Abstract
This study aimed to examine the role of decentering and committed action as mediators of the link of external and internal shame with psychological health, in people with a chronic disease diagnosis (n = 223) and without chronic disease (n = 230). Participants with chronic disease presented higher levels of both external and internal shame. Path analysis results showed that these variables seem to be negatively linked to psychological health and that their effects on this outcome seem to be reduced by the mechanisms of decentering and committed action. The tested model explained 56% of psychological health’s variance and was invariant across groups. This study emphasizes the importance of taking a decentered stance towards internal experiences and behaving accordingly to one’s personal values on psychosocial functioning, independently of disease status. These results may have particular relevance to individuals with high levels of shame.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the past decades, the prevalence of chronic diseases has been growing in Europe along with an ageing population (Busse et al., 2010; WHO, 2018). As a consequence of increasing longevity, living with one or more chronic disease has become increasingly common (Gerteis et al., 2014; Smith & O'Dowd, 2007). Indeed, chronic health conditions implicate deep life changes with a significant impact on physical, social, and psychological functioning (e.g., Alonso et al., 2004; Forestier et al., 2019). Several studies have indeed shown that chronic diseases may have a detrimental impact on quality of life and well-being (e.g., Graham et al., 2011; Pinto-Gouveia et al., 2013). Moreover, chronic patients seem to present an increased vulnerability to several mental health problems, such as depression and anxiety (e.g., Clarke & Currie, 2009; Lotfaliany et al., 2018; Trindade et al., 2015a, 2015b). In addition, literature suggests that patients with chronic diseases, particularly those with visible symptomatology, are theoretically more vulnerable to experience higher levels of shame (e.g., Casati et al., 2000; Kellett & Gilbert, 2001).
Shame has been recognized as an unwanted and powerful self-conscious emotion (involving feelings of inferiority or inadequacy, isolation, uselessness and self-judgment; Ferreira et al., 2020) that can be incapacitating and play a central role in psychosocial functioning (e.g., Dearing & Tangney, 2011; Gilbert, 1998, 2007; Kim et al., 2011; Tangney & Dearing, 2002). Some authors have argued that it is possible to distinguish two shame dimensions: external shame and internal shame, which complement each other (e.g., Gilbert, 2003, 2009; Kim et al., 2011). In the lens of the biopsychosocial and evolutionary model, developed by Gilbert (1998, 2007), external shame emerges when individuals believe that they are being judged and seen by others as inferior, defective or unattractive due to the person´s unfavourable characteristics (such as an illness or physical attributes) or due to behaviours that can be perceived as inadequate by others. With external shame, one’s attention is focused on what is going on in the mind of others about the self (Gilbert, 1998, 2007). When this experience is internalized, it arises as a self-focused feeling named internal shame. This dimension of shame relates to negative self-evaluations about the attributes, characteristics, and behaviours that individuals perceive as unpleasant or undesired (Gilbert, 2003).
A growing body of research has shown a strong association of shame with psychopathology (e.g., Kim et al., 2011; Matos et al., 2013) and quality of life outcomes (e.g., Persons et al., 2010; Singh et al., 2016). Particularly, some studies have explored the experience of shame specifically in the context of having a chronic illness and its impact on individuals’ psychological health. Trindade et al. (2018), in a study with chronically ill patients, showed that illness-related shame is negatively associated with psychological health. In another study with a sample of inflammatory bowel disease (IBD) patients, Trindade et al. (2017b) found that illness-related shame has a detrimental impact on the psychological functioning of these patients.
There is increased recognition that the relationship between shame and psychological health can be mediated by different psychological processes (e.g., Trindade et al., 2017b). One potential and unexplored mediating processes may be decentering. Decentering is defined by the ability to observe one’s internal experiences (e.g., thoughts, feelings, emotional states) as transitory events in the mind, which do not necessarily express the reality or the self truthfully and, ultimately, do not claim any particular response (Sauer & Baer, 2010). This present-focused ability implies an acceptance and non-judgemental attitude of one’s own thoughts and feelings as they occur in the mind (e.g., instead of believing the thought “I am depressed”, an individual with decentering abilities is aware that “At this moment I am thinking that I am feeling depressed”), as opposed to self-focused forms of attention (Fresco et al., 2007). Decentering has been shown to buffer against psychopathological symptomatology (e.g., Naragon-Gainey & DeMarree, 2017; Segal et al., 2002), having a positive role on individuals’ well-being (e.g., Fresco et al., 2007; Mendes et al., 2016).
Another adaptive mechanism that seems to play an important role on psychological health and well-being is committed action. Although research on this specific process is scarce, committed action appears to be a promising construct. Indeed, committed action is a key process of the psychological flexibility model of Acceptance and Commitment Therapy (ACT; Hayes et al., 1999), defined as a present-oriented process related to a lifelong on-going pattern of effective actions that are based on personal goals and life chosen values (Hayes et al., 2006; McCracken, 2013). This process of pursuing valued life directions has an underlying persistence and flexibility in its actions and requires willingness to experience pain, discomfort and failure (McCracken, 2013; McCracken et al., 2015). Recent developments have shown that committed action is linked with a higher subjective perception of psychological health and well-being (Trindade et al., 2015a, 2015b; Trompetter et al., 2013), and decreased psychological responses to stress (Cresswell et al., 2005). Particularly, Trindade et al. (2017) showed that committed action presents negative associations with depressive and anxious symptomatology on both healthy individuals and women with breast cancer.
Considering this literature, the main goal of our study is to test an integrative model to examine the relationship between the experience of external and internal shame and psychological health, and to test whether decentering and committed action significantly influence this relationship. Given the lack of studies on internal shame, it seems particularly important to explore the relationship between each of the two shame dimensions and psychological health, in two different groups (participants with and without a chronic disease diagnosis). This allows us to compare whether these processes hold the same importance in different health contexts. We hypothesize that higher levels of shame (both external and internal) may be associated with lower levels of decentering, which in turn may explain lack of committed action, which overall tends to be associated with low psychological health.
Material and Methods
Participants
This study’s total sample included 453 Portuguese adults, which comprised two groups: participants without a chronic disease diagnosis (n = 230) and participants with chronic disease (n = 223). The group of participants without chronic disease comprised 160 women and 70 men, with ages ranging between 18 and 62 (M = 31.30; SD = 10.52) and a mean of 14.28 (SD = 2.60) years of education. Regarding the marital status of the participants without chronic disease, 34.8% were married, 60.9% single, 3.5% divorced and 0.4% widowed. The group of participants with chronic disease included 196 women and 27 men, with ages ranging from 18 to 65 (M = 38.53; SD = 11.82), and a mean of 13.97 (SD = 2.88) years of education. Concerning the marital status of the participants with chronic disease, 51.1% were married, 39% single, 7.6% divorced and 1.3% widowed. The two groups presented significant differences regarding age [t(451) = − 6.89, p < 0.001], gender [χ2(1) = 22.60; p < 0.001], and also marital status [χ2(4) = 22.80; p < 0.001]. No significant differences were found [t(451) = 1.22, p = 0.225] regarding years of education.
Concerning the group of participants with chronic disease, 174 participants (78.03%) reported having one chronic disease, and 49 participants (21.97%) reported having two or more chronic diseases. Table 1 presents a description of the chronic diseases reported by participants, grouped by organ system. The most reported diseases were lupus (33.63%), fibromyalgia (10.76%), endometriosis (9.87%), and asthma (7.62%).
Measures
External and Internal Shame Scale (EISS; Ferreira et al., 2020)
EISS, Ferreira et al. (2020) measures the experience of shame in two dimensions: external and internal shame. The EISS comprises 8 items, which assess four domains of the experience of shame through two items (one related to the external dimension and one related to the internal dimension): inferiority/inadequacy (e.g., “I am different and inferior to others”), sense of isolation/exclusion (e.g., “Other people don’t understand me”), uselessness/emptiness (e.g., “I am unworthy as a person”) and criticism/judgment (e.g., “Others are judgmental and critical of me”). The items are rated on a 5-point scale, ranging from 0 (“Never”) to 4 (“Always”), according to the frequency of shame experiences. In the original study, Cronbach's alpha values were 0.80 and 0.82 for the external and internal shame subscales, respectively (Ferreira et al., 2020).
Experiences Questionnaire (EQ; Fresco et al., 2007; Gregório et al., 2015)
The EQ is a 11-item self-report instrument designed to assess decentering in daily experiences (e.g., “I can separate myself from my thoughts and feelings”), rated on a 5-point Likert scale from 1 (“Never”) to 5 (“Always”). Higher scores indicate a greater capacity to observe one’s thoughts and feelings as temporary events and separated from the self. The EQ presented good internal reliability, both in the original version (α = 0.83; Fresco et al., 2007) and in the Portuguese validation study (α = 0.81; Gregório et al., 2015).
Committed Action Questionnaire (CAQ-8; McCracken et al., 2015; Trindade et al., 2017a, b, c)
The 8-item version of the CAQ measures committed action, as conceptualized in ACT. The CAQ-8 has two subscales, one positively phrased (e.g., “I can remain committed to my goals even when there are times that I fail to reach them”) and one negatively phrased (e.g., “I find it difficult to carry on with an activity unless I experience that it is successful”), each with 4 items. CAQ-8 presented a α of 0.87 (McCracken et al., 2015). The Portuguese version also revealed good internal consistency (α = 0.79 for the breast cancer sample and of 0.86 for the healthy sample; Trindade et al., 2017a, b, c).
World Health Organization Brief Quality-of-Life Assessment Scale (WHOQOL-BREF; WHOQOL Group, 1998; Canavarro et al., 2007)
This self-report instrument assesses one’s subjective perception of their quality of life (QoL) through 24 items distributed in four specific QoL’s domains (physical, psychological, social relationships and environment) and two additional items which evaluate general QoL and general health. The items are rated on a 5-point Likert scale, with higher scores demonstrating a higher perceived QoL. Given the aim of the current study, only the psychological health (WHOQOL_Psyc) domain was used. This instrument presented psychometric adequacy in its original study (α ranging from 0.66 to 0.84; WHOQOL Group, 1998) and in the Portuguese validation study (α ranging from 0.67 to 0.87; Canavarro et al., 2007).
The alphas for the variables considered in the current study are reported in Table 2.
Procedures
The sample was recruited through online advertisements on the social network Facebook (exponential discriminative snowball sampling technique). The invitation included information regarding the general aims of the study and the target population (adults aged between 18 and 65). The voluntary nature of the participation, and the anonymity and confidentiality of the data were also assured.
Data was collected between November 2018 and March 2019. All participants gave their informed consent before participating. In order to obtain a larger sample of chronic patients, thirty-two Portuguese chronic patients associations were asked to advertise the study. Of the contacted associations, seven replied and agreed to collaborate in sample recruitment.
The initial sample was composed of 471 participants. However, considering the purpose of the study, 18 participants were excluded: 16 participants of the group with chronic disease were excluded from the database (14 were over 65, 1 reported having a disease but did not indicate which one, and 1 reported having psychiatric illness); 2 participants from the group without chronic disease were excluded (1 was under 18 years old, and the other indicated did not provide informed consent).
Data Analyses
Data analysis was conducted using IBM SPSS 20 (IBM Corp, 2011). Descriptive statistics were conducted to analyze the characteristics of the two groups (participants with and without chronic disease diagnosis). Independent t tests were conducted to estimate mean differences between groups. Pearson product-moment correlations were calculated to examine the associations between study variables (Cohen et al., 2003). Path analysis, a form of structural equation modeling (SEM; MacKinnon, 2008), was performed to examine the associations between study variables in the theoretical proposed model. This procedure enables both the analysis of structural associations and the exploration of the significance of direct and indirect effects between variables, while controlling for errors. To test regression coefficients and fit statistics, Maximum Likelihood was used as estimation method. To examine the model’s fit to empirical data, a set of goodness-of-fit indices were used: the Comparative Fit Index (CFI), the Tucker Lewis Index (TLI) and the Root Mean Square of Approximation (RMSEA). CFI and TLI are both indicative of a very good fit when values are above 0.95 (Hu & Bentler, 1999; Kline, 2005). RMSEA was examined considering that values between 0.05 and 0.08 indicate a good fit. The Bootstrap resampling procedure, with 5000 samples, was used to test the significance of the paths, with 95% bias-corrected confidence intervals (CIs) around the standardized estimates of total, direct and indirect effects (Kline, 2005).
A multi-group analysis was conducted to test whether the path coefficients are equal or invariant between groups (Byrne, 2010). For this purpose, the unconstrained (i.e., with free structural parameter coefficients) and the constrained models (i.e., where the parameters are constrained to be equal across groups) were compared. The non-significant result of the χ2 difference test indicate that the invariance tests claimed are supported (Byrne, 2010). Path analysis and multi-group analysis were performed using AMOS (v.22; Arbuckle, 2013).
Results
Descriptive and Correlation Analyses
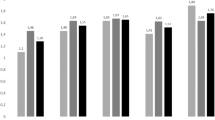
Descriptive and t-test results are reported in Table 2. Results indicated that, in comparison with the group without chronic disease, the group with chronic disease reported higher levels of external and internal shame and lower levels of decentering, committed action, and psychological health.
Correlation results (Table 3) indicated that, in both groups, the two dimensions of shame (external and internal) presented moderate to strong negative correlations with decentering and committed action. Regarding psychological health, strong negative correlations with both external and internal shame were found. In contrast, strong positive correlations between psychological health with decentering and committed action were found. Finally, in the group without chronic disease, age did not present significant correlations with any variable. The same was found for the chronic disease group with an exception: age presented a significant (albeit weak) association with external shame.
Path Analysis
A path analysis was performed to explore whether decentering and committed action mediated the link between external and internal shame with psychological health, using the total sample (N = 453). First, this model was tested through a fully saturated model (i.e., zero degrees of freedom), comprising 26 parameters. The initial analysis of the model indicated that one path was non-significant: the direct effect of external shame on committed action (bEISS_Ext = − 0.26; SEb = 0.14; Z = − 1.92; p = 0.055). This path was eliminated, and the model was readjusted.
The final model’s (Fig. 1) path coefficients were all statistically significant (p < 0.001) and explained 56% of psychological health’s variance. Moreover, the model accounted for 31% of committed action, as well as decentering. The model presented an excellent model fit to the empirical data, as indicated by the analysis of the goodness of fit indices [χ2(1) = 3.68; p = 0.055; CFI = 1.00; TLI = 0.97; RMSEA = 0.08, CI = 0.00 to 0.17, p = 0.198].
Specifically, external shame presented a significant direct effect on decentering of − 0.16 (bEISS_Ext = − 0.39; SEb = 0.13; Z = − 2.96; p = 0.003) and of − 0.14 on psychological health (bEISS_Ext = − 0.84; SEb = 0.27; Z = − 3.16; p = 0.002). In turn, internal shame had a significant direct effect on decentering of − 0.43 (bEISS_Int = − 0.96; SEb = 0.12; Z = − 7.89; p < 0.001), of − 0.30 on committed action (bEISS_Int = − 0.69; SEb = 0.11; Z = − 6.42; p < 0.001), and of − 0.33 on psychological health (bEISS_Int = − 1.81; SEb = 0.27; Z = − 6.79; p < 0.001). It was also verified that decentering had a significant direct effect on committed action of 0.33 (bEQ = 0.35; SEb = 0.05; Z = 7.12; p < 0.001) and on psychological health of 0.30 (bEQ = 0.74; SEb = 0.10; Z = 7.44; p < 0.001). Finally, committed action also presented a significant direct effect on psychological health of 0.15 (bCAQ-8 = 0.37; SEb = 0.09; Z = 4.02; p < 0.001).
The analysis of indirect effects showed that internal shame had indirect effects of − 0.14 on committed action through decentering (95% CI − 0.20 to − 0.10), and indirect effects of − 0.20 on psychological health through committed action and decentering (95% CI − 0.27 to − 0.13). In turn, external shame had an indirect effect of − 0.05 on committed action through decentering (95% CI − 0.11 to − 0.02); and an indirect effect of − 0.06 on psychological health through committed action and decentering (95% CI − 0.10 to 0.02). Finally, decentering had indirect effects of 0.05 on psychological health through committed action (95% CI 0.02 to 0.09).
To sum up, the model revealed that decentering and committed action mediated the link between external and internal shame with psychological health. Further, results from this model also demonstrated that decentering seems to explain the effect of external shame on committed action.
Multi-Group Analysis
Before undertaking the invariance tests, the path model’s analyses were separately conducted for both groups, which confirmed goodness-of-fit for both chronic disease (CFI = 1.00) and without chronic (CFI = 0.99) groups. Therefore, the invariance tests were conducted. Results from the Chi-square difference test between the unconstrained [χ2(2) = 6.44, p = 0.040] and the constrained [χ2(10) = 18.04, p = 0.054] models showed that the model was invariant for the two groups [χ2dif (8) = 11.60, p = 0.170]. Thus, at the model-level, the studied associations seem to present no significant differences across the studied groups. Lastly, critical ratio differences were calculated to test differences between both groups regarding parameter estimates. Results revealed that two parameters’ coefficients had statistically significant differences between groups: the relationship between external shame and decentering (Z = − 2.08, p < 0.05) and the relationship between internal shame and decentering (Z = 2.25, p < 0.05). This result showed that the relationship between external shame and decentering was significant only for the chronic disease group. Further, both groups presented a significant relationship between internal shame and decentering, but chronic disease group presented a lower estimate compared to the group without chronic disease.
Discussion
The present study sought to explore the differences between two groups, people with and without chronic disease diagnosis, regarding the experience of shame in its two dimensions (external and internal shame) and psychological health, as well as regarding to two adaptive psychological processes (decentering abilities and committed action). Although some studies have demonstrated the impact of shame on psychological functioning and well-being in the context of chronic disease, they do not differentiate external shame from internal shame, or focus on chronic illness-related shame exclusively (e.g., Trindade et al., 2018; Trindade et al., 2017a, b, c). Thus, our study added new data to the literature in this area. Moreover, this study intended to clarify the role of decentering abilities and committed action as potential mediators of the links of external and internal shame with psychological health.
Results allowed to verify that individuals with chronic disease presented higher levels of external and internal shame compared to individuals without a diagnosis of chronic disease. These data are in line with previous findings (e.g., Casati et al., 2000; Kellett & Gilbert, 2001; Trindade et al., 2017b) and extend them with findings on internal shame. Regarding the studied processes, the individuals without chronic disease reported higher levels of decentering and committed action compared to individuals with chronic disease. Specifically, the group with chronic disease seems to reveal a greater difficulty to take a decentered stance towards internal experiences, and a lesser tendency to engage in actions consistent with one’s personal values, which goes against results reported by other studies (e.g., McCracken, 2013). Similarly to Coutinho et al.s’ results (2019) and as expected, these two groups also differed in relation to psychological health, as the group with chronic disease scored lower in this domain.
Results from correlation analyses showed an identical pattern of relationship between variables in both groups. More specifically, results revealed strong negative associations of external and internal shame with psychological health, both for individuals with and without chronic disease. This result is consistent with literature that documented the adverse effects of shame on psychological functioning (e.g., Kim et al., 2011). In the group without chronic disease, decentering and committed action presented strong positive associations with psychological health, while in the chronic disease group, decentering was strongly and positively associated with psychological health, while committed action was moderately and positively associated with this outcome. These results seem to evidence the importance of promoting these psychological processes, both in healthy and ill populations.
To better understand the link between the studied variables, a theoretical model was tested via path analysis. The tested model hypothesized that external and internal shame may explain psychological health through decentering and committed action. This model explained 56% of the variance of psychological health and presented an adequate fit to the empirical data. Results showed that decentering abilities and committed action partially mediate the link of both external and internal shame on psychological health, which goes in line with our hypothesis.
Finally, a multi-group analysis revealed that these results were invariant across participants with and participants without chronic disease at the model level. Nevertheless, the link between shame and decentering was not invariant between the groups. External shame’s effect on decentering was only significant for the chronic disease group. Internal shame’s effect on decentering was significant for both groups, but stronger for the group of people without chronic disease. These data suggest that external shame plays a more significant role in the explanation of decentering in people with chronic disease than in people without chronic disease. In the latter, it is internal shame that seems to explain decentering. Overall, these findings seem to indicate that, in the presence of chronic disease, believing that one is judged and seen by as inferior by others may limit one’s ability to decenter from internal experiences, while in people without chronic disease it is self-evaluations that seem to influence one’s decentering abilities.
These findings cannot be considered without note some limitations. First, the cross‐sectional nature of this study does not allow the inference of causal directions between the variables. In this line, future research should be developed based on longitudinal designs. Secondly, the recruitment method (online survey) and the use of self-report measures may be susceptible to produce sample bias and does not allow the generalization of data. Thus, future studies could benefit from the use of different research methods and assessment measures (e.g., structured interviews) to confirm our findings. Another important limitation refers to the size and representability of the sample. Future research should replicate the tested model using larger samples, and in groups of people with the same chronic disease diagnosis.
These findings appear nonetheless to be promising and to have important implications, namely in the context of behavioural medicine, by showing that feelings of inadequacy or inferiority, either by perceiving a negative external evaluation or an internal negative appreciation, may negatively influence perceived psychological health. The ability to distance oneself from internal experiences and to perceive these negative internal events as transient, may lead to the engagement in actions committed to life values, and together, these two processes seem to diminish the influence of shame on psychological functioning. This seems to shed some light on the importance of decentering and committed action as adaptive mechanisms for psychological health, in both healthy and ill populations.
References
Alonso, J., Ferrer, M., Gandek, B., Ware, J. E., Aaronson, N. K., Mosconi, P., & Leplège, A. (2004). Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 13(2), 283–298. https://doi.org/10.1023/B:QURE.0000018472.46236.05
Arbuckle, J. L. (2013). Amos 2.20 User’s Guide. IBM SPSS.
Busse, R., Scheller-Kreinsen, D., & Zentner, A. (2010). Tackling chronic disease in Europe: strategies, interventions and challenges. Observatory Studies (No. 20). WHO Regional Office Europe.
Byrne, B. M. (2010). Structural Equation Modeling with AMOS. Routledge.
Canavarro, M. C., Simões, M. R., Vaz Serra, A., Pereira, M., Rijo, D., Quartilho, M., & Carona, C. (2007). WHOQOL-Bref Instrumento de Avaliação da Qualidade de Vida da Organização Mundial de Saúde [WHOQOLBref Quality of Life Assessment Instrument from the World Health Organization]. In M. R. Simões, M. M. Gonçalves & Almeida, L. S. (Coord.) Avaliação Psicológica: 46 Instrumentos válidos para a população portuguesa (Vol. III, pp. 77–100). Quarteto.
Casati, J., Toner, B. B., de Rooy, E. C., Drossman, D. A., & Maunder, R. G. (2000). Concerns of patients with inflammatory bowel disease: A review of emerging themes. Digestive Diseases and Sciences, 45, 26–31. https://doi.org/10.1023/A:105492806777
Clarke, D. M., & Currie, K. C. (2009). Depression, anxiety and their relationship with chronic diseases: A review of the epidemiology, risk and treatment evidence. The Medical Journal of Australia, 190(7), S54–S60. https://doi.org/10.5694/j.1326-5377.2009.tb02471.x
Cohen, J., Cohen, P., West, S., & Aiken, L. (2003). Applied multiple regression/correlation analysis for the behavioural sciences (3rd ed.). Lawrence Erlbaum Associates.
Coutinho, M., Trindade, I. A., & Ferreira, C. (2019). Experiential avoidance, committed action and quality of life: Differences between college students with and without chronic illness. Journal of Health Psychology. https://doi.org/10.1177/1359105319860167
Cresswell, J. D., Welch, W. T., Taylor, S. E., Sherman, D. K., Gruenewald, T. L., & Mann, T. (2005). Affirmation of personal values buffers neuroendocrine and psychological stress response. Psychological Science, 16, 846–851. https://doi.org/10.1111/j.1467-9280.2005.01624.x
Dearing, R. L., & Tangney, J. P. (Eds.). (2011). Shame in the therapy hour. APA Books.
Ferreira, C., Moura-Ramos, M., Matos, M., & Galhardo, A. (2020). A new measure to assess external and internal shame: Development, factor structure and psychometric properties of the External and Internal Shame Scale. Current Psychology. https://doi.org/10.1007/s12144-020-00709-0
Fresco, D. M., Moore, M. T., van Dulmen, M. H. M., Segal, Z. V., Ma, S. H., Teasdale, J. D., & Williams, J. M. G. (2007). Initial psychometric properties of the Experiences Questionnaire: Validation of a self-report measure of decentering. Behavior Therapy, 38, 234–246. https://doi.org/10.1016/j.beth.2006.08.003
Forestier, B., Anthoine, E., Reguiai, Z., Fohrer, C., & Blanchin, M. (2019). A systematic review of dimensions evaluating patient experience in chronic illness. Health and Quality of Life Outcomes, 17(19), 1–13. https://doi.org/10.1186/s12955-019-1084-2
Gilbert, P. (1998). What is shame? Some core issues and controversies. In P. Gilbert & B. Andrews (Eds.), Shame: Interpersonal behaviour, psychopathology and culture (pp. 3–36). Oxford University Press.
Gilbert, P. (2003). Evolution, social roles and the differences in shame and guilt. Social Research: An International Quarterly, 70(4), 1205–1230.
Gilbert, P. (2007). The evolution of shame as a marker for relationship security. In J. L. Tracy, R. W. Robins, & J. P. Tangney (Eds.), The self-conscious emotions: Theory and research (pp. 283–309). Guilford.
Gilbert, P. (2009). The compassionate mind: A new approach to the challenge of life. Constable & Robinson.
Gerteis, J., Izrael, D., Deitz, D., LeRoy, L., Ricciardi, R., Miller, T., & Basu, J. (2014). Multiple Chronic Conditions Chartbook. AHRQ Publications No, Q14-0038. Agency for Healthcare Research and Quality.
Graham, C. D., Rose, M. R., Grunfeld, E. A., Kyle, S. D., & Weinman, J. (2011). A systematic review of quality of life in adults with muscle disease. Journal of Neurology, 258(9), 1581–1592. https://doi.org/10.1007/s00415-011-6062-5
Gregório, S., Pinto-Gouveia, J., Duarte, C., & Simões, L. (2015). Expanding Research on Decentering as Measured by the Portuguese Version of the Experiences Questionnaire. Spanish Journal of Psychology, 18, 1–14. https://doi.org/10.1017/sjp.2015.18
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 1–25. https://doi.org/10.1016/j.brat.2005.06.006
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. Guilford Press.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
IBM Corp Released. (2011). IBM SPSS Statistics for Windows, Version 20.0. IBM Corp.
Kellett, S., & Gilbert, P. (2001). Acne: A biopsychosocial and evolutionary perspective with a focus on shame. British Journal of Health Psychology, 6, 1–24. https://doi.org/10.1348/135910701169025
Kim, S., Thibodeau, R., & Jorgensen, R. S. (2011). Shame, guilt, and depressive symptoms: A meta-analytic review. Psychological Bulletin, 137(1), 68–96. https://doi.org/10.1037/a0021466
Kline, R. B. (2005). Principle and practice of structural equation modeling. Guilford.
Lotfaliany, M., Bowe, S. J., Kowal, P., Orellana, L., Berck, M., & Mohebbi, M. (2018). Depression and chronic diseases: Co-occurrence and communality of risk factors. Journal of Affective Disorders. https://doi.org/10.1016/j.jad.2018.08.011
MacKinnon, D. P. (2008). Introduction to statistical mediation analysis. Erlbaum.
Matos, M., Pinto-Gouveia, J., & Duarte, C. (2013). Internalizing early memories of shame and lack of safeness and warmth: The mediating role of shame on depression. Behavioural and Cognitive Psychoterapy, 41, 479–493. https://doi.org/10.1017/S1352465812001099
McCracken, L. M. (2013). Committed action: An application of the psychological flexibility model to activity patterns in chronic pain. The Journal of Pain, 14(8), 828–835. https://doi.org/10.1016/j.pain.2013.02.009
McCracken, L. M., Chilcot, J., & Norton, S. (2015). Further development in the assessment of psychological flexibility: A shortened committed action questionnaire (CAQ-8). European Journal of Pain, 19, 677–685. https://doi.org/10.1002/ejp.589
Mendes, A. L., Ferreira, C., & Marta-Simões, J. (2016). Experiential avoidance versus decentering abilities: The role of different emotional processes on disordered eating. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, 22(3), 467–474. https://doi.org/10.1007/s40519-016-0291-7
Naragon-Gainey, K., & DeMarree, K. G. (2017). Decentering attenuates the association of negative affect and positive affect with psychopathology. Clinical Psychological Sciece. https://doi.org/10.1177/2167702617719758
Persons, E., Kershaw, T., Sikkema, K. J., & Hansen, N. B. (2010). The impact of shame on health-related quality of life among HIV-positive adults with a history of childhood sexual abuse. AIDS Patient Care and STDs, 24(9), 571–580. https://doi.org/10.1089/apc.2009.0209
Pinto-Gouveia, J., Duarte, C., Matos, M., & Fráguas, S. (2013). The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychology and Psychotherapy. https://doi.org/10.1002/cpp.1838
Sauer, S., & Baer, R. A. (2010). Mindfulness and decentering as mechanisms of change in mindfulness-and-acceptance-based interventions. In R. A. Baer (Ed.), Assessing mindfulness and acceptance processes in clientes: Illuminating the theory and practice of change (pp. 25–42). New Harbinger Publications Inc.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press.
Singh, S., Wetterneck, C. T., Williams, M. T., & Knott, L. E. (2016). The role of shame and symptom severity on quality of life in obsessive-compulsive and related disorders. Journal of Obsessive-Compulsive and Related Disorders, 11, 49–55. https://doi.org/10.1016/j.jocrd.2016.08.004
Smith, S., & O’Dowd, T. (2007). Chronic diseases: What happens when they come in multiples? British Journal of General Practice, 57(537), 268–270.
Tangney, J. P., & Dearing, R. L. (2002). Shame and guilt. Guilford Press.
Trindade, I. A., Duarte, J., Ferreira, C., Coutinho, M., & Pinto-Gouveia, J. (2018). The impact of illness-related shame on psychological health and social relationships: Testing a mediational model in students with chronic illness. Clinical Psychology and Psychotherapy, 25(3), 408–414. https://doi.org/10.1002/cpp.2175
Trindade, I. A., Ferreira, C., & Pinto-Gouveia, J. (2015a). Ulcerative colitis symptomatology and depression: The exacerbator role of maladaptive psychological processes. Digestive Diseases and Sciences, 60(12), 3756–3763. https://doi.org/10.1007/s10620-015-3786-6
Trindade, I. A., Ferreira, C., Pinto-Gouveia, J., & Nooren, L. (2015b). Clarity of personal values and committed action: Development of a shorter Engaged Living Scale. Journal of Psychopathology and Behavior Assesment, 38(2), 258–265. https://doi.org/10.1007/s10862-015-9509-7
Trindade, I. A., Ferreira, C., & Pinto-Gouveia, J. (2017a). Chronic illness-related shame: Development of a new scale and novel approach for IBD patients’ depressive symptomatology. Clinical Psychology and Psychotherapy, 24(1), 255–263. https://doi.org/10.1002/cpp.2035
Trindade, I. A., Ferreira, C., & Pinto-Gouveia, J. (2017b). Shame and emotion regulation in inflammatory bowel disease: Effects on psychosocial functioning. Journal of Health Psychology. https://doi.org/10.1177/1359105317718925
Trindade, I. A., Marta-Simões, J., Ferreira, C., & Pinto-Gouveia, J. (2017c). Developments on committed action: Validity of the CAQ-8 and analysis of committed action’s role in depressive symptomatology in breast cancer patients and healthy individuals. Clinical Psychology and Psychotherapy, 25(1), e42–e50. https://doi.org/10.1002/cpp.2125
Trompetter, H. R., Ten Klooster, P. M., Schreurs, K. M., Fledderus, M., Westerhof, G. H., & Bohlmeijer, E. T. (2013). Measuring values and committed action with engaged living scale (ELS): Psychometric evaluation in a nonclinical sample and a chronic pain sample. Psychological Assessment, 4, 1235–1246. https://doi.org/10.1037/a0033813
WHO. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychological Medicine, 28, 551–558. https://doi.org/10.1017/S0033291798006667
World Health Organization. (2018). Noncommunicable diseases. Retrieved from https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases
Acknowledgements
We would like to thank the Association for the Support of Patients with Leukemia and Lymphoma, Portuguese Lung Foundation, National Association of Cystic Fibrosis, Portuguese Federation of People with Diabetes, Portuguese Association for Supporting Women with Endometriosis, Portuguese League Against Rheumatic Diseases, and Portuguese Association of Renal Insufficient for their help during the recruitment process of the sample of patients with physical chronic disease.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Authors CF and IAT designed the study, prepared the measures and wrote the protocol. Author IM-P recruited and assessed the participants. All the authors conducted literature research and provided summaries of previous research studies, conducted the statistical analysis and wrote the manuscript throughout its development stages. CF supervised and contributed throughout the conduction of these tasks and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Inês Matos-Pina, Inês A. Trindade, and Cláudia Ferreira declares that they have no conflict of interest.
Informed consent
All participants gave their informed consent before participating.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The present study was approved by the Ethical Board of the Faculty of Psychology and Education Sciences of the University of Coimbra.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matos-Pina, I., Trindade, I.A. & Ferreira, C. Internal and External Shame in Healthy and Chronically Ill Samples: Exploring Links to Psychological Health. J Clin Psychol Med Settings 29, 412–420 (2022). https://doi.org/10.1007/s10880-022-09855-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-022-09855-y