Abstract
Objective
To investigate the relationship between the maxillary sinus ostium 2D area (SOA) and the development of mucosal cysts of the maxillary sinus (MMC).
Methods
Thirty patients (≥ 18 years) with unilateral MMC who underwent paranasal sinus CT (PNsCT) were included in this single-center retrospective study. Non-MMC sinus was used as the control group. Cyst and air volume of the maxillary sinuses, diameter, and 2-dimensional area of the ostium of the patients were calculated in the 3-dimensional volumetric analysis program. Both correlation and linear regression model analyses were performed for the relationship between MMC and SOA.
Results
Thirty patients were included (mean age of 42.30 ± 17.62 years). A total of 15/30 (50%) were male. The mean SOA in patients with MMC (8.91 ± 1.10 mm2) was lower than in patients without MMC (12.94 ± 1.35 mm2), which was statistically significant (p < 0.001). The mean sinus ostium diameter in patients with MMC (2.12 ± 0.71 mm) was higher than in patients without MMC (1.91 ± 0.82 mm), which was statistically insignificant (p = 0.295). There was a statistically significant, good level of negative linear correlation between SOA and total cyst volume (TCV) [correlation coefficient (r) = – 0.680, p < 0.001]). As a result, the regression model consisting of "Age, Sinus air volume, and TCV" variables is a good model and has statistically significant relations with SOA.
Conclusion
In conclusion, small SOAs contribute to the development of MMC. There was a negative correlation between SOA and TCV. In addition, 2D area measurement may be a more accurate method instead of diameter measurement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The maxillary sinus, which contains 10% of the mucosal cysts, is the largest of the paranasal sinuses [1,2,3]. The most common sites of mucosal cysts are the ethmoid and frontal sinuses. [4]. The prevalence of mucosal cysts of the maxillary sinus (MMC) is between 3.2% and 35.6% [2, 3, 5, 6]. Moon et al. studied using magnetic resonance imaging (MRI), they approached the most realistic prevalence and reported it as 7% [6]. MMC is divided into two groups secretory and non-secretory, and 10–20% of MMC is bilateral [2, 3, 5, 6]. Non-secretory cysts are more common. MMCs are usually asymptomatic and detected incidentally on radiological imaging methods. Coronal plane paranasal sinus computed tomography (PNsCT) is more successful in showing anatomical variations and anomalies than cone beam computed tomography (CBCT) and axial plane PNsCT imaging [7].
In the literature, there are many studies investigating the etiology of MMC and the causes affecting the maxillary sinus volume (MSV). When we reviewed the studies investigating the effects of anatomical variations and pathologies of the ostiomeatal unit on the development of MMC, we noticed that the effect of maxillary sinus ostium (MSO) on the development of MMC had not been specifically investigated. In studies, the relationship with these structures has been investigated without excluding patients with more than one pathology that may cause MSO obstruction. Specifically, we think that it would be more accurate to investigate the effect of MSO on the development of MMC. For example, MMCs are detected incidentally in CBCT imaging used by dentists. However, other ostiomeatal unit (OMU) structures, especially MSO, are not included in the field of view (FOV) in CBCT. Therefore, since the maxillary sinus drainage system cannot be evaluated, the effect of these structures on MMC and MSV is not sufficient with CBCT [8]. We also noticed that in the studies, analysis was made by making a single measurement without taking the shape of the MSO into account. In some of these studies, no relationship was found between MSO diameter and MMCs [1, 9]. MSO is oval or slit-shaped and located on the medial wall of the maxillary sinus in the anteroposterior sagittal plane, with a normal diameter of approximately 3–10 mm [10]. In our study, unlike the literatures, we thought that both three-consecutive diameter measurements and two-dimensional (2D) area measurements of the MSO would be more accurate.
To our knowledge, any studies in the literature have evaluated the relationship between MSV and MMC and the 2D area of the MSO. The first aim of our study is to investigate the relationship between 2D area of MSO and MMC development, and the second aim is to investigate whether the measurement of diameter or 2D area can be more accurate in the MSO–MMC relationship.
Materials and methods
Study population
In our study, the data of patients (≥ 18 years) who applied to Amasya University Sabuncuoğlu Şerefeddin Training and Research Hospital Emergency Service and Ear Nose and Throat Polyclinic between June 2021 and August 2022 and who underwent coronal plan PNsCT were examined. This retrospective study was conducted according to the "Declaration of Helsinki and Good Clinical Practice" after ethics committee approval (06.10.2022, issue: 94). In the study, since patient information was obtained from electronic records and censored. The ethics committee did not consider it necessary to obtain written informed consent from the patients.
Inclusion criteria
Adult patients (age > 18 years) with coronal plane PNsCT images were included.
Exclusion criteria
Patients with the following criteria were excluded from the study:
(1) Patients with image artifacts that interfere with the evaluation; (2) Pediatric patients under the age of 18 and pregnant women; (3) Osteomeatal unit variations; (4) Inflammatory and infectious pathologies of the maxillary sinus; (5) Patients with tumor presence or history; (6) Patients with nasal polyps, fractures, odontogenic cysts; (7) Septoplasty, etc. history of sinonasal surgery; (8) Septum perforation; (9) History of facial and nasal trauma; (10) Nasal septum deviation (NSD) angle > 8 (mild: < 9°, moderate: 9°–14°, and severe: 15° and above) [11]; (11) Patients with Type 3 relationship were excluded according to the anatomical relationship between the base of the maxillary sinus and the tooth root (Type 1: None of the tooth roots contacted the sinus floor; Type 2: At least one of the tooth roots was in contact with the sinus floor; Type 3: From the tooth roots at least one of them has entered the sinus floor) [12]; (12) Maxillary sinus cysts causing bone destruction; (13) Presence of accessory MSO; (14) Presence of maxillary sinus septum; (15) Presence of missing teeth in the maxillary posterior regions; (16) Mucosal thickening in the maxillary sinus ≥ 3 mm; (17) Presence of bone spur constricting the OMU and accompanying septum deviation; (18) Patients with a history of intubation; (19) Cases with bilateral MMC were excluded, and the remaining unilateral cases were controlled with the uncontrolled (non-MMC) side.
Thirty patients with unilateral MMC were included in our study. The sinuses of these patients without MMC were used as the control group. As a result, a total of 60 sinus samples were included in the analysis.
CT protocol
PNsCT scans of all patients were performed on 128-slice multidetector CT scanners (GE Medical Systems). CT acquisition specifications: Tube voltage, 120 kVp; tube current, 100–450 mA; scanning direction, craniocaudal; reconstructed kernel, standard; section thickness, 0.625 mm; and section overlap, 0.625 mm. While the patient was in the prone position, images were obtained in the coronal plane from the roof of the frontal sinus to the mandibular bone. Axial and sagittal multi-plane reformat (MPR) images were obtained with a section thickness of 0.625 mm after extraction.
PNsCT imaging analysis
The presence of the following four radiological features was defined as MMC [2] (Fig. 1a):
a PNsCT was performed on a 70-year-old male patient. There was a low attenuation, well-defined, round-shaped mucosal cyst (MMC) at the base of the left maxillary sinus that did not cause bone destruction. b In multiplane remodeling imaging and 3D volumetric post-process analysis, yellow was coded for air density and red was coded for cyst density
-
1.
Cystic lesions of homogeneous density, clearly separated from neighboring structures.
-
2.
No destruction of the adjacent bone.
-
3.
No contact between the tooth roots and the cyst.
-
4.
The contour of the cysts should be smooth and spherical.
Volumetric analysis
Coronal plane PNsCT images of the patients were transferred to the MIMICS (MIMICS® version 10.01; Materialize NV, Leuven, Belgium) program in DICOM format. A radiologist and a biomedical engineer analyzed images together. First, patients were divided into two groups according to the presence of MMC. Density threshold values were determined for air (Minimum: – 1024 HU; Maximum: – 207HU) and MMC (Minimum: – 207 HU; Maximum: 206 HU) (Fig. 1b). Total cyst volume (TCV) and residual air volume were calculated in the sinuses with cysts. The total sinus volume (TSV) sinus was calculated from the sum of these two volumes. In the non-cyst sinus, only the air volume and the TSV were calculated.
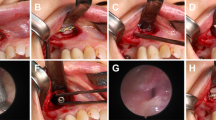
Evaluation of the area and diameter of the maxillary sinus ostium
First, SODs of both MMC and control sinuses were measured 3 times craniocaudal in the anterior–posterior direction from the sagittal plane images of the patients, and the averages of these 3 measurements were recorded (Fig. 2a, b). Then, MSOs were detected from the 3D images of the patients, and a cross-sectional image was obtained in the 2D plane. The ellipse was placed to include as much of the MSO as possible in this section plane. The area of the ellipse was calculated. The 2D cross-sectional area (SOA) of the maxillary sinus ostium was defined by the ellipse area in three-dimensional images (Fig. 2c).
a, b Sagittal plane images showed measurements of SODs on the side with and without MMC (FB: Frontal bone; MB: Maxillary bone). a SOD measurements on the MMC side (mean = 2.033 mm). b SOD measurements on the Non-MMC side (mean = 3.83 mm). c In 3D volumetric analysis, the cross-sectional surface area of both sinus ostium was measured as an ellipse and shown by magnification. 2D area of the sinus ostium (SOA) on the non-cyst side (Right): 10.56 mm2; On the cyst side (Left) SOA: 7.50 mm2. Left maxillary sinus volume (cyst volume: 6121.30 mm3 + residual air volume: 10,180.41 mm3) = 16,301.71 mm3; Right maxillary sinus volume = 14,559.16 mm3
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp. Released 2017. Armonk, NY). Kolmogorov–Smirnov test was used to evaluate the normal distribution of variables. In comparing continuous variables according to MMC groups, Student's t test [mean and standard deviation (SD)] was used for those with normal distribution. Chi-square was used instead of comparing categorical variables according to MMC groups. Pearson test was used for correlation analysis between variables. A multiple linear regression model was used to identify continuous variables affecting SOA value.
Y: Dependent variable (Sinus ostium area), β0: Intercept, β1, β2, β3, β4: Regression coefficients, X1, X2, X3, X4: Predictors.
The model fit was assessed using the appropriate residual and goodness-of-fit statistics. R-square is the value of what percentage of the variation in the dependent variable is explained by the independent variable and was used to calculate the power of the model. p < 0.05 was considered statistically significant.
Results
Demographic and anatomic features
A total of 60 samples of 30 patients with unilateral MMC were included (mean age of 42.30 ± 17.62 years). A total of 15/30 (50%) were male. There was no statistically significant relationship between the presence of MMC, and age and gender (p = 0.099; p = 0.99) (Table 1). The mean SOA (8.91 ± 1.10 mm2) in patients with MMC was lower than in patients without MMC (12.94 ± 1.35 mm2), which was statistically significant (p < 0.001). The mean SOD in patients with MMC (2.12 ± 0.71 mm) was higher than in patients without MMC (1.91 ± 0.82 mm), which was statistically insignificant (p = 0.295). The mean TSV in patients with MMC (15,249.90 ± 4511.96 mm3) was higher than in patients without MMC (13,783.06 ± 4276.02 mm3), which was statistically insignificant (p = 0.201) (Table 2).
Correlation between SOA and TCV
There was a statistically significant, good level of negative linear correlation between SOA and TCV [correlation coefficient (r) = – 0.680, p < 0.001]). There was a statistically significant, moderately positive linear correlation between SOA and sinus air volume (r = 0.451, p = 0.006) (Table 3).
Multivariable linear regression
The following formula was obtained to estimate the dependent variable SOA in the model obtained as a result of the regression analysis (Table 4);
When the multiple regression analysis model summary given in Table 4 was examined, R2 = 0.627 was obtained. According to this result, the 62.7% change in the output area is explained by the independent variables in the model. The remaining 37.3% is the effect of other variables not included in the model. As a result, the regression model consisting of "Age, Sinus air volume, and TCV" variables is a good model and has statistically significant relations with "Sinus ostium area".
Discussion
In this study, we investigated the relationship between mucosal cysts of the maxillary sinus (MMC) and maxillary sinus ostium 2D area (SOA). We also investigated whether it is more accurate to measure the sinus ostium as a diameter or as a 2D area. Our results showed a good, statistically significant, negative correlation between MMC and SOA (r = – 0.680; p < 0.001). Linear regression analysis was applied to estimate SOA measurement on the side with MMC. Age, sinus air volume, and TCV were statistically significant independent variables in the estimation of SOA value. The mean SOA in patients with MMC was lower than in patients without MMC, which was statistically significant (p < 0.001). However, SOD was higher on the side with MMC and it was not statistically significant (p = 0.295).
In MMC histology, there is a dense fluid between the thin membrane structures consisting of connective tissue cells [2]. MMC occurs due to edema in the subepithelial connective tissue. Less common, retention cysts are formed due to obstruction of the mucosal secretory glands and are most commonly detected in the maxillary sinus. It may be due to an inflammatory exudate developing in the submucosal connective tissue or a rupture of the mucous glands [2, 3, 13, 14]. Allergy, chronic rhinosinusitis, and barotrauma-causing inflammatory processes have been suggested in the etiology of MMC [2, 3, 15]. Especially in studies investigating the physiopathology of allergy, they suggested that cysts may develop as a result of mucosal damage due to allergic edema, and they strengthened their theses due to inflammatory markers, such as immunoglobulin and complement detected in cyst aspirate [2, 3, 13, 14, 16]. However, the lack of increase in immunoglobulin E and eosinophil blood contradicted their thesis [16,17,18]. In another study, they thought that due to the high protein content and high density of the cyst aspirate, it was not due to an allergic reaction but could be caused by infection [16, 17, 19].
The secretion accumulated in the maxillary sinus is mobilized from the sinus floor to the ostium in the medial superior, due to mucociliary clearance [7, 20, 21]. Mucociliary clearance is the primary defense mechanism of the respiratory tract against inhaled pathogens [22, 23]. As a result of impaired mucociliary activity and narrowing or obliteration of the sinus ostium, the secretion will not be able to reach the nasal cavity and will accumulate in the sinus. Chronic rhinosinusitis may develop as a result of inflammation in the mucosal tissue and occlusion of the mucosal channels [3, 5, 17,18,19,20,21]. As a result, the mucosal glands are unable to secrete, become cystic, and MMCs may develop [2, 3, 13, 14, 16,17,18,19]. Also, another study reported that impaired mucociliary clearance led to the development of MMC, and the size of MMC increased too much, reducing mucociliary clearance, and creating a stalemate [20, 21, 24]. Arslan et al. reported that MSO occlusion increases the risk of developing MMC by 3.64 times [4]. There are also studies in the literature reporting that there is no relationship between MMC and allergy, dental problems, or blocked OMU [1, 3, 5, 25]. Unlike Harar et al. suggested that the first event in the development of MMC was OMU obstruction and then became patent as the cyst persisted [3]. Bhattacharyya et al. reported that the mean MSO size was smaller on the sinus with MMC than on the sinus without MMC, but it was not statistically significant [1]. Unlike our study, other studies may be insignificant because they evaluate MSO with diameter measurement instead of area measurement. We measured the 2D area of the MSO and this measurement technique was our main difference. The important differences of our study from other studies are that while other studies did not exclude many factors that play a role in the etiology of MMC development, our study had a large number of exclusion criteria. The good and statistically significant negative correlation between total MMC volume and SOA in our study may be related to these physiopathological processes.
The MSO is oval-shaped from posterior to anterior and from outside to inside on the inner wall of the maxillary sinus [10]. In the literature, measurements were taken in a single section on coronal plane PNsCT images. However, we thought that this was not an accurate measurement method due to the oval shape of the MSO and we made two different measurements. First, we measured the diameter from 3 consecutive sections with the sinus ostium on the coronal plane PNsCT images and used the average in the analysis. Second, we calculated the output 2D area of the sinus ostium in the 3D images. Mean SOA was significantly lower on the side with MMC and it was statistically very significant (p < 0.001). On the contrary, we found that the mean SOD was higher on the side with MMC and it was not statistically significant (p = 0.295). The difference in the two different measurement methods showed us that the area measurement could be more accurate.
There were some important advantages in our study. In our study, our most important advantage was to specifically investigate the effect of the size of MSO on the development of MMC using a large number of exclusion criteria. Another advantage of our study is the different results we obtained because we measured the areas of the MSOs due to the oval shape of the MSO, instead of measuring the diameter in a single section.
There were some limitations in our study. First, our study was a single-center, retrospective analysis. Second, immunodeficiency, a history of allergy, and systemic diseases that may impair mucociliary clearance were not investigated. Third, there was no correlation with endoscopic examination in patients.
Conclusion
In conclusion, small SOAs contribute to the development of MMC. There was a negative correlation between SOA and TCV. In addition, according to our results, we think that 2D area measurement may be a more accurate method instead of diameter measurement due to the oval shape of the MSO. We think that new studies with larger sample numbers will be beneficial.
Data availability
The data that support the findings of this study are available on request from the corresponding author, [ATK].
References
Bhattacharyya N. Do maxillary sinus retention cysts reflect obstructive sinus phenomena? Arch Otolaryngol - Head Neck Surg. 2000;126:1369–71.
Giotakis EI, Weber RK. Cysts of the maxillary sinus: A literature review. Int Forum Allergy Rhinol. 2013;3:766–71.
Harar RPS, Chadha NK, Rogers G. Are maxillary mucosal cysts a manifestation of inflammatory sinus disease? J Laryngol Otol. 2007;121:751–4.
Arslan IB, Uluyol S, Demirhan E, Kozcu SH, Pekcevik Y, Cukurova I. Paranasal sinus anatomic variations accompanying maxillary sinus retention cysts: a radiological analysis. Turk Otolarengoloji Arsivi/Turkish Arch Otolaryngol. 2017;55:162–5.
Kanagalingam J, Bhatia K, Georgalas C, Fokkens W, Miszkiel K, Lund VJ. Maxillary mucosal cyst is not a manifestation of rhinosinusitis: Results of a prospective three-dimensional CT study of ophthalmic patients. Laryngoscope. 2009;119:8–12.
Moon IJ, Kim SW, Han DH, Shin JM, Rhee CS, Lee CH, et al. Mucosal cysts in the paranasal sinuses: Long-term follow-up and clinical implications. Am J Rhinol Allergy. 2011;25:98–102.
Gotwald TF, Zinreich SJ, Corl F, Fishman EK. Three-dimensional volumetric display of the nasal ostiomeatal channels and paranasal sinuses. Am J Roentgenol. 2001;176:241–5.
Carmeli G, Artzi Z, Kozlovsky A, Segev Y, Landsberg R. Antral computerized tomography pre-operative evaluation: relationship between mucosal thickening and maxillary sinus function. Clin Oral Implants Res. 2011;22:78–82.
Nouraei SAR, Elisay AR, Dimarco A, Abdi R, Majidi H, Madani SA, et al. Variations in paranasal sinus anatomy: implications for the pathophysiology of chronic rhinosinusitis and safety of endoscopic sinus surgery. J Otolaryngol-Head Neck Surg Le J d’oto-rhino-laryngologie Chir cervico-faciale. 2009;38:32–7.
Vaid S, Vaid N. Normal anatomy and anatomic variants of the paranasal sinuses on computed tomography. Neuroimaging Clin. 2015;25:527–48.
Elahi MM, Frenkiel S, Fageeh N. Paraseptal structural changes and chronic sinus disease in relation to the deviated septum. J Otolaryngol. 1997;26:236–40.
Aksoy U, Orhan K. Association between odontogenic conditions and maxillary sinus mucosal thickening: a retrospective CBCT study. Clin Oral Investig Clinical Oral Investig. 2019;23:123–31.
Wang JH, Jang YJ, Lee B. Natural course of retention cysts of the maxillary sinus: long-term follow-up results. Laryngoscope. 2007;117:341–4.
Omezli MM, Torul D, Cankaya S. Frequency and characteristics of retention cysts in the maxillary sinus in a Turkish patient population. Int J Stomatol Occlusion Med. 2015;8:17–21.
Jalisi S, Seo S, Lee M, Mardirossian V. Carcinoma cuniculatum of the oral cavity: a histological and clinical dilemma. Laryngoscope. 2009;119:8.
Abesi F, Mirshekar AR, Babaee N, Heidari H, Mohammadzadeh I. Prevalence of mucous retention cysts of maxillary sinus in panoramic radiography. J Babol Univ Med Sci. 2013;15:103–7.
Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2010;109:e80–7.
White SC, Pharoah MJ. Oral radiology-E-book: principles and interpretation. Elsevier Health Sciences; 2014.
Mafee MF, Valvassori GE, Becker M. Imaging of the head and neck. (No Title). 2005.
Tassoker M, Magat G, Lale B, Gulec M, Ozcan S, Orhan K. Is the maxillary sinus volume affected by concha bullosa, nasal septal deviation, and impacted teeth? A CBCT study Eur Arch Oto-Rhino-Laryngology. 2020;277:227–33.
Smith KD, Edwards PC, Saini TS, Norton NS. The prevalence of concha bullosa and nasal septal deviation and their relationship to maxillary sinusitis by volumetric tomography. Int J Dent. 2010;2010:1–5.
Cohen NA. Sinonasal mucociliary clearance in health and disease. Ann Otol Rhinol Laryngol. 2006;115:20–6.
Beule AG. Physiology and pathophysiology of respiratory mucosa of the nose and the paranasal sinuses. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2010;9:15–34.
Yenigun A, Fazliogullari Z, Gun C, Uysal II, Nayman A, Karabulut AK. The effect of the presence of the accessory maxillary ostium on the maxillary sinus. Eur Arch Oto-Rhino-Laryngology. 2016;273:4315–9.
Albu S. Symptomatic maxillary sinus retention cysts: should they be removed? Laryngoscope. 2010;120:1904–9.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ATK: Methodology. ATK, LV: Formal analysis and investigation. ATK: Writing—original draft preparation. ATK, LV: Writing—review and editing. ATK, LV: Supervision. All of the authors declare that they have all participated in the design, execution, and analysis of the paper and that they have approved the final version
Corresponding author
Ethics declarations
Conflict of interest
In this study, there were no competing interests or financial benefits to the authors.
Ethical approval
This retrospective and the single-center study was approved by the Ethical Committee of Amasya University Sabuncuoğlu Şerefeddin Training and Research Hospital 6 September 2022, number: 94). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
The study is retrospective, patient information was obtained from electronic records and censored. Since the study was retrospective, the ethics committee did not find it necessary to obtain written informed consent from the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaya, A.T., Uğur, L. Relationship between maxillary sinus mucosal cyst and sinus ostium 2D area in three-dimensional volumetric paranasal CT ımages. Oral Radiol 40, 199–206 (2024). https://doi.org/10.1007/s11282-023-00722-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-023-00722-6