Abstract
Regional tissue distress caused by microcirculatory dysfunction and mitochondrial depression underlies the condition in sepsis and shock where, despite correction of systemic oxygen delivery variables, regional hypoxia and oxygen extraction deficit persist. We have termed this condition microcirculatory and mitochondrial distress syndrome (MMDS). Orthogonal polarization spectral imaging allowed the first clinical observation of the microcirculation in human internal organs, and has identified the pivotal role of microcirculatory abnormalities in defining the severity of sepsis, a condition not revealed by systemic hemodynamic or oxygen-derived variables. Recently, sublingual sidestream dark-field (SDF) imaging has been introduced, allowing observation of the microcirculation in even greater detail. Microcirculatory recruitment is needed to ensure adequate microcirculatory perfusion and the oxygenation of tissue cells that follows. In sepsis, where inflammation-induced autoregulatory dysfunction persists and oxygen need is not matched by supply, the microcirculation can be recruited by reducing pathological shunting, promoting microcirculatory perfusion, supporting pump function, and controlling hemorheology and coagulation. Resuscitation following MMDS must include focused recruitment of hypoxic-shunted microcirculatory units and/or resuscitation of the mitochondria. A combination of agents is required for successful rescue of the microcirculation. Single compounds such as activated protein C, which acts on multiple pathways, can be expected to be beneficial in rescuing the microcirculation in sepsis.
Similar content being viewed by others
Introduction
The recent development of new medical imaging techniques, together with data from clinical investigations, has helped to identify the microcirculation as playing a key role in sepsis [1]. The array of pathogenic factors that occur in sepsis affects almost every cellular component of the microcirculation, including endothelial cells, smooth muscle cells, leukocytes, erythrocytes, and tissue cells. If not corrected directly, a poorly functioning microvasculature can lead to respiratory distress in tissue cells further fuelling microcirculatory dysfunction in a cascade of pathogenic mechanisms leading to organ failure (Fig. 1). Sakr and colleagues [2] showed that microcirculatory distress not corrected for 24 hours was the single independent factor predicting patient outcome. The central role of the microcirculation in providing oxygen to the tissue cells makes it of prime importance in determining organ function. Microcirculatory dysfunction persisting for extended periods of time can act as a motor driving the pathogenic effects of sepsis leading to organ failure in much the same way as the gut was considered to be the motor of multiorgan failure [3].
The microcirculation is the motor of sepsis. Circulatory failure as a result of sepsis can be initiated by various insults such as trauma, infection, and shock. Its treatment is initially based on correction of systemic variables. Microcirculatory distress can persist and remain undetected, a condition termed microcirculatory and mitochondrial distress syndrome (MMDS). Here, time and therapy contribute to its definition and nature. Left uncorrected, the different cellular and inflammatory components of the distressed microcirculation interact and increase in severity, fueling the respiratory distress of the parenchymal cells and ultimately leading to organ failure.
The microcirculation
Microcirculatory function is the main prerequisite for adequate tissue oxygenation and thus organ function. Its purpose is to transport oxygen and nutrients to tissue cells, ensure adequate immunological function and, in disease, to deliver therapeutic drugs to target cells. The microcirculation consists of the smallest blood vessels (<100 μm diameter) where oxygen release to the tissues takes place, and consists of arterioles, capillaries, and venules. The main cell types comprising the microcirculation are the endothelial cells lining the inside of the microvessels, smooth muscle cells (mostly in arterioles), red blood cells, leukocytes, and plasma components in blood. The structure and function of the microcirculation is highly heterogeneous in different organ systems. In general, driving pressure, arteriolar tone, hemorheology, and capillary patency are the main determinants of capillary blood flow.
Regulation of the microcirculation
The regulatory mechanisms controlling microcirculatory perfusion are classed as myogenic (sensing strain and stress), metabolic (regulation based on O2, CO2, lactate, and H+), and neurohumoral. This control system uses autocrine and paracrine interactions to regulate microcirculatory blood flow to meet the oxygen requirements of tissue cells. The endothelial cells lining the inside of the microvessels play a central role in this control system by sensing flow, metabolic, and other regulating substances to regulate arteriolar smooth-muscle-cell tone and capillary recruitment [4]. Endothelial cell-to-cell signaling transmits upstream information about hemodynamic conditions downstream [5]. The endothelium is also important in controlling coagulation and immune function, both of which directly affect and define microcirculatory function.
Regulatory dysfunction
These autoregulatory mechanisms, and thus microcirculatory function, are severely disrupted during sepsis, and their dysfunction is a defining factor in the pathophysiology of sepsis [1]. Microcirculatory dysfunction is characterized by heterogeneous abnormalities in blood flow with some capillaries being underperfused, while others have normal to abnormally high blood flow [6–10]. Functionally vulnerable microcirculatory units become hypoxic, which explains the oxygen extraction deficit associated with sepsis [8, 9, 11–13]. In this condition, the microcirculatory partial pressure of O2 (μpO2) drops below the venous pO2. This disparity has been termed the "pO2 gap", a measurement of the severity of functional shunting, the occurrence of which is more severe in sepsis than in hemorrhage [12–14]. It is the main reason why monitoring systemic hemodynamic-derived and oxygen-derived variables is not able to sense such microcirculatory distress and mask this on-going process.
In sepsis, the microcirculatory endothelial cells are no longer able to perform their regulatory function because of disturbed signal transduction pathways and loss of electrophysiological communication and smooth muscle control [4, 5]. The nitric oxide (NO) system, a central component in the autoregulatory control of microcirculatory patency, is severely disturbed in sepsis by a heterogeneous expression of inducible nitric oxide synthase (iNOS) in different areas of organ beds, resulting in pathological shunting of flow [15, 16]. Since iNOS is not expressed homogeneously in organ systems, areas lacking iNOS have less NO-induced vasodilation and become underperfused. The smooth muscle cells that line the arterioles and regulate perfusion lose their adrenergic sensitivity and tone in sepsis [17, 18]. Red blood cells become less deformable and aggregate more [19–21]. Red blood cells also play an important role in the regulation of microcirculatory blood flow by their ability to release NO in the presence of hypoxia and cause vasodilation [22, 23]. This regulatory property of red blood cells may also be affected in sepsis. These severe defects, together with the disturbed coagulation during sepsis, further impede microcirculatory perfusion and function [15, 16]. Additionally, leukocytes activated by septic inflammation generate reactive oxygen species that directly disrupt microcirculatory structures, cellular interactions, and coagulatory function [24–26]. These and other inflammatory mediators alter barrier function in the microcirculation, including junctions between cells and possibly the endothelial glycocalyx, leading to tissue edema and further oxygen extraction deficit [27, 28]. Left uncorrected, microcirculatory dysfunction leads to respiratory distress of the parenchymal cells and resultant organ failure.
Mitochondrial distress
Whether the primary cause of oxygen extraction deficit in sepsis is explained by the presence of shunted weak, hypoxic microcirculatory units or by mitochondria unable to process oxygen is a source of debate [12, 29, 30]. In a rat heart model of early sepsis, endotoxemia was observed to induce hypoxic areas in the microcirculation [12, 31]. However, in this model no mitochondrial dysfunction was found, as evidenced by the normal response of the mitochondrial energy state to hypoxia in situ [32]. It is likely that progress from early to severe sepsis is accompanied or even possibly caused by microcirculatory dysfunction, which leads to mitochondrial dysfunction with time. Brealey and colleagues [33] showed that mitochondrial dysfunction indeed plays an important role in sepsis where the level of respiratory dysfunction of mitochondria correlated with patient outcome. Mitochondrial failure associated with sepsis contributes to respiratory distress, especially in hypoxic areas [34], and can fuel tissue distress leading to organ dysfunction (Fig. 1).
Microcirculatory and mitochondrial distress syndrome
Resuscitation of the circulatory failure associated with sepsis based on correcting systemic hemodynamic- and oxygen-derived variables, but where regional and microcirculatory distress persist, has been termed microcirculatory and mitochondrial distress syndrome (MMDS) [35]. This concept has been formulated to identify the vulnerable physiological compartment masked from the systemic circulation and responsible for oxygen transport and cellular respiration that becomes dysfunctional in sepsis, and which can lead to organ failure (Fig. 1). The defining elements of the nature and severity of sepsis include the nature of the initial "hit" leading to sepsis, comorbidities, individual genetic makeup, previous therapy, and time to treatment.
The time the syndrome has persisted and the prior therapy received have a defining and modulating effect on the pathophysiology, and define the subclasses of the syndrome. The pathogenic nature of time was convincingly demonstrated by the study of Rivers and colleagues, where early treatment was shown to be associated with improved outcome [36]. This view of MMDS, where therapy and time are included in its definition, indicates that integrative evaluation of these determining factors of microcirculatory and mitochondrial function is needed for evaluation of the severity and nature of the syndrome in individual patients (Fig. 1).
Rescuing the microcirculation
The presence of microcirculatory distress, despite resuscitation based on hemodynamic and oxygen-derived endpoints, strongly suggests that microcirculatory failure is a key factor in the raised lactate levels, disturbed acid–base balance, and high gastric and/or oral CO2 levels sometimes seen under such conditions. Microcirculatory failure can occur in the presence of normal or supranormal systemic hemodynamic- and oxygen-derived variables, with microcirculatory distress being masked from the systemic circulation by shunting pathways [2, 12]. Thus, monitoring techniques are required to verify that recruitment strategies for the microcirculation are indeed effective.
Monitoring the microcirculation to optimize treatment
Several methods have been used to monitor microcirculatory function during circulatory failure in surgery and intensive care [37]. These include CO2 measurements for sublingual, buccal, and subcutaneous microcirculatory CO2 levels [38–41], as well as absorbance, reflectance and near infrared spectroscopy (NIRS), for measuring microcirculatory hemoglobin saturation [14, 42, 43]. Orthogonal polarization spectral (OPS) imaging after validation [44] was introduced by us into surgery and allowed the first direct observation of the microcirculation of human internal organs [45–48]. The technique allows microscopic visualization of the deeper lying microcirculation and the flow of red blood cells in the variably ordered microvessels of the microcirculation [45]. When applied sublingually, OPS provides a sensitivity and specificity for gauging the severity of the distributive defect in sepsis not achieved by conventional monitoring of systemic hemodynamic- or oxygen-derived variables [2]. Sublingual capnography combined with OPS imaging has been used to investigate the relationship between the microcirculation and metabolic state during resuscitation [38]. In cardiac surgery, simultaneous measurement of sublingual NIRS for deeper regional oxygenation, and reflectance spectrophotometry for measurement of superficial microcirculatory oxygen availability, gave integrative information about the redistribution of microcirculatory oxygenation occurring between these compartments during cardiac surgery. Such combinations, looking at different functional compartments of the microcirculation, can integratively ascertain the distributive alterations of oxygen transport during sepsis, septic shock, and therapy that are not provided by conventional monitoring of systemic hemodynamic- and oxygen-derived variables.
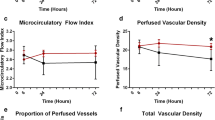
Studies by de Backer and colleagues [7], Spronk and colleagues [10], and Sakr and colleagues [2] on the sublingual microcirculation using OPS imaging in septic patients have directly associated the degree of microcirculatory distress with disease severity and response to therapy. These OPS studies have shown that the distributive defect associated with sepsis is characterized by obstructed stagnant blood flow in the smallest capillaries with near to normal flow in the larger microcirculatory vessels. This underlines the need to clinically monitor the blood flow in these small capillaries. OPS imaging is limited in this respect since OPS images of the capillaries are blurred and cannot always be detected. To this background we developed a new improved imaging modality for observation of the microcirculation called sidestream dark-field (SDF) imaging [49].
SDF imaging consists of a light guide, surrounded by 530 nm light-emitting diodes (LEDs), a wavelength of light that is absorbed by the hemoglobin of red blood cells, allowing their observation as dark cells flowing in the microcirculation (Fig. 2a; see http://www.sdfimaging.net for real-time movies). The LEDs at the tip of the guide are optically isolated from the inner image-conducting core, and pump light deep into the tissue, illuminating the microcirculation from within. This dark-field illumination applied from the side completely avoids tissue surface reflections, giving clear images of microcirculatory structures and red, as well as white, blood cell flow. The improved imaging of the leukocytes is shown in Fig. 2b. Such magnified images are providing new insights into cellular and microcirculatory properties at a level of detail not attained previously. It is expected that SDF imaging will improve the imaging modality for the microcirculation, especially for capillaries.
Sidestream dark-field (SDF) imaging. This imaging technique is an improved method of observing the human microcirculation at the bedside. (a) SDF imaging consists of a light guide surrounded by green light-emitting diodes (LEDs; wavelength 530 nm) whose light penetrates the tissue and illuminates the microcirculation. The light is absorbed by hemoglobin of the red blood cells and scattered by leukocytes. A magnifying lens projects the image onto a video camera. Placed on organ surfaces, SDF imaging provides crisp images of the red blood cells and leukocytes flowing through the microcirculation (for real-time films, see http://www.sdfimaging.net). (b) As an example of the improved image quality provided by SDF imaging, the sublingual microcirculation of a volunteer is shown, with a magnified inset showing several leukocytes.
Therapeutic options
Several therapeutic options are available for resuscitating the microcirculation in septic patients.
Volume resuscitation
Relatively intact autoregulatory mechanisms ensure that resuscitation from hypovolemic shock through volume provision is effective in recruiting vulnerable microcirculatory beds [13, 50, 51]. Volume provision also restores microcirculatory barrier function and promotes microcirculatory oxygen transport [23, 50, 52]. However, hemodilution-induced hemodynamic effects can cause a redistribution of oxygen delivery away from weak microcirculatory units within organs, as well as between organs [14] and sublingual compartments [39, 43]. The significance of such redistribution of oxygen supply and its role in the pathophysiology of sepsis and resuscitation, however, has yet to be established. Blood is a much better oxygen carrier than colloid or crystalloid fluids and transfusion indeed improves oxygen delivery to the microcirculation more so than such fluids [53]. The age of stored red blood cells, however, can affect this property of blood and may need to be taken into account [53]. Hemoglobin-based oxygen carriers are also very effective oxygen carriers to the microcirculation but still need to be developed for routine clinical implementation [54].
iNOS inhibitors and steroids
In sepsis, autoregulatory mechanisms are disturbed [55]. Simple fluid resuscitation, while effective in correcting systemic hemodynamics, can leave weak microcirculatory areas of the microcirculation hypoxemic [11, 12]. This pathological flow distribution [56] is related, among other mechanisms, to a heterogeneous expression of iNOS in different parts of organ beds resulting in pathological shunting of flow [15, 16]. Consequently, weak microcirculatory units need to be actively recruited, particularly under conditions of autoregulatory dysfunction. Of note is that iNOS-deficient mice do not exhibit the circulatory dysfunction associated with endotoxin that occurs in wild-type mice, underlining the importance of iNOS control in sepsis [57]. In recent studies in septic pigs, fluid combined with iNOS inhibition but not fluid alone, was successful in recruiting vulnerable microcirculatory beds in the intestine [50, 58]. Inhibition of iNOS also protects the barrier function of the microcirculation and can be regarded as a microcirculatory recruitment measure [59]. Anti-inflammatory agents such as steroids are highly effective at inhibiting iNOS and can prevent endotoxin-induced hypotension. Late timing of administration, however, does not have the beneficial inhibition of iNOS due to sepsis-evoked NO inhibition of the glucocorticoid receptor [60]. Such studies show the rationale of applying therapy early on. Steroids also improve autoregulatory function as observed in a rat model study of the autoregulatory properties of an isolated septic heart [55]. Most such experimental studies, however, use relatively high amounts of steroids, and clinical guidelines advise against the use of high levels of steroids in the treatment of sepsis [61]. Nevertheless, these studies indicate that reducing iNOS expression can be regarded as an important step in controlling the distributive hemodynamic defects of sepsis.
Vasodilators and vasopressors
Recruitment of microcirculatory perfusion under normovolemia can be achieved by vasodilator therapy because this increases the driving pressure of blood flow at the entrance of the microcirculation [62]. In a porcine model of sepsis, NO donors in combination with fluids improved gut microcirculatory oxygenation and corrected gastric partial pressure of CO2 (pCO2) whereas fluids alone did not [63]. In a clinical study in septic shock patients, where sublingual microcirculation was observed with OPS imaging, pressure-guided resuscitation resulted in attainment of flow in the larger vessels but not in the capillaries, where flow remained either sluggish or stagnant. This scenario directly visualizes the action of shunting pathways and identifies the microcirculation as the location of the distributive defect associated with sepsis. Vasodilator therapy by administration of nitroglycerin with adequate volume support, however, was able to recruit these stationary-flow capillaries and restore sublingual microcirculation [10]. De Backer and colleagues reported similar microcirculatory abnormalities in septic patients [7]. They further showed that the endothelial vasodilatory response was intact in septic patients by demonstrating that topical application of acetylcholine was effective in recruiting the shut-down capillaries. Sublingual OPS imaging studies in septic patients consistently found that, while pressure-guided resuscitation was effective in restoring systemic blood pressure, it did not by definition have such a correcting effect on microcirculatory perfusion [2].
From a microcirculatory perspective, vasopressors should be applied with caution and under conditions of microcirculatory monitoring. A study by Dubois and colleagues [34] reported that systemic blood pressure was restored by vasopressin in a distributive shock patient. Here, direct observation of sublingual microcirculation by OPS imaging showed no detrimental effect on microcirculatory perfusion. However, in another case–study of a septic shock patient, vasopressin, although effective in increasing blood pressure and urine output, caused a complete cessation of sublingual microcirculatory flow, constriction of the regional circulation, and death [64]. Animal experiments have also shown conflicting results: some studies have shown that vasopressin has beneficial effects on the renal microcirculation [65], while others have shown that vasopressin causes intestinal microcirculatory shutdown [66].
Multiple-action therapy
Fluid resuscitation in combination with vasoactive and inotropic support is indeed effective in recruiting the microcirculation, although its effect on the microcirculation cannot be concluded on the measurement of systemic variables alone [2, 38]. Patients whose microcirculation is not responsive to such resuscitation, however, have a poor prognosis [2]. Recruitment of the microcirculation can be accomplished via different pathways and combination therapies can be expected to be beneficial. In this way, an NO donor agent can open the microcirculation and thereby perfuse weak microcirculatory units, while an anti-inflammatory agent or specific iNOS inhibitor can reduce pathological shunting and redirect blood flow to recruit weak microcirculatory units. This may appear paradoxical from a mechanistic stance, but both therapies are effective microcirculatory recruiting maneuvers [50, 65] and could theoretically be combined. It is clear that when applying such combinational therapies, their effectiveness in recruiting the microcirculation needs to be verified for the different organ systems.
Taking into consideration that resuscitated sepsis forms a multifactorial hit resulting in microcirculatory distress, drugs with multiple sites of action might provide an effective treatment strategy for recruiting microcirculatory function during sepsis. Activated protein C (APC) [67] provides just such an integrated approach by acting on different mechanisms involved in microcirculatory distress. It has been shown, for example, that APC inhibits iNOS expression and protects against endotoxin-induced hypotension [68]. Furthermore, through its action on nuclear factor-κB levels, APC also reduces the level of tumor necrosis factor, an effect not seen when iNOS inhibitors are administered alone [69]. In addition, APC reduces leukocyte activation and the release of reactive oxygen species, as well as acting on coagulatory pathways [70]. Several studies have shown by direct intravital observation that these multifactorial actions improve the microcirculation in septic animals [71, 72]. APC initiates a number of effects that, collectively, can be regarded as a rescue strategy for microcirculatory dysfunction in sepsis. However, several questions remain in respect to the mode of action of APC. What effect does the timing and dosage of APC have on the variables known to be beneficial to the microcirculation? How do different organs react to APC? How does the presence of other therapeutic agents affect the efficacy of APC to rescue the microcirculation? Direct observation and monitoring of the microcirculation should provide an insight into these issues and may even provide endpoints for the treatment of sepsis [73].
Conclusion
In this review, we discuss the role of microcirculatory dysfunction in the development and treatment of the circulatory distributive defect associated with sepsis leading to organ failure. Conventional systemic hemodynamic- and oxygen-derived variables fail to detect such microcirculatory dysfunction and its response to the therapy. If left uncorrected, microcirculatory dysfunction can fuel cellular distress of the parenchymal cells and lead to organ dysfunction. From this perspective the microcirculation can indeed be regarded as the motor of sepsis. Recruitment maneuvers and monitoring of microcirculatory function are expected to contribute to the diagnosis and treatment of sepsis.
Abbreviations
- APC:
-
activated protein C
- iNOS:
-
inducible nitric oxide synthase
- LED:
-
light-emitting diode
- MMDS:
-
microcirculatory and mitochondrial distress syndrome
- NO:
-
nitric oxide
- NIRS:
-
near infrared spectroscopy
- OPS:
-
orthogonal polarization spectral
- pCO2:
-
partial pressure of CO2
- pO2:
-
partial pressure of O2
- μpO2:
-
microcirculatory pO2
- SDF:
-
sidestream dark-field.
References
Spronk PE, Zandstra DF, Ince C: Bench-to-bedside review: Sepsis is a disease of the microcirculation. Crit Care 2004, 8: 462-468. 10.1186/cc2894
Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL: Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med 2004, 32: 1825-1831. 10.1097/01.CCM.0000138558.16257.3F
Meakins JL, Marshall JC: The gastrointestinal tract: the 'motor' of MOF. Arch Surg 1986, 121: 197-204.
Vallet B: Endothelial cell dysfunction and abnormal tissue perfusion. Crit Care Med 2002,30(suppl 5):S229-S234. 10.1097/00003246-200205001-00010
Lidington D, Tyml K, Ouellette Y: Lipopolysaccharide-induced reductions in cellular coupling correlate with tyrosine phosphorylation of connexin. J Cell Physiol 2002, 193: 373-379. 10.1002/jcp.10179
Bateman RM, Sharpe MD, Ellis CG: Bench-to-bedside review: Microvascular dysfunction in sepsis – hemodynamics, oxygen transport, and nitric oxide. Crit Care 2003, 7: 359-373. 10.1186/cc2353
De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL: Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med 2002, 166: 98-104. 10.1164/rccm.200109-016OC
Lam C, Tyml K, Martin C, Sibbald W: Microvascular perfusion is impaired in a rat model of normotensive sepsis. J Clin Invest 1994, 94: 2077-2083.
Nakijima Y, Baudry N, Durante J, Vicaut E: Microcirculation in intestinal villi: a comparison between hemorrhagic and endotoxin shock. Am J Respir Crit Care Med 2001, 164: 1526-1530.
Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM, Zandstra DF: Nitroglycerin promotes microvascular recruitment in septic shock after intravascular volume resuscitation. Lancet 2002, 360: 1395-1396. 10.1016/S0140-6736(02)11393-6
Goldman D, Bateman RM, Ellis CG: Effect of sepsis on skeletal muscle oxygen consumption and tissue oxygenation: interpreting capillary oxygen transport data using a mathematical model. Am J Physiol Heart Circ Physiol 2004, 287: H2535-H2544. 10.1152/ajpheart.00889.2003
Ince C, Sinaappel M: Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 1999, 27: 1369-1377. 10.1097/00003246-199907000-00031
Sinaasappel M, van Iterson M, Ince C: Microvascular oxygen pressure measurements in the intestine during hemorrhagic shock and resuscitation. J Physiol (Lond) 1999, 514: 245-253. 10.1111/j.1469-7793.1999.245af.x
Schwarte LA, Fournell A, van Bommel J, Ince C: Redistribution of intestinal microcirculatory oxygenation during acute hemodilution in pigs. J Appl Physiol 2005, 98: 1070-1075. 10.1152/japplphysiol.00861.2004
Morin MJ, Unno N, Hodin RA, Fink MP: Differential expression of inducible nitric oxide synthase messenger RNA along the longitudinal and crypt-villus axes of the intestine in endotoxemic rats. Crit Care Med 1998, 26: 1258-1264. 10.1097/00003246-199807000-00031
Revelly JP, Ayuse T, Brienza N, Fessler HE, Robotham JL: Endotoxic shock alters distribution of blood flow within the intestinal wall. Crit Care Med 1996, 24: 1345-1351. 10.1097/00003246-199608000-00013
Baker CH, Wilmoth FR: Microvascular responses to E. coli endotoxin with altered adrenergic activity. Circ Shock 1984, 12: 165-176.
Price SA, Spain DA, Wilson MA, Harris PD, Garrison RN: Subacute sepsis impairs vascular smooth muscle contractile machinery and alters vasoconstrictor and dilator mechanisms. J Surg Res 1999, 83: 75-80. 10.1006/jsre.1998.5568
Baskurt OK, Temiz A, Meiselman HJ: Red blood cell aggregation in experimental sepsis. J Lab Clin Med 1997, 130: 183-190. 10.1016/S0022-2143(97)90094-9
Piagnerelli M, Boudjeltia KZ, Vanhaeverbeek M, Vincent JL: Red blood cell rheology in sepsis. Intensive Care Med 2003, 29: 1052-1061. 10.1007/s00134-003-1783-2
Siegemund M, Hardeman MR, van Bommel J, Stegenga ME, Lind A, Ince C: Red blood cell deformability in two different doses of LPS in a porcine model of endotoxemia. Intensive Care Med 1999, 25: S21. 10.1007/s001340051011
Cosby K, Partovi KS, Crawford JH, Patel RP, Reiter CD, Martyr S, Yang BK, Waclawiw MA, Zalos G, Xu X, et al.: Nitrite reduction to nitric oxide by deoxyhemoglobin vasodilates the human circulation. Nat Med 2003, 9: 1498-1505. 10.1038/nm954
Singel DJ, Stamler JS: Chemical physiology of blood flow regulation by red blood cells: the role of nitric oxide and S-nitrosohemoglobin. Annu Rev Physiol 2005, 67: 99-145. 10.1146/annurev.physiol.67.060603.090918
Cerwinka WH, Cooper D, Krieglstein CF, Ross CR, McCord JM, Granger DN: Superoxide mediates endotoxin-induced platelet–endothelial cell adhesion in intestinal venules. Am J Physiol Heart Circ Physiol 2003, 284: H535-H541.
Martins PS, Kallas EG, Neto MC, Dalboni MA, Blecher S, Salomao R: Upregulation of reactive oxygen species generation and phagocytosis, and increased apoptosis in human neutrophils during severe sepsis and septic shock. Shock 2003, 20: 208-212. 10.1097/01.shk.0000079425.52617.db
Victor VM, Rocha M, De la Fuente M: Immune cells: free radicals and antioxidants in sepsis. Int Immunopharmacol 2004, 4: 327-347. 10.1016/j.intimp.2004.01.020
Fink MP: Intestinal epithelial hyperpermeability: update on the pathogenesis of gut mucosal barrier dysfunction in critical illness. Curr Opin Crit Care 2003, 9: 143-151. 10.1097/00075198-200304000-00011
van den Berg BM, Vink H, Spaan JA: The endothelial glycocalyx protects against myocardial edema. Circ Res 2003, 92: 592-594. 10.1161/01.RES.0000065917.53950.75
Fink MP: Cytopathic hypoxia in sepsis. Acta Anaesthesiol Scand Suppl 1997, 110: 87-95.
Ince C: Microcirculatory weak units: an alternative explanation. Crit Care Med 2000, 28: 3127-3129.
Avontuur JAM, Bruining HA, Ince C: Inhibition of nitric oxide synthesis causes myocardial ischemia in endotoxemic rats. Circ Res 1995, 76: 418-425.
Eerbeek O, Milstein DMJ, Ince C: Microcirculatory dysfunction in Langendorff endotoxemic rat hearts. Shock 2004, 21: 81.
Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, Singer M: Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 2002, 360: 219-223. 10.1016/S0140-6736(02)09459-X
Dubois MJ, de Backer D, Creteur J, Anane S, Vincent JL: Effect of vasopressin on sublingual microcirculation in a patient with distributive shock. Intensive Care Med 2003, 29: 1020-1023.
Spronk PE, Kanoore-Edul VS, Ince C: Microcirculatory and mitochondrial distress syndrome (MMDS): a new look at sepsis. In Functional Hemodynamic Monitoring. Edited by: Pinsky MR, Payen D. Berlin: Springer-Verlag; Update in Intensive Care Emergency Medicine 2004, 42:47-69
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, EarlyGoal-Directed Therapy Collaborative Group: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001, 345: 1368-1377. 10.1056/NEJMoa010307
Siegemund M, van Bommel J, Ince C: Assessment of regional tissue oxygenation. Intensive Care Med 1999, 25: 1044-1060. 10.1007/s001340051011
Creteur J, De Backer D, Sakr Y, Koch M, Vincent JL: Determinant of sublingual pCO 2 in patients with septic shock. Crit Care Med Suppl 2004, 31: 419.
Guzman JA, Dikin MS, Kruse JA: Lingual, splanchnic, and systemic hemodynamic and carbon dioxide tension changes during endotoxic shock and resuscitation. J Appl Physiol 2005, 98: 108-113. 10.1152/japplphysiol.00243.2004
Venkatesh B, Morgan TJ, Hall J, Willgoss EZ: Subcutaneous gas tensions closely track ileal mucosal gas tensions in a model of endotoxemia without anaerobism. Intensive Care Med 2005, 31: 447-454. 10.1007/s00134-005-2558-8
Weil MH, Nakagawa Y, Tang W, Sato Y, Ercoli F, Finegan R, Grayman G, Bisera J: Sublingual capnometry: a new noninvasive measurement for diagnosis and quantitation of severity of circulatory shock. Crit Care Med 1999, 27: 1225-1229. 10.1097/00003246-199907000-00001
Buise MP, Ince C, Tilanus HW, Gommers D, van Bommel J: The effect of nitroglycerin on microvascular perfusion and oxygenation during gastric tube reconstruction. Anesth Analg 2005, 100: 1107-1111. 10.1213/01.ANE.0000147665.60613.CA
Atasever B, van der Veen A, Goedhart P, de Mo B, Ince C: Sublingual NIRS and reflectance spectrophotometry: new methods to monitor sublingual oxygen availability. Crit Care 2005,8(suppl 1):P73. 10.1186/cc3136
Mathura KR, Vollebrecht KC, Boer K, de Graaf JC, Ubbink DT, Ince C: Comparison of OPS imaging to intravital capillarosopy of nail fold microcirculation. J Appl Physiol 2001, 91: 74-78.
Groner W, Winkelman JW, Harris AG, Ince C, Bouma GJ, Messmer K, Nadeau R: Orthogonal polarization spectral imaging: a new method for study of the microcirculation. Nat Med 1999, 5: 1209-1212. 10.1038/13529
Mathura KR, Alic L, Ince C: Initial clinical experience with OPS imaging. In Yearbook of Intensive Care and Emergency Medicine. Edited by: Vincent JL. Berlin: Springer-Verlag; 2001:233-244.
Mathura KR, Bouma GJ, Ince C: Abnormal microcirculation in brain tumours during surgery. Lancet 2001, 358: 1698-1699. 10.1016/S0140-6736(01)06722-8
Pennings F, Bouma GJ, Ince C: Direct observation of the human cerebral microcirculation during aneurysm surgery reveals increased arteriolar contractility. Stroke 2004, 35: 1284-1288. 10.1161/01.STR.0000126039.91400.cb
Ince C: Sidestream dark field (SDF) imaging: an improved technique to observe sublingual microcirculation. Crit Care 2005,8(suppl 1):P72. 10.1186/cc3135
Siegmund M, van Bommel J, Schwarte LA, Emons M, Rademacher P, Ince C: Selective blockade of iNOS by 1400W restores the gut oxygenation in a pig model of low-dose endotoxaemia. Intensive Care Med 2005, 31: 985-992. 10.1007/s00134-005-2664-7
Van Iterson, M Siegemund, K Burhop, Ince C: Heart and gut microvascular oxygenation in pigs after resuscitation from hemorrhage by different doses of a hemoglobin based oxygen carrier. J Trauma 2003, 55: 1111-1124.
Anning PB, Finney SJ, Singh S, Winlove CP, Evans TW: Fluids reverse the early lipopolysaccharide-induced albumin leakage in rodent mesenteric venules. Intensive Care Med 2004, 30: 1944-1949. 10.1007/s00134-004-2385-3
Raat NJ, Verhoeven AJ, Mik EG, Gouwerok CW, Verhaar R, Goedhart PT, de Korte D, Ince C: The effect of storage time of human red cells on intestinal microcirculatory oxygenation in a rat isovolemic exchange model. Crit Care Med 2005, 33: 39-45. 10.1097/01.CCM.0000150655.75519.02
Van Iterson M, Ince C: Resuscitation of the microcirculation with haemoglobin based oxygen carriers following hemorrhage. In Yearbook of Intensive Care and Emergency Medicine. Edited by: Vincent JL. Berlin: Springer-Verlag; 2004:762-779.
Avontuur JA, Bruining HA, Ince C: Nitric oxide causes dysfunction of coronary autoregulation in endotoxemic rats. Cardiovasc Res 1997, 35: 368-376. 10.1016/S0008-6363(97)00132-6
Groeneveld AB, van Lambalgen AA, van den Bos GC, Bronsveld W, Nauta JJ, Thijs LG: Maldistribution of heterogeneous coronary blood flow during canine endotoxin shock. Cardiovasc Res 1991, 25: 80-88.
Hollenberg SM, Broussard M, Osman J, Parillo JE: Increased microvascular reactivity and improved mortality in septic mice lacking inducible nitric oxide synthase. Circ Res 2000, 86: 774-779.
Pittner A, Nalos M, Asfar P, Yang Y, Ince C, Georgieff M, Bruckner UB, Radermacher P, Froba G: Mechanisms of inducible nitric oxide synthase (iNOS) inhibition-related improvement of gut mucosal acidosis during hyperdynamic porcine endotoxemia. Intensive Care Med 2003, 29: 312-316.
Wang le F, Patel M, Razavi HM, Weicker S, Joseph MG, McCormack DG, Mehta S: Role of inducible nitric oxide synthase in pulmonary microvascular protein leak in murine sepsis. Am J Respir Crit Care Med 2002, 165: 1634-1639. 10.1164/rccm.2110017
Duma D, Silva-Santos JE, Assreuy J: Inhibition of glucocorticoid receptor binding by nitric oxide in endotoxemic rats. Crit Care Med 2004, 32: 2304-2310.
Keh D, Sprung CL: Use of corticosteroid therapy in patients with sepsis and septic shock: an evidence-based review. Crit Care Med 2004, 32: S527-S533. 10.1097/01.CCM.0000142983.15421.11
Buwalda M, Ince C: Opening the microcirculation: can vasodilators be useful in sepsis? Intensive Care Med 2002, 28: 1208-1217. 10.1007/s00134-002-1407-2
Siegemund M, van Bommel J, Vollebrecht K, Dries J, Ince C: Influence of NO donor SIN-1 on the gut oxygenation in a normodynamic, porcine model of low-dose endotoxaemia. Intensive Care Med 2000, 26: S362.
Boerma EC, van der Voort PHJ, Ince C: Sublingual microcirculatory flow is impaired by the vasopressin-analogue terlipressin in a patient with catecholamine-resistant septic shock. Acta Anaesth Scand 2005. doi: 1011/j/1399-6576.2005.00752.x
Albert M, Losser MR, Hayon D, Faivre V, Payen D: Systemic and renal macro- and microcirculatory responses to arginine vasopressin in endotoxic rabbits. Crit Care Med 2004, 32: 1891-1898. 10.1097/01.CCM.0000139708.10718.E3
Westphal M, Freise H, Kehe BE, Bone HG, van Aken H, Seilenkamp AW: Argenine vasopressin compromises gut mucosal microcirculation in septic rats. Crit Care Med 2004, 32: 194-200. 10.1097/01.CCM.0000104201.62736.12
Bernard GR, Vincent JL, Laterre P, Larosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr, Recombinant human protein C, Worldwide Evaluation in Severe Sepsis (PROWESS) study group: Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001, 344: 699-709. 10.1056/NEJM200103083441001
Isobe H, Okajima K, Uchiba M, Mizutani A, Harada N, Nagasaki A, Okabe K: Activated protein C prevents endotoxin-induced hypotension in rats by inhibiting excessive production of nitric oxide. Circulation 2001, 104: 1171-1175.
Brueckmann M, Hoffmann U, Dvortsak E, Lang S, Kaden JJ, Borggrefe M, Haase KK: Drotrecogin alfa (activated) inhibits NF-kappa B activation and MIP-1-alpha release from isolated mononuclear cells of patients with severe sepsis. Inflamm Res 2004, 53: 528-533. 10.1007/s00011-004-1291-z
Yamaji K, Wang Y, Liu Y, Abeyama K, Hashiguchi T, Uchimura T, Krishna Biswas K, Iwamoto H, Maruyama I: Activated protein C, a natural anticoagulant protein, has antioxidant properties and inhibits lipid peroxidation and advanced glycation end products formation. Thromb Res 2005, 115: 319-325. 10.1016/j.thromres.2004.09.011
Hoffmann JN, Vollmar B, Laschke MW, Inthorn D, Fertmann J, Schildberg FW, Menger MD: Microhemodynamic and cellular mechanisms of activated protein action during endotoxemia. Crit Care Med 2004, 32: 1011-1017. 10.1097/01.CCM.0000120058.88975.42
Iba T, Kidokoro A, Fukunaga M, Nagakari K, Shirahama A, Ida Y: Activated protein C improves the visceral microcirculation by attenuating the leukocyte–endothelial interaction in a rat lipopolysaccharide model. Crit Care Med 2005, 33: 368-372. 10.1097/01.CCM.0000153415.04995.88
Ince C: The microcirculation in distress: a new resuscitation end-point? Crit Care Med 2004, 32: 1963-1964. 10.1097/01.CCM.0000139617.88704.B9
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
CI is the chief scientific officer of MicroVision Medical, a company dedicated to the development of optical spectroscopic devices for clinical use. CI has received an honorarium for preparing this manuscript from Eli Lilly and Company.
Rights and permissions
About this article
Cite this article
Ince, C. The microcirculation is the motor of sepsis. Crit Care 9 (Suppl 4), S13 (2005). https://doi.org/10.1186/cc3753
Published:
DOI: https://doi.org/10.1186/cc3753