Abstract
Introduction
Spinal high-grade gliomas (S-HGGs) is an extremely rare entity in the literature, with only sporadic cases reported. We aim to characterize prognostic factors for post-treatment survival using the SEER database.
Methods
We examined all patients with gliomas located in the spinal cord. WHO-grade was first determined by site-specific factor-1 (WHO-grade), then supplemented by direct review of ICD-O-3 histology. Only grades 3 and 4 were included in this study. Multivariable Cox regression analysis was performed.
Results
A total of 158 high-grade spinal cord gliomas were included. Mean age at diagnosis was 36.88 years with 52.8% male. Median survival of all patients was 20 months. A stepwise Akaike information criterion was performed for multivariable Cox regression, with forced inclusion of surgery extent and postoperative radiation therapy (RT). The final model selection added tumor size in addition to these two variables. Tumor size was not related to survival in our study. The extend of surgery had no significant impact on survival of patients, whereas postoperative RT is associated with prolonged survival (HR = 0.55, CI [0.33, 0.93], p = 0.026).
Conclusion
S-HGGs are rare tumors with aggressive course of disease. We have found that overall median survival of S-HGGs is poor at 24 months, and no demographic or tumor-related factors have been confirmed. Extend of surgery is not associated with improved survival after adjusting for postoperative RT. Postoperative RT is the only factor in our study associated with prolonged survival in S-HGGs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal high-grade glioma (S-HGG) is an extremely rare disease which only comprises 30% of all spinal cord gliomas with reported annual incidence of 0.12 per 100,000 persons [1,2,3]. The existing knowledge regarding general survival and the impact of treatment on prognosis of S-HGG patients is extremely limited, with most being case reports or small case-series. As of to-date, only about 200 cases of spinal cord glioblastoma (GBM) were reported in the literature [4], with median survival ranging from 10 to 20 months depending on treatment modality [2, 3, 5,6,7,8,9,10]; whereas the median survival may be extended to 25.5 months if World Health Organization (WHO) grade III gliomas were included [2]. Reports on spinal HGGs were only seen in small institutional series with 10–20 patients [2, 7, 11], and the general characteristics and survival statistics of S-HGG has yet to be explored in large, population-based studies. In this study, we aim to report general characteristics and outcome of S-HGG using the Surveillance, Epidemiology, and End Results Program (SEER) database, with a specific emphasis on investigating the impact of extent of surgical resection and postoperative radiation therapy (RT) on overall median survival of these patients.
Methods
Study cohort
Similar to other SEER studies, this study employed a longitudinal survival study design. The study is exempt from institutional review board (IRB) as all data is publicly available. The SEER database consists of cancer patients at 18 registries across United States and is actively maintained by the National Cancer Institute (NCI). We utilized the 2015 submission, which consists of patients enrolled from 1973 to 2013.
S-HGG is the primary cohort of interest, which is defined as WHO grade III/IV gliomas located in the spinal cord. From the SEER database, all patients with tumors in the location of “spinal cord” were screened for S-HGG. Those with “caudal equina” as location were excluded from our study as they represent a different cohort, and also may have overall different management strategies compared to true intramedullary tumors. All tumors labeled “benign” or “borderline malignant” were first excluded, and those with non-gliomas or without survival status were also excluded. For remaining patients, we first determined WHO grade III/IV using the collaborative stage (CS) site-specific (SS) factor-1, which is defined as the WHO grade in central nervous system (CNS) tumors in SEER database. Next, for those with unknown WHO grade, we reviewed the International Classification of Diseases for Oncology Version 3 (ICD-O-3) and included all patients having 9430/3: Astroblastoma, 9440/3: Glioblastoma, NOS (not otherwise specified), and 9441/3: Giant Cell Glioblastoma. Among these patients, those with unknown methodology of confirmation for tumor histology were also excluded.
Definition of variables
The primary outcome of interest is time-to-event survival of patients. Survival is defined using all-cause mortality. Patient demographics including age, sex, race, insurance status and marital status were collected. Age was defined as age at diagnosis in years; for ease of analysis in regression model, age was also regrouped into four categories: 0–17, 18–39, 40–59, and 60 years or above. Race was categorized as: White, Black, Hispanic, Asian, and Others. Insurance status for patients was uninsured, Medicaid, non-Medicaid insurance, insurance NOS, or unknown. We also regrouped marital status into: married, divorced/separated/widowed, single/unmarried, or unknown. Year of diagnosis was re-grouped into decades. Cutoff for tumor-size was selected as 50 mm, which is approximately the mean of known size of tumors from the dataset. Tumor extension was defined as: localized, regional, distal/metastasis or unknown. Extent of surgical resection included no surgery, partial resection, gross total resection/total resection (GTR/TR) or unknown. RT was defined as whether the patient received post-operative RT.
Statistical analysis
Patient and lesion characteristics were summarized using descriptive statistics. In regards to survival analysis, Kaplan–Meier curve with log rank test was first performed to visualize survival curves, and univariable Cox regression analysis was performed for each of the included variables. Due to limited sample size, variable selection is pertinent for multivariable Cox regression, and we applied Akaike information criterion (AIC) for this process. It should be noted that the two treatment variables, surgery and RT, were forced into the model manually as they were variables of interest in this study. All p values in this study were two sided, and all analyses were performed using R Statistical Software (Version 3.3.2, 2016, Vienna, Austria).
Results
Patient cohort and general characteristics
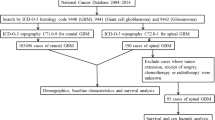
After application of inclusion and exclusion criteria, a total of 158 patients were included in our study. A depiction of study cohort selection is presented in Fig. 1. Among these patients, the most common histology by ICD-O-3 is 9440/3: glioblastoma, NOS (n = 111, 70.3%), followed by 9392/3: ependymoma, anaplastic (n = 14, 8.9%) and 9401/3: astrocytoma, anaplastic, (n = 14, 8.9%). The included tumor histology is listed in Table 1.
Patient baseline characteristics and treatment were summarized using descriptive statistics in Table 2. As shown, most patients in this study were diagnosed between 2003 and 2013 (66.3%). The average age at diagnosis of the patient cohort is 36.23 ± 21.00 years, with 52.5% male (n = 83). The majority of patients are White (n = 112, 70.9%), followed by Hispanic (n = 17, 10.8%) and Black (n = 14, 8.9%). Most patients in this study were either married or never married before, with mean age of married patients being 49.02 years and unmarried or single patients being 20.2 years. In patients with known insurance status, most were insured by non-Medicaid insurance (n = 59, 37.3%). In those with known size information, more patients had smaller tumor (size ≤ 50 mm), and most tumors were localized without further extension (63.3%). In regard to treatment, most underwent partial resection (56.3%), with only 10.8% patients having GTR/TR. 31 patients (19.6%) did not receive surgical treatment of any kind. A large proportion of patients underwent postoperative RT (63.9%), compared to 33.5% who did not receive it.
Survival analysis
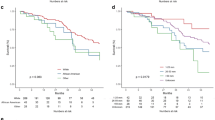
Overall median survival of this cohort of patients is 20 months (9–42.75 months), and 32 months for surviving patients with more malignant histologies (GBMs and Astroblastomas) being 17 months (7–40 months). In univariable Cox regression (Table 3), patient receiving postoperative RT sustained lower hazard ratio (HR) of 0.69 and confidence interval (CI) of 0.47–1.01 when compared to those without (p = 0.057). We also noticed that patients treated in the recent decade (years 2003–2013) had significantly better outcome compared to patients treated in years 1973–1982 (p = 0.024); however, there was no clear trend to suggest improvement of outcome throughout the years as no significance was observed for the other 2 decades. Only a trend towards significance was noted for age, with age ≥ 60 years having worse outcome compared to pediatric patients (HR = 1.59, CI [0.92, 2.75], p = 0.096). There is also a trend towards worse outcome for distal extension of tumor compared to localized tumor (HR = 1.59, CI [0.95, 2.67], p = 0.080). The Kaplan–Meier survival curve of patients by extent of surgery or postoperative RT status was illustrated in Figs. 2 and 3 respectively.
As aforementioned, a stepwise bidirectional AIC was performed, with forced inclusion of surgery extension and postoperative RT. The AIC model included tumor size, surgery, and postoperative RT. Other variables, including year of diagnosis, which demonstrated significance, was automatically excluded. In the final AIC selected multivariable Cox regression model, the extent of surgery had no significant impact on survival of patients, whereas postoperative RT remained to be a significant beneficial treatment with prolonged survival (HR = 0.54, CI [0.31, 0.95], p = 0.031).
Discussion
Patient characteristics and overall survival of spinal HGG patients
Our study explored the overall survival and effectiveness of surgical or RT treatment in patients with S-HGG in a large, population-based dataset. Concordant to previous studies, the prevalent age of onset appears to be the 3rd–4th decade of life [2, 3, 5, 11,12,13,14]. Owing to the rare occurrence, existing literature is prone to randomness from small sample size, thereby resulting invariable gender distribution, with some having only males and others having only females in the study cohort [3, 15]. In contrast, our study is statistically enabled by large sample-size via querying a population-based database, in which we found that the distribution of gender in S-HGGs is relatively balanced.
With inclusion of WHO grade III gliomas, the median survival in this cohort of patients is 20 months, longer than those with spinal GBMs, albeit concordant with previous reports on S-HGGs [2, 3, 7, 11]. Seki et al. explored the survival difference between grade III and grade IV spinal HGGs in their own series of 14 patients, and found no significant difference using log-rank test of the Kaplan–Meier curves; however, the authors specifically noted that median survival differed greatly between the two grades, with 25.5 months in grade III and 12.5 months in grade IV. The SEER dataset does not provide information regarding which spinal segment was involved. However, as evidenced in limited previous studies with S-HGGs, the distribution of S-HGGs in cervical and thoracic location were consistently reported to be approximately equal, with slightly higher proportion of thoracic lesions compared to cervical lesions, although both locations appear to have higher prevalence than lumbar location [2,3,4,5,6, 16,17,18,19]. Therefore, it can be reasonably assumed that our study cohort followed a similar distribution, and the survival associated with our study can be interpreted within the context of the described spinal segment distribution.
Prognostic factors of survival
Aside from tumor histology as aforementioned, younger age at diagnosis was also previously found to have a longer survival in these patients. In a recent retrospective study of primary GBMs by Cheng et al., a significant benefit of overall median survival was observed in younger patients, especially when using age of 40 as a cutoff. This is also consistent with another spinal cord malignant astrocytoma study by Santi et al. [14, 20]. However, in our study, only elderly patients (age ≥ 60 years) were found to have borderline significant worse prognosis than young patients, and patients age between 40 and 59 does not appear to have shorter overall median survival. Regarding the pediatric population, in a systematic review of pediatric spinal GBM patients by Konar et al., the study included 29 studies and 53 pediatric patients of ages 0–18 years, with a median survival of 10 months in the pediatric cohort, slightly worse than the generally reported median survival of 12 months for spinal GBM patients. However, the authors specifically noted that patients younger than 7 years have a better prognosis than those older than 7 years [6].
Cervical location was also reported to have a worse prognosis in patients with spinal HGGs. Seki et al. noted that when excluded patients with cervical cord lesions, the overall median survival increased from 25 to 48 months, which the authors attributed to the longer distance from lesion to brainstem [2]. This observation was also confirmed in studies including low grade spinal astrocytomas [19].
Surgery and radiation therapy on survival of spinal HGG patients
The extent of surgical resection of S-HGG patients has been controversial in the current literature. While empirically it appeared that increasing the extent of surgical resection may render improved survival of patients, data from limited literatures of different context have shown mixed results, especially in adults [2, 3, 6, 14,15,16, 19, 21, 22]. In comparison, pediatric spinal GBMs have been shown to benefit from radical surgical treatment when combined with RT [6, 23].
It must be emphasized, however, that the results of the literature need to be interpreted within the context of S-HGG instead of general spinal gliomas. In one study, McGirt and authors pointed out that the tumor grade may be an effect modifier for the relationship between extent of surgery and survival, as aggressive resection only improved survival for patients with anaplastic astrocytomas but not GBMs [16]. Of note, Adams et al. performed a SEER-based study for 135 primary malignant astrocytomas of the spinal cord and found extent of resection to be significantly associated with survival [13]. However, aside from a different population not selected by WFNS grade but by histology, another concern is the exclusion of RT in their multivariable analysis. In our analysis, we have shown that aggressive surgical resection might not be beneficial to patients (HR = 1.90). Therefore, in consideration of previous reports and results from the current study, despite a suggested aggressive regimen for S-HGGs by some which are based on the results from general spinal gliomas, there is no current evidence to support non-selective radical resection for high-grade spinal gliomas to improve survival while compromising functional status in these patients.
The benefit of postoperative RT has been revealed in multiple studies and has been advocated to be a standard treatment for these patients. One of the highlights of our study is to affirm this survival benefit of postoperative RT in S-HGG patients using a multivariable model enabled by the large sample size using the registry-based dataset. We have successfully shown that postoperative RT is associated with a 46% reduction of HR for overall survival [3, 5, 14, 15, 23].
Study limitations
Our study has several limitations that needs to be addressed for accuracy. One of the major limitations is the lack of information on chemotherapy in SEER dataset prior to the 2016 submission. This information can be crucial to the determination of effectiveness of treatment strategies, especially for patients with disseminated GBMs with early leptomeningeal infiltration. Another limitation associated with SEER database is that there is no information on the segment of spine. Although this has been addressed in our prior discussion, it is still a significant limitation to prevent us from quantifying length of survival by spine segments. Next, although the SEER database is prospectively collected, there are some inconsistencies when reconciling the WFNS grades with the actual histology of the tumor; in response to this issue, we rigorously adjusted our inclusion strategy as shown in Fig. 1 to avoid these inconsistencies. Third, the SEER database included patients since 1973, and to establish a non-selected study population we included these patients in our analysis, which may not reflect the latest RT regimen. Additionally, due to the limitation of SEER data, it is unknown whether the radiation received was intended to be definitive or palliative or adjuvant. Lastly, many of the tumors were unknown in size, posing limitation on our interpretation of tumor size effect on patient survival.
Conclusions
S-HGGs are tumors a rare occurrence with aggressive behaviors. The evidence regarding prognostic factors and effectiveness of treatment strategies has been under-reported due to limited exposure in the literature. Using a population-based approach, we have found that overall GBM constitute 70% of all S-HGGs in the population, they tend to present at age of 30–40 s, with equal male and female distribution. The overall median survival of S-HGGs is poor at 20 months, while no prognostic factors have been affirmed. More importantly, we found that extent of surgery is not associated with improved survival after adjusting for postoperative RT, and that postoperative RT remains to be the only significant factor in our study to be associated with prolonged survival for these patients. Taken together, we suggest a more prudent approach to surgical treatment of these patients, and postoperative RT should be reinforced.
References
Wong AP, Dahdaleh NS, Fessler RG et al (2013) Risk factors and long-term survival in adult patients with primary malignant spinal cord astrocytomas. J Neurooncol 115:493–503. https://doi.org/10.1007/s11060-013-1251-y
Seki T, Hida K, Yano S et al (2015) Surgical outcomes of high-grade spinal cord gliomas. Asian Spine J 9:935–941. https://doi.org/10.4184/asj.2015.9.6.935
Liu A, Sankey EW, Bettegowda C et al (2015) Poor prognosis despite aggressive treatment in adults with intramedullary spinal cord glioblastoma. J Clin Neurosci 22:1628–1631. https://doi.org/10.1016/j.jocn.2015.05.008
Shen C-X, Wu J-F, Zhao W et al (2017) Primary spinal glioblastoma multiforme: a case report and review of the literature. Medicine 96:e6634. https://doi.org/10.1097/MD.0000000000006634
Yanamadala V, Koffie RM, Shankar GM et al (2016) Spinal cord glioblastoma: 25 years of experience from a single institution. J Clin Neurosci 27:138–141. https://doi.org/10.1016/j.jocn.2015.11.011
Konar SK, Bir SC, Maiti TK, Nanda A (2017) A systematic review of overall survival in pediatric primary glioblastoma multiforme of the spinal cord. J Neurosurg Pediatr 19:239–248. https://doi.org/10.3171/2016.8.PEDS1631
Bouffet E, Allen JC, Boyett JM et al (2016) The influence of central review on outcome in malignant gliomas of the spinal cord: the CCG-945 experience. J Neurosurg Pediatr 17:453–459. https://doi.org/10.3171/2015.10.PEDS1581
Hitchon PW (2016) Letter to the editor: high-grade spinal cord glioma. J Neurosurg Spine 24:998. https://doi.org/10.3171/2015.11.SPINE151329
Matsuyama Y, Sakai Y, Katayama Y et al (2009) Surgical results of intramedullary spinal cord tumor with spinal cord monitoring to guide extent of resection. J Neurosurg Spine 10:404–413. https://doi.org/10.3171/2009.2.SPINE08698
Simonetti G, Gaviani P, Botturi A et al (2015) Clinical management of grade III oligodendroglioma. Cancer Manag Res 7:213–223. https://doi.org/10.2147/CMAR.S56975
Gu W, Gu S, Shou J, Che X (2014) Prognostic analyses of intramedullary high grade astrocytomas. Zhonghua Yi Xue Za Zhi 94:1455–1458
Garcia DM (1985) Primary spinal cord tumors treated with surgery and postoperative irradiation. Int J Radiat Oncol Biol Phys 11:1933–1939
Adams H, Avendaño J, Raza SM et al (2012) Prognostic factors and survival in primary malignant astrocytomas of the spinal cord: a population-based analysis from 1973 to 2007. Spine 37:E727–E735. https://doi.org/10.1097/BRS.0b013e31824584c0
Cheng X, Lou S, Huang S et al (2017) Primary spinal cord glioblastoma multiforme: a retrospective study of patients at a single institution. World Neurosurg. https://doi.org/10.1016/j.wneu.2017.03.120
Behmanesh B, Setzer M, Konczalla J et al (2017) Management of patients with primary intramedullary spinal cord glioblastoma. World Neurosurg 98:198–202. https://doi.org/10.1016/j.wneu.2016.10.075
McGirt MJ, Goldstein IM, Chaichana KL et al (2008) Extent of surgical resection of malignant astrocytomas of the spinal cord: outcome analysis of 35 patients. Neurosurgery 63:55–60. https://doi.org/10.1227/01.NEU.0000335070.37943.09 (discussion 60–61).
Morais N, Mascarenhas L, Soares-Fernandes JP et al (2013) Primary spinal glioblastoma: a case report and review of the literature. Oncol Lett 5:992–996. https://doi.org/10.3892/ol.2012.1076
Hernández-Durán S, Bregy A, Shah AH et al (2015) Primary spinal cord glioblastoma multiforme treated with temozolomide. J Clin Neurosci 22:1877–1882. https://doi.org/10.1016/j.jocn.2015.04.017
Nakamura M, Chiba K, Ishii K et al (2006) Surgical outcomes of spinal cord astrocytomas. Spinal Cord 44:740–745. https://doi.org/10.1038/sj.sc.3101932
Santi M, Mena H, Wong K et al (2003) Spinal cord malignant astrocytomas. Clinicopathologic features in 36 cases. Cancer 98:554–561. https://doi.org/10.1002/cncr.11514
Cooper DJ, Rosenfeld JV, Murray L et al (2011) Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med 364:1493–1502. https://doi.org/10.1056/NEJMoa1102077
Epstein FJ, Farmer JP, Freed D (1992) Adult intramedullary astrocytomas of the spinal cord. J Neurosurg 77:355–359. https://doi.org/10.3171/jns.1992.77.3.0355
Ononiwu C, Mehta V, Bettegowda C, Jallo G (2012) Pediatric spinal glioblastoma multiforme: current treatment strategies and possible predictors of survival. Childs Nerv Syst 28:715–720. https://doi.org/10.1007/s00381-012-1705-0
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Liu, J., Zheng, M., Yang, W. et al. Impact of surgery and radiation therapy on spinal high-grade gliomas: a population-based study. J Neurooncol 139, 609–616 (2018). https://doi.org/10.1007/s11060-018-2904-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2904-7