Abstract
Background: Peroxisome proliferator-activated receptor γ coactivator-1α (PGC-1α), regulated by AMPK, is an important regulator of mitochondrial fusion. At present, whether the AMPK/PGC-1α signaling pathway regulates mitochondrial dynamics in epileptic rats is still unknown. Methods: Adult male Sprague-Dawley (SD) rats were randomly divided into fourgroups: the control group (0.9% saline, n = 5), the EP groups (lithium-pilocarpine was used to induce epilepsy, and tissues were harvested at 6 and 24 h, every time point, n = 5), the EP + Compound C group (the specific inhibitor of PGC-1α, 15 mg/kg in 2% DMSO, n = 5), and the EP + DMSO group (0.9% saline + 2% DMSO, n = 5). To investigate whether PGC-1α participates in seizures by regulating the expression of mitofusin1/2(MFN1/2)in rats. Results: In this study, the behavioral results indicate that the seizure susceptibility of the rats to epilepsy was increased when the expression of PGC-1α was inhibited. Subsequently, Western blot results suggested that the expression level of both MFN1 and MFN2 in the hippocampus was higher at 6 and 24 h after an epileptic seizure. Besides, the expression of PGC-1α and MFN2 was significantly decreased in the hippocampus when the epileptic rats were treated with Compound C. Furthermore, the immunofluorescence analysis of the localization of MFN1/2 and PGC-1α showed that MFN1/2 was mainly expressed in neurons but not astrocytes in the hippocampus and cerebral cortex of rats. Meanwhile, PGC-1α colocalized with the excitatory post-synaptic marker PSD95, suggesting that PGC-1α may regulate the seizure susceptibility of the rats by mediating excitatory post-synaptic signaling. Conclusion: The AMPK/PGC-1α signaling pathway may play an important role in the lithium-pilocarpine-induced epileptic rat model by mediating the expression of fusion proteins.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Epilepsy, characterized by short, severe, and repeated neurological dysfunction, is associated with significant morbidity and mortality [1]. Up till now, nearly 70 million epileptic patients worldwide, about one-third are resistant to medical therapy [2]. Not only the quality of life but also the mental health of the epileptic patients were reduced [3, 4]. Recently, although great progress has been made in the diagnosis and treatment of epilepsy, the detailed mechanism of the occurrence and development of epilepsy still needs to be clarified [5]. We need to improve our understanding of the mechanism of epilepsy, and one such mechanistic knowledge deficit is the lack of insight into mitochondrial fusion in seizures.
The major function of mitochondria is the regulation of cellular energy metabolism, which provides most of the ATP for cellular reactions through the mitochondrial respiratory chain [6]. A dynamic network within the cell can be formed through the balance of fusion and fission of the mitochondria. Mitofusin1/2 (MFN1/2), located on the outer mitochondrial membrane, is mainly involved in regulating mitochondrial fusion [7, 8]. Disruption of the balance between mitochondrial fusion and division can lead to changes in neuronal excitability, affecting seizures [9, 10].
In the development of cardiomyopathy in PGC-1α-knockout mice, PGC-1α was shown to regulate MFN1/2 gene transcription by coactivating estrogen-related receptor alpha on conserved DNA elements [11]. It is reported that, in addition to nuclear-encoded coding genes, PGC-1α is an important regulator of the mitochondrial fusion process [12, 13]. Besides this, PGC-1α has neuroprotective effects. For example, upregulation of PGC-1α expression could protect cultured neuronal cells from oxidative stress-induced cell death [14]. However, whether PGC-1α is associated with epilepsy by mediating the regulation of mitochondrial dynamics still needs to be elucidated.
Here, a lithium-pilocarpine-induced epileptic rat model was established. Then, the specific inhibitor of PGC-1α, Compound C, was used in this model. Finally, the epileptic susceptibility and the expression of PGC-1α and MFN1/2 were observed in rats after treatment with Compound C.
Methods
Establishment of the Lithium-Pilocarpine-Induced Epileptic Seizure Rat Model
Adult male Sprague-Dawley (SD) rats weighing 200–250 g were obtained from the Experimental Animal Center of Zunyi Medical University. All experimental protocols were reviewed and approved by the Commission of Zunyi Medical University for Ethics of Experiments on Animals. The rats were maintained (five per cage) under standard animal room conditions (22–24 °C and a 12-h light/12-h dark cycle) with free access to food and water. These experiments were conducted according to the guidelines of the National Institutes of Health Guide for the Care and Use of Laboratory Animals, according to the guidelines of the World Medical Association Declaration of Helsinki. In addition, all efforts have been made to minimize the number and suffering of animals. The subsequent use of Compound C (MedChem Express, HY-13,418 A) is a selective, ATP-competitive AMPK inhibitor that also induces autophagy.
The rats were randomly divided into four groups: the control group (0.9% saline, n = 5), the EP groups (lithium-pilocarpine was used to induce epilepsy, and tissues were harvested at 6 and 24 h, every time point, n = 5), the EP + Compound C group (15 mg/kg in 2% DMSO, n = 5), and the EP + DMSO group (0.9% saline + 2% DMSO, n = 5). The lithium-pilocarpine-induced epileptic seizure rat model received an intraperitoneal injection of lithium chloride (127 mg/kg), and an injection of atropine sulfate (1 mg/kg) was administered 18–24 h later. Then, the rats were intraperitoneally injected with pilocarpine (50 mg/kg) 30 min after the administration of atropine. The rat’s total mortality is about 5% (19 alive and 1 dead in the EP group. After that, we remodeled and added to the EP group).
The rats developed stage IV or V seizure behaviors according to the Racine standard as follows [15]: stage 0, no spasm; stage I, facial myoclonus and mouth movements; stage II, head nodding; stage III, forelimb clonus; stage IV, rearing along with severe forelimb clonus; and stage V, rearing and falling. The status epilepticus (SE) was maintained for 45 min and terminated by intraperitoneal injection of atropine sulfate (1 mg/kg) and diazepam (10 mg/kg). The rats in the untreated control group received the same doses of lithium chloride and atropine sulfate but were administered 0.9% saline instead of pilocarpine. The EP + Compound C rats received an intraperitoneal injection of Compound C (15 mg/kg in 2% DMSO) and 0.9% saline when the atropine sulfate was administered [16], and the rats in the EP + DMSO group only received 2% DMSO. The EP + DMSO group and the EP + Compound C group were sacrificed after 24 h.
Immunofluorescence Staining
To confirm the subcellular localization of PGC-1α in neurons and astrocytes in the hippocampus after the seizure, the double-labeling immunofluorescence of PGC-1α in rats 24 h after seizures was performed as previously described [17]. Briefly, frozen sections were randomly selected, and the sections were incubated with a mixture of mouse anti-GFAP (1:50; Santa Cruz Biotechnology, USA, sc-71,143), rabbit anti-PGC-1α (1:50; Abcam, Cambridge, UK, ab54481) and guinea pig anti-microtubule-associated protein 2 (MAP2) (1:200, Sysy, Goettingen, Germany, 188 004) overnight at 4 °C.
The next day, the sections were incubated with a mixture of Alexa Fluor 488-conjugated goat anti-rabbit IgG (1:50, Zhongshan Golden Bridge, Inc., Beijing, China), Alexa Fluor 594-conjugated goat anti-mouse IgG (1:200, Zhongshan Golden Bridge Inc., Beijing, China), and Alexa Fluor 633-conjugated goat anti-guinea pig IgG (1:50, Abcam, Cambridge, MA, USA). Then, the sections were counterstained with DAPI (4′,6-diamidino-2-phenylindole, 1:10,000 dilution, Sigma-Aldrich, D9542) for 20 min, mounted, and sealed with 50% glycerin. In the end, the slides were observed by a laser scanning confocal microscope at 40× magnification [10].
Western Blotting
The rats were anesthetized with diazepam (10 mg/kg, Sigma-Aldrich, St. Louis, Missouri, USA), and their brains were quickly removed. Then, the hippocampus and cortex of the adjacent temporal lobe were quickly dissected and frozen. According to the manufacturer’s instructions, total protein concentrations were measured using an enhanced BCA protein assay kit (Beyotime, Haimen, China). Equal amounts of protein were separated by 10% SDS-PAGE and transferred to polyvinylidene difluoride (PVDF) membranes. After being blocked with 5% skim milk at room temperature for 1 h, the PVDF membranes were removed and incubated overnight at 4 °C with the corresponding primary antibody, including the anti-PGC-1α antibody (rabbit monoclonal antibody, 1:2,000, Abcam, ab54481), Anti-Mitofusin 1 antibody (mouse monoclonal antibody, 1:1,000 Abcam, ab57602), Anti-Mitofusin 2 antibody (rabbit monoclonal antibody, 1:5,000, Abcam, ab124773), β- tubulin (rabbit polyclonal antibody, 1:2,000, Proteintech, Inc, Rosemont, USA). β- tubulin was used as an internal control. The membranes were then incubated with HRP-conjugated secondary antibodies (1:1,000, Santa Cruz Biotechnology, CA, USA, sc-2004) at 25 °C for 1 h. Finally, the protein bands were visualized using Super Signal West Pico Chemiluminescent HRP substrate (Rockford, IL, USA). Quantity One software (Bio-Rad Laboratories, Hercules, CA, USA) was used to analyze the data.
Statistical Analysis
The Shapiro Wilke test was used to detect the normal distribution, and the Hartley test was used to test the homogeneity of variance. The data were expressed as the means ± standard deviation and were analyzed using SPSS version 18.0. The behavioral characteristics of the rats and the results of Western blot were analyzed by one-way ANOVA and Q statistics test. P < 0.05 indicated a significant difference.
Results
Effects of Compound C on the Latency and Frequency of Epileptic Seizures in Rats
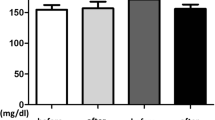
To determine the effects of Compound C on the latency and frequency of epileptic seizures in rats, we monitored the seizures in freely moving rats using behavioral observations. The latency to the first seizure was 19.35 ± 1.51 min in the EP group, 19.22 ± 1.00 min in the EP + DMSO group, and 14.91 ± 1.01 min in the EP + compound C group. The number of seizures within 1 h was 6.2 ± 0.84 in the EP group, 6.0 ± 0.71 in the EP + DMSO solvent control group, and 8.0 ± 1.22 in the EP + compound C group. There was no significant difference in the latency to the first seizure and the number of seizures within 1 h between the EP and EP + DMSO groups (P > 0.05). However, in the EP + compound C group, the latency to the first seizure was significantly reduced, the number of seizures within 1 h was increased, and the differences were statistically significant (P < 0.05) (Fig. 1). These results suggest that Compound C can significantly shorten the latency to the first seizure and increase the number of seizures in epileptic rats.
Effects of Compound C on PGC-1α and MFN1/2 Expression in Brain Tissue
Figure 2 A shows the basal level of PGC-1α expression in the normal group. The immunoblot density ratios of PGC-1α to β- tubulin in the control, EP + compound C, solvent control, and epilepsy groups (6 and 24 h) were 0.63 ± 0.02, 0.42 ± 0.03, 0.74 ± 0.03, 0.39 ± 0.01, and 0.74 ± 0.03, respectively. The expression of PGC-1α in the EP + compound C and EP-6 h groups was significantly decreased (P < 0.05) compared with that in the control group, while the expression level of PGC-1α was significantly increased in the EP-24 h group (P < 0.05).
Western blot analysis of MFN1 expression showed the expression level of MFN1 in the rat hippocampus and the immunoblot density ratios of MFN1 to β-tubulin in control, EP + compound C, solvent control, and epilepsy groups (6 and 24 h) were 0.11 ± 0.01, 0.11 ± 0.02, 0.15 ± 0.01, 0.17 ± 0.01, and 0.15 ± 0.02, respectively. The expression of MFN1 in the hippocampus in the EP + compound C group was slightly decreased (P < 0.05) compared with that in the EP + DMSO group. The expression of MFN1 in the hippocampus in the EP-6 h and EP-24 h groups was slightly increased (P < 0.05) compared with that in the control group (Fig. 2B).
The Western blot results showed that MFN2 was expressed in the rat hippocampus, and the immunoblot density ratios of MFN2 to the corresponding internal reference (β - tubulin) in control, EP + compound C, solvent control, and epilepsy groups (6 and 24 h) were 0.08 ± 0.004, 0.07 ± 0.002, 0.10 ± 0.001, 0.04 ± 0.001, and 0.09 ± 0.006, respectively. The expression of MFN2 in the EP + Compound C and EP-6 h groups was significantly decreased (P < 0.05) compared with that in the control group (Fig. 2 C).
The expression of PGC-1α (A), MFN1 (B), and MFN2 (C) in the hippocampal of the different groups were measured by immunoblot. Note: The left panel shows the Western blot image of hippocampal expression in the different groups, and the right panel shows the quantification of the data in the image shown in the left panel (* P<0.05)
Cellular Localization of PGC-1α and MFN1/2 in the Hippocampus was Measured by Immunofluorescence
The Western blot results showed that the protein expression levels of PGC-1α and MFN1/2 in the hippocampus of epileptic rats were significantly different from those of rats in the untreated control group. The expression levels of PGC-1α and MFN1/2 in the EP-24 h group were similar to the expression levels in the EP + DMSO group, and they were not significantly different from those of the solvent control group (P > 0.05). For this reason, the expression of PGC-1α and MFN1/2 in the hippocampus by immunofluorescence was measured 24 h after the seizure. The results showed that PGC-1α and MFN2 were coexpressed with the neuronal dendritic-specific marker MAP2 but not with the astrocyte-specific marker GFAP or the nuclear-specific marker DAPI in the hippocampal CA1, CA3, and DG regions in epileptic rats (Fig. 3). MFN1 was coexpressed with the neuronal dendritic-specific marker MAP2 but not with the astrocyte-specific marker GFAP in the hippocampal CA1, CA3, and DG regions in epileptic rats, and MFN1 was mainly expressed in the neuronal cell membrane (Fig. 4). To further verify how PGC-1α regulates the mitochondrial fusion protein MFN1/2, we examined the colocalization of PGC-1α with the excitatory post-synaptic marker PSD95 by immunofluorescence. Coexpression was observed in the hippocampus and the neighboring hippocampus’s temporal cortex (Fig. 5).
Discussion
AMPK is a key molecule that regulates bioenergy metabolism and can be activated by any metabolic stress that increases the AMP/ATP ratio [18]. Studies have shown that PGC-1α, which is regulated by AMPK, is involved in regulating mitochondrial respiratory genes [19]. PGC-1α interacts with transcription factors or coactivators to enhance their effects on target gene transcription. Therefore, the physiological functions of PGC-1α are mainly involved in promoting mitochondrial biogenesis and regulating glucose metabolism [20, 21]. It is also associated with neurodegenerative diseases, such as Parkinson’s disease, decreased mitochondrial damage, and mitochondrial gene expression [22]. Under hypoxic conditions, the PGC-1αnull mice have marked defects in the striatum associated with movement disorders [23]. These studies indicate that increased expression of PGC-1α reduces neuronal cell death.
The present study showed that PGC-1α expression decreased at 6 h after a seizure but increased significantly at 24 h. The change of PGC-1α expression may be related to the activation of endogenous protective mechanisms after epileptic seizures for a certain period. Furthermore, when PGC-1α expression was inhibited, the susceptibility of rats to epilepsy was increased, and the severity of epileptic seizures was exacerbated. This finding suggests that PGC-1α may be involved in epileptic seizures.
Mitochondria are double-membrane organelles that are affected by metabolic conditions, developmental stages, and environmental stimuli and have various shapes. Their dynamic morphology results from regulating the processes of fusion and division, and fusion is essential for mitochondria’s health and physiological functions [24, 25]. The fusion process is regulated by a series of proteins, including fusion protein 1/2 (mitofusin 1/2, MFN 1/2) and optic atrophy 1 (Opa1). MFN1/2 is localized on the outer mitochondrial membrane [7, 8]. The expression of MFN1 was significantly increased at 6 h after the epileptic model was established. Some studies have shown that when oxidative stress occurs in brain tissues, mitochondria actively fuse to inhibit oxidative stress, thus playing a protective role in the brain [26]; however, MFN1 expression was significantly decreased at 6 h after the seizure, which was consistent with the expression of PGC-1α. In the EP-24 h group, the expression of MFN1/2 increased significantly. We hypothesize that MFN1 and MFN2 are expressed at different times to exert synergistic effects and thus protect the brain. Besides, Compound C significantly decreased the expression of PGC-1α, and we observed that the expression of PGC-1α was consistent with the expression of MFN2. This finding is consistent with the report showing that PGC-1α mainly regulates MFN2 but not MFN1 [27]. In other words, PGC-1α may participate in epileptic seizures mainly by regulating the expression of MFN2. Also, we found that the expression of PGC-1α and MFN1/2 decreased at 72 h and 1 week compared with 24 h after the seizure, and there was no significant difference between the normal group. It may be related to the body’s self-regulation, and the specific mechanism must be further studied.
Both MFN1/2 and PGC-1α were expressed mainly in neurons but not astrocytes in the brain tissue. MFN1/2 was mainly expressed in the cytoplasm, while PGC-1α was expressed in both the cytoplasm and nucleus. Moreover, the subcellular localization of these three markers did not change significantly in epileptic conditions compared with normal conditions. This finding is consistent with previous studies showing the expression and localization of MFN1/2 and PGC-1α in mammalian brain tissue [28]. Besides, PGC-1α colocalizes with the excitatory post-synaptic marker PSD95, suggesting that PGC-1α may regulate epileptic seizures by mediating excitatory post-synaptic signaling.
The co-activation effect of PGC-1α enables it to interact with PPARγ [29]. Studies have shown that PPARγ is also expressed in neurons and can regulate epileptic seizures [30], and GW9662 (PPAR antagonist) can block the antiepileptic effect [31], which is the same as the effect of compound C in this experiment, but whether the anti-epileptic effect of PPAR and the blocking effect of GW9662 are related to the PGC-1α/PPARγ pathway needs further research to prove. In recent studies, the anti-epileptic effect of Cannabidiol has gradually been revealed. Costa et al. found that intraperitoneal injection of Cannabidiol could control epileptic seizures, and its anti-epileptic effect was related to the up-regulation of PPARγ in the hippocampal CA3 region [32], and the final effect may be related to the activation of PPARγ. It is related to the pro-inflammatory effect of inhibiting the NF-κB pathway [33]. Finally, one of the limitations of this study is that the upstream and downstream mechanisms of PGC cannot be clearly defined. Another limitation is that only behavioral assessment is used for the degree of epileptic seizures in rats, and video EEG can be used for more accurate grading [34].
Conclusion
The AMPK/PGC-1α pathway mediates the expression of fusion proteins during epileptic seizures, thereby playing a key role in regulating epileptic seizures. At present, insulin sensitizers targeting PGC-1α have been put into clinical use. Moreover, some scholars have proposed targeting MFN to improve mitochondrial structure and mitochondrial fusion to improve blood glucose homeostasis in obese patients [35]. Furthermore, some researchers have suggested targeting MFN to improve mitochondrial fusion and glucose homeostasis in obese patients. We expect that drugs targeting PGC-1α and mitochondrial fusion proteins will be used in neurology in the near future.
Data Availability
The datasets in the current study are available from the corresponding author on reasonable request.
Abbreviations
- PGC-1α:
-
Peroxisome proliferator-activated receptor γ coactivator-1α
- AMPK:
-
Adenosine 5‘-monophosphate (AMP)-activated protein kinase
- SD:
-
Sprague-Dawley
- MFN:
-
mitofusin
- EP:
-
Epilepsy
References
Mallok A, Vaillant JD, Soto MT et al (2015) Ozone protective effects against PTZ-induced generalized seizures are mediated by reestablishment of cellular redox balance and A1 adenosine receptors. Neurol Res 37(3):204–210
Thijs RD, Surges R, O’Brien TJ, Sander JW (2019) Epilepsy in adults. Lancet 393(10172):689–701
Wiglusz MS, Landowski J, Cubała WJ (2018) Prevalence of anxiety disorders in epilepsy. Epilepsy Behav 79:1–3
Katsarou AM, Moshé SL, Galanopoulou AS, INTERNEURONOPATHIES AND THEIR ROLE IN EARLY LIFE EPILEPSIES AND NEURODEVELOPMENTAL DISORDERS (2017) Epilepsia Open 2(3):284–306
Shangguan Y, Xu X, Ganbat B et al (2018) CNTNAP4 impacts Epilepsy through GABAA receptors regulation: evidence from temporal lobe Epilepsy Patients and Mouse Models. Cereb Cortex 28(10):3491–3504
Xu X, Shangguan Y, Lu S et al (2017) Tubulin β-III modulates seizure activity in epilepsy. J Pathol 242(3):297–308
Xu Z, Xu P, Chen Y et al (2015) ENT1 inhibition attenuates epileptic seizure severity via regulation of glutamatergic neurotransmission. Neuromolecular Med 17(1):1–11
Zhang Y, Gao B, Zheng F et al (2017) The phosphodiesterase 10A inhibitor PF-2545920 enhances hippocampal excitability and seizure activity involving the Upregulation of GluA1 and NR2A in post-synaptic densities. Front Mol Neurosci 10:100
Zhao Y, Li X, Zhang K, Tong T, Cui R (2018) The Progress of Epilepsy after Stroke. Curr Neuropharmacol 16(1):71–78
Luo Z, Wang J, Tang S et al (2020) Dynamic-related protein 1 inhibitor eases epileptic seizures and can regulate equilibrative nucleoside transporter 1 expression. BMC Neurol 20(1):353
Yang L, Long Q, Liu J et al (2015) Mitochondrial fusion provides an ‘initial metabolic complementation’ controlled by mtDNA. Cell Mol Life Sci 72(13):2585–2598
Venditti P, Di Meo S (2020) The role of reactive oxygen species in the life cycle of the Mitochondrion. Int J Mol Sci. 21(6):2173
Adán Areán JS, Vico TA, Marchini T et al (2021) Energy management and mitochondrial dynamics in cerebral cortex during endotoxemia. Arch Biochem Biophys 705:108900
Bertholet AM, Delerue T, Millet AM et al (2016) Mitochondrial fusion/fission dynamics in neurodegeneration and neuronal plasticity. Neurobiol Dis 90:3–19
Bulavin DV, Phillips C, Nannenga B et al (2004) Inactivation of the Wip1 phosphatase inhibits mammary tumorigenesis through p38 MAPK-mediated activation of the p16(Ink4a)-p19(arf) pathway. Nat Genet 36(4):343–350
Tang S, Luo Z, Qiu X et al (2017) Interactions between GHRH and GABAARs in the brains of patients with epilepsy and in animal models of epilepsy. Sci Rep 7(1):18110
Garcia D, Shaw RJ (2017) AMPK: mechanisms of Cellular Energy Sensing and Restoration of metabolic balance. Mol Cell 66(6):789–800
Sada N, Lee S, Katsu T, Otsuki T, Inoue T (2015) Epilepsy treatment. Targeting LDH enzymes with a stiripentol analog to treat epilepsy. Science 347(6228):1362–1367
Scharfman HE (2015) Neuroscience. Metabolic control of epilepsy. Science 347(6228):1312–1313
Rousset CI, Leiper FC, Kichev A et al (2015) A dual role for AMP-activated protein kinase (AMPK) during neonatal hypoxic-ischaemic brain injury in mice. J Neurochem 133(2):242–252
Kuczynska Z, Metin E, Liput M, Buzanska L (2021) Covering the Role of PGC-1α in the nervous system.Cells. 11(1):111
Russo E, Andreozzi F, Iuliano R et al (2014) Early molecular and behavioral response to lipopolysaccharide in the WAG/Rij rat model of absence epilepsy and depressive-like behavior, involves interplay between AMPK, AKT/mTOR pathways and neuroinflammatory cytokine release. Brain Behav Immun 42:157–168
Scarpulla RC (2008) Transcriptional paradigms in mammalian mitochondrial biogenesis and function. Physiol Rev 88(2):611–638
Lowell BB, Spiegelman BM (2000) Towards a molecular understanding of adaptive thermogenesis. Nature 404(6778):652–660
Lin J, Wu PH, Tarr PT et al (2004) Defects in adaptive energy metabolism with CNS-linked hyperactivity in PGC-1alpha null mice. Cell 119(1):121–135
St-Pierre J, Drori S, Uldry M et al (2006) Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivators. Cell 127(2):397–408
Martin OJ, Lai L, Soundarapandian MM et al (2014) A role for peroxisome proliferator-activated receptor γ coactivator-1 in the control of mitochondrial dynamics during postnatal cardiac growth. Circ Res 114(4):626–636
Tsunemi T, La Spada AR (2012) PGC-1α at the intersection of bioenergetics regulation and neuron function: from Huntington’s disease to Parkinson’s disease and beyond. Prog Neurobiol 97(2):142–151
Viswakarma N, Jia Y, Bai L et al (2010) Coactivators in PPAR-Regulated Gene Expression. PPAR Res. 2010:250126
Huang JB, Hsu SP, Pan HY et al (2020) Peroxisome Proliferator-Activated Receptor γ Coactivator 1α Activates Vascular Endothelial Growth Factor That Protects Against Neuronal Cell Death Following Status Epilepticus through PI3K/AKT and MEK/ERK Signaling. Int J Mol Sci. 21(19):7247
Lucchi C, Costa AM, Giordano C et al (2017) Involvement of PPARγ in the anticonvulsant activity of EP-80317, a ghrelin receptor antagonist. Front Pharmacol 8:676
Costa AM, Russo F, Senn L, Ibatici D, Cannazza G, Biagini G (2022) Antiseizure Effects of Cannabidiol leading to increased peroxisome proliferator-activated receptor gamma levels in the hippocampal CA3 subfield of epileptic rats. Pharmaceuticals (Basel). 15(5):495
Mori MA, Meyer E, da Silva FF, Milani H, Guimarães FS, Oliveira R (2021) Differential contribution of CB1, CB2, 5-HT1A, and PPAR-γ receptors to cannabidiol effects on ischemia-induced emotional and cognitive impairments. Eur J Neurosci 53(6):1738–1751
Costa AM, Lucchi C, Simonini C, Rosal L, Biagini G (2020) Status Epilepticus Dynamics predicts latency to spontaneous seizures in the Kainic Acid Model. Cell Physiol Biochem 54(3):493–507
Racine RJ (1972) Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol 32(3):281–294
Funding
This work was supported by grants from the National Natural Science Foundation of China (No: 81660227), the Collaborative Innovation Center of Chinese Ministry of Education (No: 2020-39), the Guizhou provincial “hundred” level innovative talents funds (No: GCC-2022-038-1), the Guizhou Provincial Science and Technology Foundation (No: ZK2022-656),and the Zunyi City Science and Technology Foundation (No: 2019-71 and 2021-30 ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All experimental procedures were reviewed and approved by the Ethics of experiments on Animals Commission of Zunyi Medical University.
Consent for Publication
Not Applicable.
Competing Interests
The authors declared no conflicts of interest concerning this article’s research, authorship, funding, and/or publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dongxu Li, Linhai Zhang contributed equally to this article.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, D., Zhang, L., Tuo, J. et al. PGC-1α Affects Epileptic Seizures by Regulating Mitochondrial Fusion in Epileptic Rats. Neurochem Res 48, 1361–1369 (2023). https://doi.org/10.1007/s11064-022-03834-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-022-03834-3