Schlesinger T, Robberecht H, Van Grieken R, Avrach WW (1985) Skin penetration of minerals in psoriatics and guinea-pigs bathing in hypertonic salt solutions. Pharmacol Res Commun 17:501–512. https://doi.org/10.1016/0031-6989(85)90123-7
Shimodozono M, Matsumoto S, Ninomiya K, Miyata R, Ogata A, Etoh S, Watanabe S, Kawahira K (2012) Acute effects of a single warm-water bath on serum adiponectin and leptin levels in healthy men: a pilot study. Int J Biometeorol 56:933–939. https://doi.org/10.1007/s00484-011-0502-x
Sieghart D, Liszt M, Wanivenhaus A, Bröll H, Kiener H, Klösch B, Steiner G (2015) Hydrogen sulphide decreases IL-1β-induced activation of fibroblast-like synoviocytes from patients with osteoarthritis. J Cell Mol Med 19:187–197. https://doi.org/10.1111/jcmm.12405
Silva A, Oliveira AS, Vaz CV, Correia S, Ferreira R, Breitenfeld L, Martinez-de-Oliveira J, Palmeira-de-Oliveira R, Pereira CMF, Palmeira-de-Oliveira A, Cruz MT (2020) Anti-inflammatory potential of Portuguese thermal waters. Sci Rep 10:22313. https://doi.org/10.1038/s41598-020-79394-9
Smallwood MJ, Nissim A, Knight AR, Whiteman M, Haigh R, Winyard PG (2018) Oxidative stress in autoimmune rheumatic diseases. Free Radic Biol Med 125:3–14. https://doi.org/10.1016/j.freeradbiomed.2018.05.086
Sukenik S, Flusser D, Abu-Shakra M (1999) The role of spa therapy in various rheumatic diseases. Rheum Dis Clin North Am 25:883–897. https://doi.org/10.1016/s0889-857x(05)70108-3
Szabó I, Varga C (2020) Finding possible pharmacological effects of identified organic compounds in medicinal waters (BTEX and phenolic compounds). Int J Biometeorol 64:989–995. https://doi.org/10.1007/s00484-019-01808-9
Tékus V, Borbély É, Kiss T, Perkecz A, Kemény Á, Horváth J, Kvarda A, Pintér E (2018) Investigation of Lake Hévíz mineral water balneotherapy and Hévíz mud treatment in murine osteoarthritis and rheumatoid arthritis models. Evid Based Complement Alternat Med 2018:4816905. https://doi.org/10.1155/2018/4816905
Tenti S, Cheleschi S, Galeazzi M, Fioravanti A (2015) Spa therapy: can be a valid option for treating knee osteoarthritis? Int J Biometeorol 59:1133–1143. https://doi.org/10.1007/s00484-014-0913-6
Tett A, Pasolli E, Farina S, Truong DT, Asnicar F, Zolfo M, Beghini F, Armanini F, Jousson O, De Sanctis V, Bertorelli R, Girolomoni G, Cristofolini M, Segata N (2017) Unexplored diversity and strain-level structure of the skin microbiome associated with psoriasis. NPJ Biofilms Microbiomes 3:14. https://doi.org/10.1038/s41522-017-0022-5
Trayhurn P, Duncan JS, Hoggard N, Rayner DV (1998) Regulation of leptin production: a dominant role for the sympathetic nervous system? Proc Nutr Soc 57:413–419. https://doi.org/10.1079/pns19980060
Uçeyler N, Valenza R, Stock M, Schedel R, Sprotte G, Sommer C (2006) Reduced levels of antiinflammatory cytokines in patients with chronic widespread pain. Arthritis Rheum 54:2656–2664. https://doi.org/10.1002/art.22026
Ustyol EA, Karaarslan F, Bekpinar S, Ozkuk K, Erdogan N (2017) Effects of balneotherapy on serum levels of shingosine-1-phosphate in patients with osteoarthritis. Altern Ther Health Med 23:10–14
Uzunoğlu E, Yentur S, Kayar AH, Turan M, Dönmez A, Direskeneli GS, Erdoğan N (2017) Effect of mild heat stress on heat shock protein 70 in a balneotherapy model. Eur J Integr Med 9:86–90
Vaamonde-García C, Vela-Anero Á, Hermida-Gómez T, Fernández-Burguera E, Filgueira-Fernández P, Goyanes N, Blanco FJ, Meijide-Faílde R (2020) Effect of balneotherapy in sulfurous water on an in vivo murine model of osteoarthritis. Int J Biometeorol 64:307–318. https://doi.org/10.1007/s00484-019-01807-w
Varga C (2019) To treat or not to treat? Misbeliefs in spa water disinfection. Int J Biometeorol 63:1135–1138. https://doi.org/10.1007/s00484-019-01722-0
Vela-Anero Á, Hermida-Gómez T, Gato-Calvo L, Vaamonde-García C, Díaz-Prado S, Meijide-Faílde R, Blanco FJ, Burguera EF (2017) Long-term effects of hydrogen sulfide on the anabolic-catabolic balance of articular cartilage in vitro. Nitric Oxide 70:42–50. https://doi.org/10.1016/j.niox.2017.08.004
Viegas J, Esteves AF, Cardoso EM, Arosa FA, Vitale M, Taborda-Barata L (2019) Biological effects of thermal water-associated hydrogen sulfide on human airways and associated immune cells: implications for respiratory diseases. Front Public Health 7:128. https://doi.org/10.3389/fpubh.2019.00128
Wang B, Shao Z, Gu M, Ni L, Shi Y, Yan Y, Wu A, Jin H, Chen J, Pan X, Xu D (2021) Hydrogen sulfide protects against IL-1β-induced inflammation and mitochondrial dysfunction-related apoptosis in chondrocytes and ameliorates osteoarthritis. J Cell Physiol 236:4369–4386. https://doi.org/10.1002/jcp.30154
Wójcik P, Gęgotek A, Žarković N, Skrzydlewska E (2021) Oxidative stress and lipid mediators modulate immune cell functions in autoimmune diseases. Int J Mol Sci 22:723. https://doi.org/10.3390/ijms22020723
Wu J, Yang F, Zhang X, Chen G, Zou J, Yin L, Yang D (2021) Hydrogen sulfide inhibits endoplasmic reticulum stress through the GRP78/mTOR pathway in rat chondrocytes subjected to oxidative stress. Int J Mol Med 47:34. https://doi.org/10.3892/ijmm.2021.4867
Xu ZS, Wang XY, Xiao DM, Hu LF, Lu M, Wu ZY, Bian JS (2011) Hydrogen sulfide protects MC3T3-E1 osteoblastic cells against H2O2-induced oxidative damage-implications for the treatment of osteoporosis. Free Radic Biol Med 50:1314–1323. https://doi.org/10.1016/j.freeradbiomed.2011.02.016
Yan X, Wu H, Wu Z, Hua F, Liang D, Sun H, Yang Y, Huang D, Bian JS (2017) The new synthetic H2S-releasing SDSS protects MC3T3-E1 osteoblasts against H2O2-induced apoptosis by suppressing oxidative stress, inhibiting MAPKs, and activating the PI3K/Akt pathway. Front Pharmacol 8:07. https://doi.org/10.3389/fphar.2017.00007
Yücesoy H, Dönmez A, Atmaca-Aydın E, Yentür SP, Saruhan-Direskeneli G, Ankaralı H, Erdoğan N, Karagülle MZ (2021) Effects of balneological outpatient treatment on clinical parameters and serum cytokine levels in patients with chronic low back pain: a single-blind randomized controlled trial. Int J Biometeorol 2021. doi: https://doi.org/10.1007/s00484-021-02109-w. Epub ahead of print
Zeyl A, Stocks JM, Taylor NA, Jenkins AB (2004) Interactions between temperature and human leptin physiology in vivo and in vitro. Eur J Appl Physiol 92:571–578. https://doi.org/10.1007/s00421-004-1084-7
Zheng L, Zhang Z, Sheng P, Mobasheri A (2021) The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res Rev 66:101249. https://doi.org/10.1016/j.arr.2020.101249
Author information
Authors and Affiliations
Contributions
Conceptualization: Antonella Fioravanti, Sara Cheleschi; data curation: Sara Cheleschi and Iole Seccafico; investigation: Sara Cheleschi, Sara Tenti, Isabel Gálvez, Eduardo Ortega; methodology: Antonella Fioravanti, Sara Cheleschi, and Iole Seccafico; supervision: Antonella Fioravanti and Eduardo Ortega; writing — original draft: Sara Cheleschi, Sara Tenti, Isabel Gálvez, Antonella Fioravanti, and Eduardo Ortega; writing — review and editing: Sara Cheleschi, Sara Tenti, and Antonella Fioravanti.
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Consent to participate
Not applicable
Consent to publish
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheleschi, S., Tenti, S., Seccafico, I. et al. Balneotherapy year in review 2021: focus on the mechanisms of action of balneotherapy in rheumatic diseases. Environ Sci Pollut Res 29, 8054–8073 (2022). https://doi.org/10.1007/s11356-021-17780-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-17780-0