The pleiotropic pharmacological actions of 9,10-anthraquinone dithiocarbamates were studied. The Way2Drug web portal was used to establish that cytotoxic, antiviral, and anticonvulsant actions were predicted for the study molecules, along with moderate toxicity. In vitro experimental studies showed that all study compounds had cytotoxic effects on tumor cell lines Hep-2, CHO, HeLa, Raji, BL, and B95-8. The high levels of cytotoxicity against cell lines Raji and B95-8 seen with derivatives II, IV, VI, and X was evidence of direct actions on Epstein-Barr virus (EBV). Along with the cytotoxic action, dithiocarbamates V, VIII, and IX showed antiviral effects against herpes virus HSV-2. Compounds VI and X, which had cytotoxic and antiviral actions, produced anticonvulsant effects 3 and 6 h after administration, while dithiocarbamate III, which had cytotoxic activity, retained its antiviral effect 24 h after administration. Dithiocarbamates with pleiotropic actions were moderately toxic (LD50 > 1000 mg/ml, mice, p.o.). Interactions between the structures and the three types of biological activity studied experimentally were assessed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Malignant neoplasms are the second most common cause of death throughout the world. Chemotherapy is widely used in the treatment of cancer and for various types of cancer, including leukemia, it remains the only effective method. Viral infections in patients with oncological disease lead to serious complications [1]. Furthermore, a number of oncoviruses, such as Epstein-Barr virus and herpes simplex virus (HSV), are associated with the occurrence and development of cancers [2,3,4]. Many patients with gliomas, meningiomas, and systemic oncological diseases develop convulsions, which generates the need for anticonvulsant therapy [5]. The combined prescription of multiple drugs (antitumor, antibacterial, antifungal, antiviral, antiemetic, anti-inflammatory, anticonvulsant, immunomodulator, etc.) with different mechanisms of action is widely used in the treatment of patients with malignant neoplasms. However, this treatment produces, along with positive effects, increases in the risk of unwanted interactions between drugs, resulting in increases in the number of side effects [6,7,8] and/or therapeutic resistance [9, 10]. Use of pharmacological agents with pleiotropic actions prevents the development and decreases the consequences of infectious complications in the chemotherapy of malignant neoplasms [11,12,13]. As a result, the development of low-toxicity substances with pleiotropic actions, combining cytotoxic, antiviral, antibacterial, antifungal, and anticonvulsant effects in a single molecule, represents a potential direction in the search for and creation of novel chemotherapeutic drugs.
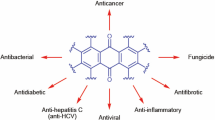
Derivatives of 9,10-anthraquinone display various pharmacological effects – antitumor, antimicrobial, antiviral, antioxidant, antiprotozoal, antidiabetic, etc. [14,15,16,17]. The search for novel pharmaceutical substances based on compounds of this class is ongoing [18,19,20]. A number of successfully functionalized derivatives of 9,10-anthraquinone are currently in various stages of preclinical and clinical trials [21]. We have previously reported the synthesis of 9,10-anthraquinone dithiocarbamates and studies of their antioxidant and antiplatelet activities [22, 23]. We have also studied the cytotoxic actions of dithiocarbamates in human lung (A549), prostate (PC3), large intestine (HT29), and breast (MCF7) tumor cell lines using the SRB method [24].
We report here the results of computer prediction of the biological activities of 9,10-anthraquinone dithiocarbamates and experimental testing of the cytotoxic, antiviral, and anticonvulsant activities, as well as the acute toxicity of these compounds, and evidence was obtained of the potential of the search for pleiotropic pharmacological substances among compounds of this chemical class.
Experimental Section
Predictions of biological activity were made using the web services PASS Online, CLC-Pred, and Acute Rat Toxicity in the Way2Drug web portal [25,26,27,28]. Input data for obtaining prediction results were the structural formulas of substances presented as MOL files. MOL files were prepared using the program MarvinSketch (www.chemaxon.com). Prediction results were lists of probable types of biological activity with assessments of two probabilities - the presence of activity Pa and the absence of activity Pi.
Cytotoxic activity was studied using cell cultures included in the catalog of the European Collection of Cell Cultures (ECACC): Hep-2 (human throat epidermoid carcinoma cells), HeLa (human cervical cancer cells), Raji (human type B undifferentiated lymphoblasts from a Burkitt’s lymphoma, which contain EBV), CHO cells (Chinese hamster ovary cells), BL (an experimental B-cell line), and B95-8 (EBV-transformed marmoset leukocytes which chronically produce EBV). Epithelial cell line were grown in sterile flasks (Sigma, USA) in medium containing 45% DMEM (Sigma, USA), 45% RPMI 1640 (Sigma, USA), and 10% heat-inactivated (56°C) fetal calf serum (Sigma, USA), and antibiotics – penicillin/streptomycin (0.1%). Cells were reseeded after forming monolayers. Cell dilutions were determined using a Goryaev counting chamber and a Lomo inverted microscope (Russia) with magnification ×70. Cells were removed from flask surfaces with 0.02% Versene solution, suspended in nutrient medium, and their concentrations in suspension were then adjusted to 3 × 105 cells/ml. Lymphoblast cell lines were cultured in medium containing 90% RPMI 1640 (Sigma, USA), 10% heat-inactivated (56°C) embryonic calf serum (Sigma, USA), and 0.1% penicillin/streptomycin. Plates with cell cultures were incubated at 37°C in a 5% CO2 atmosphere. Starting solutions of test substances I – X were prepared in DMSO. Substance dilutions were prepared in growth medium. Solutions were filtered through syringe membrane filters (Sarstedt, Germany) with pore diameter 0.45 μm and stored for use at +4°C. Studies used the MTT method [29]. Cells were grown in 96-well plates in medium. After incubation for 24 h, culture medium was replaced with medium containing dissolved substances at different concentrations (200 μl per well). Two-fold serial dilutions of compounds were made in nutrient medium without fetal calf serum. Old medium was replaced with fresh in control samples (no substances). Platelets with cells were kept in an incubator at 37°C in a 5% CO2 atmosphere for 72 h. Cell monolayers were monitored using a Lomo inverted microscope (Russia) (ocular ×7, objective ×10). MTT(sigma, USA) was dissolved in sterile phosphate buffer pH 7.2 at room temperature to a concentration of 5 mg/ml; 20 μl of MTT solution was placed in each well of the 96-well plate and incubated for 2 – 4 h at 37°C. Medium was removed after incubation and 150 μl of 96% ethanol was added to dissolve formazan crystals. The optical densities of solution were determined spectrophotometrically using a Multiscan FC universal microplate reader (Thermo Scientific, USA) at 540 nm. Concentrations of compounds producing 50% inhibition of cell viability (CC50) were compared with controls. Analysis of substance CC50 concentrations was by linear regression in Microsoft Excel. The cytotoxic actions of study compounds were compared with that of reference agent mitoxantrone.
Antiviral activity was studied in strains of human serotype 5 adenovirus (Ad h5), US herpes simplex virus type 1 (HSV-1/US), BH herpes simplex type 2 virus (HSV-2/BH). Ad h5 was obtained from the collection of the Institute of Microbiology, Budapest Medical University. HSV-1/US was obtained from the collection of the Institute of Antiviral Chemotherapy, Center for Clinical and Theoretical Medicine (Germany). HSV-2/BH was obtained from the collection of the Institute of Epidemiology and Infectious Diseases, Ukrainian Academy of Medical Sciences. Antiviral actions of substances were evaluated in terms of inhibition of the cytopathic effects of viruses using the spectrophotometric MTT method. Cells were infected with 40 μl of a previously determined dose of virus at 24 h of cell growth and formation of monolayers in 96-well plates. Virus was adsorbed at room temperature for 2 h in a 5% CO2 atmosphere. Cells were washed to remove unadsorbed virus with Hank’s balanced salt solution and 200 μl of two-fold dilutions of test substances was added to each well. Platelets with cells were incubated in an incubator at 37°C in a 5% CO2 atmosphere, 20 μl of MTT solution (5 mg/ml) were added to each well, and incubation was continued in a 5% CO2 atmosphere at 37°C for 4 h. Medium was then removed from each well and 150 μl of DMSO was added to wash stain from cells. plates were read using a Multiscan FC automatic plate reader (Thermo Scientific, USA) at 540 nm. The optical density of each well was compared with the optical density of solvent as control. Percentage inhibition of virus multiplication was determined as
where ODcs is the mean optical density of control samples, ODvc is the mean optical density of the virus control, and ODes is the mean optical density of the experimental samples.
The extent of the antiviral activity of compounds was assessed in terms of EC50– the concentration of compound producing 50% inhibition of virus replication in cultures of infected cells. The index of selectivity (IS) was used to identify compounds for further studies and was calculated using Equation (2). Compounds with IS ≥ 4 were regarded as active, with potential for further in vivo study.
The antiviral activities of test substances were compared with those of reference agents acyclovir (for HSV-1/US EC50 = 7.7 ± 0.9 μg/ml, HSV-2/BH EC50 = 1.75 ± 0.33) and ganciclovir (for Ad h5 EC50 = 60 ± 0.85 μg/ml).
The anticonvulsant activities of compounds I – X were studied in white male mice (18 – 22 g). All animals were kept in conditions of a 12-h light regime and in a standard location for animals, with free access to water and food in compliance with the European Convention for the Protection of Vertebrates Used for Experimental and Other Specific Purposes (Strasbourg, 1986) and the Guidelines of the European Council for Studies on Biological Materials of Human Origin (2006). Animals were obtained from Odessa National Medical University (ONMU); the studies were approved by the ONMU Ethics Committee. The anticonvulsant activities of compounds were studied at a dose of 100 mg/kg and were compared with reference drug – valproic acid (VPA), used at a dose of 200 mg/kg. Mice received compounds p.o. in Tween 80/water emulsion and controls consisted of Tween 80/water emulsion. The anticonvulsant activities of compounds were determined using a corasol model, which includes determination of the minimum effective dose (MED) of corasol inducing clonic-tonic convulsions (CTC) and tonic extension (TE) in the experimental animals on i.v. infusion of 1% aqueous corasol solution into the tail vein. The corasol doses for induction of clonic-tonic convulsions (DCTC) and tonic extension (DTE) were calculated in relation to controls. The anticonvulsant effects of compounds were evaluated at specified time points after administration (3, 6, and 24 h) as compared with the control group. MED (%) was calculated as:
where MED is the minimum effective dose of corasol inducing DCTC or DTE, V is the volume of corasol solution, and m is the weight of the animal, g.
The acute toxicity of compounds was studied using a method analogous to that described in [30]. Acute toxicity (LD50) in mice was determined by p.o. administration of compounds I – X. Mice were divided into groups of 10 animals in each and anthraquinone derivatives were given as single doses of 100, 250, 500, and 1000 mg/kg in Tween-80/water emulsion, while the control group received only Tween-80 in water. Observations for possible toxic symptoms in the animals were continued for 24 h after substance administration. The toxicity class for anthraquinone derivatives was determined using the OECD classification [31].
Data from all biological experiments were processed statistically using Student’s t test; results were regarded as significant at p < 0.05.
Results and Discussion
Prediction of Biological Activity
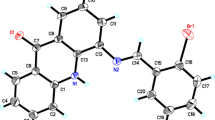
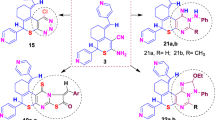
A rational approach to the search for novel biologically active substances with the necessary properties is based on computer prediction of biological activity on the basis of their structural formulas [32,33, – 34]. The computer program PASS Online [35] has now been used to predict more than 4000 types of biological activity [26]. The effectiveness of using PASS Online has been confirmed by many years of employment by 23,000 researchers from more than 100 countries around the world. Several hundred predictions of biological activity using this web service have been confirmed experimentally [36, 37]. The potential for computer prediction of biological activity suggested by this web service has significantly widened in recent years as a result of use of the Way2Drug platform [25]. The present study used in silico prediction to identify the most likely of the previously unknown types of biological activity of derivatives for the9,10-anthraquinone dithiocarbamates I – X studied here (Fig. 1) [22].
Results obtained by computer evaluation of biological activity using PASS Online are given in Table 1. As shown from the data in this Table, all compounds are predicted to be neurotransmitter reuptake inhibitors, pointing to the likely presence of anticonvulsant activity, and most compounds were predicted also to have antiviral activity.
Cytotoxicity in relation to cancer cell lines was predicted using PASS CLC-Pred (Cell Line Cytotoxicity Predictor) [27]. Analysis of the data showed (Table 2) that the most likely were interactions between the study compounds with lung, lymphoid, breast gland tissue cell lines and for some compounds also uterine cervix, brain, and large intestine cells.
Relatively low probabilities Pa in the predictions (Tables 1 and 2) may be evidence for significant novelty in the study compounds as compared with substances for which information is present in the PASS training set.
Acute toxicity LD50 was predicted for rats via four different routes of administration – i.p., i.v., p.o., and s.c. – using the online resource Acute Rat Toxicity [28]. The results (Table 3) showed that the study dithiocarbamates could be classified as intermediate-toxicity, low-toxicity, or nontoxic compounds on the classification described in [31].
Thus, computer results point to the potential for studying the antitumor, antiviral, and anticonvulsant activities of dithiocarbamate derivatives of 9,10-anthraquinones I – X. Experimental confirmation of prediction results would identify pleiotropic compounds with sets of pharmacological actions.
Biological Activities of Compounds I – X
Studies of the cytotoxic actions of compounds I – X used available cell cultures – Hep-2, CHO, HeLa, Raji, BL, and B95-8, which provided for assessment of the cytotoxicity of dithiocarbamates I – X in relation to epidermoid carcinoma, ovary, uterine cervix, and lymphoblastoid cells, effects on which were predicted by PASS CLC-Pred. This resulted in determination of the concentrations of study compounds (Table 4) suppressing cell viability by 50% (CC50). Analysis of the data in Table 4 shows that the cytotoxic effects of dithiocarbamates I – X on the test cell lines Hep-2, CHO, A549, HeLa, Raji, BL, and B85-8 confirmed the prediction data in all cases.
In particular, the study compounds displayed cytotoxicity against cultures of human throat carcinoma Hep-2 cells in the range CC50 = 0.7 – 1 μM; the most active was compound IV. Study dithiocarbamates I – X showed cytotoxic effects in cultures of CHO Chinese hamster ovary cells with CC50 = 0.4 – 19.7 μM; CHO cells were most sensitive to dithiocarbamate V. Cytotoxicity for compounds I – X in HeLa uterine cervix cell cultures gave CC50 = 0.7 – 2.8 μM, and compound V produced a cytotoxic effect at a lower concentration than the other test substances. Studies of the cytotoxicity of compounds I – X against cultures of undifferentiated human B-type lymphoblastoid cells from Burkitt’s lymphoma (Raji cells) showed that CC50 values of dithiocarbamates were in the range CC50 < 0.001 to 0.2 μM, while cultures of experimental cell line BL obtained from a patient with type B lymphoma had cytotoxicity from <0.001 to 0.5 μM. Compounds IV and X showed high cytotoxicity to Raji and BL cells with CC50 concentrations of <0.001 μM, while dithiocarbamate VI had an analogous level of cytotoxic actions only in relation to the Raji cell population.
The effects of substituents and their positions in the anthraquinone ring on the level of cytotoxic action were also studied. In the case of Hep-2 cells, changes in the location of the substituent from position 1 (compounds I – III) to position 2 (derivatives IV – VI) of the anthraquinone ring led to an increase in the cytotoxic effect. Introduction of a chlorine atom at position 3 (compounds VII and VIII) increased CC50 as compared with dithiocarbamates IV and V; the only case in which there was a decrease in the concentration elicitin 50% inhibition of this cell population compared with dithiocarbamate VI was derivative X. The following patterns were identified in the actions of study compounds on CHO cells. Movement of the diethyl fragment to position 2 led to an increase in CC50, while additional introduction of a chlorine atom had no significant effect on activity. The presence of a morpholine ring in position 2 of 9,10-anthraquinone increased the cytotoxic effect, though introduction of a chlorine atom in position 3 led to a sharp decrease. Substitution of the morpholine fragment (compound VIII) by a piperidine fragment (compound IX) increased CC50. Movement of the pyrrolidine ring to position 2 (compound VI) and introduction of an additional halogen atom (compound X) led to a significant decrease the parameter expressing cytotoxicity and, thus, an increase in cytotoxic activity. In the case of the actions of dithiocarbamates I – VI on HeLa cells, substituent positions had no significant effects on activity except for derivative V, where there was a reduction in CC50. The presence of a chlorine atom in the molecules of compounds VII and VIII significantly decreased the cytotoxic action. Results obtained with Raji cells showed the following. Compound IV, which contained a diethyl residue in position 2, was more active in terms of cytotoxicity than compounds I and VII. The presence of a pyrrolidine fragment in position 2 and introduction of a halogen into the molecule led to significant decreases in CC50. Analysis of data for BL cells showed that the presence of the diethyl fragment in positions 1 and 2 in compounds I and IV had no effect on the cytotoxic effect. The presence of a morpholine ring in compounds V and VIII led to increases in CC50, while its replacement with a piperidine residue had virtually no effect on the cytotoxic action. Of interest were results obtained in B95-8 cells with compound II, which led to elimination of 50% of the cell population from a concentration as low as 0.01 μM; this may be evidence of a direct antiviral action against Epstein-Barr virus (EBV).
Studies of the antiviral activity of dithiocarbamates I – X against strains of human adenovirus 5 serotype Ad h5 and herpes simplex types 1 (HSV-1/US) and 2 (HSV-2/BH) showed that study compounds had no antiadenovirus activity. Experiments on antiherpes activity against herpesviruses HSV-1 showed that derivative IX had minor antiviral activity. Antiviral activity against type 2 herpesvirus HSV-2 was seen with compounds V, VIII, and IX, which had actions close to that of reference agent ganciclovir (EC50 values were 75 ± 0.9, 70 ± 1.2, and 60 ± 0.8 μg/ml respectively). Compound VIII had the greatest potential: the index of selectivity was IS = 7. Studies were also run in Raji cells, which contain the Epstein-Barr virus genome in episomal form and, due to synthesis of certain oncolytic proteins, maintains the culture in the immortal state, providing a convenient model for studies of the latent form of EBV infection. Analysis of the values obtained identified compounds IV, VI, and X, which at extremely low concentrations (<0.5 μg/ml) led to elimination of virus-associated cells, such that they can be regarded as having potential for further studies for antitumor therapy. It is important to note the fact that for compounds IV and X, the effects seen here were confirmed in cell cultures obtained from a patient with B lymphoma.
As noted above, antiviral activity was predicted with low probability, which may be evidence that these compounds have significant novelty as compared with substances included in the PASS training set. Thus, comparison of prediction results with experimental data leads to the conclusion that prediction is supported in relation to antiviral activity in the study compounds without any differentiation of their actions on particular viruses (an antiadenovirus effect was predicted, but not supported on testing with the available adenovirus strains; compounds V, VIII, and IX showed activity against herpesvirus type 2, while substances IV, VI, and X showed activity against EBV, which was not predicted).
The anticonvulsant effects of anthraquinone derivatives I – X were studied using the corasol test, which is a widely used research model of generalized myoclonic convulsions in humans [38]. The dynamics of this action were studied for a dose of 100 mg/kg at early (3 and 6 h) and late (24 h) time points after single p.o. doses. These results showed that only five compounds (I, III, VI, IX, and X) had anticonvulsant effects throughout the in vivo test period. As shown in Figs. 2 and 3, studies of the anticonvulsant actions of compounds gave mean values of DCTC and DTE of 145% and 144% at 3 h post-administration and 168% and 162% at 6 h post-administration as compared with animals of the control group (100%). Thus, anthraquinone derivatives I, III, VI, IX, and X showed minor antiviral effects at the early time points. It should be noted that the antiviral action of compound III at 3 and 6 h after single p.o. doses were analogous to that of the reference agent valproic acid (200 mg/kg). The data indicate that administration of study compounds 24 h before i.v. corasol produced anticonvulsant activity, with mean DCTC and DTE of 145% and 143% respectively, which is evidence of a minor prolongation of the effect in these derivatives (Fig. 4). The effects of all compounds were less than that of valproic acid, which had DCTC and DTE values of 238% and 236% respectively. Analysis of the structure-activity interaction showed that substitution of the diethyldithiocarbamate fragment by a pyrrolidinedithiocarbamate fragment in position 1 of 9,10-anthraquinone led to an increase in anticonvulsant activity. At the same time, movement of the latter to position 2 (compound VI) and the presence of a chlorine atom in position 3 (compound X) decreased the anticonvulsant effect. Substitution of the pyrrolidine residue by a piperidine residue had no effect on the anticonvulsant properties.
Comparison of results on prediction of anticonvulsant activity with the experimental results showed that anticonvulsant activity was confirmed experimentally for compounds I, III, VI, IX, and X, which had the highest Pa values.
The results obtained from the present studies using in silico, in vitro, and in vivo methods identified that the moderately toxic 9,10-anthraquinone dithiocarbamate derivatives III, IV, VI, IX, and X are potential pharmacological substances with pleiotropic actions whose selectivities in relation to particular cell lines and different viruses are due to the features of their chemical structures, determining differences in the mechanisms of the pleiotropic actions. These studies established that the presence of cytotoxic, antiviral, and anticonvulsant actions and acute toxicity predicted using PASS Online, CLC-Pred, and Acute Rat Toxicity (Tables 1–3) on the Way2Drug platform were confirmed by in vitro and in vivo experimental results. A search based on structural similarity in the information system containing data on more than half a million actively studied pharmaceutical substances, Clarivate Analytics Integrity [39], showed that even using a threshold for the Tanimoto coefficient of similarity TC > 70% did not identify any analogs of the test compounds. As previous studies [40] have shown that at TC > 85% there is only a 30% probability that structural analogs will have the same biological activity, this result supports the novelty of the 9,10-anthraquinone dithiocarbamates studied here as noted above.
The test compounds were found to have marked cytotoxic activity against tumor cell lines Hep-2, HeLa, Raji, CHO, BL, and B95-8, while compounds II, IV, VI, and X included particularly promising compounds, as they displayed cytotoxic effects against EBV-containing tumor cells Raji and B95-8. Dithiocarbamate VIII had activity against herpesvirus type 2 HSV-2 with EC50 = 70 μg/ml with IS = 7. Studies of anticonvulsant activity using the corasol test showed that dithiocarbamate III had the greatest anticonvulsant activity in the early (3 and 6 h) and late (24 h) time points as compared with compounds I, VI, IX, and X. Assessment of acute toxicity in mice given p.o. substances showed that test compounds were moderately toxic (LD50 > 1000 mg/kg). The effects of different substituents on the types of biological activity studied here were investigated, indicating the potential for further targeted optimization of the structure and properties of substances of this class. This study was supported by the Ukrainian Ministry of Education and Science (Project No. 0118000908) and the Basic Studies Program for Scientific Research of the State Academies of Science of the Russian Federation, 2013 – 2020.
References
V. T. DeVita, T. S. Lawrence, and S. A. Rosenberg, Cancer: Principles and Practice of Oncology, Wolters Kluwer Lippincott Williams & Wilkins, Philadelphia (2011).
P. De Paoli and A. Carbone, Int. J. Cancer, 133(7), 1517 – 1529 (2013).
J. L. Kutok and F. Wang, Annu. Rev Pathol., No. 1, 375 – 404 (2006).
J. Jalouli, M. M. Jalouli, D. Sapkota, et al., Anticancer Res., 32(2), 571 – 580 (2012).
C. P. Benit and CJ. Vecht, Neuro-Oncology Practice, 3, No. 4, 245 – 260 (2016).
H. Brotz-Oesterhelt and N. A. Brunner, Curr. Opin. Pharmacol., 8(5), 564 – 573 (2008).
A. L. Hopkins, G. R. Bickerton, I. M. Carruthers, et al., Cur. Top. Med. Chem., 11(10), 1292 – 1300 (2011).
J. U. Peters, J. Med. Chem., 56(22), 8955 – 8971 (2013).
G. Housman, S. Byler, S. Heerboth, et al., Cancers,6, 3, 1769 – 1792 (2014).
H. Zahreddine and K. L. Borden, Front. Pharmacol., 4, 28 (2013).
B. Deslouches and Y. P. Di, Oncotarget, 8(28), 46635 – 46651 (2017).
V. W. C. Soo, B. W. Kwan, H. Quezada, et al. Curr. Top. Med. Chem., 17(10), 1157 – 1176 (2017).
M. Micozzi, Fundamentals of Complementary, Alternative, and Integrative Medicine, Elsevier, Riverport Lane (2018).
A. Q. Acton, Anthraquinones — Advances in Research and Application, Scholarly Editions, Atlanta (2013).
V. I. Zvarich, M. V. Stasevich, O. V. Stan’ko, et al., Pharm. Chem. J., 48(9), 584 – 588 (2014).
M. Stasevych, V. Zvarych, V. Lunin, et al., Indian J. Pharm. Sci., 77(5), 634 – 637 (2015).
M. Stasevych, V. Zvarych, V. Lunin, et al., Monatsh. Chem., 149(6), 1111 – 1119 (2018).
E. M. Malik and C. E. Muller, Med. Res. Rev., 36(4), 705 – 748 (2016).
L. M. L. Nollet and J. A. Gutierrez-Uribe, Phenolic Compounds in Food. Characterization and Analysis, CRC Press, Boca Raton (2018).
A. S. Tikhomirov, A. A. Shtil, and A. E. Shchekotikhin, Recent Pat. Anti-Cancer Drug Discov., 13, 159 – 183 (2018).
Clarivate Analytics Integrity, 2018; http: //integrity.Thomson-Pharma.com (accessed June 23, 2018).
V. Zvarych, M. Stasevych, V. Lunin, et al., Monatsh. Chem., 147(12), 2093 – 2101 (2016).
T. I. Halenova, I. V. Nikolaeva, M. V. Stasevych, et al., Res. J. Pharm. Biol. Chem. Sci., 8, 1626 – 1632 (2017).
M. Stasevych, V. Zvarych, V. Lunin., et al., SAR QSAR Environ. Res., 28(5), 355 – 366 (2017).
D. S. Druzhilovskiy, A. V. Rudik, D. A. Filimonov, et al., Rus. Chem. Bull.,66(10), 1832 – 1841 (2017).
D. A. Filimonov, D. S. Druzhilovskiy, A. A. Lagunin, et al., Biomed. Chem. Res. Meth., 1, e00004 (2018).
A. A. Lagunin, V. I. Dubovskaja, A. V. Rudik, et al., PLOS One, 13, e0191838 (2018).
A. Lagunin, A. Zakharov, D. Filimonov, et al., Mol. Inf.,30(2 – 3), 241 – 250 (2011).
T. Mosmann, Immunol. J. Meth., 65(1 – 2), 55 – 63 (1983).
M. Ahmed, Pharmacol. Pharmacy, 6, 185 – 189 (2015).
J. Švarc-Gajiæ, General Toxicology, Nova Science Publishers Inc., New York (2010).
S. M. Ivanov, A. A. Lagunin D. A. Filimonov, et al., Pharm. Chem. J., 52(8), 758 – 762 (2018).
R. K. P. Tripathi and S. R. Ayyannan, Med. Chem. Res., 27(3), 709 – 725 (2018).
V. V. Knyazev, V. S. Rogovskii, E. D. Sveshnikova, et al., Pharm. Chem. J., 52(3), 205 – 208 (2018).
A. Lagunin, A. Stepanchikova, D. Filimonov, et al., Bioinformatics, 16(8), 747 – 748 (2000).
PASS Online, 2019; http: //www.way2drug.com/PASSOnline/index.php (accessed July 15, 2019).
K. Anusevicius, V. Mickevicius, M. Stasevych, et al., Res. Chem. Intermed.,41(10), 7517 – 7540 (2015).
M. V. Nesterkina and I. A. Kravchenko, Chem. Nat. Compd.,52(2), 237 – 239 (2016).
Clarivate Analytics Integrity (2019); https://integrity.clarivate.com/(accessed July 15, 2019).
Y. C. Martin, J. L. Kofron, and L. M. Traphagen, J. Med. Chem., 45(19), 4350 – 4358 (2002).
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Khimiko-Farmatsevticheskii Zhurnal, Vol. 53, No. 11, pp. 25 – 33, November, 2019.
Rights and permissions
About this article
Cite this article
Stasevich, M.V., Zvarich, V.I., Novikov, V.P. et al. 9,10-Anthraquinone Dithiocarbamates as Potential Pharmaceutical Substances with Pleiotropic Actions: Computerized Prediction of Biological Activity and Experimental Validation. Pharm Chem J 53, 905–913 (2020). https://doi.org/10.1007/s11094-020-02098-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11094-020-02098-x