Abstract
Objectives
We investigated and compared the errors generated by multislice computed tomography (MSCT), cone-beam computed tomography (CBCT), and digital dental casts when used to provide digital data about dental structures.
Methods
Ten A20 skull models were scanned with MSCT and CBCT, and dental plaster cast models were optically scanned in three dimensions. The maxillary dental area was then compared. The distance between the three-dimensional scan data of the skull and each set of digital dental data were measured. Reference data were then overlapped with the experimental digital model using surface-based registration. The distance of errors was measured with the shortest distance measurement function. The distances between each experimental digital model and the reference scan data were measured, and error values were determined for all maxillary teeth and each tooth surface area. Errors were measured for all teeth from the central incisors to the second molar on both the left and right sides. Errors were measured from the mesial, distal, and labial surfaces and the tooth cusp tip area for each tooth.
Results
The digital dental casts had the smallest error (p < 0.001). The error in the digital dental casts (mean ± standard deviation) was 0.10 ± 0.12 mm. The CBCT error was 0.34 ± 0.38 mm, which was significantly greater than the MSCT error (0.19 ± 0.16 mm) (p < 0.001).
Conclusions
We recommend the use of digital dental casts with digital dental imaging for three-dimensional measurement of the dental area because this technique had the smallest errors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Analog measurement techniques have become relics of the past in dentistry. Digital dental models are replacing plaster cast models, and treatment modalities are adopting digital technologies such as computer-aided design and computer-aided manufacturing [1, 2].
There are two main types of digital dental imaging data: computed tomography (CT) scan data and optical scan data for dental models or natural teeth. CT scans generate three-dimensional (3D) images of the craniofacial area and provide data regarding inner anatomical structures. The drawbacks of CT scans are radiation and metallic artifacts, which may be present in images because of amalgam plugs, dental prostheses, and orthodontic brackets and which may undermine the accuracy of imaging data [3]. Cone-beam CT (CBCT) scans have recently become widely used for dental images because of their low radiation dosage requirements, increased accessibility, and relatively low cost [4]. However, CBCT scans have a narrow field of view (FOV) and may be prone to larger errors than multislice CT (MSCT) scans [5, 6]. Dental impression models are being replaced by digital models, which are easy to use and manipulate via computers and optical scan devices [7, 8]. Although optical scans have the advantage of not requiring radiation, they cannot be used to visualize internal structures or regions with insufficient direct light.
Digital dental data can be used for a wide range of purposes in dental clinics, including orthognathic surgeries, orthodontics, restoration of teeth, and prostheses. In orthognathic surgery, digital dental data are required to establish a diagnosis, formulate surgical plans, manufacture CAD/CAM-based surgical devices, and assist with navigation during surgery. In orthodontics, digital dental data are useful not only when establishing the diagnosis and treatment plans, but also when saving and evaluating data regarding treatment outcomes; moreover, they can be used in place of plaster dental cast models. Digital dental data can also be used for dental restorations and prostheses when CAD/CAM restorative prosthetics are used. Moreover, they are useful in a wide range of other dental fields not mentioned above. Therefore, it is imperative that digital dental data be compared with data from other techniques. Some previous studies have compared MSCT with CBCT [9] or CT data with digital dental models [10], and others have compared dental plaster models with digital dental models for measurements [11]. However, researchers have rarely compared all three modalities (MSCT, CBCT, and digital dental models) within the same study.
In the present study, we compared the errors generated by MSCT and CBCT imaging and digital dental casts when these techniques are used to provide digital data for dental structures.
Materials and methods
Skull models
We used 10 A20 skull models (3B Scientific, Hamburg, Germany) (Fig. 1a). The craniomaxillary region of the skull models was scanned with MSCT and CBCT, and dental plaster cast models were optically scanned in three dimensions. We then compared the digital dental data acquired by the three types of scans.
Digital modeling with MSCT
MSCT scanning was performed with the Siemens Sensation 64 (Siemens Medical Solutions, Malvern, PA, USA) with a 0.4375-mm pixel size, 22.40-cm FOV, and 0.6-mm slice thickness. The MSCT settings were as follows: 120 kVp [peak], 137.5 mA, and a filter function algorithm of H60f. CT scanning of the experimental model was performed under these settings.
Digital Imaging and Communications in Medicine (DICOM) files were opened in Mimics version 14.0 (Materialise, Leuven, Belgium). This program converts DICOM files to stereolithography (STL) file formats. CT DICOM data were converted to STL files under the following settings: threshold values to construct 3D images of the CT data were set at 226–3071 Hounsfield units (these were the threshold values previously set for bones in the Mimics program). The 3D structure quality was set to the optimal 3D calculation in the Mimics program.
Digital modeling of CBCT
We first scanned the 10 skull models by CBCT with Implagraphy (VATECH Co. Ltd., Hwaseong, Korea). The settings were as follows: 12.0- × 8.5-cm FOV, 85 kVp [peak], 7.0 mA, 24-s maximum scanning time, and 0.202-mm voxel size. Each DICOM file was then opened in Mimics (Materialise). DICOM data for CBCT were converted to STL files by the same process used to convert MSCT DICOM files.
Digital dental casts
Dental impressions of each of the 10 maxillary models were taken using alginate (Alginoplast; Heraeus, Hanau, Germany). We then constructed maxillary dental cast models by casting the impression mold with dental plaster (Mutsumi Chemical Industries Co. Ltd., Yokkaichi, Japan). We created a 3D scan of each of the dental cast models with a non-contact 3D optical scanner (Rexcan DS2; Solutionix, Seoul, Republic of Korea) and acquired the digital dental cast as STL format data.
3D Light scan data of skull model as reference for measurements
Each of the 10 A20 skull models was three-dimensionally scanned with smartSCAN (AICON 3D Systems GmbH, Braunschweig, Germany), a non-contact optical scanner (Fig. 1b). The camera resolution was set to 1.3 megapixels, and accuracy was set to ±15 µm. Each file was saved in STL format. Computer interface was IEEE 1394B (FireWire®B)/GigE, and principle of operation was the miniaturized projection technique. The smallest and largest FOVs were 30 and 1500 mm, respectively, in the sensor of the device. The minimum acquisition time of the sensor was 1 s, and the light source was a white light-emitting diode. Two professional high-resolution digital charge-coupled device cameras were used. The 3D measurement system of AICON 3D Systems GmbH was certified as ISO 9001:2008.
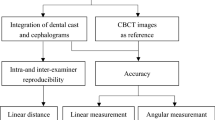
Image overlap between reference data and experimental data for error measurement
We overlapped each of the three different 3D experimental scan files (STL) for the skull models with optical scan images of the skull models as reference data using the Rapidform XOV2 program (INUS Technology, Seoul, Korea). A surface-based best-fit algorithm was used to overlap the data. The procedures were as follows: First, we overlapped the 3D scan (STL) files with reference data for the skull models for each experimental datum using paired-point registration. Three anatomical paired points were used to overlap the images. Next, to minimize any potential errors, the 3D scan (STL) files and the experimental data were overlapped based on whole-surface data from the dental and maxillary portions of the skull models using surface-based registration.
Error measurement and analysis
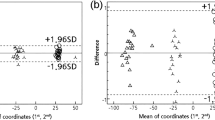
We used XOV/verifier SP2, a Rapidform program with a heightened error-inspection function, to measure the distance between the 3D scan data and each set of digital dental data (i.e., MSCT, CBCT, and digital dental cast) (Fig. 2 XOV Reference data were overlapped with the experimental digital model using surface-based registration. The distance of the error was measured using the shortest distance measurement function in the program with the 3D distance measurement tool in the software. We used the iterative closest-point algorithm to overlap the surface-based images. The errors between the overlapped experimental data and reference baseline data were measured using the 3D Euclidean distances at the error measurement points. The t algorithm to o function in the XOV2 Rapidform software was used for error measurement.
The distances between each experimental digital model and the reference scan data were measured, and error values were determined for all maxillary teeth and each tooth surface area. Errors were measured for all teeth from the central incisors to the second molar on both the left and right sides in each of the 10 models. Errors were measured from the mesial, distal, and labial surfaces and the tooth cusp tip area for each tooth. Errors were measured in each area five times, and absolute error values were measured for each scanning method. Errors in each measurement of the surface area and tooth area were compared, and the significance of the errors was verified by analysis of variance in IBM SPSS Statistics 21 (IBM Corp., Armonk, NY, USA).
The error between the baseline model and experimental data is indicated on a color-coded scale; a negative value indicates that the experimental data are smaller than the baseline data, and a positive value indicates that the experimental data are greater than the baseline data. Green represents an error between −0.1 mm and +0.1 mm. The blue darkens as the error nears −1 mm, and the red darkens as the error nears +1 mm (Figs. 2, 3, 4).
Results
The digital dental casts had the lowest error (p < 0.001). The error for digital dental casts (mean ± standard deviation) was 0.10 ± 0.12 mm, which was significantly lower than that for MSCT (0.19 ± 0.16 mm) (p < 0.001). The error for CBCT was 0.34 ± 0.38 mm, which was significantly greater than that for MSCT (0.19 ± 0.16 mm) (p < 0.001).
The digital dental casts also had the smallest errors measured from each of the four surfaces of the teeth (p < 0.001), with mean errors ranging from 0.08 to 0.12 mm. MSCT had a large error value at the tooth tip (mean 0.36 mm), with mean errors in other regions ranging from 0.11 to 0.16 mm (Table 1). Mean errors in CBCT ranged from 0.28 to 0.38 mm. There was no significant difference in mean errors at the tooth tip between MSCT and CBCT (0.36 and 0.38 mm, respectively; p = 0.269). Similarly, there was no significant difference in mean errors in the distal areas between MSCT and digital dental casts (0.11 and 0.12 mm, respectively; p = 0.834). Both MSCT and CBCT yielded large errors at the tooth tip but small errors in the distal area when the four surfaces of the tooth were compared. By contrast, digital casts had large errors in the distal area (Table 2).
In terms of errors associated with each tooth, digital dental casts had the smallest errors and CBCT had the largest errors (p < 0.001) (Table 3). For all teeth, the order of error size from smallest to largest was digital dental casts, MSCT, and CBCT (Table 4). The mean errors in the digital dental cast for each tooth ranged from 0.08 to 0.12 mm and were similar to the error sizes at the tooth surfaces. For MSCT, the mean errors from the second molar to the central incisors ranged from 0.16 to 0.22 mm. The mean errors for CBCT at the same areas ranged from 0.23 to 0.46 mm. CBCT yielded errors of 0.45, 0.39, and 0.46 mm at the central incisor, lateral incisor, and canine areas, respectively. For MSCT, the mean errors from the first premolar to the second molar ranged from 0.16 to 0.19 mm, while those from the central incisor to the canine ranged from 0.20 to 0.22 mm. For CBCT, the mean errors from the first premolar to the second molar area ranged from 0.23 to 0.32 mm, and those from the central incisors to the canine area ranged from 0.39 to 0.46 mm. For both MSCT and CBCT, there were larger errors in the anterior than posterior teeth area; however, the error trend was the opposite for digital casts, where the mean errors from the first premolar to the second molar area ranged from 0.10 to 0.12 mm and the mean error from the central incisors to the canine area was 0.08 mm.
Discussion
Digital dental casts had the smallest errors overall, and CBCT had the largest errors in the dental area. The differences in errors among digital dental casts, MSCT, and CBCT were statistically significant.
In the teeth area, there were large errors at the tooth tip associated with MSCT (mean 0.36 mm) and CBCT (mean 0.38 mm), but the difference in the errors between the two methods was not significant (p = 0.269). The mean error at the tooth tip for the digital dental casts was 0.09 mm; there was ~0.3 mm of difference in the mean errors between MSCT and CBCT compared with the digital dental casts. The difference for MSCT may have been induced by the slice thickness during MSCT scanning. For CBCT, the mean errors were ~0.3 mm overall; the mean errors in the four surfaces of the teeth ranged from 0.28 to 0.38 mm. This difference in CBCT may have resulted from the voxel size of the CT device [12]. Higher resolution with a smaller voxel size (0.202 mm) than that used in this study may yield more accurate dental measurements.
For MSCT, the mean errors from the central incisors to the canines ranged from 0.20 to 0.22 mm. The mean errors in the same region for CBCT ranged from 0.39 to 0.46 mm. For CBCT, there were larger errors in the anterior tooth than in the posterior tooth area, ranging from 0.23 to 0.32 mm. This may be due to the fact that the anterior tooth area has narrower mesial and distal areas and a smaller incisal edge area. In addition, longer distances between the cone beam source and the tooth area (e.g., molars and incisors) may have resulted in larger errors [13]. Conversely, there were similar mean errors in the posterior tooth area (~0.1 mm) than in the anterior tooth area (0.08 mm) in the digital dental casts. However, the errors yielded by the dental casts might have been the result of errors made during the dental impression and plaster cast-making processes.
Recent advances in and the wide availability of CT have allowed dentists to construct 3D images of the maxillofacial region, permitting more accurate measurement of structures in this region. In addition to dental measurements, imaging technologies have enabled the development of more methods of 3D analysis of dental structures based on various reference planes and points compared with traditional analog measurements of dental casts [14].
Previous studies that compared CBCT with digital dental casts and facial casts based on linear measurement references found that digital dental casts and facial plaster casts were more accurate than CBCT [15, 16]. The results of the present study are in line with these previous studies; we also found that digital dental casts had the smallest error.
The process of analyzing digital images on a computer can be affected by a number of error types [17]. For example, there may be errors in the measurement techniques used by the hardware or software of CT equipment. Moreover, image errors may result from the settings used for imaging and software, such as the matrix size, slice thickness, and voxel size. A previous study compared CT images of the mandible when CBCT was used and reported that the settings of CBCT could be adjusted to a lower kVp and mA when the error in the cross-sectional images was not significant under the following CBCT settings: 60, 80, 100, and 120 kvP, and 10 and 15 mA [18]. The CBCT equipment used in the present study was set from 50 to 90 kVP and 4 to 10 mA. Furthermore, we presume that the image impression of the experimental model in this study can be taken under these settings because it was a simple manufactured skull model. However, although this study set the CBCT at 85 kvP and 7 mA for CT scanning of the experimental model, these settings may provide insufficient evidence. Additional studies on other optimum CBCT settings using actual human cranial bones or soft tissues are required, and future studies should proceed based on these optimum CBCT settings.
We acquired CT images by MSCT in this study. In MSCT, there are correlations among accuracy, slice thickness, and voxel size [19]. Compared with MSCT, CBCT has a relatively small scan FOV that ranges from 15 to 20 cm, and it is deemed most accurate in the middle of the image in the scan field [20]. Because of its small radiation dosage, CBCT is becoming increasingly popular in the dental field, and it is frequently used to generate maxillofacial images [4]. Although CBCT is limited in terms of the regions it can scan, it is highly efficient for scanning the jaw region, although this depends upon the anatomical size and accessibility of the jaw. More studies of CBCT in dentistry are underway. Although its accuracy is acceptable, it may not be as good as that of MSCT [5, 6, 9, 21]. Nevertheless, CBCT is often preferred over MSCT because of its low radiation dosage and high-quality images [22]. It should be noted that in the present study, larger errors were associated with CBCT than with MSCT. This study used only one type of equipment to perform CBCT and MSCT. Future studies should conduct experiments with various types of CT equipment.
We believe that the data acquired via 3D optical scanning of the jaw would have some degree of error in terms of the actual size of the jaw model. It is difficult to use contact scanners on sizable and complex anatomical structures, such as the skull, and non-contact scanners may induce errors that are insignificantly different from those induced by contact scanners [23].
Importantly, the measurement method for reference must be more accurate than that used in the experimental measurement groups. The present study used the non-contact 3D optical scanning method for reference measurement. It is easier to acquire data with a non-contact 3D optical scanner, but the scanner has limitations in capturing data from anatomical structures with blind spots not reached by light. CT images can provide skull data, including information on the internal structures, but errors may be induced by the equipment, CT settings, and image slice thickness. In a comparative study of the accuracy of MSCT and CBCT at the dental implant site, the overall mean of the absolute error of MSCT and CBCT was 0.75 and 0.49 mm, respectively [24]. These CT device errors may differ by the CT equipment used, the environmental image-taking settings, and the imaging software. In the present study, the camera resolution was set to 1.3 megapixels, and the accuracy was set to ±15 µm in the optical scanner for reference measurement. Although the above-mentioned study [24] could not completely show the error of MSCT and CBCT for dental measurement, the data obtained from optical scanning in the present study can be regarded as reference data in the point of accuracy.
Each image datum of the 3D light-scans was automatically combined in the software using the least-squares registration function. There may be another error in this process. Although light-scans as reference data may have a little error in the scanning process and scanner equipment itself, they can be considered a research method tool. Previous reports using light-scans as reference data showed the determination between experimental imaging and reference data in each study [25–27]. Furthermore, the present study compared the acquisition of surface information for dental measurements. The 3D optical scanning data act as a baseline with which to compare the experimental results, rather than an accurate representation of the size of the jaw. We believe that a study method will be developed in the future to measure the absolute size of the jaw and teeth as the gold standard reference data from which additional dentomaxillofacial errors can be measured.
One of the drawbacks associated with using CT in dentistry is that the images may have metallic artifacts that can cloud interpretation of the images. Dental CT images may need to be substituted with other accurate digital dental data because they are distorted by the presence of metal artifacts and thus cannot accurately display the occlusal conditions of the jaw to the extent required for treating dentofacial deformity [25]. Digital jaw images that convey dental and occlusal information have enabled simulation surgeries that allow surgeons to predict the displacement of neighboring bone fragments and to manufacture surgical guides and devices [28]. For CT images, however, prosthodontics or orthodontic brackets in the dental region may result in metallic artifacts and distort the images. In such cases, therefore, alternative dental images may be required for a more accurate representation of the occlusal and dental conditions of patients [26].
We used a 3D optical scanner designed for plaster models to scan the dental plaster models in this study. It is impossible to optically scan a jaw model with the same equipment. A scanner used to scan a jaw model can also be used to three-dimensionally scan a plaster model; however, it is easier to conduct the experiment and acquire data using a dental scanner that automatically overlaps data collected from each direction. In addition, dental plaster model scanners are used in the clinical setting. Therefore, the present study used different scanners to scan the dental plaster model and the skull model. Various 3D light-scanning methods are used to scan dental cast models or impression materials or even the natural teeth using an intraoral scanner. Use of dental impression materials may be easier than use of a direct chairside intraoral scanner [29]. Further research on intraoral dental scanners is needed for verification. However, although optical scans have an advantage in that they do not require radiation, a downside is that they cannot visualize internal structures and regions without sufficient direct light.
This study has some limitations that should be noted. First, fresh cadavers are the ideal model with which to investigate CT or 3D optical scanning to measure errors in human studies. We used manufactured craniofacial models instead of fresh cadavers or dry skulls for this study because the use of fresh cadavers can lead to errors due to anatomical dental or bone defects and prosthodontics. In future studies, it will be necessary for researchers to use intact real human skulls with whole teeth or experimental materials similar to those of the human body to confirm the reliability of our results. Second, when converting CT image data to the STL file format, the results may be affected by the 3D reconstruction and converting algorithms used by each type of software [27]. In this study, we used only one type of software to convert DICOM data to STL files under identical conditions. Therefore, we assume that there were no significant differences in processing among the converted images. However, it should be noted that errors can occur during the conversion process from the DICOM to STL file format. Third, for measurements of error, experimental data must be compared with reference data. In the present study, we overlapped each experimental digital data point with reference data using a surface-based registration method for this task. For the registration procedure, voxel-based registration can also be used.
In conclusion, among the different types of digital technologies used to image dental areas, digital dental casts had the smallest errors. MSCT had smaller errors than CBCT. The present study showed an ~0.3-mm overall mean error associated with CBCT. In addition, there may be larger errors in the anterior than posterior tooth area in CBCT images. We recommend the use of digital dental casts for 3D measurement with digital dental imaging.
References
Marchack CB. CAD/CAM-guided implant surgery and fabrication of an immediately loaded prosthesis for a partially edentulous patient. J Prosthet Dent. 2007;97:389–94.
Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J. 2009;28(1):44–56.
Nkenke E, Zachow S, Benz M, Maier T, Veit K, Kramer M, et al. Fusion of computed tomography data and optical 3D images of the dentition for streak artefact correction in the simulation of orthognathic surgery. Dentomaxillofac Radiol. 2004;33(4):226–32.
Kau CH, Bozic M, English J, Lee R, Bussa H, Ellis RK. Cone-beam computed tomography of the maxillofacial region–an update. Int J Med Robot. 2009;5(4):366–80.
Liang X, Lambrichts I, Sun Y, Denis K, Hassan B, Li L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT). Part II: on 3D model accuracy. Eur J Radiol. 2010;75(2):270–4.
Mischkowski RA, Pulsfort R, Ritter L, Neugebauer J, Brochhagen HG, Keeve E, et al. Geometric accuracy of a newly developed cone-beam device for maxillofacial imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(4):551–9.
Jedlinska A. The comparison analysis of the line measurements between plaster and virtual orthodontic 3D models. Ann Acad Med Stetin. 2008;54(2):106–13.
DeLong R, Heinzen M, Hodges JS, Ko CC, Douglas WH. Accuracy of a system for creating 3D computer models of dental arches. J Dent Res. 2003;82(6):438–42.
Dillenseger JP, Matern JF, Gros CI, Bornert F, Goetz C, Le Minor JM, et al. MSCT versus CBCT: evaluation of high-resolution acquisition modes for dento-maxillary and skull-base imaging. Eur Radiol. 2015;25(2):505–15.
Tarazona B, Llamas JM, Cibrian R, Gandia JL, Paredes V. A comparison between dental measurements taken from CBCT models and those taken from a digital method. Eur J Orthod. 2013;35(1):1–6.
Leifert MF, Leifert MM, Efstratiadis SS, Cangialosi TJ. Comparison of space analysis evaluations with digital models and plaster dental casts. Am J Orthod Dentofacial Orthop. 2009;136(1):16.e1–4 (discussion 16).
Patcas R, Muller L, Ullrich O, Peltomaki T. Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2012;141(1):41–50.
Parsa A, Ibrahim N, Hassan B, van der Stelt P, Wismeijer D. Influence of object location in cone beam computed tomography (NewTom 5G and 3D Accuitomo 170) on gray value measurements at an implant site. Oral Radiol. 2014;30(2):153–9.
Hernandez Y, Tarazona B, Zamora N, Cibrian R, Gandia J, Paredes V. Comparative study of reproducibility and accuracy in measuring mesiodistal tooth sizes using three different methods: 2D digital, 3D CBCT, and 3D CBCT segmented. Oral Radiol. 2015;31(3):165–72.
de Waard O, Rangel FA, Fudalej PS, Bronkhorst EM, Kuijpers-Jagtman AM, Breuning KH. Reproducibility and accuracy of linear measurements on dental models derived from cone-beam computed tomography compared with digital dental casts. Am J Orthod Dentofacial Orthop. 2014;146(3):328–36.
Xu Y, Li J, Zhao S, Shi B, Zheng Q, Wang Y. Accuracy of a plastic facial cast fabricated with a custom tray in comparison with cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(3):e238–45.
Widmann G, Stoffner R, Bale R. Errors and error management in image-guided craniomaxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(5):701–15.
Panmekiate S, Apinhasmit W, Petersson A. Effect of electric potential and current on mandibular linear measurements in cone beam CT. Dentomaxillofac Radiol. 2012;41(7):578–82.
Loubele M, Van Assche N, Carpentier K, Maes F, Jacobs R, van Steenberghe D, et al. Comparative localized linear accuracy of small-field cone-beam CT and multislice CT for alveolar bone measurements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(4):512–8.
Panzarella FK, Junqueira JL, Oliveira LB, de Araujo NS, Costa C. Accuracy assessment of the axial images obtained from cone beam computed tomography. Dentomaxillofac Radiol. 2011;40(6):369–78.
Pauwels R, Nackaerts O, Bellaiche N, Stamatakis H, Tsiklakis K, Walker A, et al. Variability of dental cone beam CT grey values for density estimations. Br J Radiol. 1021;2013(86):20120135.
Hofmann E, Schmid M, Sedlmair M, Banckwitz R, Hirschfelder U, Lell M. Comparative study of image quality and radiation dose of cone beam and low-dose multislice computed tomography–an in vitro investigation. Clin Oral Investig. 2014;18(1):301–11.
Persson A, Andersson M, Oden A, Sandborgh-Englund G. A three-dimensional evaluation of a laser scanner and a touch-probe scanner. J Prosthet Dent. 2006;95(3):194–200.
Al-Ekrish AA, Ekram M. A comparative study of the accuracy and reliability of multidetector computed tomography and cone beam computed tomography in the assessment of dental implant site dimensions. Dentomaxillofac Radiol. 2011;40(2):67–75.
Choi Y-S, Kim M-K, Lee J-W, Kang S-H. Impact of the number of registration points for replacement of three-dimensional computed tomography images in dental areas using three-dimensional light-scanned images of dental models. Oral Radiol. 2014;30(1):32–7.
Kang SH, Lee JW, Lim SH, Kim YH, Kim MK. Dental image replacement on cone beam computed tomography with three-dimensional optical scanning of a dental cast, occlusal bite, or bite tray impression. Int J Oral Maxillofac Surg. 2014;43(10):1293–301.
Kang SH, Kim MK, Kim HJ, Zhengguo P, Lee SH. Accuracy assessment of image-based surface meshing for volumetric computed tomography images in the craniofacial region. J Craniofac Surg. 2014;25(6):2051–5.
Uechi J, Okayama M, Shibata T, Muguruma T, Hayashi K, Endo K, et al. A novel method for the 3-dimensional simulation of orthognathic surgery by using a multimodal image-fusion technique. Am J Orthod Dentofacial Orthop. 2006;130(6):786–98.
Grunheid T, McCarthy SD, Larson BE. Clinical use of a direct chairside oral scanner: an assessment of accuracy, time, and patient acceptance. Am J Orthod Dentofacial Orthop. 2014;146(5):673–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sang-Hoon Kang, Yeon-Ho Kim, and Moon-Key Kim declare that they have no conflict of interest.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent was not needed in the study.
Rights and permissions
About this article
Cite this article
Kang, SH., Kim, YH. & Kim, MK. Comparison of digital dental images yielded by digital dental casts, cone-beam computed tomography, and multislice computed tomography for measurement of dental area. Oral Radiol 33, 23–31 (2017). https://doi.org/10.1007/s11282-016-0242-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-016-0242-z