Abstract
Neuroinflammation and imbalance of neurotransmitters play pivotal roles in seizures and epileptogenesis. Aucubin (AU) is an iridoid glycoside derived from Eucommia ulmoides that possesses anti-inflammatory and neuroprotective effects. However, the anti-seizure effects of AU have not been reported so far. The present study was designed to investigate the effects of AU on pilocarpine (PILO) induced seizures and its role in the regulation of neuroinflammation and neurotransmission. We found that AU reduced seizure intensity and prolonged the latency of seizures. AU significantly attenuated the activation of astrocytes and microglia and reduced the levels of interleukine-1 beta (IL-1β), high mobility group box 1 (HMGB1), tumor necrosis factor-α (TNF-α). Furthermore, the contents of γ-aminobutyric acid (GABA) were increased while the levels of glutamate were decreased in the hippocampus with AU treatment. The expression of γ-aminobutyric acid type A receptor subunit α1 (GABAARα1) and glutamate transporter-1 (GLT-1) protein were up-regulated in AU treatment group. However, AU had no significant effect on N-methyl-d-aspartate receptor subunit 2B (NR2B) expression in status epilepticus (SE). In conclusion, our findings provide the first evidence that AU can exert anti-seizure effects by attenuating gliosis and regulating neurotransmission. The results suggest that AU may be developed as a drug candidate for the treatment of epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy a common neurological disorders that is characterized by spontaneous recurrent seizures due to excessive synchronous discharge from brain neurons [1]. There are approximately 70 million people worldwide who are suffering from epilepsy [2]. Although the majority of patients with epilepsy have achieved seizure remission with antiepileptic drugs (AEDs), about 30% of patients are still not effectively controlled with available drugs [3]. In addition, adverse drug reactions caused by AEDs can greatly reduce the quality of life of patients [3, 4]. Thus, it’s urgent to understand the molecular mechanisms of epileptogenesis and develop novel antiepileptic agents to modify the epileptic process.
The pathogenesis of epilepsy is complex [5], though the theory implicating an imbalance between excitatory and inhibitory transmitters is widely recognized [6]. Glutamate is the primary excitatory neurotransmitter in the brain [7], and excessive glutamate in the synaptic cleft induces excitotoxicity via activated N-methyl-d-aspartate receptors (NMDAR), which promote calcium influx and subsequent neuronal death [8]. Extracellular glutamate is mainly taken up via the excitatory amino acid transporter (EAAT2/GLT-1) in astrocytes [9]. As such, suppression of NMDAR activity and enhancement of glutamate uptake could be an effective way to inhibit the occurrence of epilepsy. γ-aminobutyric acid (GABA) is the principal inhibitory neurotransmitter [7] and it exerts a postsynaptic inhibitory action mainly via GABAA receptors [10]. Importantly, enhanced GABAARα1 expression can increase the seizure threshold and inhibit the development of recurrent spontaneous seizures after status epilepticus (SE), suggesting that GABAARα1 functions as an inhibitory factor in the occurrence of epilepsy [11]. These findings indicated that GABAAR-mediated inhibitory neurotransmission is a therapeutic target for epilepsy.
Neuroinflammation is characterized by reactivity of astrocytes and microglia [12]. The inflammation response, astrocytosis and microglial activation were observed in the brain tissues from patients with temporal lobe epilepsy (TLE). The same pathological phenomenon was also observed in various animal models of epilepsy [13]. As a brain injury factor, epileptic seizures could induce the resting state of astrocytes and microglia into activated form once it attacks [14]. Activation of astrocytes and microglia releases various inflammatory molecules, mainly interleukine-1 beta (IL-1β), high mobility group box 1 (HMGB1), tumor necrosis factor-α (TNF-α). In turn, several studies have shown that these inflammatory factors could promote seizures and epileptogenesis [15,16,17]. Currently, several anti-inflammatory or immunosuppressive drugs are being used to control seizures in some patients with epileptic syndromes that are resistant to conventional AEDs [18]. For example, intravenous immunoglobulin (IVIG) can suppress seizures in some types of intractable epilepsy [19] by reducing the levels of cytokines and suppressing the activation of astrocytes [20, 21]. Moreover, a recent study found that treatment with the IL-1β synthesis inhibitor VX-765 or the IL-1 receptor antagonist IL-1RA could reduce the onset of seizures and inhibit the augmentation of epileptogenesis in various animal models of epilepsy [22]. The above evidence suggests that suppression of neuroinflammatory pathways is a potential target for the treatment of refractory epilepsy.
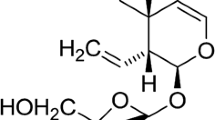
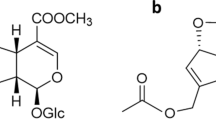
Aucubin (AU) is a natural monomeric compound, that is typically acquired from Eucommia ulmoides Oliv, a small tree native to China [23]. AU demonstrates anti-inflammatory and neuroprotective effects, although various pharmacological effects have been reported [24]. There are several reports suggest that AU can inhibit the activation of extracellular signal-regulated kinase (ERK), the degradation of κBa (IκBα) and activation of nuclear factor κB (NF-κB) to antagonize various inflammatory cytokines, including interleukin-1β (IL-1β), IL-6 and TNF-α [25,26,27]. In recent years, the study on the potential pharmacological effects of AU on the nervous system has also become a hot spot. Our previous study demonstrated that AU ameliorated epilepsy-induced hippocampal neuronal damage by inducing autophagy and inhibiting necroptosis in lithium-pilocarpine-induced rat model of SE [28]. Recent studies have also shown that AU facilitates the differentiation of neural precursor cells into GABAergic neurons, promotes neurite outgrowth in neural stem cells, and enhances lengthening and thickness of axons and re-myelination 3 weeks after sciatic nerve injury, suggesting that AU might improve neurodegenerative disorders and peripheral nerve injury by promoting nerve growth and regeneration [29, 30]. However, the effect of AU on epileptic seizures has not been fully explored. Whether AU can regulate neuroinflammation and neurotransmitters remains unknown. Therefore, the purpose of this study was to investigate the anti-epileptic effect of AU and its potential mechanism. Based on these background information, we are committed to investigate whether AU reduces seizures and whether its action is related to the inhibition of neuroinflammation and the regulation of neurotransmitters. An epileptic mouse was used to observe changes in animal behavior following AU treatment and to assess the activation of glial cells, the expression of inflammatory factors, and the content of glutamate and GABA in the hippocampus.
Materials and Methods
Animals
Male ICR mice (6 weeks old, weighing 18–22 g) were provided by Hunan SJA Laboratory Animal Co. Ltd. The mice were housed in a controlled environment at 20–22 °C, 12 h light and dark cycles, with food and water ad libitum. All experimental protocols were approved by the Ethics Committee of Central South University and were carried out in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals (NIH Publications NO. 80 − 23, revised 1996). All possible efforts were made ensure the animals comfort and to minimize the number of animals used.
Grouping and Treatment
Mice were randomly divided into five groups of eight animals each. All treatments were given via an intraperitoneal (i.p.) route in a volume of 10 ml/kg and include the (1) normal control group (NC, 0.9% normal saline, i.p.), (2) epileptic model group (PILO, 320 mg/kg, i.p.), (3) AU low-dose group (AU-L, 50 mg/kg, i.p.), (4) AU high-dose group (AU-H, 100 mg/kg, i.p.); (5) Sodium valproate group (VPA ,300 mg/kg, i.p.). The drugs were dissolved in saline to prepare for injection. The AU was extracted from the Eucommia ulmoides Oliv in our laboratory, the purity of which was more than 98%. The extraction technology we first established was awarded a patent of Chinese national invention in 2015, No. 201410376884.0, State Intellectual Property Office, P. R. China. Mice in the treatment groups were administered once daily for 7 days. Pilocarpine was used to induce seizures at 30 min after the last administration of AU.
Induction of Status Epilepticus
Animals were subjected to the LiCl-pilocarpine model of SE. Briefly, the mice were treated intraperitoneally with lithium chloride (LiCl, 127 mg/kg, i.p., Sigma–Aldrich, USA) 12–18 h prior to the administration of pilocarpine (320 mg/kg, i.p., Sigma–Aldrich, USA). Mice were injected 30 min prior to the pilocarpine hydrochloride injection with scopolamine methylbromide (1 mg/kg, i.p., National Institutes for Food and Drug Control, China) to minimize peripheral cholinomimetic effects. Behavioral changes were recorded and graded according to the Racine scale [31]: 0, no abnormality; 1, mouth and facial movements; 2, head nodding; 3, forelimb clonus; 4, rearing and bilateral forelimb clonus; 5, rearing, falling and jumping; 6, death. The beginning of SE was defined as the onset of continuous stage 4 or 5 seizures or multiple stage 4/5 seizures without regaining normal behavior between seizures. SE was allowed to last for 60 min and then 10% chloral hydrate (3 ml/kg) was injected to terminate the seizures. The seizure scores and the latency of the seizures were recorded. The seizure latency was defined as the time from injection of pilocarpine to the first appearance of seizure activity. Mice were sacrificed by cervical dislocation or 10% chloral hydrate at 24 h after SE. The brain was collected forimmunohistochemical analysis. The dissociated hippocampus was obtained for assessing neurotransmitters levels and/or western-blot analysis.
Immunohistochemical Analysis
The activation of astrocytes and microglia was measured via immunohistochemistry analysis of glial fibrillary acidic protein (GFAP) and ionized calcium binding adapter molecule 1(Iba1). The animals were anesthetized and perfused transcardially with ice-cold phosphate buffer solution (PBS, 0.01 M, pH 7.4) followed by a chilled 4% (w/v) paraformaldehyde at 15 ml/min for 5 min. The brains were carefully removed after perfusion and postfixed overnight in 4% paraformaldehyde at 4 °C. Coronal sections through the dorsal hippocampus were obtained and used for immunohistochemical analysis. After dewaxing and hydration, the sections were incubated in a 3% hydrogen peroxide solution for 30 min. Antigen retrieval was carried out under boiling conditions. The sections were incubated in goat serum for 2 h to block the antigens and then incubated overnight at 4 °C with mouse monoclonal anti-GFAP (1:50, CST, USA) and Rabbit monoclonal anti-Iba1 (1:8000, Abcam, USA). The following day the sections were washed and incubated for 1 h with either Biotin-labeled Goat Anti- Mouse IgG (H + L) (1:2000, Beyotime Biotechnology, China) or Biotin-labeled Goat Anti- Rabbit IgG (H + L) (1:500, Beyotime Biotechnology, China). After rinsing three times with PBS, a DAB kit (Zsbio, China) was used to visualize the sites of antibody binding. Sections were observed under a microscope (Nikon Eclipse Ci, Japan) and pictures were taken (Nikon DS-U3, Japan) at 400x magnification. Ten random fields per specimen were analyzed automatically and semi-quantitatively using Image Pro Plus 6.0 pathology image analysis software. The same regions were fixed across all the images to calculate the area and integrated optical density (IOD). The IOD/area of the target protein was obtained for each image.
Western Blot Analysis
The hippocampus was dissected on ice, preserved in liquid nitrogen and then homogenized in ice-cold PBS buffer and then added RIPA lysis buffer (Beyotime, China) containing phenylmethanesulfonyl fluoride (PMSF; Beyotime, China) and phosphatase inhibitors (Servicebio, Switzerland). The concentration of protein in the supernatant was detected via BCA assay (BCA Protein Assay Kit, Beyotime Biotechnology). The protein extracts were then separated via sodium dodecyl sulfate–polyacrylamide gel electrophoresis and transferred onto a polyvinylidene difluoride (PVDF) membrane (Millipore, USA). The PVDF membrane was blocked in newly prepared TBST buffer (Trisbuffered saline solution containing 0.05% Tween-20) supplemented with 5% skim milk for 1 h at ambient temperature. The membrane was then cut into multiple target bands and incubated with mouse anti-GFAP antibody (1:1000, CST, USA), rabbit anti-Iba1 antibody (1:1000, Abcam, USA), rabbit anti-HMGB1 antibody (1:500, ImmunoWay, USA), rabbit anti-IL-1β antibody (1:500, Milipore, USA), mouse anti-TNF-α antibody (1:500, Proteintech, USA), or mouse anti-GABARα1 antibody (1:500, Proteintech, USA), mouse anti-NR2B antibody (1:500, Abcam, USA), rabbit anti-GLT-1 antibody (1:1000, Proteintech, USA), mouse anti-β-actin antibody (1:500, Santa Cruz, USA) in TBST buffer overnight at 4 °C. The membrane was then incubated with HRP-labeled Goat Anti-Rabbit IgG (H + L) (1:1000, Beyotime Biotechnology, China) or HRP-labeled Goat Anti-Mouse IgG (H + L) (1:1000, Beyotime Biotechnology, China) for 1 h. Immunoreactive bands were visualized using Amersham ECL Prime Western Blotting Detection Reagent (GE, USA). Quantitative analysis of the gray value of the bands using Image J software (National Institutes of Health, USA).
Biochemistry Detection
For the determination of glutamate and GABA levels in the hippocampus tissues, the tissues were homogenized in ice-cold PBS buffer and centrifuged at 12,000 rpm for 10 min at 4°. The supernatant was used in the subsequent assays. The content of GABA was measured using an ELISA Kit for Gamma-Aminobutyric Acid(Cloud-Clone Corp. USA) in accordance with the manufacturer’s instructions. Briefly, the sample was added into the prepared Detection Reagent A and incubated for 1 h at 37°. After washing off the unbound conjugate, Detection Reagent B was added to each microplate well and incubated for 30 min at 37 °C. The substrate solution and stop solution were used for color development reaction and termination, respectively, and absorbance was measured at 450 nm using a microplate reader (Beckman Coulter, USA). Each experiment was repeated three times. The concentration of glutamate in the hippocampus was assessed via an ultraviolet colorimetry method according to the instruction of Glutamic acid measurement kit (Nanjing Jiancheng Bioengineering Institute, China).
Statistical Analysis
All results were expressed as the Mean ± Standard Error of the Mean(SEM). The seizure score was analyzed using the Kruskal–Wallis test. The mortality rate was analyzed via the Chi-squared test. Other data were determined using one-way ANOVA tests, followed by Tukey tests for multiple comparisons with SPSS 18.0 software (SPSS Inc., USA). A value of p < 0.05 was considered statistically significant.
Results
AU Alleviates Li-Pilocarpine-Induced Seizure Activity
Behavioral testing was performed to evaluate the anticonvulsive effects of AU in Li-pilocarpine-induced seizure model. Statistical analysis revealed that pretreatment with high doses of AU could reduce seizure intensity (Fig. 1a, p < 0.05) and also prolong the latency for the onset of seizures (Fig. 1b, p < 0.05). However, low-doses of AU did not display a protective effect. The VPA group had a lower seizure score (Fig. 1a, p < 0.05) and a longer latency than the PILO group (Fig. 1b, p < 0.05). The mortality rate in the PILO group was 75.0%, however, the mortality rate in this group dropped to 12.5% following high-dose AU treatment (Fig. 1c, p < 0.05). These findings suggest that the high dose of AU has an anti-epileptic activity.
AU alleviates LiCl-pilocarpine-induced seizure activity. a Indicates seizure scoring. b Indicates latency to the first convulsion. c Indicates percentage mortality. NC normal control group (0.9% normal saline), PILO epileptic model group (Pilocarpine), AU Aucubin, VPA sodium valproate. AU-L AU-L + PILO, AU-H AU-H + PILO, VPA VPA + PILO. Values for percentage mortality are expressed in percentage. PILO 320 mg/Kg, AU 50,100 mg/Kg, VPA 300 mg/Kg, n = 8. Compared with PILO group, *, **, *** p < 0.05, 0.01, 0.001
AU Inhibits Activation of Astrocytes and Microglia
Activation of astrocytes and microglia was observed in the hippocampus of Li-pilocarpine treated animals, as assessed using anti-GFAP and anti-Iba1 antibodies. The number of GFAP and Iba1 labelled cells were increased in the hippocampal CA1 and CA3 regions of Li-pilocarpine treated animals, suggesting that epileptic seizures could result in gliosis (Fig. 2a–f, p < 0.05). Morphologically, the activated astrocytes and microglia in the hippocampal region of the Li-pilocarpine treated animals displayed clear signs of hypertrophy. A small number of reactive astrocytes were found in the control animals. In contrast, GFAP immunoreactivity was enhanced by 1.3-fold in the hippocampus regions of the PILO and VPA groups (Fig. 2c, p < 0.05). Quantification of Iba1 immunoreactivity also demonstrateda1.3-fold increase in the hippocampus regions of the PILO and VPA groups (Fig. 2f, p < 0.05). However, pretreatment with AU 100 mg/kg significantly decreased the activation of astrocytes and microglia, as based on their morphology and quantificative analysis compared to the PILO and VPA groups (Fig. 2, p < 0.05). A significant increase in GFAP and Iba1 protein was also observed in the hippocampus of the PILO and VPA groups compared to the control group, as based on Western-blot analyses (Fig. 2g–i, p < 0.05). However, pretreatment with 100 mg/kg AU resulted in a significant decrease in hippocampal GFAP and Iba1 protein levels compared to the PILO and VPA groups (Fig. 2g–i, p < 0.05). These findings suggest that the high dose of AU could inhibit the activation of astrocytes and microglia in pilocarpine-induced SE.
AU inhibits activation of astrocytes and microglia. a, b The GFAP immunoreactivity in the hippocampal CA1 and CA3 regions. c Quantitative expression of GFAP immunoreactivity. d, e The Iba1 immunoreactivity in the hippocampal CA1 and CA3 regions. f Quantitative expression of Iba1 immunoreactivity. Values are mean ± SEM(n = 4). g The expression levels of GFAP and Iba1 protein were analyzed via Western blot. h, i The semi-quantitative analyses for Western blot in panel. Values are mean ± SEM (n = 3). AU-L AU-L + PILO, AU-H AU-H + PILO, VPA VPA + PILO. PILO 320 mg/Kg, AU 50,100 mg/Kg, VPA 300 mg/Kg. Compared with PILO group, *,**,*** p < 0.05, 0.01, 0.001
AU Reduces the Levels of Proinflammatory Cytokines
Inflammatory cytokines are released from astrocytes and microglia after seizures. To determine whether AU can reduce the production of proinflammatory cytokines, the levels of IL-1β, HMGB1 and TNF-α protein in the hippocampus were detected by Western-blot analysis. We found that pilocarpine treatment significantly increased IL-1β, HMGB1 and TNF-α levels in the hippocampus (Fig. 3, p < 0.05). Moreover, pretreatment with VPA did not reduce the expression of the above inflammatory factors. However, treatment of AU showed a significant reduction in the levels of these cytokines, suggesting that AU could reduce the seizure-induced inflammatory response.
AU reduces the levels of proinflammatory cytokines. a The expression levels of IL-1β, HMGB1 and TNF-α protein were analyzed via Western blot. b, c, d The semi-quantitative analyses for Western blot in panel. AU-L AU-L + PILO, AU-H AU-H + PILO, VPA VPA + PILO. Values are mean ± SEM (n = 3). PILO 320 mg/Kg, AU 50,100 mg/Kg, VPA 300 mg/Kg. Compared with PILO group, *, **, *** p < 0.05, 0.01, 0.001
AU Increases the GABA Levels and Decreases the Glutamate Levels
The imbalance between neuronal excitation and inhibition due to a decrease in GABAergic and/or an increase in glutamatergic transmission are responsible for the occurrence of epileptic seizures. To address the possibility that AU regulates the levels of amino acid neurotransmitters, glutamate and GABA were detected via colorimetry or ELISA. Treatment with pilocarpine increased the content of glutamate in the hippocampus (Table 2; Fig. 4b, p < 0.05), in contrast, GABA levels were decreased in the hippocampus of pilocarpine-induced epileptic animals (Table 1; Fig. 4a, p < 0.05). Pretreatment with 100 mg/kg of AU and 300 mg/kg of VPA significantly abolished these increased glutamate level and the decreased GABA levels induced by pilocarpine (Fig. 4, p < 0.05). These results revealed that AU could serve to correct the balance between glutamate and GABA in the hippocampus, which might contribute to the anti-seizure effect of AU treatment.
AU increases the GABA levels and decreases the glutamate levels. a The content of GABA in NC, PILO, AU-L, AU-H and VPA-treated groups. b The content of glutamate in NC, PILO, AU-L, AU-H and VPA-treated groups. AU-L AU-L + PILO, AU-H AU-H + PILO, VPA VPA + PILO. Values are mean ± SEM (n = 6). PILO 320 mg/Kg, AU 50,100 mg/Kg, VPA 300 mg/Kg. Compared with PILO group, *, **, *** p < 0.05, 0.01, 0.001
AU Upregulates the Expression of the GABAARα1 Protein
Glutamate acts on NMDAR to induce postsynaptic depolarization, which is essential for neuronal excitability and GABAAR is crucial for GABA-mediated inhibition. Therefore, the effect of AU on the expression of these receptors was also investigated. As shown in Fig. 5b, injection of pilocarpine downregulated the expression of the GABAARα1 protein. In contrast, there was a significant increase in expression of GABAARα1 in the hippocampus in the high-dosage AU group compared with the PILO group (Fig. 5b, p < 0.05). However, NR2B was not significantly affected by AU or VPA compared with the PILO group (Fig. 5c). Thus, the anti-epileptic effect of AU could be related to the upregulation of GABAARα1.
AU upregulates the expression of GABAARα1 protein. a The expression levels of GABAARα1 and NR2B protein were analyzed via Western blot. b, c The semi-quantitative analyses for Western blot in panel. AU-L AU-L + PILO, AU-H AU-H + PILO, VPA VPA + PILO. Values are mean ± SEM (n = 3). PILO 320 mg/Kg, AU 50,100 mg/Kg, VPA 300 mg/Kg. Compared with PILO group, *, **, *** p < 0.05, 0.01, 0.001
AU Upregulates the Expression of GLT-1
GLT-1 is the most prominent glutamate transporter expressed in the mammalian brain and is responsible for removing glutamate from the extracellular space (ECS). To investigate whether AU could promote the clearance of glutamate, we analyzed the expression of GLT-1 in the hippocampus. Western-blot analysis revealed that pilocarpine treatment resulted in decreased levels of GLT-1 in the hippocampus (Fig. 6, p < 0.05). Importantly, a significant increase in hippocampal GLT-1 protein levels was apparent in the AU-H and VPA groups compared to the pilocarpine treated animals (Fig. 6, p < 0.05). These results indicated that AU might enhance the clearance of extracellular glutamate to exert its antiepileptic effect.
AU upregulates the expression of GLT-1 protein. a The expression levels of GLT-1 protein were analyzed via Western blot. b The semi-quantitative analyses for Western blot in panel. AU-L AU-L + PILO, AU-H AU-H + PILO, VPA VPA + PILO. Values are mean ± SEM (n = 3). PILO 320 mg/Kg, AU 50,100 mg/Kg, VPA 300 mg/Kg. Compared with PILO group, *, **, *** p < 0.05, 0.01, 0.001
Discussion
AU is an important bioactive constituent of E. ulmoides [32], and is used in folk and traditional Chinese medicine. AU exhibits multiple pharmacological effects, including anti-inflammation, anti-oxidant, and anti-apoptosis [24]. Although few studies concerning the effects of AU on the nervous system have been reported, some studies have shown that AU has neuroprotective effects. AU inhibits the loss of hippocampal neurons in the CA1 sub-region to alleviate cognitive dysfunction in a rat model of diabetic encephalopathy [33]. Our previous study also demonstrated that AU could attenuate epilepsy-induced hippocampal damage by inducing autophagy and suppressing necroptosis [28]. In the present study, we assessed the effects of AU treatment in an epileptic mouse model and found that AU could reduce seizure activity, inhibit gliosis and neuroinflammatory cytokines, and regulate the levels of neurotransmitters in the hippocampus.
Pilocarpine-induced SE is the most widely used model of TLE, as this model can reproduce spontaneous recurrent seizures, extensive brain structure and cellular damage, and is resistant to current antiepileptic drugs [34]. Pilocarpine acts on the M1 muscarinic and NMDA receptors to trigger or maintain seizures [35]. Lithium pre-treatment lowers the mortality rate associated with pilocarpine treatment, and also reinforce the epileptogenic action of pilocarpine [36]. In the present study, the Li-pilocarpine model of epilepsy was treated with AU, and it was observed that AU could reduce the intensity of the seizures and lengthen the latency to the onset of SE in these mice. Moreover, AU significantly reduced the mortality of the pilocarpine treated animals. These findings indicated that AU might inhibit SE or complex partial seizures.
Over the last decade, preclinical and clinical evidence has demonstrated that epileptic seizures can provoke inflammatory responses and activate glial cells. Immunohistochemical analysis of brain tissues from animal models of epilepsy or patients with drug-resistant epilepsy has shown the activation of glial cells and the accumulation of multiple inflammatory cytokines including IL-1β, HMGB1 and TNF-α [37,38,39,40]. Our present study also found that pilocarpine treatment induced the proliferation and activation of astrocytes and microglia in the hippocampus after SE. The expression of GFAP and Iba1 was increased after SE, moreover, the levels of IL-1β, HMGB1 and TNF-α were significantly increased in the hippocampus of pilocarpine-treated animals. Previous reports have indicated that glia cells participate in modulating diverse neuronal functions, including the modulation of synaptic function and plasticity, buffering neurotransmitter and ion to mediate the extracellular microenvironment, maintain the integrity of the Blood Brain Barrier (BBB) [41, 42], and regulation of the cellular immunity to participate in restore and healing [43]. These physiological functions of normal glia help maintain tissue homeostasis, but disruption of glial functions may cause seizures or promote epileptogenesis [44]. Reactive astrocytes reduce glutamate uptake in the ECS, which decreases the threshold for inducing seizures and increase epileptic hyperexcitability. Reactive astrocytes can also downregulate glutamine synthetase (GS) expression, which reduces the synthesis of neuronal GABA and helps trigger the onset of seizures [45]. Besides regulating neuronal excitability, activated astrocytes can also release a large number of pro-inflammatory cytokines, such as IL-1β and HMGB1 [46]. These cytokines activate the IL1R/TLR system, which reduces the seizure threshold to promote seizure onset and recurrence [47]. The activation of IL1R/TLR also stimulates Src-kinase-mediated phosphorylation of the GluN2B subunit of the NMDA receptor, which enhances the NMDAR-mediated excitability to induce further seizures [48]. Microglia are integral to inflammatory processes in experimental models and human epilepsy [47, 49]. On the one hand, activated microglia can promote astrocytes; on the other hand, microglia cooperate with astrocytes to promote the release of pro-inflammatory factors, such as TNF-α [50, 51], which in turn promotes astrocytic glutamate release thereby contributing to cell loss and seizures [49]. TNF-α can also promote the endocytosis of GABA-A receptors, therefore decreasing inhibitory strength and reinforcing excitability [52]. Notably, the extent of microglial activation correlates with seizure frequency and disease duration in these drug-resistant epilepsies [53]. Therefore, neuroinflammation plays a vital role in the pathogenesis of epilepsy. As such, it may be beneficial to reduce inflammation in the brain of patients with epilepsy, which may serve to reduce brain damage and improve neuronal function. Growing evidence has demonstrated that AU dramatically attenuates inflammatory responses to improve various disease conditions, including acute pulmonary injury, osteoarthritis and obesity-induced atherosclerosis [54,55,56]. In addition, AU can inhibit hippocampal neuronal death to retard cognitive impairment in a rat model of diabetic encephalopathy [57]. Moreover, our previous studies have demonstrated that AU has protective effects on hippocampal neurons in PILO-induced epileptic rats [28]. In the present study, the effects of AU on inflammation were studied in pilocarpine-treated animals. A significant decrease in the number of activated astrocytes and microglia was observed following AU treatment, suggesting that AU attenuates seizure-induced gliosis. Treatment of the pilocarpine-treated animals with AU also reduced the protein levels of IL-1β, HMGB1 and TNF-α. These results suggested that the anti-epileptic effect of AU might be achieved by suppressing neuroinflammation. However, administration of VPA to the pilocarpine-treated animals had no effect on the inhibition of the activation of astrocyte and microglia. In addition, VPA did not suppress IL-1β, HMGB1 or TNF-αexpression. A prior study has indicated that VPA can induce microglial activation in an in vitro astroglia/microglia co-culture model [13]. Another study has shown that VPA is unable to reduce the expression of IL-1β and TNF-α expression in pentylenetetrazol or pilocarpine-induced seizures [58]. Our results are in line with these previous findings, suggesting that VPA is unsuitable for reducing inflammatory conditions in the development of chronic epilepsy. These might be the reason why VPA has no benefit for some patients with refractory epilepsy. VPA controls the generation and propagation of seizures mainly by increasing turnover of GABA and thereby potentiating GABAergic functions in some specific brain regions. Furthermore, the effect of VPA on neuronal excitation mediated by the NMDA subtype of glutamate receptors might be important for its anticonvulsant effects [59]. Because of AU has a significant anti-inflammatory effect and VPA has a prominent anti-seizure effect, the combination of AU and VPA may benefit for patients with refractory and drug-resistant epilepsy, but the explicit effects still need to be verified in subsequent experiments.
The balance of glutamatergic and GABAergic transmission is important for normal neurological function. However, dysfunction in this balance can lead to the occurrence and progression of seizures [7]. Elevation of extracellular glutamate mediated neuronal excitation has been generally considered a critical factor in the pathological process of epilepsy. Increased extracellular glutamate is strongly associated with decreased epileptogenic hippocampal volume in patients with drug resistant epilepsy [60]. Moreover, raised glutamate levels have been observed in various animal models of epilepsy [61]. In the present study, we observed a high concentration of glutamate in the hippocampus of pilocarpine-treated animals. The glutamate transporter, particularly glutamate transporter-1 (GLT-1) in astrocytes, is responsible for the removal of glutamate from the ECS [62]. Human tissue data have revealed that the GLT-1 immunoreactivity was reduced in the sclerotic hippocampus [9]. The deficiency of GLT-1 in rodents revealed that GLT-1 is the major regulator of glutamate uptake [63]. Overexpression of GLT-1 attenuated epileptogenesis and reduced seizure frequency in transgenic mice [64]. Here, we found that pretreatment with AU could promote the expression of GLT-1, suggesting that AU might promote the clearance of glutamate in the hippocampus. In addition, we found that VPA could also promote the expression of GLT-1. However, a previous study showed that VPA decreased GLT-1 in hippocampi in albino rats with chronic, spontaneous, recurrent seizures induced by amygdalar injection of FeCl3 [65]. These observations are contrary to our results and are most likely due to the use of albino rats, or the induction method itself may alter the effect of VPA on GLT-1 expression. Therefore, the effect of VPA on GLT-1 in epilepsy is worthy of follow-up study. Glutamic acid regulates brain excitability by binding to NMDA receptors, especially on the NR2 subunit. The NR2B subunit antagonist ifenprodil, reduces epileptic discharge and inhibits mossy fiber sprouting of granule cells [66]. Here we also explored the effect of AU on NR2B expression in SE. However, our experimental results showed that AU had no significant effect on NR2B expression. The small sample size and large variation among groups may be the reason for the ineffectiveness of AU on the expression of NR2B in the hippocampus. These results indicate that the anti-epileptic effect of AU might be related to the clearance of glutamate by way of increased expression of GLT-1.
Impairment of GABA-mediated inhibition facilitates neuronal hyperexcitability to trigger seizures due to the abnormal release or synthesis of GABA. GABAergic interneurons and basal GABA efflux are decreased during the first spontaneous seizure and latent period in pilocarpine-induced TLE [61]. Promoting the release of GABA to enhance GABA-mediated inhibition is an important target for anti-epileptic drugs [67]. An in vitro study found that AU promotes differentiation of NPCs into GABAergic neurons [30]. In this current study, we found that AU also increased the level of GABA in hippocampus in SE. GABAAR is the primary mediator of fast inhibitory synaptic transmission in the central nervous system [68] and decreased function of the GABAAR has been observed in models of epilepsy [69]. The inhibition of GABAAR also causes the occurrence of seizures [70]. GABAARα1 is the most abundant GABAAR subtype and is the target of benzodiazepines used to treat anxiety disorders, insomnia and epilepsy [71]. A previous study demonstrated that the expression of the GABAARα1 subunit mRNA is decreased after pilocarpine-induced SE [72]. In the present study, we showed that pilocarpine-induced the downregulation of the GABAARα1 protein in pilocarpine-induced SE. Moreover, AU increased the expression of GABAARα1 in the hippocampus. These results revealed that AU might increase the content of GABA and improve the expression of GABAARα1 to suppress epileptic seizures.
In this present study, we demonstrated that AU has an inhibitory effect on pilocarpine-induced seizures. We also discovered that AU could suppress neuroinflammation and modify neurotransmission in the hippocampus in a pilocarpine-induced epileptic mouse model. Epilepsy is a chronic progressive neurological disease, and whether AU can inhibit epileptogenesis in a chronic epileptic model still requires further study. In addition, the specific mechanism of AU’s action needs to explored further in vitro.
Conclusion
AU reduced the severity of epileptic seizures and prolonged the latency period prior to the first seizure. Moreover, AU inhibited microgliosis and astrogliosis in pilocarpine-induced SE and decreased the expression of pro-inflammatory cytokines. AU also served to modify the imbalance between GABA and glutamate as well as upregulate GABAAR levels. Furthermore, AU promoted the clearance of glutamate by enhancing the expression of the GLT-1 protein. These results suggest that AU can inhibit seizure activity and its action might be related to the reduction of neuroinflammation as well as the regulation of neurotransmission. Together, these results provide an experimental basis for the development of novel anti-epileptic drugs.
References
Fisher RS, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, Engel J Jr (2005) Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 46:470–472
Singh A, Trevick S (2016) The epidemiology of global epilepsy. Neurol Clin 34:837–847
Loscher W, Schmidt D (2011) Modern antiepileptic drug development has failed to deliver: ways out of the current dilemma. Epilepsia 52:657–678
Patel DC, Wilcox KS, Metcalf CS (2017) Novel targets for developing antiseizure and, potentially, antiepileptogenic drugs. Epilepsy Curr 17:293–298
Yuen AWC, Keezer MR, Sander JW (2018) Epilepsy is a neurological and a systemic disorder. Epilepsy & Behav E&B 78:57–61
Amtul Z, Aziz AA (2017) Microbial proteins as novel industrial biotechnology hosts to treat epilepsy. Mol Neurobiol 54:8211–8224
Guerriero RM, Giza CC, Rotenberg A (2015) Glutamate and GABA imbalance following traumatic brain injury. Curr Neurol Neurosci Rep 15:27
Wang Y, Qin ZH (2010) Molecular and cellular mechanisms of excitotoxic neuronal death. Apoptosis 15:1382–1402
Proper EA, Hoogland G, Kappen SM, Jansen GH, Rensen MG, Schrama LH, van Veelen CW, van Rijen PC, van Nieuwenhuizen O, Gispen WH, de Graan PN (2002) Distribution of glutamate transporters in the hippocampus of patients with pharmaco-resistant temporal lobe epilepsy. Brain 125:32–43
Werner FM, Covenas R (2011) Classical neurotransmitters and neuropeptides involved in generalized epilepsy: a focus on antiepileptic drugs. Curr Med Chem 18:4933–4948
Raol YH, Lund IV, Bandyopadhyay S, Zhang G, Roberts DS, Wolfe JH, Russek SJ, Brooks-Kayal AR (2006) Enhancing GABA(A) receptor alpha 1 subunit levels in hippocampal dentate gyrus inhibits epilepsy development in an animal model of temporal lobe epilepsy. J Neurosci 26:11342–11346
Devinsky O, Vezzani A, Najjar S, De Lanerolle NC, Rogawski MA (2013) Glia and epilepsy: excitability and inflammation. Trends Neurosci 36:174–184
Dambach H, Hinkerohe D, Prochnow N, Stienen MN, Moinfar Z, Haase CG, Hufnagel A, Faustmann PM (2014) Glia and epilepsy: experimental investigation of antiepileptic drugs in an astroglia/microglia co-culture model of inflammation. Epilepsia 55:184–192
Vezzani A, Aronica E, Mazarati A, Pittman QJ (2013) Epilepsy and brain inflammation. Exp Neurol 244:11–21
Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL, Marinovich M (2003) Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci 23:8692–8700
Librizzi L, Noe F, Vezzani A, de Curtis M, Ravizza T (2012) Seizure-induced brain-borne inflammation sustains seizure recurrence and blood-brain barrier damage. Ann Neurol 72:82–90
Shimada T, Takemiya T (2014) Role of inflammatory mediators in the pathogenesis of epilepsy. Mediators Inflamm 2014:901902
Najjar S, Pearlman D, Miller DC, Devinsky O (2011) Refractory epilepsy associated with microglial activation. Neurologist 17:249–254
Mikati MA, Kurdi R, El-Khoury Z, Rahi A, Raad W (2010) Intravenous immunoglobulin therapy in intractable childhood epilepsy: open-label study and review of the literature. Epilepsy & Behav E&B 17:90–94
Crow AR, Song S, Semple JW, Freedman J, Lazarus AH (2007) A role for IL-1 receptor antagonist or other cytokines in the acute therapeutic effects of IVIg? Blood 109:155–158
Li D, Li P, He Z, Cen D, Meng Z, Liang L, Luo X (2012) Human intravenous immunoglobulins suppress seizure activities and inhibit the activation of GFAP-positive astrocytes in the hippocampus of picrotoxin-kindled rats. Int J Neurosci 122:200–208
Dey A, Kang X, Qiu J, Du Y, Jiang J (2016) Anti-inflammatory small molecules to treat seizures and epilepsy: from bench to bedside. Trends Pharmacol Sci 37:463–484
Zhao Y, Li Y, Wang X, Sun W (2008) The experimental study of Cortex Eucommiae on meridian tropsim: the distribution study of aucubin in rat tissues. J Pharm Biomed Anal 46:368–373
Lv PY, Feng H, Huang WH, Tian YY, Wang YQ, Qin YH, Li XH, Hu K, Zhou HH, Ouyang DS (2017) Aucubin and its hydrolytic derivative attenuate activation of hepatic stellate cells via modulation of TGF-beta stimulation. Environ Toxicol Pharmacol 50:234–239
Jeong HJ, Koo HN, Na HJ, Kim MS, Hong SH, Eom JW, Kim KS, Shin TY, Kim HM (2002) Inhibition of TNF-alpha and IL-6 production by Aucubin through blockade of NF-kappaB activation RBL-2H3 mast cells. Cytokine 18:252–259
Park KS, Chang IM (2004) Anti-inflammatory activity of aucubin by inhibition of tumor necrosis factor-alpha production in RAW 264.7 cells. Planta Med 70:778–779
Wang SN, Xie GP, Qin CH, Chen YR, Zhang KR, Li X, Wu Q, Dong WQ, Yang J, Yu B (2015) Aucubin prevents interleukin-1 beta induced inflammation and cartilage matrix degradation via inhibition of NF-kappaB signaling pathway in rat articular chondrocytes. Int Immunopharmacol 24:408–415
Wang J, Li Y, Huang WH, Zeng XC, Li XH, Li J, Zhou J, Xiao J, Xiao B, Ouyang DS, Hu K (2017) The protective effect of aucubin from Eucommia ulmoides against status epilepticus by inducing autophagy and inhibiting necroptosis. Am J Chin Med 45:557–573
Kim YM, Sim UC, Shin Y, Kim Kwon Y (2014) Aucubin promotes neurite outgrowth in neural stem cells and axonal regeneration in sciatic nerves. Exp Neurobiol 23:238–245
Song M, Kim H, Park S, Kwon H, Joung I, Kim Kwon Y (2018) Aucubin promotes differentiation of neural precursor cells into GABAergic neurons. Exp Neurobiol 27:112–119
Inoue O, Sugiyama E, Hasebe N, Tsuchiya N, Hosoi R, Yamaguchi M, Abe K, Gee A (2009) Methyl ethyl ketone blocks status epilepticus induced by lithium-pilocarpine in rats. Br J Pharmacol 158:872–878
He X, Wang J, Li M, Hao D, Yang Y, Zhang C, He R, Tao R (2014) Eucommia ulmoides Oliv.: ethnopharmacology, phytochemistry and pharmacology of an important traditional Chinese medicine. J Ethnopharmacol 151:78–92
Xue HY, Jin L, Jin LJ, Li XY, Zhang P, Ma YS, Lu YN, Xia YQ, Xu YP (2009) Aucubin prevents loss of hippocampal neurons and regulates antioxidative activity in diabetic encephalopathy rats. Phytother Res 23:980–986
Curia G, Longo D, Biagini G, Jones RS, Avoli M (2008) The pilocarpine model of temporal lobe epilepsy. J Neurosci Methods 172:143–157
Nirwan N, Siraj F, Vohora D (2018) Inverted-U response of lacosamide on pilocarpine-induced status epilepticus and oxidative stress in C57BL/6 mice is independent of hippocampal collapsin response mediator protein-2. Epilepsy Res 145:93–101
Martin E, Pozo M (2006) Animal models for the development of new neuropharmacological therapeutics in the status epilepticus. Curr Neuropharmacol 4:33–40
Choi J, Koh S (2008) Role of brain inflammation in epileptogenesis. Yonsei Med J 49:1–18
Aronica E, Crino PB (2011) Inflammation in epilepsy: clinical observations. Epilepsia 52 Suppl 3:26–32
Aronica E, Ravizza T, Zurolo E, Vezzani A (2012) Astrocyte immune responses in epilepsy. Glia 60:1258–1268
Graeber MB, Li W, Rodriguez ML (2011) Role of microglia in CNS inflammation. FEBS Lett 585:3798–3805
Friedman A, Kaufer D, Heinemann U (2009) Blood-brain barrier breakdown-inducing astrocytic transformation: novel targets for the prevention of epilepsy. Epilepsy Res 85:142–149
de Lanerolle NC, Lee TS, Spencer DD (2010) Astrocytes and epilepsy. Neurotherapeutics 7:424–438
Hanisch UK, Kettenmann H (2007) Microglia: active sensor and versatile effector cells in the normal and pathologic brain. Nat Neurosci 10:1387–1394
Wetherington J, Serrano G, Dingledine R (2008) Astrocytes in the epileptic brain. Neuron 58:168–178
Ortinski PI, Dong J, Mungenast A, Yue C, Takano H, Watson DJ, Haydon PG, Coulter DA (2010) Selective induction of astrocytic gliosis generates deficits in neuronal inhibition. Nat Neurosci 13:584–591
Crespel A, Coubes P, Rousset MC, Brana C, Rougier A, Rondouin G, Bockaert J, Baldy-Moulinier M, Lerner-Natoli M (2002) Inflammatory reactions in human medial temporal lobe epilepsy with hippocampal sclerosis. Brain Res 952:159–169
Maroso M, Balosso S, Ravizza T, Liu J, Aronica E, Iyer AM, Rossetti C, Molteni M, Casalgrandi M, Manfredi AA, Bianchi ME, Vezzani A (2010) Toll-like receptor 4 and high-mobility group box-1 are involved in ictogenesis and can be targeted to reduce seizures. Nat Med 16:413–419
van Vliet EA, Aronica E, Vezzani A, Ravizza T (2018) Review: Neuroinflammatory pathways as treatment targets and biomarker candidates in epilepsy: emerging evidence from preclinical and clinical studies. Neuropathol Appl Neurobiol 44:91–111
Vezzani A, French J, Bartfai T, Baram TZ (2011) The role of inflammation in epilepsy. Nat Rev Neurol 7:31–40
Volterra A, Meldolesi J (2005) Astrocytes, from brain glue to communication elements: the revolution continues. Nat Rev Neurosci 6:626–640
Liu W, Tang Y, Feng J (2011) Cross talk between activation of microglia and astrocytes in pathological conditions in the central nervous system. Life Sci 89:141–146
Stellwagen D, Beattie EC, Seo JY, Malenka RC (2005) Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J Neurosci 25:3219–3228
Boer K, Spliet WG, van Rijen PC, Redeker S, Troost D, Aronica E (2006) Evidence of activated microglia in focal cortical dysplasia. J Neuroimmunol 173:188–195
Park KS (2013) Aucubin, a naturally occurring iridoid glycoside inhibits TNF-alpha-induced inflammatory responses through suppression of NF-kappaB activation in 3T3-L1 adipocytes. Cytokine 62:407–412
Young IC, Chuang ST, Hsu CH, Sun YJ, Liu HC, Chen YS, Lin FH (2017) Protective effects of aucubin on osteoarthritic chondrocyte model induced by hydrogen peroxide and mechanical stimulus. BMC Complement Altern Med 17:91
Zhou Y, Li P, Duan JX, Liu T, Guan XX, Mei WX, Liu YP, Sun GY, Wan L, Zhong WJ, Ouyang DS, Guan CX (2017) Aucubin alleviates bleomycin-induced pulmonary fibrosis in a mouse model. Inflammation 40:2062–2073
Xue HY, Lu YN, Fang XM, Xu YP, Gao GZ, Jin LJ (2012) Neuroprotective properties of aucubin in diabetic rats and diabetic encephalopathy rats. Mol Biol Rep 39:9311–9318
Gomez CD, Buijs RM, Sitges M (2014) The anti-seizure drugs vinpocetine and carbamazepine, but not valproic acid, reduce inflammatory IL-1beta and TNF-alpha expression in rat hippocampus. J Neurochem 130:770–779
Loscher W (2002) Basic pharmacology of valproate: a review after 35 years of clinical use for the treatment of epilepsy. CNS Drugs 16:669–694
Cavus I, Pan JW, Hetherington HP, Abi-Saab W, Zaveri HP, Vives KP, Krystal JH, Spencer SS, Spencer DD (2008) Decreased hippocampal volume on MRI is associated with increased extracellular glutamate in epilepsy patients. Epilepsia 49:1358–1366
Soukupova M, Binaschi A, Falcicchia C, Palma E, Roncon P, Zucchini S, Simonato M (2015) Increased extracellular levels of glutamate in the hippocampus of chronically epileptic rats. Neuroscience 301:246–253
Danbolt NC (2001) Glutamate uptake. Prog Neurobiol 65:1–105
Rothstein JD, Dykes-Hoberg M, Pardo CA, Bristol LA, Jin L, Kuncl RW, Kanai Y, Hediger MA, Wang Y, Schielke JP, Welty DF (1996) Knockout of glutamate transporters reveals a major role for astroglial transport in excitotoxicity and clearance of glutamate. Neuron 16:675–686
Kong Q, Takahashi K, Schulte D, Stouffer N, Lin Y, Lin CL (2012) Increased glial glutamate transporter EAAT2 expression reduces epileptogenic processes following pilocarpine-induced status epilepticus. Neurobiol Dis 47:145–154
Ueda Y, Willmore LJ (2000) Molecular regulation of glutamate and GABA transporter proteins by valproic acid in rat hippocampus during epileptogenesis. Exp Brain Res 133:334–339
Wang XM, Bausch SB (2004) Effects of distinct classes of N-methyl-D-aspartate receptor antagonists on seizures, axonal sprouting and neuronal loss in vitro: suppression by NR2B-selective antagonists. Neuropharmacology 47:1008–1020
Kammerer M, Brawek B, Freiman TM, Jackisch R, Feuerstein TJ (2011) Effects of antiepileptic drugs on glutamate release from rat and human neocortical synaptosomes. Naunyn Schmiedebergs Arch Pharmacol 383:531–542
Barnard EA, Darlison MG, Fujita N, Glencorse TA, Levitan ES, Reale V, Schofield PR, Seeburg PH, Squire MD, Stephenson FA (1988) Molecular biology of the GABAA receptor. Adv Exp Med Biol 236:31–45
Gibbs JW, Sombati S, DeLorenzo RJ, Coulter DA (1997) Physiological and pharmacological alterations in postsynaptic GABA(A) receptor function in a hippocampal culture model of chronic spontaneous seizures. J Neurophysiol 77:2139–2152
Macdonald RL, Twyman RE, Ryan-Jastrow T, Angelotti TP (1992) Regulation of GABAA receptor channels by anticonvulsant and convulsant drugs and by phosphorylation. Epilepsy Res 9:265–277
Uusi-Oukari M, Korpi ER (2010) Regulation of GABA(A) receptor subunit expression by pharmacological agents. Pharmacol Rev 62:97–135
Grabenstatter HL, Russek SJ, Brooks-Kayal AR (2012) Molecular pathways controlling inhibitory receptor expression. Epilepsia 53 Suppl 9:71–78
Acknowledgements
This study was supported by the National Development of Key Novel Drugs for Special Projects of China (Grant No.: 2017ZX09304014), the Natural Science Foundation of Hunan Province (Grant No.: 2016JJ4116) and the Hunan Key Laboratory for Bioanalysis of Complex Matrix Samples (2017TP1037).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, S., Zeng, X., Zong, W. et al. Aucubin Alleviates Seizures Activity in Li-Pilocarpine-Induced Epileptic Mice: Involvement of Inhibition of Neuroinflammation and Regulation of Neurotransmission. Neurochem Res 44, 472–484 (2019). https://doi.org/10.1007/s11064-018-2700-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-018-2700-y