Abstract
Purpose
High-grade spinal glioma (HGSG) is an extremely rare, malignant neoplasm insufficiently described in the literature. We sought to investigate the effect of epidemiological risk factors and treatment strategies on the prognosis of HGSGs using the National Cancer Database (NCDB).
Methods
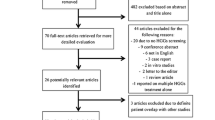
Patients with diagnosis codes specific for HGSG were queried from the NCDB during the years 2004–2016. Kaplan–Meier curves were generated with log-rank testing performed to assess factors affecting survival. Univariate and multivariate Cox regression analysis was also performed to investigate overall survival.
Results
396 patients were identified with a histologically-confirmed diagnosis of HGSG between 2004–2016. The mean survival time for all patients was 24.5 months (SD: 20.3). Multivariate Cox proportional-hazards regression analysis revealed that tumor size of 26–50 mm (HR 4.96, 95% CI 1.76–13.98, p < 0.01) and greater than 50 mm (HR 4.67, 95% CI 1.43–15.23, p = 0.01) were associated with worsened overall survival in comparison to lesions less than 26 mm. While quality of life was not investigated, both Kaplan–Meier log-rank testing and regression analysis failed to demonstrate an association of survival outcomes with extent of resection, radiotherapy, or chemotherapy.
Conclusion
The current study represents the largest retrospective analysis of adult primary high-grade spinal glioma to date. Our analysis found no relationship between the extent of surgical resection and survival outcomes. In addition, we failed to show any statistically significant survival benefit with radiotherapy or chemotherapy. This disease process has a poor prognosis without a current modality of treatment that improves survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intramedullary spinal cord tumors are relatively rare neoplasms accounting for 2–4% of all central nervous system neoplasms [1]. Spinal cord gliomas comprise approximately 6–8% of all these intrinsic spinal cord tumors, with high-grade variants found in between 7–30% of this sub-population [2, 3]. The incidence of this rare malignant neoplasm has been reported to be as low as 0.22 persons per 100,000 persons; unsurprisingly, the vast majority of existing literature is based on case reports and case series data [4]. The prognosis for this unfortunate population continues to be quite poor, with median survival time estimated to be between 12 and 24 months, dependent on factors such as histology, gender, and treatment modality [4, 5].
While literature pertaining to radiotherapy and surgical treatment has been published in small single-institution studies, there is limited information available on high-grade spinal glioma (HGSG) patients in regards to large, population-based studies that explore current trends in outcomes and treatment [5, 6]. The current study seeks to elucidate survival risk factors with the use of the largest cancer database available for public use, the National Cancer Database (NCDB). Aggregating both grade III and grade IV HGSG patients, we have specifically sought to investigate the epidemiology and the effect of current treatment trends on outcomes in adults with this rare malignancy.
Methods
Study population
This was a population-based study that employed a longitudinal survival analysis of the selected cohort. The data for this study was derived from the National Cancer Database (NCDB), a prospectively collected cancer registry maintained jointly by the American College of Surgeons and the American Cancer Society. This database is sourced from over 1,500 cancer centers and represents more than 70% of newly diagnosed cancer cases and more than 34 Mio. historical records. Our study used the most recent release of the database that provided patient data between the years 2004 and 2016.
For the purpose of our study, we specified our primary cohort as all adult patients with primary HGSG, including WHO grades III and IV. We identified all histologic subtypes that would satisfy this criteria as classified by the International Classification of Diseases for Oncology, Third Edition (ICD-O-3). This included all patients with the following confirmed histopathological diagnoses: malignant glioma (9380/3), anaplastic oligoastrocytoma (9382/3), anaplastic ependymoma (9392/3), anaplastic astrocytoma (9401/3), astroblastoma (9430/3), glioblastoma (9440/3), giant cell glioblastoma (9441/3), gliosarcoma (9442/3), and anaplastic oligodendroglioma (9451/3). From the NCDB database, all patients with tumors originating from the spinal cord (primary site code C72.0) were first queried, and then screened for patients with the aforementioned ICD-O-3 diagnosis codes specifying HGSG. We included only adults for which HGSG was their first and primary tumor. Subsequent tumors, recurrences, and cases diagnosed at autopsy were not considered for this analysis. In addition, we excluded all cases that lacked histopathological confirmation (i.e. imaging, direct visualization, clinical diagnosis, or unknown).
NCDB data are publicly available and de-identified, and thus did not require review from our Institutional Review Board.
Statistical analysis
Descriptive analyses were performed to evaluate patient, tumor, and treatment characteristics. Survival status was the variable employed to assess outcomes in this study. This outcome variable was defined as either alive or not alive (i.e. all-cause mortality). This value was determined as the interval in months between the time of diagnosis and death or last follow-up as reported by NCDB. All available demographic and treatment data were analyzed with respect to survival status.
The student’s t test was used for comparison of all continuous variables, while the Fisher exact test (or chi-squared test when appropriate) was used for all categorical variables. Kaplan–Meier curves were generated for comparative visualization of various demographic and treatment variables. All-inclusive multivariate Cox proportional hazard regression was used to analyze survival and adjust for confounding, reducing the likelihood of bias. Coefficients in the model were converted to hazard ratios (HR) for analysis of survival outcomes. All p values were reported as 2-sided, with statistical significance defined as p < 0.05. Statistical analysis was performed using R statistical software (version 3.4.0, 2017; R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline demographics
Over the 13-year period between 2004 and 2016, there were 20,281 adult patients (18 years or older at the time of diagnosis) were identified in the NCDB that were classified as spinal cord tumor patients. Among this population, 440 patients were identified as those with a first and primary malignancy with high-grade glioma diagnosis codes, and of this sub-population, 396 patients were reported to have a histology-confirmed diagnosis. Our analysis suggests a prevalence of 2.2% of primary high-grade spinal glioma among all spinal cord tumors. Baseline characteristics of the entire population are reported in Table 1. The age distribution of the population was evenly distributed between 18–35, 35–55, and 55 years and over age groups (34.8% vs 33.8% vs 31.3%, respectively). The majority of patients were male sex (n = 218, 55.0%). The majority of the population was white (n = 305, 77.0%), followed by black (13.3%), and finally other (n = 33, 8.3%). Further analysis of those coded as other revealed primarily Hispanic origin (70%) followed by a small number of patients with Asian ancestry. Most patients in the cohort (n = 312, 78.8%) were healthy with a Charlson-Deyo score of 0 at the time of diagnosis. Most patients were diagnosed in the most recent time period of 2014–2016 (n = 128, 32.3%). While most tumors lacked information regarding size, 26–50 mm was the most common (n = 69, 17.4%).
Treatment characteristics
Surgery was performed in the majority of cases (n = 326, 82.3%) (Table 2). When surgery was not performed, it was either not recommended (n = 64, 16.2%) or not recommended due to comorbidities (n = 3, 0.8%). The majority of the cohort underwent partial resection (n = 198, 50.0%), while gross-total resection occurred in 23 cases (5.8). In a minority of patients, surgery was performed but the extent of resection was unknown (n = 105, 26.5%). On average, surgery was performed 8.2 days (SD: 23.6) after diagnosis, and patients spent 7.3 days (SD: 8.6) in the hospital after surgery.
Most patients underwent radiation therapy of some kind (n = 277, 69.9%). The most common treatment modality was intensity-modulated radiation treatment (IMRT) (n = 78, 28.1%), followed by conventional methods of external beam radiation therapy (EBRT). A small number of patients underwent proton therapy (n = 5, 1.8%). Radiotherapy was started an average of 45.2 days (SD: 36.1) after diagnosis, performed for an average of 18.6 volumes (SD: 16.7), and for an average treatment duration of 27.6 days (SD: 24.1). The mean regional dose used was 3091.3 cGy (SD: 2292.5). A boost treatment was employed in 71 patients, for an average dose of 194.9 cGy (SD: 607.6). Finally, nearly half of patients received chemotherapy (n = 195, 49.2%). Treatment was not administered due to patient refusal in 8 cases (2.0%). Chemotherapy was started an average of 47.2 days (SD: 46.1) after diagnosis.
Survival analysis
The mean survival time for all patients was 24.5 months (SD: 20.3) (Table 1). Kaplan–Meier log-rank testing demonstrated that tumor size (Fig. 1d) had a statistically significant impact on overall survival; notably, tumor size of less than 26 mm appeared to be associated with improved survival. Kaplan–Meier log-rank testing did not demonstrate an association between age, gender, race, or tumor grade with survival (Fig. 1a, b, c, e). This testing also failed to demonstrate an association of surgery, radiotherapy, or chemotherapy with overall survival (Fig. 2a, b, c). On univariate regression, other race (non-white, non-black) and tumor size had statistically significant associations with survival (p < 0.05). After adjustment for the confounding effects of each variable, multivariate survival analysis also revealed that tumor size of 26–50 mm (hazard ratio [HR] 4.96, 95% confidence interval [CI] 1.76–13.98, p < 0.01) and greater than 50 mm (HR 4.67, 95% CI 1.43–15.23, p = 0.01) were both associated with worsened overall survival in comparison to lesions less than 26 mm (Table 3). Age greater than 55 was associated with potentially improved survival (HR 0.51, 95% CI 0.26–0.97, p = 0.04), but this was not felt to be clinically significant; moreover, there was no indication of this association on univariate analysis. The association of race (other) and survival demonstrated in univariate analysis was lost upon multivariate regression. While tumor size of less than 26 mm was associated with improved outcomes, surgical extent of resection, radiotherapy, and chemotherapy did not independently have a statistically significant association with survival outcomes.
Discussion
Intramedullary spinal cord tumors represent approximately 2–4% of all central nervous system neoplasms and 15% of all spinal cord tumors, excluding metastasis. The majority of these neoplasms are low-grade, with previous studies estimating high-grade variants to occur in 7–30% of these spinal cord tumor cases, equating to an overall prevalence of between 2–5% of all spinal cord tumors [3]. While high-grade neoplasms pose a clear delineation in comparison to low-grade lesions, there have been reports of malignant transformation in low-grade tumors [7]. The results of our epidemiologic investigation agree with previously reported figures, suggesting an overall prevalence of 2.2% of primary high-grade spinal glioma among all spinal cord tumors. This unfortunate population represents an extremely challenging population that has long been resistant to modern treatment strategies. Owing to the rarity of these lesions in conjunction with the difficulties in improving survival, the existing literature has been unclear in regards to both outcome and the effectiveness of currently pursued treatment paradigms.
These highly aggressive lesions have been found to frequently develop in the cervicothoracic segments of the spinal cord, with a slight preponderance for the first several decades of life. These patients typically have a short clinical history prior to the time of diagnosis. Surgical resection of these intrinsic lesions is inherently high-risk due to the infiltrating nature of many of the neoplasms with unclear margins, stereotypical location high in the spinal cord, and presence of pre-operative deficits. In a 30-year single-institution review of 22 surgical patients, Raco and colleagues (2010) found that the most common presenting symptoms were hypesthesia or paresthesia (91%), motor dysfunction (86%), and sphincter dysfunction (41%). In this small series, surgery was associated with a clear worsening of neurologic deficits in 64% of patients; however, adjuvant therapy was associated with a longer mean survival time [8]. In an investigation regarding the prognostic effect of extent of resection in 35 patients with malignant astrocytoma of the spinal cord, McGirt et al. (2008) found that while 40% of patients experienced postoperative neurologic decline, radical resection was associated with improved outcomes in grade III patients. However, radical surgery for grade IV lesions with postoperative radiotherapy fared no better than historical controls of biopsy and radiotherapy alone [9]. Less encouraging results were found in a series of 46 spinal cord astrocytoma patients by Babu et al. (2014), noting that surgical resection was associated with a higher rate of neurologic complications, and extent of resection was actually associated with worsened postoperative state (66.7% vs. 18.8%, P = 0.0069). Moreover, surgical resection was not associated with a survival benefit in comparison to biopsy alone [10]. In the largest series of spinal cord astrocytomas of all types, Minehan et al. (2009) reported that surgical treatment was associated with shorter survival times in 136 patients. In addition, histologic type was noted to be the most important prognostic variable, again underscoring the questionable efficacy of surgical resection in high-grade lesions [11]. A number of smaller case series have similarly reported conflicting evidence in regards to the association between surgical resection and outcome, with most patients being subject to high rates of neurologic complications and poor survival times [5, 12].
The existing literature has been even less clear in regards to radiotherapy, with no established guidelines for treatment. A recent systematic review of treatment paradigms in intramedullary spinal cord tumors by Hamilton et al. (2019) reported that while radiation therapy increased the risk of mortality in low-grade lesions, it may offer a modest survival benefit in high-grade lesions [13]. A small series by Kahn et al. (2011) found that while overall survival was extremely poor in high-grade groups, photon treatment was associated with improved outcomes in comparison to proton therapy in multivariate analysis [14]. Several studies have noted benefits of post-operative radiotherapy after incomplete resection in low-grade ependymoma; however, none of these studies have reported encouraging findings in high-grade lesions [15,16,17]. In an analysis of 45 non-ependymoma glioma patients undergoing radiotherapy, Choi et al. (2019) reported that only tumor grade was a prognostic indicator of overall survival, with high-grade lesions exhibiting high rates of seeding (45%) [6].
A population-based study of the Surveillance, Epidemiology, and End Results (SEER) database of high-grade spinal glioma by Liu et al. (2018) found that while the extent of resection was not associated with improved outcomes, postoperative radiotherapy was associated with a 42% reduction in hazard ratio in multivariate analysis; however, Kaplan–Meier log-rank testing failed to show statistical significance in this parameter [18]. These findings are contrasted with a previous SEER database study by Milano et al. (2010) that interestingly found that radiotherapy was associated with worsened survival outcomes [19]. Fakhreddine and colleagues (2013) from M.D. Anderson Cancer Center found that while postoperative radiotherapy and extent of resection did not affect progression-free survival, chemotherapy was associated with improved outcomes in multivariate analysis [20]. Notably, the literature is exceedingly sparse in regards to evidence regarding the use of chemotherapeutic agents in this population. Kaley et al. (2012) reported findings in the usage of either temozolomide or bevacizumab for high-grade spinal glioma in 8 patients; however, this series was not designed for a comparative analysis and suggested future studies [21].
Aggregating both grade III and grade IV HGSG patients, the current study represents the largest and most up-to-date retrospective analysis of adult primary high-grade spinal glioma conducted. The data is drawn from a nationwide database and encompasses recently treated patients between 2004 and 2016. Our findings suggest that high-grade spinal glioma in adults is not a surgical disease with current microsurgical techniques. Neither the presence of surgery nor extent of resection were associated with improved survival outcomes in the largest cohort to date. Moreover, the historically reported postoperative complications rates of as high as 66.7% further underscore the necessity of careful deliberation of the cost–benefit of surgical intervention in these challenging patients. Moreover, while our study failed to show any effect on overall survival, it should be considered that aggressive resection may negatively impact a patient’s remaining quality of life in a terminal disease. The current study also failed to show any significant survival benefit with radiotherapy or chemotherapy. The wide variance in radiation type, dose, and fractions highlights the lack of clear evidence and guidelines in this neoplasm. Similar to surgery, the cost–benefit of these non-surgical treatment modalities must be carefully considered in this highly aggressive disease. Perhaps most importantly, our findings emphasize the pressing need for further research and advancements in the treatment of high-grade spinal glioma.
Our study is subject to several limitations which must be considered when interpreting the presented results. The use of NCDB, a large, registry-based dataset, renders our analysis vulnerable to several confounding factors that are not routinely collected, thus were unable to be controlled for. A large number of patients did not have information regarding tumor size, limiting the power of the assessment on overall status. In addition, the specific methodology employed in measuring tumor size cannot conclusively be ascertained from our dataset, and the chance exists for variability in measurement practices. Specific chemotherapeutic agents and doses could also be crucial in determining potent treatment strategies; however, such data was unavailable as well. Furthermore, the lack of data on tumor location, specifically which spinal segment was affected, may be a possible confounder, owing to the fact that cervical HGSGs are associated with a poorer prognosis, possibly due to the compression of more critical neural structures [5, 12]. There may also exist significant variability in coding practices in regards to surgery and extent of resection; notably, different coders may classify patients differently depending the nature of surgical intervention (biopsy alone vs. resection) as well as reported extent of resection (sub-total vs. gross-total). In addition, while the small number of patients that underwent gross-total resection may be emblematic of the intrinsic difficulties in surgical treatment, the sample size notably limits our assessment of the effect of extent of resection. Finally, our methodology aggregated both grade III and grade IV HGSG patients. While our KM analysis did not demonstrate a statistically significant impact on survival depending on grading between these high-grade types, aggregating these tumors may alter our results in regards to treatment outcomes. There exists the possibility that lower grades may be more amenable to resection or other treatment modalities, or may have different patterns in overall survival when analyzing various demographic factors.
Despite these drawbacks, our study provides a description of the largest sample of HGSG patients to date. In addition, the use of the NCDB affords more representative and generalizable data compared to smaller, single-institution reports. Although definitive evidence regarding the efficacy of treatment regimens should be elucidated from robust, prospective trials, our analysis has inherent value in illustrating survival trends in a rare tumor entity that is difficult to examine in a clinically meaningful manner. From this analysis, there does not seem to be a modality that treats this rare disease process. Therefore, other experimental therapies may be efficacious in the future [22].
Conclusion
Aggregating both grade III and grade IV HGSG patients, the current study represents the largest and most up-to-date retrospective analysis of adult primary high-grade spinal glioma conducted. Our analysis found no relationship between the extent of surgical resection and survival outcomes. In addition, we failed to show any statistically significant survival benefit with radiotherapy or chemotherapy. This disease process has a poor prognosis without a current modality of treatment that improves survival. The risks and side effects of these treatment modalities must be carefully considered in this highly aggressive disease given potentially limited survival benefits. This disease process has a poor prognosis without a current modality of treatment that improves survival.
References
Chamberlain MC, Tredway TL (2011) Adult primary in- tradural spinal cord tumors: a review. Curr Neurol Neurosci Rep 11:320–328
Epstein FJ, Farmer JP, Freed D (1992) Adult intramedullary astrocytomas of the spinal cord. J Neurosurg 77:355–359
Minehan KJ, Shaw EG, Scheithauer BW, Davis DL, Onofrio BM (1995) Spinal cord astrocytoma: pathological and treatment considerations. J Neurosurg 83:590–595
Wong AP, Dahdaleh NS, Fessler RG et al (2013) Risk factors and long-term survival in adult patients with primary malignant spinal cord astrocytomas. J Neurooncol 115:493–503
Seki T, Hida K, Yano S et al (2015) Surgical outcomes of high- grade spinal cord gliomas. Asian Spine J 9:935–941
Choi SH, Yoon HI, Yi S et al (2019) Treatment outcomes of radiotherapy for primary spinal cord glioma. Strahlenther Onkol 195(2):164–174
Ryu SJ, Kim JY, Kim KH et al (2016) A retrospective observational study on the treatment outcomes of 26 patients with spinal cord astrocytoma including two cases of malignant transformation. Eur Spine J 25(12):4067–4079
Raco A, Piccirilli M, Landi A, Lenzi J, Delfini R, Cantore G (2010) High-grade intramedullary astrocytomas: 30 years’ experience at the neurosurgery department of the University of Rome “Sapienza”. J Neurosurg Spine 12(2):144–153
McGirt MJ, Goldstein IM, Chaichana KL, Tobias ME, Kothbauer KF, Jallo GI (2008) Extent of surgical resection of malignant astrocytomas of the spinal cord: outcome analysis of 35 patients. Neurosurgery 63(1):55–61
Babu R, Karikari IO, Owens TR, Bagley CA (2014) Spinal cord astrocytomas: a modern 20-year experience at a single institution. Spine 39(7):533–540
Minehan KJ, Brown PD, Scheithauer BW, Krauss WE, Wright MP (2009) Prognosis and treatment of spinal cord astrocytoma. Int J Radiat Oncol Biol Phys 73(3):727–733
Nakamura M, Chiba K, Ishii K et al (2006) Surgical outcomes of spinal cord astrocytomas. Spinal Cord 44(12):740–745
Hamilton KR, Lee SS, Urquhart JC, Jonker BP (2019) A systematic review of outcome in intramedullary ependymoma and astrocytoma. J Clin Neurosci 63:168–175
Kahn J, Loeffler JS, Niemierko A, Chiocca EA, Batchelor T, Chakravarti A (2011) Long-term outcomes of patients with spinal cord gliomas treated by modern conformal radiation techniques. Int J Radiat Oncol Biol Phys 81(1):232–238
Lee SH, Chung CK, Kim CH et al (2013) Long-term outcomes of surgical resection with or without adjuvant radiation therapy for treatment of spinal ependymoma: a retrospective multicenter study by the Korea Spinal Oncology Research Group. Neuro-Oncology 15(7):921–929
Lin YH, Huang CI, Wong TT et al (2005) Treatment of spinal cord ependymomas by surgery with or without postoperative radiotherapy. J Neurooncol 71(2):205–210
Wahab SH, Simpson JR, Michalski JM, Mansur DB (2007) Long term outcome with post-operative radiation therapy for spinal canal ependymoma. J Neurooncol 83(1):85–89
Liu J, Zheng M, Yang W, Lo SL, Huang J (2018) Impact of surgery and radiation therapy on spinal high-grade gliomas: a population-based study. J Neurooncol 139(3):609–616
Milano MT, Johnson MD, Sul J et al (2010) Primary spinal cord glioma: a Surveillance, Epidemiology, and End Results database study. J Neurooncol 98(1):83–92
Fakhreddine MH, Mahajan A, Penas-prado M et al (2013) Treatment, prognostic factors, and outcomes in spinal cord astrocytomas. Neuro-Oncology 15(4):406–412
Kaley TJ, Mondesire-Crump I, Gavrilovic IT (2012) Temozolomide or bevacizumab for spinal cord high-grade gliomas. J Neurooncol 109(2):385–389
Kheirkhah P, Denyer S, Bhimani AD et al (2018) Magnetic drug targeting: a novel treatment for intramedullary spinal cord tumors. Sci Rep 8(1):11417
Funding
The grant support from the AOSPine Innovation Grant was utilized for funding this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nunna, R.S., Khalid, S., Ryoo, J.S. et al. Adult primary high-grade spinal glioma: a nationwide analysis of current trends in treatment and outcomes. J Neurooncol 147, 633–641 (2020). https://doi.org/10.1007/s11060-020-03458-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03458-z