Abstract
The primary end point when treating acute shock is to restore blood circulation, mainly by reaching macrocirculatory parameters. However, even if global haemodynamic goals can be achieved, microcirculatory perfusion may remain impaired, leading to cellular hypoxia and organ damage. Interestingly, few methods are currently available to measure the adequacy of organ blood flow and tissue oxygenation. The rise in tissue partial pressure of carbon dioxide (CO2) has been observed when tissue perfusion is decreased. In this regard, tissue partial pressure of CO2 has been proposed as an early and reliable marker of tissue hypoxia even if the mechanisms of tissue partial pressure in CO2 rise during hypoperfusion remain unclear. Several technologies allow the estimation of CO2 content from different body sites: vascular, tissular (in hollow organs, mucosal or cutaneous), and airway. These tools remain poorly evaluated, and some are used but are not widely used in clinical practice. The present review clarifies the physiology of increasing tissue CO2 during hypoperfusion and underlines the specificities of the different technologies that allow bedside estimation of tissue CO2 content.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
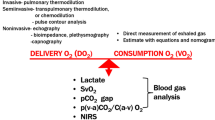
Early resuscitation of shock states has been recommended by guidelines from medical societies for several years [1], and to optimise treatment, macrocirculatory parameters are generally used [1]. However, even if targeted macrocirculatory parameters are obtained, microcirculatory disturbances can persist, leading to organ dysfunction. Indeed, the generally recommended assessment of global haemodynamic parameters [1] may fail to reflect both the imbalance between oxygen demand–oxygen supply and the status of the microcirculation [2]. Moreover, in various situations, such as septic shock, alterations in metabolic pathways called “cytopathic hypoxia” can lead to additional tissue damage [3].
There have been many approaches to assessing the specific adequacy of tissue perfusion. Clinical evaluation of tissue perfusion consists of measurements, such as the capillary refill time, the skin temperature of the distal parts of the body (fingers, toes, earlobe and nose), and the presence of mottled skin [4]. Although the monitoring of tissue oxygenation adequacy is more difficult to achieve in critically ill patients, various techniques to estimate microcirculatory perfusion may reveal microcirculatory impairment in diverse situations (laser Doppler blood flow, side stream dark field imaging, near infra-red spectroscopy, etc.) [2, 3, 5–7].
Increase in tissue CO2 has been observed when tissue perfusion is inadequately low due to a stagnation phenomenon [8] and/or “non-metabolic production” [9]. Therefore, the monitoring of tissue PCO2 may allow the identification of altered microcirculatory perfusion. Although mechanisms leading to this increase in tissue PCO2 in shock are not well understood, these variations seem to be related to tissue perfusion. The measurement of CO2 and the estimation of tissue CO2 content can be obtained using diverse techniques applied to a variety of sites in and on the body.
In the present review, we will first discuss the physiology of CO2 metabolism in the tissue and then describe several available methods for estimating the tissular CO2 content, notably during low flow states.
2 Metabolism of CO2
The first descriptions of energy metabolism were proposed by Lavoisier, Priestley and Black over 200 years ago. These pioneers demonstrated that to produce energy (i.e., heat), combustion needed oxygen as a substrate. Most cellular activities require energy that is mainly obtained from the degradation of adenosine triphosphate (ATP). ATP generation requires oxygen that must be present in sufficient amounts in the mitochondria to allow the generation of an adequate concentration of ATP via the Krebs’ cycle and the electron transport system. Under aerobic conditions, oxygen consumption (\(\dot{\text{V}}\)O2) depends on the basal metabolic activity of tissue and any additional energy requirements (physical activity, fever, etc.) results in a further increase in \(\dot{\text{V}}\)O2. Conversely, factors that decrease \(\dot{\text{V}}\)O2 include starvation, hypothermia, and general anaesthesia [10]. In critically ill patients, \(\dot{\text{V}}\)O2 is generally increased [10, 11] and the magnitude of the increase in \(\dot{\text{V}}\)O2 may range from 20 % after surgery, 60 % in severe sepsis, up to 100 % in patients with large burns [10].
The substrates of energy metabolism also influence \(\dot{\text{V}}\)O2 for a given metabolic rate, as different amounts of oxygen are required for the production of the same amount of energy from carbohydrate, fat or protein. Therefore, in steady states, \(\dot{\text{V}}\)O2 varies despite a same level of energy expenditure, according to the substrate utilised [12].
During ATP generation, CO2 is produced (\(\dot{\text{V}}\)CO2). This production is not directly related to oxygen but from the oxidation of substrates during the process. The ratio between CO2 production (\(\dot{\text{V}}\)CO2) and O2 consumption (\(\dot{\text{V}}\)O2) associated with metabolic processes at a cellular level is called the respiratory quotient (RQ = \(\dot{\text{V}}\)CO2/\(\dot{\text{V}}\)O2). The respiratory quotient generally varies between 0.7 and 1 and is related to the predominant metabolic substrate (for example when lipids are used, R = 0.7, but when glucose is the main substrate, R = 1, resulting in more CO2 produced for the same oxygen consumption). Because \(\dot{\text{V}}\)CO2 is related to the metabolic rate in steady state, the same factors that influence \(\dot{\text{V}}\)O2 also affect \(\dot{\text{V}}\)CO2. However, the expected change in \(\dot{\text{V}}\)CO2 is not necessarily equal to the change in \(\dot{\text{V}}\)O2. For example, when the metabolic rate is increased as a result of injury or sepsis, fat metabolism tends to increase and the RQ decreases [12–14].
The rise in partial pressure of carbon dioxide (PCO2) in tissue has been observed in critically ill patients with shock. To explain this phenomena, several hypotheses have been suggested though the main mechanism is unclear and remains a source of debate [15].
First, an increase in metabolism is associated with higher production of CO2 by cells; however, this increase in production is associated with a parallel increase in blood flow due to the regulatory role of oxygen demand in tissues. As a result, the CO2 produced by the augmentation of metabolism is cleared by the blood flow due to the washout phenomenon (CO2 ‘’dilution’’) so that tissue PCO2 remains constant [16]. Conversely, in low flow states, tissular CO2 increases are related to an imbalance between CO2 production and a decreased washout, whereas the washout effect seems to be predominant.
A second hypothesis has suggested that “anaerobic metabolism” occurs with specific conditions (ischemia, mitochondrial dysfunction, etc.), resulting in the production of lactate and hydrogen (H+) protons (metabolic acidosis) by the tissue. In the present setting, the excess of protons produced during cellular hypoxia is buffered by bicarbonate ions and results in a rise of CO2 (“non-metabolic CO2”) inside the extracellular space (Fig. 1) [9, 17–22].
The model for lactic acid buffering by bicarbonate, explaining the relative increase of CO2 during “non-aerobic metabolism”. This effect can be measured at different places: tissular: site 1; venous-arterial difference (Delta PCO2): site 2; respiratory gases (\(\dot{\text{V}}\)CO2/\(\dot{\text{V}}\)O2): site 3 (redraw from [22])
Once produced, CO2 is distributed in three different forms. First, as CO2 is excessively soluble, CO2 is mainly dissolved and diffuses readily across tissue, equilibrating with blood or the immediate environment (gastric space for example). Second, depending on the chemical characteristics of the surrounding environment (pH, temperature, Haldane effect, etc.) and the presence of carbonic anhydrase (present in red blood cells), CO2 equilibrates with the HCO3 content according to the following computation: CO2 + H2O = H2CO3 − + H+. Finally, CO2 may combine with other compounds (protein).
As a result, the interpretation of tissue CO2 content is complex as it is influenced by both aerobic production, non-metabolic production [9, 20], flow stagnation, impaired washout of CO2 [23–25] and the distribution of the various forms. However, the concept that tissue CO2 levels rise sharply during low flow conditions and/or tissue hypoxia remains relevant [26, 27] and carbon dioxide monitoring may help achieve the goal of adequate resuscitation during shock [28–33].
3 Methods of measurement
3.1 Venous to arterial CO2 difference
The arterio-venous difference in carbon dioxide tension (ΔPCO2) can be calculated after simultaneous sampling of arterial and mixed venous blood: ΔPCO2 = PvCO2 − PaCO2. This parameter can be considered as a marker of the adequacy of the venous blood flow to remove the CO2 produced by the peripheral tissues [34, 35]. Therefore, ΔPCO2 has been proposed as a marker of low flow-induced tissue hypoxia and organ damage.
Experimentally, in an animal model of acute haemorrhage, Van der Linden and colleagues found a significant correlation between blood lactate levels and ΔPCO2 during a bleeding protocol [36]. A progressive increase in ΔPCO2 was observed during the \(\dot{\text{V}}\)O2/DO2 dependent period with progressive flow reduction [37]. Vallet et al. [38] showed that the veno-arterial CO2 difference, representing the local production of an isolated perfused limb tissue submitted to hypoxia, increased only if the present model was associated with low flow conditions (hypoxic ischemia), but not when the model was absolute hypoxia alone (hypoxic hypoxia). These observations supported the hypothesis that the increase in pCO2 was related to a stagnation phenomenon. When the blood flow was preserved, even under hypoxic conditions, the veno-arterial CO2 difference did not increase because the blood flow was able to remove the CO2 produced from peripheral tissue (wash out phenomenon). Thus, the rise in tissue PCO2 may be a reliable sign that blood flow is decreasing [16].
Several clinical studies have shown that ΔPCO2 and cardiac index are inversely correlated in circulatory failure [37, 39–43]. Moreover, a high value of ΔPCO2 is associated with a poor outcome in surgical patients [18]. Bakker studied patients with septic shock and showed that the ΔPCO2 was smaller in survivors than in non-survivors, despite a similar cardiac index, DO2 and \(\dot{\text{V}}\)O2 indices [43]. In a recent review, Lamia and collaborators suggested that ΔPCO2 could be considered as a marker of the adequacy of venous blood flow to remove the total CO2 produced by the peripheral tissues in shock, as an increase in venous return is the principal determinant of an increase in venous CO2 clearance [44]. The present statement means that changes in venous CO2 clearance could be a good predictor of changes in cardiac output and venous return.
Similarly, an inverse correlation has been found between central venous to arterial carbon dioxide tension difference and cardiac index, suggesting that a central venous blood sample is sufficient, instead of a pulmonary arterial mixed blood sample, for the measurement and interpretation of the venous to arterial CO2 difference [45]. Indeed, ΔPCO2 could even be considered as a better indirect assessment of systemic blood flow than ScVO2 in resuscitated septic-shock patients [46]. This could be explained by the fact that O2 supply may adapt to the tissue O2 extraction capabilities although the bulk tissue perfusion remains insufficient to wash out the accumulating tissue CO2 produced by the resuscitated metabolism. In this regard, It has been shown that a ΔPCO2 > 6 mmHg may help identify patients who remain inadequately resuscitated during septic shock or high risk surgery and could, in this context, serve as a complementary tool to SvO2 for goal directed therapy [20, 46].
In a medical ICU, an increase in ΔPCO2 was reported in 10 patients with low cardiac output due to congestive heart failure in the absence of global hypoxia as demonstrated by the normal lactate level [47]. These findings emphasise the lack of specificity of ΔPCO2 in detecting tissue hypoxia. However, with serum lactate as a traditional indicator of tissue hypoxia, increased lactate clearance by the liver may delay the detection of elevated (or decreased) lactate levels in the blood [48]. Moreover, lactate that is produced must be transported in the blood to be adequately measured, so that local non-perfusion may fail to washout lactate that is produced and may ‘stagnate’ in the tissue (mesenteric ischaemia, compartment syndrome, etc.).
3.2 Combination of veno-arterial PCO2 difference with arterio-venous PO2 difference
In critically ill patients with tissue hypoperfusion, Mekontso-Dessap and colleagues showed a close correlation between blood lactate concentration and the ratio of veno-arterial difference in PCO2 to arterio-venous difference in O2 (ΔPCO2/ΔPO2), obtained via a pulmonary arterial catheter. Furthermore, there was no correlation between blood lactate concentration and ΔPCO2 alone and blood lactate concentration and ΔPO2 alone [49]. Therefore, the present study suggests that the ΔPCO2/ΔPO2 ratio may be more relevant than O2 derived and CO2 derived parameters taken individually. The present finding was also confirmed recently by Monnet et al. [50] using venous samples obtained through a central venous catheter, which suggested that anaerobic parameters should be taken into account during resuscitation.
3.3 Gastric tonometry
There is much evidence showing that the splanchnic region is particularly vulnerable to shock, and this site seems to be a sensitive target for detecting early signs of hypoperfusion [51]. The principle of gastric tonometry is based on the measurement of PCO2 in the lumen of the stomach given its equilibrium with the gastric mucosa CO2 by diffusion. If local haemodynamics are compromised, the tissue CO2 that accumulates is detected in the lumen of the organ [51]. The gastric tonometer consists of a standard nasogastric tube with a silicone balloon at the end. The CO2 diffuses from the gastric mucosa and equilibrates with the content inside the balloon (gas or saline). A sample of the content in the balloon is withdrawn, and the pCO2 is determined (Fig. 2). Monitoring of gastric intra-mucosal carbon dioxide pressure (PgCO2) has been demonstrated to be a marker of gastric mucosal dysoxia and a predictor of morbidity and mortality in critically ill patients [9], with a strong prognostic value [52, 53]. Monitoring of gastric intra-mucosal pH was initially proposed. However, the partial pressure of the carbon dioxide (PCO2) gap, defined as the difference between gastric mucosal PCO2 (PgCO2) and arterial PCO2, may more specifically reflect the adequacy of gastric mucosal blood flow [54] and may also be an independent factor in predicting mortality [55].
Principle of gastric tonometry (see text) (from [88])
However, the clinical use of gastric tonometry is cumbersome, and the interpretation of related measurements could be complex as the procedure suffers from methodological limitations. Gastroc tonometry is challenging to perform at the bedside (enteral feeding and acid suppressive must be avoided) and, moreover, the measurements are dependent on the time required to reach equilibration (approximately 15 min). The latter leads to a delayed responsiveness to therapeutic interventions [35, 56]. For all of these reasons, gastric tonometry has not gain widespread acceptance and has fallen into disuse (Table 1).
In addition to the gastric space, other locations have been proposed for evaluating tissue CO2. Sato and colleagues, then later Totapally and colleagues, found identical changes in CO2 using oesophageal and gastric tonometry in models of shock, and presumed that oesophageal tonometry could serve as a convenient alternative to gastric tonometry [57, 58]. The midgut or sigmoid have also been proposed as potential anatomic sources that could provide the same type of information. However, these procedures have not been used as the former is difficult to access and the latter is technically more challenging than gastric tonometry, with potential methodological artefacts resulting from bacterial production of CO2 [59].
3.4 Sublingual capnometry
Sublingual capnometry is simple, non-invasive, and inexpensive as well as could provide near instantaneous information about the adequacy of gastrointestinal tissue perfusion in critically ill patients, even if the anatomical perfusion differs from the distal gut. The present measurement is based on a carbon sensing diode containing a fluorescent indicator that is excited by light conducted through an optical fibre and then transmits the fluorescent emission back to the instrument [9].
It has been found that the tongue may behave functionally as part of the splanchnic circulation; indeed, it was demonstrated that in the case of decreased perfusion, blood flow to the sublingual region and splanchnic bed falls to a similar degree [60, 61]. In a heterogeneous group of ICU patients, an excellent correlation was found between sublingual and gastric intra-mucosal tissue CO2 [29]. Weil et al. observed parallel alterations between sublingual capnometry and gastric tonometry, suggesting that both areas could be equally affected during shock [31]. The present technology has already been correlated with the severity of shock [16] and could be a useful method for discriminating between survivors and non-survivors among critically ill patients, with a potentially superior responsiveness to therapy than lactate [30]. Unfortunately, the device is no longer commercially available (Table 1) [35].
3.5 Transcutaneous CO2 (ear lobe)
Measurement of PCO2 on the surface of human skin was first described in 1960 by Severinghaus [62]. Transcutaneous measurement of PCO2 makes use of the fact that CO2 gas diffuses through body tissue and skin and can be detected by a sensor at the skin surface [63]. The concept is based on the occurrence of local hyperaemia induced by warming the skin, which increases the supply of arterial blood to the dermal capillary bed underneath the sensor. Second, a correction algorithm is applied to take into account the elevation of temperature [63]. According to the method described by Severinghaus and Bradley, the CO2 is measured potentiometrically by determining the pH of an electrolyte layer separated from the skin by a highly permeable membrane [64]. The change in pH is proportional to the logarithm of the change in PCO2. The pH is determined by measuring the potential between a miniaturised pH glass electrode and an Ag/AgCl reference electrode (Fig. 3) [63].
Electrode of Severinghaus, combined with a SpO2 sensor on an ear lobe (see text) (from [63])
A transcutaneous PCO2 device could potentially reflect the partial pressure in arterial blood after arterialisation of the skin by local warming. This technique has been evaluated in the ICU where, using an ear lobe sensor as a surrogate for PaCO2, it has been shown to be both safe and feasible. It may be an acceptable method for monitoring trends that correlate well with PaCO2, independent of PaCO2 levels [65, 66].
More recently, Vallee et al. [67] used this cutaneous sensor method, attached to an ear lobe and calibrated to 37 °c, to estimate the tissue PCO2 in patients in septic shock. They show that the cutaneous ear lobe CO2 at inclusion was significantly higher in patients with septic shock than in the control group, and they demonstrated a significantly greater gradient between cutaneous CO2 and arterial CO2 or PETCO2 in patients in septic shock compared to the control group. The values of these gradients during a fluid challenge seemed to decrease in conjunction with an improvement in the microcirculatory parameters, as evaluated by skin blood flow [67].
3.6 Capnography: end tidal CO2 (PETCO2)
Capnography is the standard of care for monitoring the adequacy of ventilation and the proper placement of the endotracheal tube in patients receiving general anaesthesia and is increasingly being used to monitor patients who are receiving mechanical ventilation in intensive care units. This technique is used to approximate the blood partial pressure in carbon dioxide and to aid in the assessment and treatment of patients in cardiac arrest [68]. Indeed, this method allows for non-invasive and continuous monitoring of carbon dioxide levels and can provide valuable information regarding the respiratory condition of the patient [69].
The capnogram characterizes the concentration of carbon dioxide versus time in a gas sample throughout the respiratory cycle [70]. The PCO2 of the last alveolar gas that was exhaled past the airway opening is defined as the end-tidal CO2 (PETCO2). However, the capnogram does not contain information about volume. The continuous measurement of CO2 in the absence of exhaled flow can artificially create a horizontal tail on the alveolar plateau of the capnogram [70].
While a variety of techniques can be used to measure PETCO2, infrared absorption spectroscopy is typically used in clinical practice. Infrared light can be passed through a sample of gas to an infrared detector. As the concentration of carbon dioxide increases, the intensity of the light that reaches the detector decreases as the carbon dioxide gas strongly absorbs the infrared light (e.g., approx. 4.3 microns). At this wavelength, there is minimal spectral interference from other gases that may also be present (water, oxygen, nitrous oxide, and inhaled anaesthetic agents) [69].
Two types of capnographs exist. Mainstream capnographs use sensors that are placed directly into the breathing circuit of a ventilator, and sidestream capnographs draw a sample of gas away from the breathing circuit e.g. 50–150 ml/min sample flow rate. The response of a sidestream device to detect changes in CO2 concentrations is delayed by a few seconds (e.g., 3 s) because the gas must travel through the sampling line before being analysed [69].
Exhaled CO2 is mainly determined in haemodynamically stable conditions by the relationship between pulmonary blood flow and alveolar ventilation [71]. Therefore, PETCO2 is related to the CO2 delivered to the lung (blood content in CO2) and the adequacy of pulmonary elimination of blood CO2. It is approximately equal to the arterial CO2 if the ventilation/perfusion characteristics of the lung are within the normal range and the arterial-PETCO2 difference is in the normal range from 4 to 6 mmHg. [72]. Unfortunately, the correlation between PETCO2 and PaCO2 is not perfect and varies with dead space, shunt, and ventilation/perfusion mismatching [70, 71].
During a cardiac arrest, PETCO2 is very low. This reflects the low cardiac output resulting from cardio-pulmonary resuscitation, despite high levels in CO2 in tissue that, in turn, results from poor clearance. However, it has been shown that higher levels of PETCO2 reflect better cardiac output during resuscitation, and a greater likelihood of successful resuscitation. A PETCO2 < 10 mmHg after 20 min of specialised cardio-pulmonary life support could be predictive of mortality [68].
Acute changes in PETCO2 have been shown to correlate strongly with changes in cardiac output in experimental [73, 74] and clinical settings. Consequently, the present method has been proposed as a non-invasive alternative to continuous assessment of cardiac output in different shock states [75]. Dubin and colleagues [73] compared PETCO2 and cardiac output and found a good correlation in dogs submitted to haemorrhagic shock, with the greatest decrease in PETCO2 in the lowest flow states. Similarly, Adrogue et al. [76] demonstrated a correlation between cardiac output and PETCO2 in dogs submitted to pharmacologic vasodilatation, haemorrhage, increased intra-thoracic pressure and cardiac arrest. The lowest PETCO2 was found when the cardiac output was severely compromised.
More recently, two clinical studies have evaluated the end tidal CO2 as an assessment of fluid responsiveness in critically ill patients during a passive leg raising test. These authors compared the CO2 parameter to cardiac output computed by haemodynamic monitors, the PiCCO (Pulsion Medical Systems, Munich, Germany) or the CardioQ-ODM oesophageal Doppler monitor (Deltex Medical, Chicester, UK) [77, 78]. It appears that the changes in PETCO2 induced by a passing leg raising test was predictive of fluid responsiveness in mechanically ventilated patients in shock and was more accurate than pulse pressure variations. Nevertheless, lung function and compensatory mechanisms may preserve relatively normal PETCO2 values until moderate to severe falls in cardiac output and haemodynamic instability, rendering PETCO2 monitoring relatively insensitive or less sensible in “pre-shock” conditions. This can be explained by the logarithmic relationship between PETCO2 and cardiac output shown in a previous experimental study [73]. Moreover, for Levine and colleagues, “EtCO2 provides useful, additional information, but is not sufficient as an independent monitoring system/diagnostic device to change our current practice” [79].
3.7 \(\dot{\text{V}}\)CO2 and respiratory quotient
Early in the twentieth century, Benedict and Atwater demonstrated that heat production in humans could be determined indirectly by measuring respiratory gas exchange and computing the corresponding heat production from the energy content of nutrients. Indirect calorimetry, that is to say the measure of oxygen consumption as a measure of the amount of oxygen taken up from the respiratory gases (\(\dot{\text{V}}\)O2) and CO2 production (\(\dot{\text{V}}\)CO2) directly to the airway, was then accepted as a method for measuring energy expenditure and substrate utilisation in humans. The results obtained from gas exchange measurements (indirect calorimetry) are identical with actual metabolic state only when the CO2 and the O2 pools of the body are in steady state. The ratio in then called the respiratory exchange ratio and is equivalent to the respiratory quotient.
The ability to measure gas exchange in critically ill patients provides new insight into the physiology and management of nutrition. Metabolic measurements using indirect calorimetry are an aid to evaluating the patient’s nutritional assessment and to developing a plan of management. In addition, measuring the oxygen cost of breathing is clinically beneficial because it avoids inducing excessive work of breathing. As an example, in patients with mechanical ventilation, continuous monitoring of \(\dot{\text{V}}\)O2 has been described as a useful method for predicting the success of weaning from mechanical ventilation [80–82] and can also evaluate the relationship between O2 delivery and consumption [83, 84].
However, there are some drawbacks of the method. The measurement of \(\dot{\text{V}}\)CO2 is sensitive to changes in ventilation. Any change in the ventilation setting will directly affect the measured \(\dot{\text{V}}\)CO2 until a new steady state has been reached. Similarly, changes in the breathing pattern will also influence \(\dot{\text{V}}\)CO2 because changes in tidal volume will alter the dead space to tidal volume ratio, even if the ventilation per minute remains unchanged. Finally, if the production of CO2 remains constant, changes in the ventilatory setting could affect PaCO2. As a result, a new steady state is only reached after a delay before the amount of CO2 removed by ventilation can correspond exactly to the metabolic production of CO2 [11].
For this reason, historically, the study of carbon dioxide kinetics in the body has been mostly confined to equilibrium conditions (steady states). Study of gas kinetics during non-steady-states are few and have required the development of new technologies [70]. In this purpose, a new metabolic module (E-COVX module, Datex-Ohmeda, Helsinki, Finland) has been developed to be used specifically in mechanically ventilated patients [85, 86]. This device has been compared with a validated metabolic monitor (Deltatrac II Datex-Ohmeda, Helsinki, Finland) under controlled steady state conditions, thereby opening the way for its utilisation in intensive care settings. The correlation and the agreement between the two methods (the new one and the Gold-Standard) were equally adequate, with an unvarying reproducibility at high inspired oxygen concentrations values, [85].
Perturbations in the airway respiratory quotient have been used in athletes as well as in individuals with cardiac disease. During voluntary exercise, the airway respiratory quotient increases when the ventilatory threshold is reached. At this stage, the increase in airway O2 consumption is associated with a disproportionate increase in airway CO2 production, a phenomenon that occurs concomitantly to acidosis and lactatemia [87].
The airway respiratory quotient has been observed to fluctuate in response to tissue perfusion states in clinical settings as well. Cohen et al. [22] showed that the airway respiratory quotient increases in experimental haemorrhagic shock in swine and decreases as shock is reversed during resuscitation. This was similarly explained by a decrease in \(\dot{\text{V}}\)O2 relative to shock, but a lesser decrease in \(\dot{\text{V}}\)CO2 due to increasing CO2 in tissue despite the decrease in metabolism. As an example of the present finding, we present here an observation of the same phenomenon in a patient admitted to our intensive care unit for shock (Fig. 4). The authors believe that the present concept could be of interest when monitoring shocked patients. This method may be useful for detecting increases in CO2 in tissue during shock or hypoperfusion because it can be monitored continuously and non-invasively. However, the present method requires that the patient be well adapted to the ventilator, while simultaneously maintaining control of all the metabolic demands and ventilation settings. Further studies are necessary to confirm the potential use of this device during shock.
4 Perspectives, conclusion
Hypoperfusion leading to multi-organ failure is a frequent issue observed in critically ill patients and cannot always be predicted by measuring classic macrohaemodynamic parameters. In this regard, tissue pressure carbon dioxide monitoring may be useful for this purpose. Several sensitive, non- invasive techniques and devices with validated effectiveness at the bedside have been proposed for clinical use. Unfortunately, these techniques have limitations. In addition, blood flow repartition across each organ cannot be assessed. However, monitoring the adequacy of microcirculation as a part of the global haemodynamic by evaluating the tissue CO2 content could help clinicians to implement or adapt a patient’s therapy to assure the best organ perfusion.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228. doi:10.1007/s00134-012-2769-8.
Ince C. The microcirculation is the motor of sepsis. Crit Care. 2005;9(Suppl 4):S13–9. doi:10.1186/cc3753.
Spronk PE, Zandstra DF, Ince C. Bench-to-bedside review: sepsis is a disease of the microcirculation. Crit Care. 2004;8(6):462–8. doi:10.1186/cc2894.
Ait-Oufella H, Lemoinne S, Boelle PY, Galbois A, Baudel JL, Lemant J, Joffre J, Margetis D, Guidet B, Maury E, Offenstadt G. Mottling score predicts survival in septic shock. Intensive Care Med. 2011;37(5):801–7. doi:10.1007/s00134-011-2163-y.
Neviere R, Mathieu D, Chagnon JL, Lebleu N, Millien JP, Wattel F. Skeletal muscle microvascular blood flow and oxygen transport in patients with severe sepsis. Am J Respir Crit Care Med. 1996;153(1):191–5.
Lima A, Bakker J. Noninvasive monitoring of peripheral perfusion. Intensive Care Med. 2005;31(10):1316–26. doi:10.1007/s00134-005-2790-2.
Schober P, Schwarte LA. From system to organ to cell: oxygenation and perfusion measurement in anesthesia and critical care. J Clin Monit Comput. 2012;26(4):255–65. doi:10.1007/s10877-012-9350-4.
De Backer D, Creteur J. Regional hypoxia and partial pressure of carbon dioxide gradients: what is the link? Intensive Care Med. 2003;29(12):2116–8.
Marik PE. Regional carbon dioxide monitoring to assess the adequacy of tissue perfusion. Curr Opin Crit Care. 2005;11(3):245–51.
Huang YC. Monitoring oxygen delivery in the critically ill. Chest. 2005;128(5 Suppl 2):554S–60S. doi:10.1378/chest.128.5_suppl_2.554S.
Viale JP, Annat G, Bertrand O, Delafosse B, Percival C, Bui-Xuan B, Motin J. Continuous measurement of gas exchange during artificial ventilation. Ann Fr Anesth Reanim. 1986;5(4):424–9.
Peronnet F, Meyer T, Aguilaniu B, Juneau CE, Faude O, Kindermann W. Bicarbonate infusion and pH clamp moderately reduce hyperventilation during ramp exercise in humans. J Appl Physiol. 2007;102(1):426–8. doi:10.1152/japplphysiol.00559.2006.
Caresta E, Pierro A, Chowdhury M, Peters MJ, Piastra M, Eaton S. Oxidation of intravenous lipid in infants and children with systemic inflammatory response syndrome and sepsis. Pediatr Res. 2007;61(2):228–32. doi:10.1203/01.pdr.0000252441.91671.e5.
Samra JS, Summers LK, Frayn KN. Sepsis and fat metabolism. Br J Surg. 1996;83(9):1186–96.
Peronnet F, Aguilaniu B. Lactic acid buffering, nonmetabolic CO2 and exercise hyperventilation: a critical reappraisal. Respir Physiol Neurobiol. 2006;150(1):4–18. doi:10.1016/j.resp.2005.04.005.
Almac E, Siegemund M, Demirci C, Ince C. Microcirculatory recruitment maneuvers correct tissue CO2 abnormalities in sepsis. Minerva Anestesiol. 2006;72(6):507–19.
Whipp BJ, Ward SA, Lamarra N, Davis JA, Wasserman K. Parameters of ventilatory and gas exchange dynamics during exercise. J Appl Physiol. 1982;52(6):1506–13.
Silva JM Jr, Oliveira AM, Segura JL, Ribeiro MH, Sposito CN, Toledo DO, Rezende E, Malbouisson LM. A large venous-arterial PCO(2) is associated with poor outcomes in surgical patients. Anesthesiol Res Pract. 2011;2011:759792. doi:10.1155/2011/759792.
Schlichtig R, Bowles SA. Distinguishing between aerobic and anaerobic appearance of dissolved CO2 in intestine during low flow. J Appl Physiol. 1994;76(6):2443–51.
Futier E, Robin E, Jabaudon M, Guerin R, Petit A, Bazin JE, Constantin JM, Vallet B. Central venous O(2) saturation and venous-to-arterial CO(2) difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care. 2010;14(5):R193. doi:10.1186/cc9310.
Randall HM Jr, Cohen JJ. Anaerobic CO2 production by dog kidney in vitro. Am J Physiol. 1966;211(2):493–505.
Cohen IL, Sheikh FM, Perkins RJ, Feustel PJ, Foster ED. Effect of hemorrhagic shock and reperfusion on the respiratory quotient in swine. Crit Care Med. 1995;23(3):545–52.
Dubin A, Murias G, Estenssoro E, Canales H, Badie J, Pozo M, Sottile JP, Baran M, Palizas F, Laporte M. Intramucosal-arterial PCO2 gap fails to reflect intestinal dysoxia in hypoxic hypoxia. Crit Care. 2002;6(6):514–20.
Grum CM, Fiddian-Green RG, Pittenger GL, Grant BJ, Rothman ED, Dantzker DR. Adequacy of tissue oxygenation in intact dog intestine. J Appl Physiol. 1984;56(4):1065–9.
Guzman JA, Kruse JA. Development and validation of a technique for continuous monitoring of gastric intramucosal pH. Am J Respir Crit Care Med. 1996;153(2):694–700.
Fries M, Weil MH, Chang YT, Castillo C, Tang W. Microcirculation during cardiac arrest and resuscitation. Crit Care Med. 2006;34(12 Suppl):S454–7. doi:10.1097/01.CCM.0000247717.81480.B2.
Weil MH, Sun S. Tissue capnometry. Crit Care Med. 2001;29(2):460.
Fink MP. Tissue capnometry as a monitoring strategy for critically ill patients: just about ready for prime time. Chest. 1998;114(3):667–70.
Marik PE. Sublingual capnography: a clinical validation study. Chest. 2001;120(3):923–7.
Marik PE, Bankov A. Sublingual capnometry versus traditional markers of tissue oxygenation in critically ill patients. Crit Care Med. 2003;31(3):818–22. doi:10.1097/01.CCM.0000054862.74829.EA.
Weil MH, Nakagawa Y, Tang W, Sato Y, Ercoli F, Finegan R, Grayman G, Bisera J. Sublingual capnometry: a new noninvasive measurement for diagnosis and quantitation of severity of circulatory shock. Crit Care Med. 1999;27(7):1225–9.
Fang X, Tang W, Sun S, Huang L, Chang YT, Castillo C, Weil MH. Comparison of buccal microcirculation between septic and hemorrhagic shock. Crit Care Med. 2006;34(12 Suppl):S447–53. doi:10.1097/01.CCM.0000246011.86907.3A.
Ristagno G, Tang W, Sun S, Weil MH. Role of buccal PCO2 in the management of fluid resuscitation during hemorrhagic shock. Crit Care Med. 2006;34(12 Suppl):S442–6. doi:10.1097/01.CCM.0000247722.24781.D0.
Groeneveld AB. Interpreting the venous-arterial PCO2 difference. Crit Care Med. 1998;26(6):979–80.
Dres M, Monnet X, Teboul JL. Hemodynamic management of cardiovascular failure by using PCO(2) venous-arterial difference. J Clin Monit Comput. 2012;26(5):367–74. doi:10.1007/s10877-012-9381-x.
Van der Linden P, Rausin I, Deltell A, Bekrar Y, Gilbart E, Bakker J, Vincent JL. Detection of tissue hypoxia by arteriovenous gradient for PCO2 and pH in anesthetized dogs during progressive hemorrhage. Anesth Analg. 1995;80(2):269–75.
Zhang H, Vincent JL. Arteriovenous differences in PCO2 and pH are good indicators of critical hypoperfusion. Am Rev Respir Dis. 1993;148(4 Pt 1):867–71.
Vallet B, Teboul JL, Cain S, Curtis S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol. 2000;89(4):1317–21.
Durkin R, Gergits MA, Reed JF 3rd, Fitzgibbons J. The relationship between the arteriovenous carbon dioxide gradient and cardiac index. J Crit Care. 1993;8(4):217–21.
Groeneveld AB, Vermeij CG, Thijs LG. Arterial and mixed venous blood acid-base balance during hypoperfusion with incremental positive end-expiratory pressure in the pig. Anesth Analg. 1991;73(5):576–82.
Mecher CE, Rackow EC, Astiz ME, Weil MH. Venous hypercarbia associated with severe sepsis and systemic hypoperfusion. Crit Care Med. 1990;18(6):585–9.
Rackow EC, Astiz ME, Mecher CE, Weil MH. Increased venous-arterial carbon dioxide tension difference during severe sepsis in rats. Crit Care Med. 1994;22(1):121–5.
Bakker J, Vincent JL, Gris P, Leon M, Coffernils M, Kahn RJ. Veno-arterial carbon dioxide gradient in human septic shock. Chest. 1992;101(2):509–15.
Lamia B, Monnet X, Teboul JL. Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol. 2006;72(6):597–604.
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, Pamukov N, Horst HM. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med. 2005;31(6):818–22. doi:10.1007/s00134-005-2602-8.
Vallee F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, Samii K, Fourcade O, Genestal M. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 2008;34(12):2218–25. doi:10.1007/s00134-008-1199-0.
Teboul JL, Mercat A, Lenique F, Berton C, Richard C. Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med. 1998;26(6):1007–10.
Levraut J, Ciebiera JP, Chave S, Rabary O, Jambou P, Carles M, Grimaud D. Mild hyperlactatemia in stable septic patients is due to impaired lactate clearance rather than overproduction. Am J Respir Crit Care Med. 1998;157(4 Pt 1):1021–6.
Mekontso-Dessap A, Castelain V, Anguel N, Bahloul M, Schauvliege F, Richard C, Teboul JL. Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med. 2002;28(3):272–7. doi:10.1007/s00134-002-1215-8.
Monnet X, Julien F, Ait-Hamou N, Lequoy M, Gosset C, Jozwiak M, Persichini R, Anguel N, Richard C, Teboul JL. Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit Care Med. 2013;41(6):1412–20. doi:10.1097/CCM.0b013e318275cece.
Chapman MV, Mythen MG, Webb AR, Vincent JL. Report from the meeting: gastrointestinal tonometry: state of the art. 22nd–23rd May 1998, London, UK. Intensive Care Med. 2000;26(5):613–22.
Friedman G, Berlot G, Kahn RJ, Vincent JL. Combined measurements of blood lactate concentrations and gastric intramucosal pH in patients with severe sepsis. Crit Care Med. 1995;23(7):1184–93.
Oud L, Haupt MT. Persistent gastric intramucosal ischemia in patients with sepsis following resuscitation from shock. Chest. 1999;115(5):1390–6.
Schlichtig R, Mehta N, Gayowski TJ. Tissue-arterial PCO2 difference is a better marker of ischemia than intramural pH (pHi) or arterial pH–pHi difference. J Crit Care. 1996;11(2):51–6.
Levy B, Gawalkiewicz P, Vallet B, Briancon S, Nace L, Bollaert PE. Gastric capnometry with air-automated tonometry predicts outcome in critically ill patients. Crit Care Med. 2003;31(2):474–80. doi:10.1097/01.CCM.0000050445.48656.28.
Russell C. Comment on Vieillard-Baron et al.: “Bedside echocardiographic evaluation of hemodynamics in sepsis: is qualitative evaluation sufficient?”. Intensive Care Med. 2007; 33(6):1106; author reply 1107. doi:10.1007/s00134-007-0611-5.
Sato Y, Weil MH, Tang W, Sun S, Xie J, Bisera J, Hosaka H. Esophageal PCO2 as a monitor of perfusion failure during hemorrhagic shock. J Appl Physiol. 1997;82(2):558–62.
Totapally BR, Fakioglu H, Torbati D, Wolfsdorf J. Esophageal capnometry during hemorrhagic shock and after resuscitation in rats. Crit Care. 2003;7(1):79–84.
Walley KR, Friesen BP, Humer MF, Phang PT. Small bowel tonometry is more accurate than gastric tonometry in detecting gut ischemia. J Appl Physiol. 1998;85(5):1770–7.
Jin X, Weil MH, Sun S, Tang W, Bisera J, Mason EJ. Decreases in organ blood flows associated with increases in sublingual PCO2 during hemorrhagic shock. J Appl Physiol. 1998;85(6):2360–4.
Nakagawa Y, Weil MH, Tang W, Sun S, Yamaguchi H, Jin X, Bisera J. Sublingual capnometry for diagnosis and quantitation of circulatory shock. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1838–43.
Severinghaus J. Carbon dioxide tension and perfusion in the tissue. Anaesthesist. 1960;9:50–5.
Eberhard P. The design, use, and results of transcutaneous carbon dioxide analysis: current and future directions. Anesth Analg. 2007;105(6 Suppl):S48–52. doi:10.1213/01.ane.0000278642.16117.f8.
Severinghaus JW, Bradley AF. Electrodes for blood pO2 and pCO2 determination. J Appl Physiol. 1958;13(3):515–20.
Bendjelid K, Schutz N, Stotz M, Gerard I, Suter PM, Romand JA. Transcutaneous PCO2 monitoring in critically ill adults: clinical evaluation of a new sensor. Crit Care Med. 2005;33(10):2203–6.
Rodriguez P, Lellouche F, Aboab J, Buisson CB, Brochard L. Transcutaneous arterial carbon dioxide pressure monitoring in critically ill adult patients. Intensive Care Med. 2006;32(2):309–12. doi:10.1007/s00134-005-0006-4.
Vallee F, Mateo J, Dubreuil G, Poussant T, Tachon G, Ouanounou I, Payen D. Cutaneous ear lobe Pco(2) at 37 degrees C to evaluate microperfusion in patients with septic shock. Chest. 2010;138(5):1062–1070. doi:10.1378/chest.09-2690.
Levine RL, Wayne MA, Miller CC. End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest. N Engl J Med. 1997;337(5):301–6. doi:10.1056/NEJM199707313370503.
Ortega R, Connor C, Kim S, Djang R, Patel K. Monitoring ventilation with capnography. N Engl J Med. 2012;367(19):e27. doi:10.1056/NEJMvcm1105237.
Breen PH, Isserles SA, Taitelman UZ. Non-steady state monitoring by respiratory gas exchange. J Clin Monit Comput. 2000;16(5–6):351–60. doi:10.1023/A:1011447500984.
West JB. Respiratory physiology: the essentials. 4th ed. Baltimore: Williams & Wilkins; 1990.
Nunn JF, Hill DW. Respiratory dead space and arterial to end-tidal carbon dioxide tension difference in anesthetized man. J Appl Physiol. 1960;15:383–9.
Dubin A, Murias G, Estenssoro E, Canales H, Sottile P, Badie J, Baran M, Rossi S, Laporte M, Palizas F, Giampieri J, Mediavilla D, Vacca E, Botta D. End-tidal CO2 pressure determinants during hemorrhagic shock. Intensive Care Med. 2000;26(11):1619–23.
Ornato JP, Garnett AR, Glauser FL. Relationship between cardiac output and the end-tidal carbon dioxide tension. Ann Emerg Med. 1990;19(10):1104–6.
Jin X, Weil MH, Tang W, Povoas H, Pernat A, Xie J, Bisera J. End-tidal carbon dioxide as a noninvasive indicator of cardiac index during circulatory shock. Crit Care Med. 2000;28(7):2415–9.
Adrogue HJ, Rashad MN, Gorin AB, Yacoub J, Madias NE. Arteriovenous acid-base disparity in circulatory failure: studies on mechanism. Am J Physiol. 1989;257(6 Pt 2):F1087–93.
Monge Garcia MI, Gil Cano A, Gracia Romero M, Monterroso Pintado R, Perez Madueno V, Diaz Monrove JC. Non-invasive assessment of fluid responsiveness by changes in partial end-tidal CO2 pressure during a passive leg-raising maneuver. Ann Intensive Care. 2012;2:9. doi:10.1186/2110-5820-2-9.
Monnet X, Bataille A, Magalhaes E, Barrois J, Le Corre M, Gosset C, Guerin L, Richard C, Teboul JL. End-tidal carbon dioxide is better than arterial pressure for predicting volume responsiveness by the passive leg raising test. Intensive Care Med. 2013;. doi:10.1007/s00134-012-2693-y.
Levine RL. End-tidal CO2: physiology in pursuit of clinical applications. Intensive Care Med. 2000;26(11):1595–7.
Miwa K, Mitsuoka M, Takamori S, Hayashi A, Shirouzu K. Continuous monitoring of oxygen consumption in patients undergoing weaning from mechanical ventilation. Respiration. 2003;70(6):623–30.
McDonald NJ, Lavelle P, Gallacher WN, Harpin RP. Use of the oxygen cost of breathing as an index of weaning ability from mechanical ventilation. Intensive Care Med. 1988;14(1):50–4.
Shikora SA, Bistrian BR, Borlase BC, Blackburn GL, Stone MD, Benotti PN. Work of breathing: reliable predictor of weaning and extubation. Crit Care Med. 1990;18(2):157–62.
Danek SJ, Lynch JP, Weg JG, Dantzker DR. The dependence of oxygen uptake on oxygen delivery in the adult respiratory distress syndrome. Am Rev Respir Dis. 1980;122(3):387–95.
Kaufman BS, Rackow EC, Falk JL. The relationship between oxygen delivery and consumption during fluid resuscitation of hypovolemic and septic shock. Chest. 1984;85(3):336–40.
McLellan S, Walsh T, Burdess A, Lee A. Comparison between the Datex-Ohmeda M-COVX metabolic monitor and the Deltatrac II in mechanically ventilated patients. Intensive Care Med. 2002;28(7):870–6. doi:10.1007/s00134-002-1323-5.
Briassoulis G, Michaeloudi E, Fitrolaki DM, Spanaki AM, Briassouli E. Influence of different ventilator modes on Vo(2) and Vco(2) measurements using a compact metabolic monitor. Nutrition. 2009;25(11–12):1106–14. doi:10.1016/j.nut.2009.01.018.
Davis JA, Whipp BJ, Lamarra N, Huntsman DJ, Frank MH, Wasserman K. Effect of ramp slope on determination of aerobic parameters from the ramp exercise test. Med Sci Sports Exerc. 1982;14(5):339–43.
Ackland G, Grocott MP, Mythen MG. Understanding gastrointestinal perfusion in critical care: so near, and yet so far. Crit Care. 2000;4(5):269–81. doi:10.1186/cc709.
Conflict of interest
The authors declare that they have no conflict of interest in relationship with this article entitled.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Danin, PE., Siegenthaler, N., Levraut, J. et al. Monitoring CO2 in shock states. J Clin Monit Comput 29, 591–600 (2015). https://doi.org/10.1007/s10877-014-9638-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9638-7