Abstract
This retrospective study aimed to analyze volumetric changes of the maxillary sinus after modified endoscopic-assisted sinus surgery (MESS) and to assess short-term treatment outcomes. The volumes of the total maxillary sinus, aeration, and sinus pathology were calculated using computed tomography data obtained prior to surgery and six months after surgery. Postoperative radiological improvement was assessed using the Lund–Mackay score. Bone regeneration around the bony window was evaluated during plate removal. A total of 32 patients were evaluated. Compared with before surgery, air and sinus pathology volumes improved significantly (air, increase by 6.0 cm3, p < 0.001; sinus pathology, decrease by 6.4 cm3, p < 0.001). However, there was no statistically significant change in the total maxillary sinus volume after surgery. The preoperative Lund–Mackay score was 2.9, decreasing to 0.4 six months after surgery (p < 0.001). The only predictors of postoperative aeration rate and Lund–Mackay score were preoperative sinus pathology volume (p = 0.049) and Lund–Mackay score (p = 0.015), respectively. The continuity between the bony window and surrounding sinus wall was restored in all patients. The results of this study suggest that MESS can be a successful, effective, and minimally invasive surgical treatment option for treating maxillary sinus diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Since the advent of the endoscope, the standard treatment modality for treating inflammatory conditions or benign pathologies in the maxillary sinus has changed from a radical approach to minimally invasive endoscopic sinus surgery (ESS)2. In ESS, the key is to clear the pathology at the ostiomeatal complex. ESS is based on the concept that resolving the obstruction of the common drainage pathway can improve ventilation and mucociliary clearance, thereby restoring the physiological function of the maxillary sinus2. Despite reports of successful surgical outcomes in endonasal ESS, the success rate of revision surgery for recurrent maxillary sinusitis is as low as 69.8%3. Although ESS has been suggested to completely remove pathological mucosa (including edema, hyperplasia, or metaplasia) in refractory maxillary sinusitis, however, it is difficult to remove pathologic lesions in the lateral or antero-medial region of the maxillary sinus using conventional ESS2,4. Additionally, in cases of odontogenic maxillary sinusitis, it is difficult to clear dental pathology through ESS due to its narrow field of view and limited range of motion. Removal of foreign bodies, such as dental implants, teeth, or endodontic material, also requires wider access to the maxillary sinus than ESS can provide5. Therefore, in certain situations, more radical surgical treatments are needed, such as radical antrectomy with mega-antrostomy through an endonasal endoscopic approach or open surgery through an intraoral transmaxillary approach6,7.
The Caldwell-Luc procedure (CLP) is an open surgery through the intraoral approach that has been widely performed for several decades. Although CLP allows rapid symptom improvement, it has potential complications such as postoperative maxillary cyst, facial asymmetry, and facial paresthesia8. Another complication of the CLP is difficulty in recovering physiological function of the maxillary sinus after surgery. Complete stripping of the inflamed hyperplastic sinus mucosa in CLP often causes osteogenesis and osteitis of the sinus wall and damages the mucociliary function of the sinus membrane, which can lead to atrophy of the maxillary sinus cavity and disturb physiological function9. Due to these complications, a surgical method that only removes pathological mucosa through direct access under an endoscopic view has recently been preferred.
For various pathologic conditions in the maxillary sinus excluding malignant tumors, we performed modified endoscopic-assisted sinus surgery (MESS)10,11. This procedure preserves the normal sinus membrane because only pathological mucosa is removed. The procedure is performed via an intraoral approach with the help of an endoscope and rigid fixation of a bony window, which is created for direct access to the sinus cavity. In addition, widening of the narrowed ostium is performed, if necessary. Maxillary sinus surgery through various intraoral approaches, including MESS, has effectively resolved maxillary sinus diseases. However, the direct removal of lesions within the maxillary sinus and the creation of bony windows through these intraoral approaches may change the volume of the maxillary sinus after surgery, as in CLP. Therefore, this study aims to investigate the treatment outcome of MESS for treating inflammatory or cystic pathologies in the maxillary sinus and to assess volumetric changes of the maxillary sinus after MESS.
Patients and methods
Patients
This retrospective case series included consecutive patients who underwent MESS for the treatment of inflammatory conditions or cystic pathologies in the maxillary sinus at the Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital, Seoul, South Korea, between 2020 and 2022. The inclusion criteria were as follows: (1) the availability of computed tomography (CT) images taken preoperatively (T0) and at least 6 months after surgery (T1) using multi-detector CT; (2) patients in whom the plate that was used for fixation of the bony window was removed. Patients who met following exclusion criteria were excluded: (a) malignant tumors; (b) congenital facial deformity; (c) a history of radiation therapy in the head and neck area; (d) CT images with a field of view that does not include the maxillary sinus, ethmoidal sinus, frontal sinus, sphenoidal sinus, or ostiomeatal complex; (e) cone-beam CT images.
Surgical procedures
All patients received MESS under general anesthesia or intravenous conscious sedation (Fig. 1). After incision of approximately 2 cm was made in the maxillary vestibular area, the mucoperiosteum was elevated to expose the antero-lateral wall of the maxillary sinus. To allow direct access to the maxillary sinus cavity, a bony window approximately 10 mm × 10 mm in size was made on the sinus wall with a small round bur of 0.5 mm. Before the complete separation of the bony window, a micro-plate for stabilization of the bony window was applied and fixed to the maxillary sinus wall with micro-screws. A maxillary sinus membrane was incised using a No. 12 scalpel. The sinus pathology and mucosal status within the maxillary sinus were evaluated using an endoscope. When edematous, hyperplastic, and/or inflamed mucosa was present, only the pathological tissue above the periosteum was selectively removed. Therefore, the periosteum was preserved as much as possible. In cases where a foreign body (such as tooth remnant, dental implant or bone graft material) migrated into the maxillary sinus, the foreign body was removed completely. Then, the entire maxillary sinus mucosa was examined using an endoscope to confirm the presence of any inflammatory pathologic lesions. After multiple gentle warm irrigations of the sinus cavity, the incised sinus membrane was sutured as much as possible using Vicryl 6 − 0 (Polyglactin 910, Johnson & Johnson Co., Somerville, NJ, USA). Then, the bony window was firmly fixed in its original position using pre-applied microplates and screws.
Surgical procedures of modified endoscopic-assisted sinus surgery. (A) Mucoperiosteal elevation, (B) Creation of the bony window and application of the micro-plate, (C) Separation of the bony window and access to the sinus cavity, (D) Examination of the sinus pathology and sinus membrane, (E,F) Removal of the sinus pathology (dental implant in this case) using endoscope, (G) Evaluation of the sinus membrane (a normal sinus membrane showing a vascular network and a patent ostium were found in this case), (H) Reposition and fixation of the bony window.
Postoperative healing and recurrence were assessed clinically and radiographically using a panoramic view and Waters’ view. After resolution of the maxillary sinusitis was observed in clinical and radiological examinations, a second operation was performed under local anesthesia to remove the plate and screws.
Radiographic evaluation
To assess the severity of the maxillary sinusitis and treatment outcomes, preoperative (T1) and postoperative (T2) CT images were evaluated. The degree of maxillary sinus opacification was evaluated by classifying it into no opacification, partial opacification, subtotal opacification, and total opacification12. Total opacification was defined as the absence of air within the maxillary sinus. Subtotal opacification was defined as the presence of air in < 30% of the maxillary sinus volume. Partial opacification was defined when opacification was limited to the sinus floor and air occupied more than 30%. The CT findings of the maxillary sinus, anterior and posterior ethmoidal sinuses, sphenoid sinus, frontal sinus, and ostiomeatal complex were scored using the Lund–Mackay (LM) scoring system as follows: 0, no opacification; 1, partial opacification; 2, complete opacification. For the ostiomeatal complex, the CT images were scored as 0 (not obstructed) or 2 (obstructed) depending on the presence or absence of obstruction.
Volumetric analysis
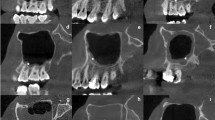
All CT scans were obtained by using SOMANTON definition edge (Siemens AG, Erlangen, Germany) within the parameters of 140 kVp, 20 mA and 0.19 s exposure time with a slice thickness of 2 mm. The images were saved as the Digital Imaging and Communications in Medicine (DICOM) format. After CT data were imported to Mimics software (Materialise, Leuven, Belgium), the area excluding hard tissue was determined using a threshold ranging from − 1024 to 226 Hounsfield units. Next, in order to examine the maxillary sinus alone, the other paranasal sinuses and nasal airway were removed from the determined area using the following borders of the maxillary sinus: bony wall of the maxillary sinus and the narrowest space of the ostium between the infundibulum and uncinate process. Through the reconstruction process, a three-dimensional model of the maxillary sinus was obtained, and the total sinus volume was calculated (Fig. 2). The aeration area was obtained using a threshold value ranging from − 1024 to − 450 Hounsfield units, from which the area of sinus pathology was then calculated13. The three-dimensional models for the total maxillary sinus, aeration, and sinus pathology were reconstructed, and each respective volume was calculated.
Statistical analysis
The Kolmogorov-Smirnov test was performed to determine the normal distribution of the data. The Wilcoxon Signed-rank test was conducted to assess postoperative changes in the LM score and the volumes of the total maxillary sinus, aeration, and sinus pathology. Comparisons between the operated- and non-operated sides were made using the Mann–Whitney U test. To evaluate the reproducibility of the volumetric measurements, 60 randomly selected maxillary sinuses were analyzed by the same examiner over a 12-week interval. To determine the influencing factors for postoperative outcomes, including postoperative aeration rate (the ratio of air volume to total maxillary sinus volume) and LM score, univariate linear regression analysis was performed for variables including age, sex, preoperative LM score, type of sinus pathology, preoperative volumes of the total maxillary sinus, aeration, and sinus pathology, and preoperative aeration rate. All variables with p < 0.2 in the univariate regression analysis were entered into a stepwise multiple linear regression with backward elimination to select an appropriate model. Reproducibility was assessed using intraclass correlation coefficients for total sinus volume and ranged from 0.969 to 0.999. The significance level was set at p < 0.05. All statistical analysis was performed using SPSS 26.0 for Windows (SPSS IBM, New York, USA).
Ethical approval
This study was approved by the Institutional Review Board of Seoul National University Dental Hospital (IRB no. ERI23027). All methods were performed in accordance with the relevant guidelines and regulations. All patients were informed of the surgical procedure with potential risks and benefits, and written informed consent was obtained from all patients.
Results
A total of 32 patients (18 males and 14 females, mean age 44.0 ± 19.1 years, age range 18–81 years) were recruited for this study. The demographic and clinical data are presented in Table 1. 21 patients underwent MESS for the treatment of maxillary sinusitis (Group 1; 9 males and 12 females; mean age, 50.9 ± 19.7 years), and 11 patients underwent the procedure for cystic diseases in the maxillary sinus (Group 2; 5 males and 6 females; mean age, 30.8 ± 9.9 years). The pathologies associated with maxillary sinusitis in Group 1 included peri-implantitis (4 patients), maxillary sinus floor augmentation surgery (3 patients), apical periodontitis (3 patients), and displaced dental root (3 patients). In Group 2, eight patients were diagnosed with antral pseudocysts and three patients with odontogenic keratocysts.
Total opacification, subtotal opacification, and partial opacification were found preoperatively in 6 sinuses, 6 sinuses, and 20 sinuses, respectively (Table 2). At 6 months postoperatively, complete resolution of the sinus opacification after surgery were observed in 28 sinuses, while one and three patients exhibited subtotal opacification and partial opacification of the maxillary sinus, respectively. The LM score decreased significantly from 2.9 ± 2.5 preoperatively to 0.4 ± 0.8 postoperatively (p < 0.001) (Fig. 3). Specifically, with respect to ostial patency, obstruction of ostiomeatal complex was observed in 12 out of 32 patients preoperatively, while it was found in only one patient postoperatively.
Depending on the type of sinus pathology, 6, 5, and 10 maxillary sinuses in Group 1 had total opacification, subtotal opacification, and partial opacification before surgery, respectively (Table 3). Postoperatively, in Group 1, there were only three partial opacifications. Group 2 included 1 subtotal opacification and 10 partial opacifications before surgery, but only 1 subtotal opacification 6 months after surgery. The LM score for Group 1 was 3.8 ± 2.7 before surgery and 0.5 ± 0.9 at 6 months after surgery (p < 0.001). Group 2 had a mean LM score of 1.4 ± 0.5 before surgery and 0.3 ± 0.6 at 6 months after surgery (p = 0.003). Regarding ostial patency, all 12 patients who showed preoperative obstruction of the ostiomeatal complex belonged to Group 1, and all but one patient recovered ostiomeatal complex patency postoperatively. In Group 2, there were no changes in ostiomeatal complex patency postoperatively.
In the volumetric analysis on the operated side, the air volume increased significantly from 11.2 ± 10.5 cm3 (46.5%) to 18.2 ± 8.7 cm3 (82.1%) postoperatively (p < 0.001), while the sinus pathology volume decreased significantly from 10.7 ± 6.7 cm3 (54.4%) to 3.4 ± 4.3 cm3 (17.9%) (p < 0.001) (Table 4). There were no significant changes in the total sinus volume after MESS (p = 0.822). In comparison with the non-operated side, there was no significant difference in the total maxillary sinus volume on the operated side both before (p = 0.092) and 6 months after surgery (p = 0.067). Depending on the types of sinus pathologies, the preoperative total maxillary sinus and air volumes were 19.7 ± 5.7 cm3 and 6.7 ± 9.3 cm3 (30.1%) in Group 1, and 25.0 ± 5.6 cm3 and 19.8 ± 6.6 cm3 (75.1%) in Group 2 (Table 5). Postoperatively, the air volume increased significantly to 15.9 ± 7.4 cm3 (79.7%) in Group 1 (p < 0.001) and 22.8 ± 9.5 cm3 (86.7%) in Group 2 (p = 0.041). However, there were no significant changes in the total maxillary sinus volume for either Group 1 (p = 0.414) or 2 (p = 0.374).
In univariate regression analysis to determine factors affecting treatment outcomes, preoperative volumes of aeration and sinus pathology showed a significantly positive (p = 0.036) and negative (p = 0.049) association with postoperative aeration rate, respectively (Table 6). In terms of postoperative LM score, preoperative LM score and sinus pathology volume showed a significant positive association (p = 0.015 and p = 0.024, respectively) with postoperative LM score, while preoperative aeration rate and preoperative air volume exhibited a significant negative association (p = 0.023 and p = 0.039, respectively). In final multiple linear regression analysis, the preoperative sinus pathology volume was the only variable significantly associated with postoperative aeration rate (regression coefficient, β, − 1.221; 95% CI, − 2.438 to − 0.005; p < 0.049; adjusted R2 = 0.094), and preoperative LM score was the only variable significantly associated with postoperative LM score (regression coefficient, β, 0.142; 95% CI, 0.030–0.255; p < 0.015; adjusted R2 = 0.154).
With regard to postoperative bone healing of the repositioned bony window, all patients experienced partial or complete bone regeneration with restoration of continuity with the maxillary sinus wall around the window (Fig. 4).
Discussion
The purpose of this study was to assess the treatment outcome after MESS using three-dimensional volumetric analysis. The study’s hypothesis was that the maxillary sinus volume can be maintained after MESS with significant radiological improvement. The specific aim was to compare the changes in the total maxillary sinus volume and aeration between inflammatory and cystic diseases. In this study, the sinus aeration recovered significantly during the postoperative period, while the volume of the maxillary sinus cavity remained stable. Those with inflammatory diseases in Group 1 exhibited a greater increase in air volume postoperatively than did those in Group 2 with cystic diseases. However, both groups showed a similar volume percentage of sinus aeration and no significant changes in the total sinus volume approximately 6 months after surgery. The only predictors of postoperative aeration rate and LM score were preoperative sinus pathology volume and LM score, respectively.
An intraoral approach has several advantages over other surgical techniques such as ESS, as follows: (1) optimal visualization and access to the specific region in the maxillary sinus (2) easy removal of the pathologic tissue and/or odontogenic infection origin (3) preservation of the normal, physiologic nasal structures. Despite these advantages, several concerns have been raised about postoperative healing of the maxillary sinus4,14. First, mucosal stripping to remove inflammatory tissue within the sinus leads to osteogenesis and fibrosis on the inner surface of the sinus wall, which can cause hypoplasia and dysfunction of the maxillary sinus1. Similar postoperative changes can be frequently found after CLP. Although it is a study on the endonasal approach, Kikawada et al.1. emphasized the preservation of the periosteum in removing pathological mucosa to promote regeneration of the normal maxillary sinus and maintain sinus volume. By using a high-pressure water jet to remove diffuse pathologic mucosa and to preserve the periosteum, they achieved resolution of maxillary sinus disease with no reduction of cavity in 81% of patients. In the present study, only the pathological mucosa in the maxillary sinus was removed through an intraoral approach, and the periosteum was preserved. To preserve the periosteum, the pathological tissue identified through an endoscope was removed using a flexible suction tip with a smooth rubber tip and a curved curette. Numerous vascular structures remaining in the inner wall of the maxillary sinus were confirmed through the endoscope. In addition, the remaining sinus mucosa was continuously checked through tactile sensation to determine whether the periosteum was intact. In the postoperative volumetric analysis, for the patients with maxillary sinusitis, the overall total maxillary sinus volume was maintained 6 months after surgery. Although the short-term evaluation of six month is one of limitations of this study, the selective removal of only pathological tissue and the preservation of the periosteum to the greatest extent possible may have helped minimize osteogenesis of the sinus walls and maintaining the cavity volume. Of all 32 patients, 11 patients showed a decrease in the maxillary sinus volume on the operated side. Of these 11 patients, 7 patients exhibited a volume decrease of less than 10%, 2 patients showed a volume decrease of more than 10% but less than 20%, and 1 patient showed a volume reduction of 41.1%. The patient who showed the greatest volume reduction has a history of previous ESS and underwent MESS as a reoperation due to persistent lesions. Before MESS, this patient characteristically showed a thickened maxillary sinus bony wall due to severe osteitis15.
Another concern related to the intraoral approach is the complications arising from osseous defect and scar tissue. These include obliteration of the maxillary sinus due to ingrowth of surrounding soft tissue, impairment of normal physiological function, soft tissue depression caused by an osseous defect, and paresthesia of the infraorbital neve due to scar contracture16,17,18. Additionally, the risk of complications during maxillary sinus floor augmentation for implant rehabilitation can be increased. Therefore, several investigators have proposed repositioning the bony window using absorbable suture material or methods that do not separate the bony window from the periosteum or sinus mucosa19,20. In the present study, to enhance postoperative bone healing and recovery of the sinus, several efforts were made during the formation and repositioning of the bony window. First, bony window was created using a small round bur of 0.5 mm diameter to minimize the bony gap. Additionally, to prevent the bony window from shifting to one side and causing a wider gap on the opposite side during fixation, the microplate was pre-fixed before separating the bony window, which minimized positional changes of the bony window. Finally, to minimize the size of the bony window and prevent its micromovement, rigid fixation using a 4-hole microplate was applied in most cases. When the metal plate was removed, the continuity between the bony window and surrounding sinus wall was restored in all patients. The plate was removed at least 6 months after MESS, with an average removal time of 10.6 months. Although repositioning of the bony window using the plate has disadvantages such as the complexity of the procedure and the need to remove it, these results suggest that the efforts made during the surgical procedure may have led to predictable and favorable bone regeneration.
In the present study, all but one patient with maxillary sinusitis could be classified as having odontogenic origin. Specific management guidelines to treat odontogenic maxillary sinusitis have not been clearly established. Yoshida et al.21 only extracted infected tooth in 32 patients with OMS and reported that the OMS resolved in 20 patients (62.5%). They suggested that the extent of preoperative opacification of the ethmoidal sinus and frontal sinus is significantly associated with OMS healing when treated by extraction alone. In a retrospective study of 98 patients with OMS12, clinical and radiological resolution was reported in 91 patients (92.9%) through an intraoral approach for treating the odontogenic origin with simultaneously ESS. In the present study, 18 of 21 patients with maxillary sinusitis (85.7%) achieved complete resolution following MESS, with all 21 patients showing clinical resolution and radiological improvement postoperatively.
Regarding the cystic pathologies, 8 antral pseudocysts and 2 odontogenic keratocysts were included in this study. Most cases of antral pseudocysts and odontogenic keratocysts do not cause inflammation in the maxillary sinus; therefore, such cases can usually be treated relatively simply by enucleation. Therefore, the overall condition of the maxillary sinus mucosa is normal and there is little damage to the mucosa during surgery. These patients typically have favorable postoperative healing of the sinus. Based on this phenomenon, patients with non-inflammatory cystic disease were included in this study and analyzed as a control group to compare the surgical outcome and volume changes after MESS to those of patients with inflammatory sinus diseases.
Lastly, we evaluated the prognostic factors influencing the treatment outcomes of MESS through univariate and multiple regression analyses. Preoperative pathology volume within the maxillary sinus and preoperative LM were identified as the sole prognostic factors for postoperative maxillary sinus aeration rate and postoperative LM score. These results indicate that the more severe the preoperative maxillary sinus disease, the poorer the treatment outcomes. They emphasize the importance of early diagnosis and treatment of maxillary sinus diseases to achieve successful treatment outcomes, including functional recovery of the sinus.
This study has several limitations. First, the CT slice thickness was relatively thick (2 mm), which may affect the exact calculation of the total maxillary sinus volume and aeration volumes. Second, this study has a relatively small number of patients due to its retrospective nature. Although more patients received modified endoscopic sinus surgery than were included, fewer patients had undergone pre- and postoperative CTs. In future studies, it is necessary to evaluate volumetric changes of the sinus volume in a greater number of patients using thinner CT slices.
Conclusions
The findings of this study suggest that MESS can be an effective treatment option for maxillary sinus diseases based on its successful treatment outcomes and stable postoperative recovery of the maxillary sinus. Volumetric analysis showed improved aeration and sinus pathologies, while maintaining total maxillary sinus volume without atrophy or osteogenesis.
Data availability
The datasets generated during and/or analyzed during this study are available from the corresponding author on reasonable request.
References
Kikawada, T., Nonoda, T., Matsumoto, M., Kikura, M. & Kikawada, K. Treatment of intractable diseased tissue in the maxillary sinus after endoscopic sinus surgery with high-pressure water jet and preservation of the periosteum. Arch. Otolaryngol. Head Neck Surg.126, 55–61. https://doi.org/10.1001/archotol.126.1.55 (2000).
Bassiouni, A., Naidoo, Y., Wormald, P. J. & When FESS fails: The inflammatory load hypothesis in refractory chronic rhinosinusitis. Laryngoscope122, 460–466. https://doi.org/10.1002/lary.22461 (2012).
King, J. M., Caldarelli, D. D. & Pigato, J. B. A review of revision functional endoscopic sinus surgery. Laryngoscope104, 404–408. https://doi.org/10.1288/00005537-199404000-00002 (1994).
Costa, F. et al. Surgical treatment of aspergillus mycetomas of the maxillary sinus: review of the literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod103, e23–29. https://doi.org/10.1016/j.tripleo.2006.12.015 (2007).
Felisati, G. et al. Sinonasal complications resulting from dental treatment: Outcome-oriented proposal of classification and surgical protocol. Am. J. Rhinol Allergy27, e101–106. https://doi.org/10.2500/ajra.2013.27.3936 (2013).
Cho, D. Y. & Hwang, P. H. Results of endoscopic maxillary mega-antrostomy in recalcitrant maxillary sinusitis. Am. J. Rhinol. 22, 658–662. https://doi.org/10.2500/ajr.2008.22.3248 (2008).
Abd el-Fattah, H., Nour, Y. A. & el-Daly, A. Endoscopic radical antrectomy: A permanent replacement for the Caldwell-Luc operation. J. Laryngol. Otol.122, 268–276. https://doi.org/10.1017/S0022215107006718 (2008).
DeFreitas, J. & Lucente, F. E. The Caldwell-luc procedure: Institutional review of 670 cases: 1975–1985. Laryngoscope98, 1297–1300. https://doi.org/10.1288/00005537-198812000-00004 (1988).
Xu, G. Z., Yang, C., Fan, X. D., Hu, Y. K. & Yu, C. Q. Functional surgery for the treatment of dentigerous cyst in the maxillary sinus. J. Craniofac. Surg.26, e84–86. https://doi.org/10.1097/SCS.0000000000001287 (2015).
Han, J. J. et al. Schneiderian membrane regeneration after lateral bony window repositioning in modified endoscopic-assisted maxillary sinus surgery: transmission electron microscopy evaluation. J. Craniofac. Surg.33, e701–e706. https://doi.org/10.1097/SCS.0000000000008603 (2022).
Kim, D., Kim, Y. & Han, J. J. Removal of calcium hydroxide paste leaked into the maxillary sinus. Ear Nose Throat J.1455613231191378. https://doi.org/10.1177/01455613231191378 (2023).
Costa, F., Emanuelli, E., Franz, L., Tel, A. & Robiony, M. Single-step surgical treatment of odontogenic maxillary sinusitis: A retrospective study of 98 cases. J. Craniomaxillofac. Surg.47, 1249–1254. https://doi.org/10.1016/j.jcms.2019.04.012 (2019).
Koc, O. & Tuz, H. H. Effect of maxillary surgical movement on nasal cavity and maxillary sinus dimensions and function after Le Fort I osteotomy. Int. J. Oral Maxillofac. Surg.51, 806–812. https://doi.org/10.1016/j.ijom.2021.10.006 (2022).
Chobillon, M. A. & Jankowski, R. What are the advantages of the endoscopic canine fossa approach in treating maxillary sinus aspergillomas? Rhinology42, 230–235 (2004).
Snidvongs, K., Sacks, R. & Harvey, R. J. Osteitis in Chronic rhinosinusitis. Curr. Allergy Asthma Rep.19. https://doi.org/10.1007/s11882-019-0855-5 (2019).
Murray, J. P. Complications after treatment of chronic maxillary sinus disease with Caldwell-luc procedure. Laryngoscope93, 282–284 (1983).
Choi, B. H., Yoo, J. H. & Sung, K. J. Radiographic comparison of osseous healing after maxillary sinusotomy performed with and without a periosteal pedicle. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod82, 375–378. https://doi.org/10.1016/s1079-2104(96)80300-3 (1996).
Scolozzi, P., Martinez, A., Lombardi, T. & Jaques, B. Lateral antrotomy as a surgical approach for maxillary sinus: A modified technique with free bone flap repositioning and fixation with a titanium plate. J. Oral Maxillofac. Surg.67, 689–692. https://doi.org/10.1016/j.joms.2008.09.016 (2009).
Biglioli, F. & Goisis, M. Access to the maxillary sinus using a bone flap on a mucosal pedicle: Preliminary report. J. Craniomaxillofac. Surg.30, 255–259. https://doi.org/10.1054/jcms.2002.0279 (2002).
Abello, P. Functional surgery of the maxillary sinus. Revue De Laryngol.-Otol.-Rhinol.79, 747–750 (1958).
Yoshida, H. et al. Relationship between infected tooth extraction and improvement of odontogenic maxillary sinusitis. Laryngoscope Investig. Otolaryngol.7, 335–341. https://doi.org/10.1002/lio2.765 (2022).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1C1C1014734).
Author information
Authors and Affiliations
Contributions
S.G.C. collected the data and wrote the main manuscript text. S.G.C. and J.J.H. analyzed the data. W.L. contributed to the analysis of the results and prepared figures. J.J.H. designed and finalized the whole manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Choi, S.G., Lee, WU. & Han, J.J. Treatment outcome of modified endoscopic assisted sinus surgery for treating maxillary sinus diseases with three dimensional volumetric analysis. Sci Rep 14, 21620 (2024). https://doi.org/10.1038/s41598-024-72840-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72840-y
- Springer Nature Limited