Abstract
Purpose
Obesity usually induces overactive bladder (OAB) associated with detrusor overactivity, which is related to increased contractility of the detrusor smooth muscle (DSM). Small-conductance Ca2+-activated K+ (SK) channels play a constitutive role in the regulation of DSM contractility. However, the role of SK channels in the DSM changes in obesity-related OAB is still unknown. Here, we tested the hypothesis that obesity-related OAB is associated with reduced expression and activity of SK channels in DSM and that SK channels activation is a potential treatment for OAB.
Methods
Female Sprague–Dawley rats were fed a normal diet (ND) or a high-fat diet (HFD) and weighed after 12 weeks. Urodynamic studies, quantitative reverse transcription-polymerase chain reaction (qRT-PCR), and isometric tension recording were performed.
Results
Increased average body weights and urodynamically demonstrated OAB were observed in HFD rats. qRT-PCR experiments revealed a decrease in the mRNA expression level of SK channel in DSM tissue of the HFD rats. Isometric tension recordings indicated an attenuated relaxation effect of NS309 on the spontaneous phasic and electrical field stimulation-induced contractions that occurred via SK channel activation in HFD DSM strips.
Conclusions
Reduced expression and activity of SK channels in the DSM contribute to obesity-related OAB, indicating that SK channels are a potential therapeutic target for OAB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of obesity, which is defined as abnormal or excessive fat accumulation, has doubled since 1980. More than 35% of adults aged 20 years or older were overweight in 2008 [1]. Obesity is associated with an increased risk of many chronic diseases, including diabetes, cardiovascular disease, and cancer [1, 2]. In addition, data from epidemiological studies revealed that weight gain in adulthood are related to a higher prevalence of lower urinary tract symptoms (LUTS) [3,4,5].
As a common type of LUTS, overactive bladder (OAB) is characterized by urgency, with or without urgency urinary incontinence and is usually associated with urodynamically demonstrable detrusor overactivity (DO) [6, 7]. In addition, OAB has a significant effect on the mental health and quality of life of patients, and the incidence of OAB has increased. The potential etiology and contributing factors of OAB remain complex and unclear, but obesity is a well-known specific cause of OAB [3,4,5]. OAB is more likely to be observed in obese people [3, 8]. Rats with obesity induced by a high-fat diet (HFD) became overweight and exhibited non voiding contractions (NVCs) that were suggestive of DO [9, 10]. Thus, HFD-induced obesity animal models are usually used to study the pathophysiology of OAB. The inflammation that results from obesity in detrusor smooth muscle (DSM) may be an important contribution to obesity-associated LUTS, including OAB [9,10,11]. On the other hand, DO is also due to the enhanced contractility of DSM, characterized by spontaneous phasic contractions; therefore, changes in the expression and function of DSM regulatory proteins may cause a difference in DSM contractility [12,13,14].
Ca2+-activated K+ channels play very important roles in the regulation of contractility by means of controlling the membrane potential and the repolarization, and after hyperpolarization phases of the action potential in DSM cells [15,16,17,18]. Small-conductance Ca2+-activated K+ (SK) channels and intermediate-conductance Ca2+-activated K+ (IK) channels, which are two members of Ca2+-activated K+ channel family, have similar electrophysiological characteristics and are classified as Ca2+-activated but voltage-insensitive channels [18]. SK channels, which are typically represented by three subtypes (SK1, SK2, and SK3), are activated only by increased intracellular Ca2+, and these channels have a regulatory effect on the membrane potential and thus are important factors for controlling the contractility of smooth muscle, including DSM [13, 14, 19,20,21,22,23,24,25,26,27]. However, IK channels, whose expression has been shown in the DSM, have no significant effect on the regulation of DSM contractility [19, 20, 22,23,24, 27, 28].
The pharmacological activation of SK channels induced a marked hyperpolarization effect on DSM cell membrane potential followed by significant relaxation of the DSM [22, 23, 27]. In addition, the selective SK channel inhibitor apamin caused a dramatic increase in the amplitude of spontaneous contractions in rodent and human DSM [22,23,24, 27, 29,30,31,32,33,34,35]. Furthermore, SK3 channel-overexpressing DSM cells showed enhanced whole cell currents, and the regulatory effect of apamin was attenuated in SK2 knockout mice [32, 36]. Our previous studies revealed that the decreased expression and activity of SK channels were tightly associated with OAB in a partial bladder outlet obstruction (PBOO) animal model [13, 14]. Recently, it was revealed that obesity induced alteration of atrial electrical activities and changed the activities of IK and SK channels [37]. However, the changes in the regulatory effect of SK/IK channels on DSM contractility in obesity-induced OAB remain unknown.
In the present study, a rat model of obesity induced by a HFD was used to further investigate the molecular and functional changes in SK/IK channels that occur in the DSM under these conditions using cystometry, quantitative reverse transcription-polymerase chain reaction (qRT-PCR), and isometric tension recordings. A selective SK/IK channel opener, 6,7-dichloro-1H-indole-2,3-dione3-oxime (NS309), and SK and IK channel inhibitors (apamin and TRAM-34, respectively) were applied in this study. We demonstrate that attenuated SK/IK channel expression and activity contributes to obesity-associated OAB.
Materials and methods
Animals
A total of 70 adult female Sprague–Dawley (SD) rats (China Medical University) with an average weight of 207.8 ± 9.4 g were used in this study. For 12 weeks, the study animals were housed three per cage with a 12-h light–dark cycle and fed either a normal diet (ND) (fat: 5%; protein: 20%; and carbohydrate: 75%) or a HFD (fat: 30%; protein: 14%; and carbohydrate: 56%) that induces obesity as previously described [9, 11]. All rats were weighed at 12 weeks, and urodynamic studies were conducted in ten rats from each group. The study animals were then sacrificed in a carbon dioxide tank prior to the collection of bladder specimens. All experimental procedures were approved by the Institutional Animal Care and Use Committee of China Medical University.
Cystometry
General anesthesia was induced by 5% isoflurane/O2 gas inspiration using a facial mask. A catheter was inserted into the bladder dome after surgically exposing the bladder and connected to a physiological pressure transducer and an injection pump (Dantec Menuet, Denmark). Cystometry was performed by infusing warm saline (37–38 °C) into the bladder at a rate of 12 ml/h. Three voiding events were recorded for each rat to assess the following parameters: maximum voiding pressure (the maximum pressure during voiding), bladder capacity (the volume of saline infused to induce voiding), voiding volume (the micturition volume), voiding interval (the interval between voids), and the number of NVCs during one voiding event. NVCs were defined as spontaneous contractions (> 4 cm H2O from the baseline bladder pressure) that did not result in a void. Bladders that were assessed by cystometry were not used in other experiments.
DSM tissue collection
The rats were euthanized by CO2 inhalation followed by thoracotomy. The urinary bladders were rapidly removed and preserved in cold dissection solution. The urinary bladders were cut open longitudinally, and the mucosa was removed. DSM strips (5–7 mm long and 2–3 mm wide) from the urinary bladder dome were collected.
qRT-PCR
Total RNA was isolated using TRIzol reagent (Invitrogen, Waltham, MA, USA) from mucosa-free rat DSM strips. Reverse transcription of total RNA was performed using the SuperScript™ First-Strand Synthesis System (Invitrogen, Waltham, MA, USA) according to the manufacturer’s instructions. Real-time PCR was then performed using the synthesized cDNA on an ABI PRISM 7500 sequence detection system with the SYBR GREEN PCR Master Mix [38]. Real-time PCR was carried out to analyze the mRNA expression of the SK1, SK2, SK3, IK channels, and β-actin using specific primers (Table 1). The PCR conditions were 94 °C for 1 min followed by 35 cycles of 95 °C for 30 s and 58 °C for 40 s [9, 13, 14, 39]. All of the reactions were run three times and normalized to β-actin. All qRT-PCR products from intact whole DSM tissues and isolated DSM cells were purified using the GenElute PCR Clean-Up Kit (Sigma-Aldrich, St. Louis, MO, USA), and the sequences of the detected genes were confirmed by direct sequencing of the amplified PCR products [40].
Isometric DSM tension recordings
Isometric DSM contraction recordings were made as previously described [13, 41, 42]. Isolated DSM strips were secured to isometric force–displacement transducers and placed in physiological saline solution aerated with 95% O2/5% CO2 (pH 7.4) at 37 °C. The DSM strips were initially tensioned (10 mN) during an equilibration period of 45–60 min. To minimize the effect of neurotransmitters released from neurons on the DSM, 1 µM tetrodotoxin (TTX), a selective inhibitor of neuronal voltage-gated Na+ channels, was present during the spontaneous phasic contraction recordings.
In another experimental series, nerve-evoked contractions were induced by electrical field stimulation (EFS) using a pair of platinum electrodes mounted in the tissue bath parallel to the DSM strip in the absence of TTX. The EFS pulses were generated using a PHM-152I stimulator (MED Associates, St. Albans, VT, USA). The EFS pulse parameters were as follows: 0.75 ms pulse width, 20 V pulse amplitude, 3 s stimulus duration, and reversal of the polarity at alternating pulses. After the equilibration period, the DSM strips were subjected to continuous repetitive EFS with increasing frequencies from 0.5 to 50 Hz at 3 min intervals. The contractions were recorded using a MyoMED myograph system (MED Associates, St. Albans, VT, USA).
Solutions and drugs
The dissection solution contained the following components: 80 mM monosodium glutamate, 55 mM NaCl, 6 mM KCl, 10 mM glucose, 10 mM HEPES, and 2 mM MgCl2; the pH was adjusted to 7.3 with NaOH. The physiological saline solution was freshly prepared daily and contained the following components: 119 mM NaCl, 4.7 mM KCl, 24 mM NaHCO3, 1.2 mM KH2PO4, 2.5 mM CaCl2, 1.2 mM MgSO4, and 11 mM glucose; the solution was aerated with 95% O2/5% CO2 to obtain a pH of 7.4. NS309 was purchased from Sigma-Aldrich (St. Louis, MO, USA). NS309 was dissolved in DMSO, while all other chemicals were dissolved in double-distilled water. The maximum DMSO concentration in the bath solution did not exceed 0.1%.
Data analysis and statistics
Relative differences in the PCR results were calculated by using the comparative Ctmethod (\({2^{ - \Delta \Delta {C_{\text{t}}}}}\)) after determining the Ct values for the reference (β-actin) and target (SK1, SK2, SK3, or IK) genes in each sample [9, 13, 14]. The relative mRNA expression level of the target gene was calculated after normalization to β-actin expression. MiniAnalysis software (Synaptosoft, Decatur, GA, USA) was used to analyze five DSM contraction parameters including contraction amplitude, muscle integral force (the area under the curve of the phasic contractions), duration (defined as the width of the contraction at 50% of the amplitude), frequency (contractions per minute), and tone (phasic contractions in the baseline curve). For the analysis of the compound effects, one 5-min-long stable recording made prior to the application of the compounds was analyzed for the control, and another 5-min-long stable recording was analyzed after the application of each concentration of the compounds. For spontaneous phasic contractions, every parameter under control conditions was taken to be 100%, and the data were normalized. The contraction amplitude at every EFS frequency was normalized to the amplitude at an EFS frequency of 50 Hz under control conditions (taken to be 100%) and expressed as a percentage of the EFS-induced contraction. Data were further analyzed with GraphPad Prism 5.0 software (GraphPad Software, San Diego, CA, USA). Data are expressed as the mean ± SEM; n = the number of strips or cells, and N = the number of rats. Statistical significance was tested using one-way ANOVA, followed by Dunnett’s multiple comparison test, a t test, or a paired Student’s t test, and P < 0.05 was considered statistically significant.
Results
Obesity induced by a HFD
There was no statistically significant difference in body weight between the two groups before feeding (HFD 201.2 ± 6.9 g, N = 40; ND 206.9 ± 8.1 g, N = 30; P > 0.05). The average body weight of the HFD rats was significantly increased after 12 weeks (HFD 646.1 ± 11.3 g, N = 40; ND 349.8 ± 9.7 g, N = 30; P < 0.05). However, the bladder weight of the HFD rats (91.9 ± 5.2 mg, N = 40) did not differ significantly from that of the ND animals (93.6 ± 3.7 mg, N = 30; P > 0.05) after the HFD treatment.
OAB was induced by HFD treatment
Twelve weeks after HFD feeding, the bladder capacity was significantly reduced compared to that of ND rats (HFD 0.34 ± 0.08 ml, N = 10; ND 0.68 ± 0.06 ml, N = 10; P < 0.05; Fig. 1a, b), with a notably decreased voiding volume (0.33 ± 0.09 ml in HFD, N = 10; 0.67 ± 0.07 ml in ND, N = 10; P < 0.05; Fig. 1a, c). The maximum voiding pressure did not differ significantly between the rats of two groups (ND 42.5 ± 6.7 cm H2O, N = 10; HFD 43.1 ± 7.6 cm H2O, N = 10; P > 0.05; Fig. 1a, d). In addition, the HFD rats had a shorter voiding interval (HFD 1.9 ± 0.5 min, N = 10; ND 3.9 ± 0.4 min, N = 10; P < 0.05; Fig. 1a, e) and a significantly increased frequency of NVCs (HFD 3.6 ± 0.8, N = 10; ND 0.47 ± 0.3, N = 10; P < 0.05; Fig. 1a, f) compared to those in the ND rats, indicating that OAB had been induced.
OAB was induced by HFD-treatment. Representative urodynamic recording trace showing the changes in bladder function in HFD rats (a). Reduced bladder capacity (b), decreased voiding volume (c), shorter voiding intervals (e), and more frequent NVCs (f) were observed in rats in the HFD group compared with those in the ND group (N = 10 in each; P < 0.05). However, there was no significant difference in maximum voiding pressure (d) between the two groups (P > 0.05). *P < 0.05 for ND versus HFD; NS nonsignificant
Decreased mRNA expression levels of the SK channels were detected in the DSM of HFD rats
Our results established that the genes for the SK1, SK2, and SK3 channels were significantly decreased in the DSM from HFD rats compared to the levels in ND animals (Fig. 2a–c). HFD treatment significantly reduced the relative mRNA expression of the SK1–SK3 channel to 60.7 ± 0.2, 62.7 ± 0.2, and 26.1 ± 0.1% (n = 16, N = 5), respectively, compared to the values observed in ND rats (n = 16, N = 5; P < 0.05; Fig. 2a–c). However, there was no significant difference in the mRNA expression level of IK channels (1.22-fold decrease, HFD vs. ND; P > 0.05; Fig. 3d) in the rat DSM between the two groups. (P > 0.05; Fig. 2d). The present molecular study indicates that HFD treatment is associated with decreased mRNA expression of SK channels but not IK channels in the rat DSM.
Decreased mRNA expression levels were foundfor the SK channels in the DSM of HFD rats. Decreased relative mRNA expression levels of SK1 (a), SK2 (b), and SK3 (c) channels in DSM tissue in the ND and HFD groups (n = 16, N = 5 in each; P < 0.05) without significant changes in relative mRNA expression level of the IK (d) channel (P > 0.05). *P < 0.05 for ND versus HFD; NS nonsignificant
NS309, a selective SK/IK channel activator, had an attenuated relaxation effect on spontaneous phasic contraction in isolated DSM strips from HFD rats. Representative recordings of DSM strips isolated from ND (a) and HFD (b) rats showing the concentration-dependent relaxation effects of NS309 (30 nM–10 µM) on spontaneous phasic contractions. Cumulative concentration–response curves illustrating the effects of NS309 on the amplitude (c), muscle integral force (d), duration (e), frequency (f), and tone (g) of spontaneous phasic contractions in ND DSM strips (n = 12, N = 6) and HFD DSM strips (n = 12, N = 7; P < 0.05). *P < 0.05 for ND versus HFD; #P < 0.05 for control versus NS309
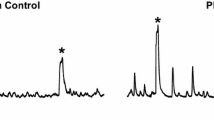
Selective pharmacological activation of SK channel with NS309 had an attenuated relaxation effect on spontaneous phasic contractions in isolated DSM strips from HFD rats
Here, NS309, a selective SK/IK channel activator, was applied to test whether there were changes in the effect of SK/IK channels on spontaneous phasic contraction, which represents the contractility in isolated DSM strips from HFD rats. NS309 (0.3–10 µM) showed a concentration-dependent inhibitory effect on spontaneous phasic contractions in isolated DSM strips for both ND rats (n = 12, N = 6; P < 0.05; Fig. 3) and HFD rats (n = 12, N = 7; P < 0.05; Fig. 3). However, an attenuated relaxation effect of NS309 on spontaneous phasic contractions was recorded in isolated DSM strips from HFD rats (Fig. 3). In addition, NS309 caused the following contraction parameters to decrease: amplitude (17.9 ± 3.7% vs. 61.5 ± 5.1%), muscle integral force (16.5 ± 4.2% vs. 58.4 ± 4.7%), duration (51.2 ± 4.7% vs. 73.4 ± 5.1%), frequency (47.5 ± 4.8% vs. 82.9 ± 4.9%), and tone (80.1 ± 3.2% vs. 92.1 ± 3.3%), respectively (ND vs. HFD, P < 0.05; Fig. 3).
Apamin, a selective SK channel inhibitor, and TRAM-34, an IK channel inhibitor, were applied to determine whether the attenuated effects of NS309 were mediated by SK channels in isolated DSM strips from HFD rats. Apamin (1 µM) significantly antagonized the relaxation effect of NS309, as indicated by all contraction parameters (n = 12, N = 7; P < 0.05; Fig. 4). However, another experimental protocol indicated that there was no significant difference in the effects of NS309 in the presence or absence of TRAM-34 (100 µM) (n = 13, N = 7; P > 0.05; Fig. 4). Therefore, the relaxation effect of NS309 on the spontaneous phasic contractions in isolated DSM strips from HFD rats occurred via the activation of SK channels.
The relaxation effect of NS309 on spontaneous phasic contractions in isolated DSM strips from HFD rats occurred viaSK channelactivation. Original recordings illustrating the different effects of NS309 (30 nM–10 µM) on HFD DSM spontaneous phasic contractions in the presence of 1 µM apamin (a), a selective SK channel blocker, or 100 µM TRAM-34 (b), a selective IK channel blocker. The presence of 100 µM TRAM-34 did not change the cumulative concentration response curve showing the inhibitory effects of NS309 on the amplitude (c), muscle integral force (d), duration (e), frequency (f), and tone (g) in isolated DSM strips from HFD rats (n = 13, N = 7; P > 0.05). The inhibitory effect of NS309 on spontaneous phasic contractions was decreased in isolated DSM strips from HFD rats pretreated with 1 µM apamin to block SK channels (n = 12, N = 7; P < 0.05). *P < 0.05 for Apamin + NS309 versus NS309 or TRAM-34 + NS309 versus NS309
These series of experiments indicates that a HFD induces an attenuated relaxation effect on SK channel activation and on spontaneous phasic contractions in isolated DSM strips.
NS309 has a decreased inhibitory effect on EFS-induced contraction in isolated DSM strips from HFD rats via the activation of SK channels
In addition, 10 µM NS309 significantly decreased the amplitude of EFS-induced contractions in isolated DSM strips from ND (n = 12, N = 7; P < 0.05; Fig. 5a, c) and HFD rats (n = 13, N = 7; P < 0.05; Fig. 5b, d). Furthermore, the inhibitory effect of NS309 (10 µM) on the amplitude of EFS-induced contractions (amplitude decreased to 72.1 ± 5.5%) was attenuated in isolated DSM strips from HFD rats compared with the inhibitory effect on the amplitude (decreased to 23.5 ± 4.1%) in isolated DSM strips from ND rats at the highest EFS stimulation frequency of 50 Hz (P < 0.05; Fig. 5a–d).
The inhibitory effect of NS309 on EFS-induced contractions was attenuated in DSM strips from HFD rats. Original recordings of DSM strips illustrating the inhibitory effects of NS309 (10 µM) on EFS-induced contractions (stimulation frequency 0.5–50 Hz) in the ND (a) and HFD (b) groups. Frequency response curves indicating the differences in the amplitude of EFS-induced contractions in the presence and absence of NS309 (10 µM) in ND DSM strips (c) (n = 12, N = 7) and HFD DSM strips (d) (n = 13, N = 7; P < 0.05). *P < 0.05 for control versus NS309
Next, the HFD DSM strips were preincubated with apamin or TRAM-34 to determine whether the relaxation effect of NS309 on EFS-induced contractions was mediated by SK channels. Apamin (1 µM), the selective SK channel blocker, significantly abolished the relaxation of NS309 on EFS-induced contractions at almost all stimulation frequencies (n = 13, N = 7; P < 0.05; Fig. 6a, c). NS309 (10 µM) reduced the amplitude of EFS-induced contractions to 87.2 ± 4.1% in the presence of apamin (1 µM) (n = 13, N = 7) compared to 72.1 ± 5.5% in the absence of apamin pretreatment (n = 13, N = 7; P < 0.05). However, pretreatment with TRAM-34 had no significant inhibitory effect on the NS309-induced inhibition of EFS-induced contraction (n = 13, N = 7; P > 0.05; Fig. 6b, c). Therefore, the inhibitory effect of NS309 on the amplitude of EFS-induced contractions was mediated by SK channels.
SK channels were found to play a constitutive role in the relaxation effect of NS309 on EFS-induced contractions in HFD DSM strips. Original recordings illustrating the different effects of 10 µM NS309 on EFS-induced contractions of HFD DSM strips pretreated with 1 µM apamin (a) or 100 µM TRAM-34 (b). Frequency response curves illustrating the attenuated relaxation effects of NS309 (10 µM) on the amplitude of EFS-induced contractions in HFD DSM strips in the presence of 1 µM apamin (n = 13, N = 7) (c). Frequency response curves showing that NS309 (10 µM) significantly decreased the EFS-induced contractions in HFD DSM strips in the presence of 100 µM TRAM-34 (n = 13, N = 7; P < 0.05) (c). *P < 0.05 for apamin + NS309 versus NS309 or TRAM-34 + NS309 versus NS309
Our functional study establishes the attenuated regulation effect of SK channels on HFD DSM strip contractility, which is consistent with the molecular experiments.
Discussions
In the present study, we revealed that mRNA expression level of SK1–SK3 channels was significantly decreased in DSM and that selective pharmacological activation of SK channels with NS309 had an attenuated relaxation effect on spontaneous phasic and EFS-induced contractions in isolated DSM strips from HFD rats. The discovery provides important insight into the etiology of OAB.
OAB, affecting the mental health and quality of life of patients, is closely related to diet-induced obesity [5, 43]. In addition, HFD feeding is one of the most commonly used animal models for obtaining important insights into the etiology of OAB. Recently, OAB was observed in obese rats fed a HFD for 24 weeks [44]. We established that rats fed a HFD for 12 weeks showed OAB and increased inflammatory responses in the DSM [9]. In our present study, the rats that were fed a HFD exhibited increased body weight without significant changes in bladder weight, which is consistent with previous studies [9, 44, 45]. In addition, data from our urodynamic study indicated OAB in obese rats, which manifested as more frequent NVCs and shorter voiding intervals, as well as decreased bladder capacity and voiding volume (Fig. 1). However, the maximum voiding pressure did not change significantly in the HFD-induced obese rats (Fig. 1). Therefore, the model of HFD-induced obesity employed here, in which the rats displayed increased body weight and urodynamically established OAB, closely reflects the changes reported in humans.
Recently, we established that the attenuated expression and activity of SK channels, not IK channel, are contributed to PBOO-induced OAB in an animal model [13, 14]. In addition, SK channels had a regulatory effect on the contractility of neurogenic OAB patients’ detrusor strips, which indicated a close association between SK channels and development of OAB [46]. In our present study, a significant reduction in the mRNA expression of SK1, SK2, and SK3 was observed without notable changes in IK mRNA expression when comparing the DSM of HFD rats to the DSM of ND rats (Fig. 2). Our qRT-PCR results provide direct molecular evidence that the decreased expression of SK channels in the DSM is associated with HFD-induced OAB.
It is well known that SK channels and not IK channels play an important regulatory role in DSM contractility, so any changes in the expression of SK channels could significantly alter DSM function [22, 23]. Spontaneous phasic contractions, a feature of DSM, are usually observed in isolated DSM strips obtained from many animals [47]. Here, we assessed all parameters of spontaneous phasic contractions in isolated DSM strips to reveal whether decreased expression of SK channels could result in the different regulatory effect of SK channels on contractility in isolated DSM strips from HFD-induced OAB rats. The pharmacological activation of SK channels with NS309 had an attenuated relaxation effect on spontaneous phasic contractility in isolated DSM strips from HFD rats compared to that in DSM strips from ND rats (Fig. 3). In addition, the application of apamin or TRAM-34 demonstrated that the decreased effect of NS309 on HFD DSM strip contractility is related to the attenuated function of SK channels, not IK channels (Fig. 4).
Acetylcholine and ATP, which are released by parasympathetic nerves, can activate purinergic P2X receptors and muscarinic receptors, resulting in DSM contraction during micturition [47]. EFS at stimulation frequencies 0.5–50 Hz, which can activate the cholinergic and purinergic nerves located in DSM, was performed to determine whether the SK channel modulation of EFS-induced contractions differed between DSM isolated strips from HFD and ND rats. The effect of NS309 on the amplitude of EFS-induced contractions was lower in DSM isolated strips from HFD rats (Fig. 5). Furthermore, preincubation with apamin or TRAM-34 established that the relaxation effect of NS309 on EFS-induced contraction occurred via SK channels, not IK channels (Fig. 6). Combined with the data from the spontaneous phasic contraction experiments, these results clearly show that the selective pharmacological activation of SK channels with NS309 has an attenuated relaxation effect on HFD rat DSM contractility.
OAB, which is generally induced by PBOO, obesity or neurogenic disorders, is closely related to urodynamically demonstrable DO, which is due to the changed DSM contractility [9, 13, 48, 49]. The myogenic basis is associated with an enhanced spontaneous contractile activity of myocytes [49]. It is well known that SK channels act as a negative feedback element in DSM contractility [50]. Therefore, one of the possible explanations for the results of our present study is that the attenuated SK channel expression and activity contribute to the increased DSM contractility, and further OAB in HFD-induced obesity rats.
Our present study provides a notable contribution elucidating the critical functional role of SK channel in obesity-induced OAB. The significantly reduced mRNA expression level of SK1, SK2, and SK3 channels in the DSM from HFD rats was established. In addition, the molecular experiments results were confirmed by functional studies, which indicated a reduced regulatory effect of SK channels on both spontaneous phasic and EFS-induced contractility in isolated DSM strips from HFD-induced obesity rats. Antimuscarinic agents can competitively inhibit acetylcholine which is the main neurotransmitter in DSM to reduce nerve sensitivity, thereby playing a constitutive role in the treatment of OAB. However, conventional antimuscarinic pharmacotherapy causes side effects such as dry mouth, constipation, headache, cardiac, and so on that limit the application of these drugs [51, 52]. Therefore, SK channel activators could be potential strategies for the treatment of these patients.
References
Weisman A et al (2018) Evolving trends in the epidemiology, risk factors, and prevention of type 2 diabetes: a review. Can J Cardiol 34(5):552–564
Murphy M, Robertson W, Oyebode O (2017) Obesity in international migrant populations. Curr Obes Rep 6(3):314–323
Mydlo JH (2004) The impact of obesity in urology. Urol Clin North Am 31(2):275–287
Richter HE et al (2010) The impact of obesity on urinary incontinence symptoms, severity, urodynamic characteristics and quality of life. J Urol 183(2):622–628
Rohrmann S et al (2005) Association between markers of the metabolic syndrome and lower urinary tract symptoms in the Third National Health and Nutrition Examination Survey (NHANES III). Int J Obes (London) 29(3):310–316
Andersson KE (2003) Storage and voiding symptoms: pathophysiologic aspects. Urology 62(5 Suppl 2):3–10
Andersson KE (2009) Prospective pharmacologic therapies for the overactive bladder. Ther Adv Urol 1(2):71–83
Bunn F et al (2015) Is there a link between overactive bladder and the metabolic syndrome in women? A systematic review of observational studies. Int J Clin Pract 69(2):199–217
Ding H et al. (2017) Treatment of obesity-associated overactive bladder by the phosphodiesterase type-4 inhibitor roflumilast. Int Urol Nephrol 49:1723–1730
Oberbach A et al (2014) High fat diet-induced molecular and physiological dysfunction of the urinary bladder. Urologe A 53(12):1805–1811
Fan EW et al (2014) Changes of urinary bladder contractility in high-fat diet-fed mice: the role of tumor necrosis factor-alpha. Int J Urol 21(8):831–835
DiSanto ME et al (2003) Alteration in expression of myosin isoforms in detrusor smooth muscle following bladder outlet obstruction. Am J Physiol Cell Physiol 285(6):C1397–C1410
Li N et al (2016) Partial bladder outlet obstruction is associated with decreased expression and function of the small-conductance Ca2+-activated K+ channel in guinea pig detrusor smooth muscle. Int Urol Nephrol 49(1):17–26
Li N et al (2017) Expression and function of the small-conductance Ca2+-activated K+ channel is decreased in urinary bladder smooth muscle cells from female guinea pig with partial bladder outlet obstruction. Int Urol Nephrol 49:1147–1155
Heppner TJ, Bonev AD, Nelson MT (1997) Ca(2+)-activated K+ channels regulate action potential repolarization in urinary bladder smooth muscle. Am J Physiol 273(1 Pt 1):C110–C117
Hristov KL et al (2011) Large-conductance voltage- and Ca2+-activated K+ channels regulate human detrusor smooth muscle function. Am J Physiol Cell Physiol 301(4):C903–C912
Hristov KL et al (2012) Suppression of human detrusor smooth muscle excitability and contractility via pharmacological activation of large conductance Ca2+-activated K+ channels. Am J Physiol Cell Physiol 302(11):C1632–C1641
Petkov GV (2012) Role of potassium ion channels in detrusor smooth muscle function and dysfunction. Nat Rev Urol 9(1):30–40
GrgicI et al (2009) Endothelial Ca+-activated K+ channels in normal and impaired EDHF-dilator responses–relevance to cardiovascular pathologies and drug discovery. Br J Pharmacol 157(4):509–526
Wulff H, Zhorov BS (2008) K+ channel modulators for the treatment of neurological disorders and autoimmune diseases. Chem Rev 108(5):1744–1773
Kohler M et al (1996) Small-conductance, calcium-activated potassium channels from mammalian brain. Science 273(5282):1709–1714
Parajuli SP et al (2012) Pharmacological activation of small conductance calcium-activated potassium channels with naphtho[1,2-d]thiazol-2-ylamine decreases guinea pig detrusor smooth muscle excitability and contractility. J Pharmacol Exp Ther 340(1):114–123
Parajuli SP et al (2013) NS309 decreases rat detrusor smooth muscle membrane potential and phasic contractions by activating SK3 channels. Br J Pharmacol 168(7):1611–1625
Afeli SA, Rovner ES, Petkov GV (2012) SK but not IK channels regulate human detrusor smooth muscle spontaneous and nerve-evoked contractions. Am J Physiol Renal Physiol 303(4):F559–F568
Coleman N et al (2014) New positive Ca2+-activated K+ channel gating modulators with selectivity for KCa3.1. Mol Pharmacol 86(3):342–357
Ni Y et al (2013) Bisoprolol reversed small conductance calcium-activated potassium channel (SK) remodeling in a volume-overload rat model. Mol Cell Biochem 384(1–2):95–103
Soder RP et al (2013) SK channel-selective opening by SKA-31 induces hyperpolarization and decreases contractility in human urinary bladder smooth muscle. Am J Physiol Regul Integr Comp Physiol 304(2):R155–R163
Ohya S et al (2000) SK4 encodes intermediate conductance Ca2+-activated K+ channels in mouse urinary bladder smooth muscle cells. Jpn J Pharmacol 84(1):97–100
Herrera GM, Heppner TJ, Nelson MT (2000) Regulation of urinary bladder smooth muscle contractions by ryanodine receptors and BK and SK channels. Am J Physiol Regul Integr Comp Physiol 279(1):R60–R68
Imai T et al (2001) Effects of different types of K+ channel modulators on the spontaneous myogenic contraction of guinea-pig urinary bladder smooth muscle. Acta Physiol Scand 173(3):323–333
Buckner SA et al (2002) Spontaneous phasic activity of the pig urinary bladder smooth muscle: characteristics and sensitivity to potassium channel modulators. Br J Pharmacol 135(3):639–648
Herrera GM et al (2003) Urinary bladder instability induced by selective suppression of the murine small conductance calcium-activated potassium (SK3) channel. J Physiol 551(Pt 3):893–903
Hashitani H, Brading AF (2003) Ionic basis for the regulation of spontaneous excitation in detrusor smooth muscle cells of the guinea-pig urinary bladder. Br J Pharmacol 140(1):159–169
Hashitani H, Brading AF (2003) Electrical properties of detrusor smooth muscles from the pig and human urinary bladder. Br J Pharmacol 140(1):146–158
Hashitani H, Brading AF, Suzuki H (2004) Correlation between spontaneous electrical, calcium and mechanical activity in detrusor smooth muscle of the guinea-pig bladder. Br J Pharmacol 141(1):183–193
Thorneloe KS et al (2008) Small-conductance, Ca2+-activated K+ channel 2 is the key functional component of SK channels in mouse urinary bladder. Am J Physiol Regul Integr Comp Physiol 294(5):R1737–R1743
Haddock RE et al (2011) Diet-induced obesity impairs endothelium-derived hyperpolarization via altered potassium channel signaling mechanisms. PLoS ONE 6(1):e16423
Yang S, Li YP (2007) RGS10-null mutation impairs osteoclast differentiation resulting from the loss of [Ca2+]i oscillation regulation. Genes Dev 21(14):1803–1816
He X et al (2013) BMP2 genetically engineered MSCs and EPCs promote vascularized bone regeneration in rat critical-sized calvarial bone defects. PLoS ONE 8(4):e60473
Gui L et al (2012) Role of small conductance calcium-activated potassium channels expressed in PVN in regulating sympathetic nerve activity and arterial blood pressure in rats. Am J Physiol Regul Integr Comp Physiol 303(3):R301–R310
Xin W et al (2014) Constitutive PKA activity is essential for maintaining the excitability and contractility in guinea pig urinary bladder smooth muscle: role of the BK channel. Am J Physiol Cell Physiol 307(12):C1142–C1150
Xin W et al (2014) BK channel-mediated relaxation of urinary bladder smooth muscle: a novel paradigm for phosphodiesterase type 4 regulation of bladder function. J Pharmacol Exp Ther 349(1):56–65
Rohrmann S et al (2004) Associations of obesity with lower urinary tract symptoms and noncancer prostate surgery in the Third National Health and Nutrition Examination Survey. Am J Epidemiol 159(4):390–397
Rahman NU et al (2007) An animal model to study lower urinary tract symptoms and erectile dysfunction: the hyperlipidaemic rat. BJU Int 100(3):658–663
Gharaee-Kermani M et al (2013) Obesity-induced diabetes and lower urinary tract fibrosis promote urinary voiding dysfunction in a mouse model. Prostate 73(10):1123–1133
Oger S et al (2011) Effects of potassium channel modulators on myogenic spontaneous phasic contractile activity in human detrusor from neurogenic patients. BJU Int 108(4):604–611
Andersson KE, Arner A (2004) Urinary bladder contraction and relaxation: physiology and pathophysiology. Physiol Rev 84(3):935–986
Hristov KL et al (2013) Neurogenic detrusor overactivity is associated with decreased expression and function of the large conductance voltage- and Ca2+-activated K+ channels. PLoS ONE 8(7):e68052
Brading AF (1997) A myogenic basis for the overactive bladder. Urology 50(6A Suppl):57–67 (discussion 68–73)
Petkov GV (2011) Role of potassium ion channels in detrusor smooth muscle function and dysfunction. Nat Rev Urol 9(1):30–40
Abrams P, Andersson KE (2007) Muscarinic receptor antagonists for overactive bladder. BJU Int 100(5):987–1006. https://doi.org/10.1111/j.1464-410X.2007.07205.x
Andersson KE (2016) Potential future pharmacological treatment of bladder dysfunction. Basic Clin Pharmacol Toxicol 119:75–85
Acknowledgements
Supported by the LNCCC LNCCC-D16-2015 grant to Ning Li; the National Science Foundation of Liaoning Province 2015020493 grant to Ning Li.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All applicable International, National, and Institutional Guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Li, N., Ding, H., Li, Z. et al. Effect of high-fat diet-induced obesity on the small-conductance Ca2+-activated K+ channel function affecting the contractility of rat detrusor smooth muscle. Int Urol Nephrol 51, 61–72 (2019). https://doi.org/10.1007/s11255-018-2016-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-018-2016-5