Abstract
Purpose
Overactive bladder (OAB), usually accompanied by partial bladder outlet obstruction (PBOO), is associated with detrusor overactivity (DO) which is related to the increased urinary bladder smooth muscle (UBSM) cells excitability. Small-conductance Ca2+-activated K+ (SK) channels play a constitutive regulatory role of UBSM excitability and contractility. PBOO is associated with the decreased SK channels mRNA expression and the attenuated regulative effect of SK channels on UBSM contractility. However, the regulation of SK channels in PBOO UBSM cell excitability is less clear. Here, we tested the hypothesis that PBOO is associated with decreased expression and function of SK channels in UBSM cells and that SK channels are a potential target for the treatment of OAB.
Methods
Cystometry indicated that DO was achieved 2 weeks after PBOO in female guinea pigs. Using this animal model, we conducted single-cell quantitative reverse transcription-polymerase chain reaction (qRT-PCR) and patch-clamp electrophysiology.
Results
The single-cell qRT-PCR experiments indicated the reduced SK channel mRNA expression in PBOO UBSM cells. Patch-clamp studies revealed that NS309 had a diminished effect on resting membrane potential hyperpolarization via the activation of SK channels in PBOO UBSM cells. Moreover, attenuated whole-cell SK channel currents were demonstrated in PBOO UBSM cells.
Conclusions
The attenuated expression and function of SK channels, which results in the increased UBSM cells excitability and contributes to DO, was discovered in PBOO UBSM cells, suggesting that SK channels might be potential therapeutic targets for the control of OAB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive bladder (OAB), which is described as urgency, with or without incontinence, is observed in almost half of partial bladder outlet obstruction (PBOO) patients and is closely associated with detrusor overactivity (DO) [1,2,3]. PBOO can lead to various structural and functional alterations in the lower urinary tract, including urinary bladder smooth muscle (UBSM) remodeling [2,3,4]. Meanwhile, DO is associated with the increased excitability of UBSM cells in PBOO, and changes in the expression and function of UBSM regulatory proteins may contribute to an altered UBSM contractile phenotype [5, 6]. Therefore, PBOO animal models, which can imitate this pathological condition, are often used to study the pathophysiology of OAB.
USBM shows spontaneous phasic contractions driven by spontaneous action potentials. The resting membrane potential (RMP) plays a constitutive role in controlling cell excitability [7, 8]. In UBSM, Ca2+-activated K+ channels can be divided into three groups: large-conductance Ca2+-activated K+ (BK) channels, small-conductance Ca2+-activated K+ (SK) channels, and intermediate-conductance Ca2+-activated K+ (IK) channels [9]. The function and mechanism of BK channels, as very important regulators of UBSM excitability and contractility, have been widely investigated both under physiological conditions and in PBOO [7, 9,10,11,12,13,14,15].
The expression of IK channels has been established in the UBSM of various species including mice, rat, guinea pigs and humans, but IK channels do not appear to play a constitutive role in regulating UBSM function [16,17,18]. On the other hand, SK channels, which are divided into three subtypes (SK1, SK2, and SK3) in mammals, have a small conductance of 4–14 pS; they show substantial physiological effects as powerful modulators in many cell types, including UBSM cells [16,17,18,19,20,21].
Previous researches indicated that whole-cell currents are increased in SK3 channel-overexpressing murine UBSM cells and that the knockout of SK2 channels in mice reduces apamin sensitivity to UBSM contractility [22, 23]. It has been suggested that changes in the expression of SK channels may result in altered UBSM excitability and contractility. Our recent studies established that 2-week PBOO is associated with the decreased SK channel mRNA expression and the attenuated regulatory effect of SK channels on guinea pig UBSM contractility [24]. However, the regulatory role of SK/IK channels in UBSM cells excitability during the development of PBOO is still unknown [12, 25].
In the present study, cystometry, single-cell quantitative reverse transcription-polymerase chain reaction (qRT-PCR), and perforated whole-cell patch-clamp were applied to investigate the mechanism of pharmacological activation and inhibition of SK/IK channels in 2-week PBOO guinea pig UBSM cells. The selective SK/IK channel opener, 6,7-dichloro-1H-indole-2,3-dione 3-oxime (NS309), as well as the SK and IK channel inhibitors apamin and TRAM-34, respectively, were applied in this study. We established that reduced expression and function of SK channels was discovered in guinea pig UBSM cells with PBOO.
Materials and methods
Animals
A total of 61 adult female Hartley Albino guinea pigs (China Medical University) with an age ranging from 8 to 10 weeks and average weight of 403.1 ± 7.5 g were used in this study. All experimental procedures were approved by the Institutional Animal Care and Use Committee of China Medical University.
Surgically induced PBOO in guinea pigs
PBOO was induced as previously described [24]. The urinary bladder, bladder neck and proximal urethra were exposed under anesthesia with 5% isoflurane/O2 gas inspiration. A plastic tube was placed into the urinary bladder via the urethral orifice followed tying the proximal urethra around the catheter, and then the catheter was removed and the incision was closed. The sham operation employed the same procedure except for tying the ligature. Prophylactic antibiotics with ampicillin (100 mg/kg sc) were applied after the operation, along with buprenorphine (0.05 mg/kg sc) to control postoperative pain.
Cystometry
Two weeks after obstruction, general anesthesia was induced with 5% isoflurane/O2 gas inspiration. A catheter was inserted into the bladder dome after surgically exposing the bladder and was connected to a physiological pressure transducer and an injection pump (Dantec Menuet, Denmark). Cystometry was performed by infusing warm saline (37–38 °C) into the bladder at a rate of 12 ml/h. Three voiding events were recorded for each guinea pig to assess the following parameters: maximum voiding pressure (the maximum pressure during voiding), bladder capacity (the volume of saline infused to induce the voiding), voiding volume (the volume of micturition), voiding interval (the interval between voids), and the number of non-voiding contractions (NVCs) during one voiding event. NVCs were defined as spontaneous contractions (>4 cmH2O from the baseline bladder pressure) that did not result in a void.
UBSM single-cell isolation
Guinea pigs were euthanized 2 weeks after PBOO by CO2 inhalation followed by thoracotomy. The urinary bladders were rapidly taken out and cut open longitudinally followed removing the mucosa. One to two UBSM strips were incubated in 2 ml of dissection solution supplemented with 1 mg/ml bovine serum albumin (BSA), 1 mg/ml papain, and 1 mg/ml DL-dithiothreitol at 37 °C for 12–18 min. UBSM strips were then transferred and incubated at 37 °C for 12–15 min in 2 ml of dissection solution supplemented with 1 mg/ml BSA, 0.5 mg/ml type II collagenase, 0.5 mg/ml trypsin inhibitor, and 100 μM CaCl2. The digested UBSM tissues were then washed three times with dissection solution supplemented with 1 mg/ml BSA and gently triturated with a fire-blunted Pasteur pipette to disperse single UBSM cells.
Single-cell qRT-PCR
Total RNA was isolated from freshly isolated UBSM cells using Trizol reagent (Invitrogen, Waltham, MA, USA). Reverse transcription of total RNA was operated using the SuperScript™ first-strand synthesis system (Invitrogen, Waltham, MA, USA) according to the manufacturer’s instructions. Real-time PCR was then performed using the synthesized cDNA on an ABI PRISM 7500 sequence detection system with SYBR GREEN PCR Master Mix [26]. Real-time PCR was carried out to analyze the mRNA expression of SK1, SK2, SK3, IK channels, and β-actin using specific primers (Table 1). The PCR conditions were 94 °C for 1 min followed by 95 °C for 30 s and then 58 °C for 40 s for a total of 35 cycles [27]. All of the reactions were run three times and normalized to β-actin. qRT-PCR products were purified using the GenElute PCR Clean-Up Kit (Sigma-Aldrich, St. Louis, MO, USA), and the sequencing of the SK1–SK3 (Kcnn1–Kcnn3), IK (Kcnn4) and β-actin (actb) genes was confirmed by direct sequencing of the amplified PCR products [28].
Electrophysiological recordings
The amphotericin-B-perforated whole-cell patch-clamp technique was performed to record the RMP and whole-cell currents from freshly isolated guinea pig UBSM single cells as described previously [13, 14]. In brief, patch-clamp recordings were performed using an Axopatch 200B amplifier system and Digidata 1440A controlled with pCLAMP 10.2 software (Molecular Devices, Union City, CA, USA). The recording currents were filtered at 1 kHz with an eight-pole Bessel filter model 900CT/9L8L (Frequency Devices, Ottawa, IL, USA) and sampled at a rate of 10 kHz. The borosilicate glass pipettes were pulled and polished to achieve a final tip resistance of 4–7 MΩ. Whole-cell K+ currents were recorded by holding the UBSM cells at −70 mV, and voltage depolarization was performed from −40 to +80 mV for 200 ms in 20 mV steps; then, cells were repolarized back to −70 mV. The NS309 sensitive outward K+ currents were recorded in the presence of paxilline to block BK channels and TRAM-34 to block IK channels. UBSM cell RMP was recorded in the current-clamp mode of the patch-clamp technique without any current input (Ih = 0). All patch-clamp experiments were conducted at room temperature (22–23 °C).
Solutions and drugs
The dissection solution contained the following: 80 mM monosodium glutamate, 55 mM NaCl, 6 mM KCl, 10 mM glucose, 10 mM HEPES, and 2 mM MgCl2; the pH was adjusted to 7.3 with NaOH. The extracellular solution for patch-clamp experiments contained the following: 134 mM NaCl, 6 mM KCl, 1 mM MgCl2, 2 mM CaCl2, 10 mM glucose, and 10 mM HEPES; the pH was adjusted to 7.4 with NaOH. The pipette solution contained the following: 110 mM potassium aspartate, 30 mM KCl, 10 mM NaCl, 1 mM MgCl2, 10 mM HEPES, and 0.05 mM EGTA; the pH was adjusted to 7.2 with NaOH and supplemented with freshly dissolved 200 μg/ml amphotericin-B in dimethyl sulfoxide (DMSO). The trypsin inhibitor, BSA, and amphotericin-B were obtained from ThermoFisher Scientific (Fair Lawn, NJ, USA). Papain was purchased from Worthington Biochemical (Lakewood, NJ, USA). Paxilline, type II collagenase, TRAM-34, apamin, and NS309 were purchased from Sigma-Aldrich (St. Louis, MO, USA). Amphotericin-B, TRAM-34, paxilline, and NS309 were dissolved in DMSO, while all other chemicals were dissolved in double-distilled water. The maximal DMSO concentration did not exceed 0.1% in the bath solution.
Data analysis and statistics
The relative differences in the PCR results were calculated by using the comparative Ct method (2−ΔΔCt) after determining the Ct values for the reference (β-actin) and target (SK1, SK2, SK3, or IK) genes in each sample [29, 30]. The relative mRNA expression level of the target gene was calculated by normalization to β-actin expression. The RMP was measured as the average of the last 5 min of recording under each experimental condition and analyzed using Clampfit 10.2 (Molecular Devices, Union City, CA, USA). The mean values of the last 50 ms pulse of the 200 ms depolarization step of the recordings were analyzed using Clampfit 10.2 and were used to plot the current–voltage relationships. Data were further analyzed with GraphPad Prism 5.0 software (GraphPad software, San Diego, CA, USA). Data are expressed as mean ± SEM; n = the number of cells and N = the number of guinea pigs. Statistical significance was tested using a t test, or paired Student’s t test, and P < 0.05 was considered statistically significant.
Results
DO was successfully achieved 2 weeks after PBOO
Two weeks after inducing PBOO, bladder capacity was remarkably reduced (PBOO 1.83 ± 0.31 ml, N = 11; sham control 2.64 ± 0.18 ml, N = 9; P < 0.05; Table 2), with a significantly decreased voiding volume (0.91 ± 0.29 ml in PBOO, 1.85 ± 0.27 ml in sham control, P < 0.05; Table 2). Meanwhile, an increased maximum voiding pressure was observed in PBOO guinea pigs (61.2 ± 10.1 cmH2O, N = 11) compared to sham control animals (33.7 ± 7.1 cmH2O, N = 9; P < 0.05; Table 2). Moreover, there was a decrease in the voiding interval (PBOO 4.58 ± 0.89 min, N = 11; sham control 8.37 ± 0.49 min, N = 9; P < 0.05; Table 2) and more frequent NVCs were detected (sham control 0.47 ± 0.19, N = 9; PBOO 4.78 ± 0.41, N = 11; P < 0.05; Table 2), indicating that DO was already induced 2 weeks after PBOO.
SK channels, not IK channels, indicated a significantly decreased mRNA expression levels in PBOO UBSM cells
The mRNA expression of SK channels, not IK channels, was altered in PBOO bladder mucosa and smooth muscle, including rat and guinea pig [12, 17, 24, 25]. Accordingly, we compared the gene expression of SK/IK channels between sham control and PBOO guinea pig UBSM cells using single-cell qRT-PCR. Our data demonstrate that the mRNA expression of SK1–SK3 channels was markedly decreased to 64.2 ± 0.2%, 70.7 ± 0.1%, and 23.6 ± 0.2% (N = 5) in PBOO UBSM cells, respectively, compared with sham controls (N = 4; P < 0.05; Fig. 1a–c). However, there was no significant reduction in IK channel mRNA expression in guinea pig UBSM cells 2 weeks after PBOO (P > 0.05; Fig. 1d). These single-cell qRT-PCR results indicate that the decreased mRNA expression of SK channels may contribute to the altered excitability of PBOO guinea pig UBSM cells.
SK channels, not IK channels, indicated a significantly decreased mRNA expression levels in PBOO UBSM cells. Single-cell qRT-PCR analyses indicating that the mRNA expression of SK1 (a), SK2 (b), and SK3 (c) channels was reduced to 64.2 ± 0.2, 70.7 ± 0.1, and 23.6 ± 0.2%, respectively, (*P < 0.05) without significant alterations in IK channel mRNA expression (d) (P > 0.05; NS non-significant) in PBOO UBSM cells (N = 5) compared with UBSM cells in sham controls (N = 4). Data are shown as relative mRNA expression normalized to β-actin
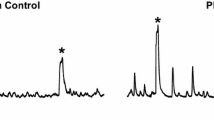
Pharmacological activation of SK channels has an attenuated hyperpolarization effect on the RMP of PBOO UBSM cells
Recently, it has been established that SK channels, not IK channels, are important regulators of UBSM cell excitability under physiological conditions [16,17,18, 31]. Here, we assessed whether the regulation of SK/IK channels on the RMP of UBSM cells changed during PBOO using the current-clamp mode (I = 0) with the amphotericin-B-perforated whole-cell patch-clamp technique. The average UBSM cell capacitance was 27.3 ± 1.3 pF in sham control UBSM cells (n = 8, N = 5) and 26.2 ± 1.1 pF in UBSM cells from PBOO guinea pigs (n = 25, N = 18; P > 0.05). NS309 (10 μM), a SK/IK channel activator, significantly hyperpolarized UBSM cell RMP from a control value of −23.6 ± 2.2 to −29.8 ± 1.8 mV in sham control UBSM cells (n = 8, N = 5; P < 0.05; Fig. 2a) and from values of −22.8 ± 1.7 to −26.2 ± 2.4 mV in UBSM cells from PBOO guinea pigs (n = 8, N = 6; P < 0.05; Fig. 2b). There was no significant difference in the RMP of sham control UBSM cells (n = 8, N = 5) and PBOO UBSM cells before the application of NS309 (n = 8, N = 6; P > 0.05). Furthermore, the effect of hyperpolarization induced by NS309 was attenuated in PBOO UBSM cells (3.5 ± 0.8 mV; n = 8, N = 6) compared with sham control UBSM cells (6.1 ± 0.9 mV; n = 8, N = 5; P < 0.05; Fig. 2a–c).
Pharmacological activation of SK/IK channels has an attenuated hyperpolarization effect on the RMP of PBOO UBSM cells. Original recordings illustrating the effect of NS309 (10 μM) on the RMP in a sham control UBSM cell (a) and in a PBOO UBSM cell (b). c Summary data showing the differences in the hyperpolarization effect on the RMP in the absence or presence of NS309 (10 μM) in sham control UBSM cells (n = 8, N = 5; *P < 0.05) and PBOO UBSM cells (n = 8, N = 6; *P < 0.05). NS309 (10 μM) caused reduced hyperpolarization of the RMP of PBOO UBSM cells compared with sham control UBSM cells (# P < 0.05)
The role of SK channels in PBOO UBSM cell RMP hyperpolarization induced by NS309 was further examined by applying apamin, a selective SK channel inhibitor, before the addition of NS309. Apamin (1 μM) did not significantly hyperpolarize the UBSM cell RMP which was −24.6 ± 1.4 mV in the absence of apamin and −23.7 ± 2.8 mV in the presence of apamin (n = 9, N = 6; P > 0.05; Fig. 3a, c). In the presence of apamin (1 μM), the subsequent application of NS309 (10 μM) did not significantly change the RMP, recorded as −25.5 ± 1.1 mV (n = 9, N = 6; P > 0.05; Fig. 3a, c).
The RMP hyperpolarization induced by NS309 occurs via the activation of SK but not IK channels in PBOO UBSM cells. Representative recordings in current-clamp mode illustrating the NS309 (10 μM)-induced hyperpolarizing effect on PBOO UBSM cell RMP in the presence of 1 μM apamin to block SK channels (a) or 1 μM TRAM-34 to block IK channels (b). c Summary data showed that apamin (1 μM) could not hyperpolarize the RMP and NS309 (10 μM) did not have any effect on the RMP in PBOO UBSM cells pretreated with 1 μM apamin (n = 9, N = 6; P > 0.05; NS non-significant). d Summary data illustrating that pharmacological inhibition of IK channels with TRAM-34 (1 μM) did not change the PBOO UBSM cell RMP (n = 8, N = 6; P > 0.05; NS non-significant), and could not alter the NS309-induced hyperpolarizing effect on PBOO UBSM cell RMP (n = 8, N = 6; *P < 0.05)
In addition, TRAM-34, a selective IK channel inhibitor, was present before the application of NS309 in PBOO UBSM cells to explore whether NS309-induced PBOO UBSM cell RMP hyperpolarization was mediated via the activation of IK channels. Our results indicate that the UBSM cell RMP (−27.2 ± 1.6 mV) did not change significantly after the application of TRAM-34 (1 μM) (n = 8, N = 6; P > 0.05; Fig. 3b, d). NS309 (10 μM) significantly hyperpolarized the PBOO UBSM cell RMP from −26.1 ± 2.2 to −29.3 ± 2.2 mV in the presence of TRAM-34 (1 μM) (n = 8, N = 6; P < 0.05; Fig. 3b, d).
In conclusion, our current-clamp data demonstrate that the RMP hyperpolarization induced by NS309, which occurred via the activation of SK but not IK channels, was attenuated in PBOO UBSM cells.
NS309-induced whole-cell SK currents are decreased in freshly isolated PBOO guinea pig UBSM cells
It has already been shown that NS309-induced whole-cell K+ currents occur due to the activation of SK channels, not IK channels, in freshly isolated rat UBSM cells [18]. In this series of experiments, we examined whether NS309-induced steady-state SK currents changed in PBOO UBSM cells using a depolarizing voltage-step protocol at a holding potential of −70 mV in the presence of paxilline (300 nM) and TRAM-34 (1 μM) to block BK and IK currents. The average guinea pig UBSM cell capacitance was 26.5 ± 1.2 pF in sham control UBSM cells (n = 11, N = 8) and 27.4 ± 0.7 pF in UBSM cells from PBOO guinea pigs (n = 22, N = 17; P > 0.05).
Firstly, the current–voltage relationships illustrate that NS309 significantly increased whole-cell K+ currents in both sham control UBSM cells (n = 11, N = 8; P < 0.05; Fig. 4a, c) and UBSM cells from PBOO guinea pigs (n = 12, N = 9; P < 0.05; Fig. 4b, d). Moreover, it was found that NS309-sensitive whole-cell K+ currents were attenuated in PBOO UBSM cells compared with UBSM cells from sham control guinea pigs (P < 0.05; Fig. 4e).
NS309-induced whole-cell SK currents are decreased in PBOO freshly isolated guinea pig UBSM cells. Original recordings illustrating that 10 μM NS309 increased the voltage-dependent steady-state whole-cell SK currents in a sham control UBSM cell (a) and in a PBOO UBSM cell (b). Current–voltage relationships illustrating the reduced effect of NS309 (10 μM) on whole-cell SK currents in PBOO UBSM cells (n = 12, N = 9; *P < 0.05) (d, e) compared with sham control UBSM cells (n = 11, N = 8; *P < 0.05; NS non-significant) (c, e). SK currents were recorded in the presence of paxilline and TRAM-34 to block BK and IK channels
Secondly, a selective SK channel blocker, apamin (1 μM), was added before the application of NS309 in PBOO UBSM cells to determine whether NS309-induced whole-cell K+ currents were mediated via the activation of SK channels. The current–voltage relationships show that NS309 had no significant effect on whole-cell K+ currents in the presence of 1 μM apamin (n = 10, N = 8; P > 0.05; Fig. 5).
Pharmacological inhibition of SK channels with apamin (1 μM) abolishes the activating effect of NS309 on whole-cell SK currents in PBOO UBSM cells. a Representative voltage-clamp recordings showing that blocking SK channels with 1 μM apamin decreased NS309-sensitive whole-cell SK currents. b Current–voltage relationships illustrating 10 μM NS309 did not affect the whole-cell SK currents in the presence of 1 μM apamin (n = 10, N = 8; P > 0.05). SK currents were recorded in the presence of paxilline and TRAM-34
These data provide evidence that NS309-induced whole-cell K+ currents, which occur due to the activation of SK channels, were reduced in PBOO UBSM cells compared to UBSM cells from sham control guinea pig. The voltage-clamp data, which were consistent with the current-clamp data, established that the regulation of SK channels in UBSM cell excitability was decreased 2-week after PBOO induction.
Discussion
The present study revealed that SK channels play a constitutive role in the pathophysiology of PBOO and established a significant decrease in the expression and function of SK channels in the UBSM cells under these conditions. We discovered the mRNA expression of the SK1–SK3 channels was significantly decreased in PBOO UBSM cells, and pharmacological activation of SK channels with NS309 had a reduced effect on RMP hyperpolarization, and whole-cell SK currents were reduced in PBOO UBSM freshly isolated cells.
In our previous research, DO was successfully induced 2 weeks after PBOO, which is in line with reports in the literature [24, 32, 33]. In the present study, cystometry indicated reduced bladder capacity and voiding volume, a shorter voiding interval, an increased maximum voiding pressure, and more frequent NVCs in PBOO guinea pigs (Table 2). The present results further established that PBOO animal models were suitable for studying the pathophysiology of OAB.
Our previous research discovered the decreased mRNA expression of SK channels, but not IK channels, in PBOO guinea pig UBSM, which could contribute to the reduced regulatory role of SK channels in UBSM contractility [24]. However, the results seemed contradictory to some previous researches shown in the literature and the possible reasons for the above-mentioned differences perhaps included the species-based differences in the expression of SK channel subtype in UBSM [12, 16,17,18, 22, 25, 31]. In the present study, we collected the freshly isolated UBSM single cells in qRT-PCR to exclude any potential contamination by other non-UBSM cell types including endothelial cells, fibroblasts, vascular cells and neurons within the UBSM layers [16, 17]. Our present data indicated a significant decrease in the mRNA expression of SK1, SK2, and SK3, but no statistically significant changes in IK mRNA expression in PBOO guinea pig UBSM cells (Fig. 1) [24]. These data are in accordance with our previous molecular result using UBSM tissues and provide further evidence that the attenuated expression of SK channels, not IK channels, contributes to PBOO.
A reduced effect of SK channels on RMP has been shown in PBOO UBSM cells [25]. It is known that SK channels play a critical role in UBSM cell excitability [16,17,18, 31], but the function of SK channels has not been studied in PBOO UBSM cells by the perforated patch-clamp technique. In the present study, we report that the pharmacological activation of SK channels with NS309 remarkably hyperpolarized the RMP in both sham control and PBOO UBSM cells. However, NS309 treatment led to reduced RMP hyperpolarization in UBSM cells from PBOO guinea pigs compared to sham control UBSM cells (Fig. 2). Furthermore, apamin and TRAM-34 were applied to confirm that NS309 regulates UBSM RMP via SK channels, not IK channels (Fig. 3).
SK current activation was detected at a holding potential in the range of −40 to −30 mV, which is close to the RMP values in UBSM cells [34]. Therefore, the perforated patch-clamp technique was performed to record SK currents in the presence of paxilline and TRAM-34 to block BK and IK currents. Our patch-clamp data indicated that NS309-sensitive currents were significantly decreased in UBSM cells from PBOO guinea pigs compared to sham control UBSM cells (Fig. 4). It has already been established that the inhibitory effect of NS309 on UBSM cell excitability is mediated by SK channels but not IK channels under physiological conditions [18]. Furthermore, apamin was applied to confirm that NS309-sensitive currents were via SK channels, not IK channels (Fig. 5). Therefore, the patch-clamp data are consistent with our molecular data and show that SK channel function is significantly reduced in PBOO UBSM cells, although SK channels still play a regulatory role in cell excitability. Furthermore, our present patch-clamp data elucidated that the reduced inhibitory effect of SK channels in PBOO UBSM contractility indicated in our previous study was perhaps due to the attenuated regulatory role of SK channels in RMP and the decreased SK current in PBOO UBSM cells [24].
In summary, the present study revealed an outstanding decrease in the mRNA expression level of the SK1, SK2, and SK3 channels in UBSM cells from PBOO guinea pigs. Furthermore, we investigated SK channel activity in PBOO UBSM cells using the perforated patch-clamp approach and discovered the attenuated RMP hyperpolarization and decreased whole-cell SK currents in UBSM cells from PBOO guinea pigs. Taken together, the attenuated expression and function of SK channels is associated with PBOO and SK channels could represent novel therapeutic targets for the pharmacological treatment of OAB.
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21(2):167–178
Andersson KE (2003) Storage and voiding symptoms: pathophysiologic aspects. Urology 62(5 Suppl 2):3–10
Oelke M, Baard J, Wijkstra H, de la Rosette JJ, Jonas U, Hofner K (2008) Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur Urol 54(2):419–426. doi:10.1016/j.eururo.2008.02.017
Chacko S, Chang S, Hypolite J, Disanto M, Wein A (2004) Alteration of contractile and regulatory proteins following partial bladder outlet obstruction. Scand J Urol Nephrol Suppl 215:26–36. doi:10.1080/03008880410015147
Bing W, Chang S, Hypolite JA, DiSanto ME, Zderic SA, Rolf L, Wein AJ, Chacko S (2003) Obstruction-induced changes in urinary bladder smooth muscle contractility: a role for Rho kinase. Am J Physiol Renal Physiol 285(5):F990–F997. doi:10.1152/ajprenal.00378.2002
DiSanto ME, Stein R, Chang S, Hypolite JA, Zheng Y, Zderic S, Wein AJ, Chacko S (2003) Alteration in expression of myosin isoforms in detrusor smooth muscle following bladder outlet obstruction. Am J Physiol Cell Physiol 285(6):C1397–C1410. doi:10.1152/ajpcell.00513.2002
Heppner TJ, Bonev AD, Nelson MT (1997) Ca(2+)-activated K+ channels regulate action potential repolarization in urinary bladder smooth muscle. Am J Physiol 273(1 Pt 1):C110–C117
Hashitani H, Brading AF (2003) Ionic basis for the regulation of spontaneous excitation in detrusor smooth muscle cells of the guinea-pig urinary bladder. Br J Pharmacol 140(1):159–169. doi:10.1038/sj.bjp.0705320
Petkov GV (2011) Role of potassium ion channels in detrusor smooth muscle function and dysfunction. Nat Rev Urol 9(1):30–40. doi:10.1038/nrurol.2011.194
Hristov KL, Chen M, Kellett WF, Rovner ES, Petkov GV (2011) Large-conductance voltage- and Ca2+-activated K+ channels regulate human detrusor smooth muscle function. Am J Physiol Cell Physiol 301(4):C903–C912. doi:10.1152/ajpcell.00495.2010
Hristov KL, Parajuli SP, Soder RP, Cheng Q, Rovner ES, Petkov GV (2012) Suppression of human detrusor smooth muscle excitability and contractility via pharmacological activation of large conductance Ca2+-activated K+ channels. Am J Physiol Cell Physiol 302(11):C1632–C1641. doi:10.1152/ajpcell.00417.2011
Kita M, Yunoki T, Takimoto K, Miyazato M, Kita K, de Groat WC, Kakizaki H, Yoshimura N (2010) Effects of bladder outlet obstruction on properties of Ca2+-activated K+ channels in rat bladder. Am J Physiol Regul Integr Comp Physiol 298(5):R1310–R1319. doi:10.1152/ajpregu.00523.2009
Xin W, Li N, Cheng Q, Petkov GV (2014) BK channel-mediated relaxation of urinary bladder smooth muscle: a novel paradigm for phosphodiesterase type 4 regulation of bladder function. J Pharmacol Exp Ther 349(1):56–65. doi:10.1124/jpet.113.210708
Xin W, Li N, Cheng Q, Fernandes VS, Petkov GV (2014) Constitutive PKA activity is essential for maintaining the excitability and contractility in guinea pig urinary bladder smooth muscle: role of the BK channel. Am J Physiol Cell Physiol 307(12):C1142–C1150. doi:10.1152/ajpcell.00167.2014
Hristov KL, Afeli SA, Parajuli SP, Cheng Q, Rovner ES, Petkov GV (2013) Neurogenic detrusor overactivity is associated with decreased expression and function of the large conductance voltage- and Ca(2+)-activated K(+) channels. PLoS ONE 8(7):e68052. doi:10.1371/journal.pone.0068052
Afeli SA, Rovner ES, Petkov GV (2012) SK but not IK channels regulate human detrusor smooth muscle spontaneous and nerve-evoked contractions. Am J Physiol Renal Physiol 303(4):F559–F568. doi:10.1152/ajprenal.00615.2011
Parajuli SP, Soder RP, Hristov KL, Petkov GV (2012) Pharmacological activation of small conductance calcium-activated potassium channels with naphtho[1,2-d]thiazol-2-ylamine decreases guinea pig detrusor smooth muscle excitability and contractility. J Pharmacol Exp Ther 340(1):114–123. doi:10.1124/jpet.111.186213
Parajuli SP, Hristov KL, Soder RP, Kellett WF, Petkov GV (2013) NS309 decreases rat detrusor smooth muscle membrane potential and phasic contractions by activating SK3 channels. Br J Pharmacol 168(7):1611–1625. doi:10.1111/bph.12049
Wulff H, Zhorov BS (2008) K+ channel modulators for the treatment of neurological disorders and autoimmune diseases. Chem Rev 108(5):1744–1773. doi:10.1021/cr078234p
Ni Y, Wang T, Zhuo X, Song B, Zhang J, Wei F, Bai H, Wang X, Yang D, Gao L, Ma A (2013) Bisoprolol reversed small conductance calcium-activated potassium channel (SK) remodeling in a volume-overload rat model. Mol Cell Biochem 384(1–2):95–103. doi:10.1007/s11010-013-1785-5
Coleman N, Brown BM, Olivan-Viguera A, Singh V, Olmstead MM, Valero MS, Kohler R, Wulff H (2014) New positive Ca2+-activated K+ channel gating modulators with selectivity for KCa3.1. Mol Pharmacol 86(3):342–357. doi:10.1124/mol.114.093286
Thorneloe KS, Knorn AM, Doetsch PE, Lashinger ES, Liu AX, Bond CT, Adelman JP, Nelson MT (2008) Small-conductance, Ca(2+)-activated K+ channel 2 is the key functional component of SK channels in mouse urinary bladder. Am J Physiol Regul Integr Comp Physiol 294(5):R1737–R1743. doi:10.1152/ajpregu.00840.2006
Herrera GM, Pozo MJ, Zvara P, Petkov GV, Bond CT, Adelman JP, Nelson MT (2003) Urinary bladder instability induced by selective suppression of the murine small conductance calcium-activated potassium (SK3) channel. J Physiol 551(Pt 3):893–903. doi:10.1113/jphysiol.2003.045914
Li N, He X, Li Z, Liu Y, Wang P (2016) Partial bladder outlet obstruction is associated with decreased expression and function of the small-conductance Ca2+-activated K+ channel in guinea pig detrusor smooth muscle. Int Urol Nephrol. doi:10.1007/s11255-016-1455-0
Li L, Jiang C, Song B, Yan J, Pan J (2008) Altered expression of calcium-activated K and Cl channels in detrusor overactivity of rats with partial bladder outlet obstruction. BJU Int 101(12):1588–1594. doi:10.1111/j.1464-410X.2008.07522.x
Yang S, Li YP (2007) RGS10-null mutation impairs osteoclast differentiation resulting from the loss of [Ca2+]i oscillation regulation. Genes Dev 21(14):1803–1816. doi:10.1101/gad.1544107
He X, Dziak R, Yuan X, Mao K, Genco R, Swihart M, Sarkar D, Li C, Wang C, Lu L, Andreadis S, Yang S (2013) BMP2 genetically engineered MSCs and EPCs promote vascularized bone regeneration in rat critical-sized calvarial bone defects. PLoS ONE 8(4):e60473. doi:10.1371/journal.pone.0060473
Gui L, LaGrange LP, Larson RA, Gu M, Zhu J, Chen QH (2012) Role of small conductance calcium-activated potassium channels expressed in PVN in regulating sympathetic nerve activity and arterial blood pressure in rats. Am J Physiol Regul Integr Comp Physiol 303(3):R301–R310. doi:10.1152/ajpregu.00114.2012
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3(6):1101–1108
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(−ΔΔC(T)) method. Methods 25(4):402–408. doi:10.1006/meth.2001.1262
Soder RP, Parajuli SP, Hristov KL, Rovner ES, Petkov GV (2013) SK channel-selective opening by SKA-31 induces hyperpolarization and decreases contractility in human urinary bladder smooth muscle. Am J Physiol Regul Integr Comp Physiol 304(2):R155–R163. doi:10.1152/ajpregu.00363.2012
Kubota Y, Hashitani H, Shirasawa N, Kojima Y, Sasaki S, Mabuchi Y, Soji T, Suzuki H, Kohri K (2008) Altered distribution of interstitial cells in the guinea pig bladder following bladder outlet obstruction. Neurourol Urodyn 27(4):330–340. doi:10.1002/nau.20502
Scheepe JR, de Jong BW, Wolffenbuttel KP, Arentshorst ME, Lodder P, Kok DJ (2007) The effect of oxybutynin on structural changes of the obstructed guinea pig bladder. J Urol 178(4 Pt 2):1807–1812. doi:10.1016/j.juro.2007.03.187
Petkov GV, Heppner TJ, Bonev AD, Herrera GM, Nelson MT (2001) Low levels of K(ATP) channel activation decrease excitability and contractility of urinary bladder. Am J Physiol Regul Integr Comp Physiol 280(5):R1427–R1433
Funding
This study was funded by a Grant from LNCCC of LNCCC-D16-2015 to Ning Li.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Li, N., Ding, H., He, X. et al. Expression and function of the small-conductance Ca2+-activated K+ channel is decreased in urinary bladder smooth muscle cells from female guinea pig with partial bladder outlet obstruction. Int Urol Nephrol 49, 1147–1155 (2017). https://doi.org/10.1007/s11255-017-1592-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1592-0