Abstract
Purpose
We aimed to study the long-term outcomes of cryoballoon (CB) pulmonary vein isolation (PVI) in treating Chinese patients with atrial fibrillation (AF).
Methods
A total of 122 patients (48 women, mean age 57.4 ± 11.3) underwent CB PVI (first generation CB 44.3%, second generation CB 55.7%) for AF (paroxysmal 65.6%, persistent 10.7% and long-standing persistent 23.8%).
Results
PVI was achieved in 113 (92.6%) patients with CB alone, and it was achieved in all patients with additional touch-up by 8-mm-tip cryocatheter. The mean procedural and fluoroscopic duration were 171.9 ± 41 and 46.6 ± 14.6 min respectively. The recurrence-free survival for paroxysmal and non-paroxysmal AF was 77% and 59% respectively at 1 year and progressively declined over time to reach a plateau of 52% and 30% for paroxysmal and non-paroxysmal AF respectively at 5 years. In patients undergoing PVI with second-generation CB, the recurrence-free survival was 75% for paroxysmal AF and 45% for non-paroxysmal AF at 5 years. With multivariate Cox regression analysis, the types of CB (use of second-generation CB: HR 0.49; 95% CI 0.28–0.85; p = 0.011) and size of left atrium (LA) (larger LA size: HR 1.52; 95% CI 1–2.14; p = 0.017) independently predicted recurrence. Transient phrenic nerve injury (PNI) occurred in four (3.3%) patients and persistent PNI occurred in four (3.3%) patients. Other complications occurred in 10 (8.2%) patients with no procedure-related death.
Conclusions
Long-term success of CB PVI for AF declined over time and reached a plateau at 5 years. CB types and LA size are independent predictors for long-term recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cryoballoon (CB) pulmonary vein isolation (PVI) for the treatment of atrial fibrillation (AF) has been increasingly adopted worldwide [1, 2]. On the other hand, it has been shown to be non-inferior to radiofrequency catheter ablation in treating symptomatic drug-refractory paroxysmal AF in terms of both efficacy and safety [3]. Furthermore, a reduction in healthcare utilization and costs have been recently reported [4, 5]. However, there is a scarcity of data in the very long-term outcomes and predictors of recurrence for CB PVI in the treatment of Asians, including Chinese patients with paroxysmal or persistent AF. In addition, there is a paucity of data on the use of compound motor action potential (CMAP) and luminal esophageal temperature (LET) monitoring for prevention of phrenic nerve injury (PNI) and esophageal thermal lesions (ETL) respectively during CB PVI procedures [6, 7]. Therefore, we studied prospectively the very long-term outcomes and predictors of arrhythmic recurrence in a cohort of Chinese patients who have undergone CB PVI for AF. Our experience in using CMAP and LET monitoring in these procedures is also reported.
2 Methods
2.1 Patient population
This was a single-center prospective study on consecutive patients who were aged 18 to 80 and underwent CB PVI procedures for paroxysmal or persistent AF in the period between May 2008 and December 2017 in Princess Margaret Hospital in Hong Kong. Exclusion criteria included prior history of left atrial (LA) catheter ablation, congenital heart disease, LA thrombus, and pregnancy. The study protocol was approved by the Ethics Committee of the investigation centre. All patients gave written informed consent before recruitment into the study.
2.2 Management before ablation
Cardiac computed tomography was performed to reveal LA and PV anatomy. All patients were put on either warfarin with international normalized ratio maintained between 2.0 and 3.0 or fixed doses of non-vitamin K antagonist oral anticoagulants (NOACs) for at least 4 weeks before the procedure. Ablation was performed with un-interrupted warfarin while NOAC was stopped 2–5 days according to renal function beforehand [8]. Transesophageal echocardiography was performed the day before procedure to rule out LA thrombus. All antiarrhythmic drugs including amiodarone were discontinued at least 5 days before ablation.
2.3 CB PVI procedure
The CB PVI procedure has been described previously [3]. In brief, the ablation procedure was performed under local anesthesia and conscious sedation with midazolam and fentanyl. Intravenous heparin was given to maintain an activated clotting time of over 300 s throughout the procedure. A steerable decapolar electrode catheter was placed in the coronary sinus, and a steerable quadripolar electrode catheter was placed in the right ventricle for pacing support when vasovagal reaction occurred after CB ablation of the left-sided PVs. This catheter was moved to the right subclavian vein or superior vena cava for phrenic nerve (PN) stimulation during CB ablation of the right-sided PVs. A single transseptal puncture was performed with the Brockenbrough needle and an 8 French sheath (SL1 guiding catheter, St Jude Medical, St Paul, MN, USA or Mullin transseptal guiding introducer, Medtronic, Minneapolis, MN, USA) which was then exchanged for a 15 French steerable transseptal sheath (FlexCath or FlexCath Advance, Medtronic Cryocath, Minneapolis, MN, USA). The 10.5 French 28 or 23 mm cryoballoon catheter (Arctic Front or Arctic Front Advance, Medtronic Cryocath, Minneapolis, MN, USA) was then introduced via the steerable transseptal sheath to the LA for PVI. Mapping of PV potentials was performed with a stand-alone circular catheter (Optima Plus, St Jude Medical, St. Paul, MN, USA) or an inner lumen catheter (Achieve, Medtronic Cryocath, Minneapolis, MN, USA) placed inside the cryoballoon catheter since its availability in May 2011. In general, two consecutive cryoapplications of 4 min each were delivered to each PV ostium or antrum with first-generation CB (Arctic Front) and for second-generation CB (Arctic Front Advance), two consecutive cryoapplications of 3 min each were used for each PV. Additional cryoapplications were delivered to achieve PVI if necessary. The procedural endpoint was electrical isolation of all PVs with entry ± exit block. Touch-up with an 8-mm-tip cryoablation catheter (Freezor Max 5, Medtronic, Minneapolis, MN, USA) was performed if procedural endpoint could not be achieved with CB alone. To prevent PNI, compound motor action potential (CMAP) [6] of the right hemi-diaphragm was monitored while pacing the PN in the right subclavian vein or superior vena cava during CB ablation of right-sided PVs since September 2013. Before that, PN function was monitored only by palpation of diaphragmatic contraction. Cryoablation was immediately stopped when a 30% drop in the amplitude of CMAP or a decrease in diaphragmatic contraction with palpation was observed. To prevent ETL, LET was monitored by a self-expanding catheter containing 12 temperature sensors (S-Cath, Circa Scientific, Englewood, CO, USA) (Fig. 1) since March 2015 [7, 9]. Cryoablation was stopped once any temperature sensor detected a fall in LET to 20 °C.
Panels a, b show the RAO and LAO views respectively during CB ablation of the LIPV with LET monitoring by a self-expandable catheter with 12 temperature sensors spanning the whole length of the esophagus. The six pairs of temperature sensors are indicated by blue arrows. RAO: right anterior oblique, LAO: left anterior oblique, CB: cryoballoon, LIPV: left inferior pulmonary vein, LET: luminal esophageal temperature, LAO: left anterior oblique
2.4 Post-ablation management and follow-up
All patients underwent continuous ECG monitoring in the coronary care unit for 24 h after ablation. For patients on NOAC, the first dose was resumed 24–48 h after the procedure. Oral anticoagulation was continued for 3 months, and its subsequent need depended on the CHA2DS2VASc score of the patients. Previously used antiarrhythmic drugs were given for 3 months after the procedure. Patients were scheduled for clinic follow-up 1 month and then quarterly afterwards. History on symptom recurrence of palpitations was specifically taken, and a 12-lead ECG was performed during each follow-up. A 24-h Holter monitoring was performed during each follow-up for the first 12 months after the procedure and then arranged when necessary. A 3-month blanking period was adopted for recurrence of atrial arrhythmias. Re-ablation was avoided during the blanking period. Recurrence was defined as documented occurrence of AF, atrial flutter, or atrial tachycardia lasting over 30 s.
2.5 Statistical analysis
Descriptive statistics are presented for all data. For normally distributed data, they are expressed as mean and standard deviation and comparison was performed by Student’s t test. For non-normally distributed data, they are expressed as median with maximum and minimum values stated, and the Mann-Whitney U test was used to assess statistical significance. For categorical data, absolute and relative frequencies were determined and the 95% confidence intervals were calculated. Fisher exact test or chi-square test was performed to assess statistical significance. Independent predictors of arrhythmic recurrence were modeled by multivariate Cox regression. Kaplan-Meier survival analysis was used to study the long-term recurrence of atrial arrhythmias. Log-rank test was used to compare Kaplan-Meier curves. For regression analysis, a univariate analysis was performed first and variables with p values of < 0.1 were included for multivariate analysis. Statistics were performed with the Statistical Package for Social Science (IBM SPSS version 19, Chicago, IL, USA). A p value of < 0.05 was considered as statistically significant.
3 Results
3.1 Clinical and procedural characteristics
A total of 122 patients (48 women, mean age 57.4 ± 11.3) with mean CHA2DS2VASc score 1.7 ± 1.4 underwent CB PVI for AF (paroxysmal 65.6%, persistent 10.7% and long-standing persistent 23.8%) in the period between May 2008 and December 2017 in Princess Margaret Hospital in Hong Kong. The clinical and procedural characteristics are summarized in Tables 1 and 2, respectively. The second-generation CB was used in 68 (55.7%, 95% CI 51.2–60.2%) patients, and the first-generation CB was used in the remaining patients. The large 28-mm CB was used in 114 (93.4%, 95% CI 91.2–95.6%) patients. The mean number of cryoapplications was 9.3 ± 3. The mean procedural and fluoroscopic duration were 171.9 ± 41 and 46.6 ± 14.6 min respectively. The fluoroscopic duration was significantly shorter when second-generation CB was used (42.9 ± 13.3 vs 51.3 ± 15 min, p = 0.002) or during the last 61 patients of this cohort (42.9 ± 13.6 vs 50.3 ± 14.8 min, p = 0.005). PVI was achieved in 113 (92.6%, 95% CI 90.2–95%) patients with CB alone and additional touch-up ablation by an 8-mm-tip cryocatheter enabled subsequent achievement of PVI in all patients. Transient PNI occurred in four (3.3%, 95% CI 1.7–4.9%) patients and subsided before the procedures ended. Persistent PNI occurred in another four (3.3%, 95% CI 1.7–4.9%) patients and subsided after 1 day, 3 weeks, and 8 and 20 months respectively. No significant difference in PNI was observed between patients treated with first or second generation CB (5.6 vs 7.4%, p = 0.690). Other complications occurred in 10 (8.2%, 95% CI 5.7–10.7%) patients, and there was no procedure-related death.
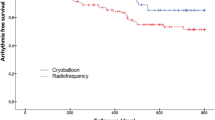
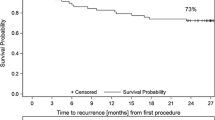
3.2 Long-term outcomes of CB PVI for AF
The mean and median follow-up for this patient cohort was 30.9 ± 28.6 and 20 months (2–117) respectively. The recurrence rates after CB PVI over long-term follow-up are summarized in Fig. 2. The 1-year recurrence-free survival for paroxysmal and non-paroxysmal AF was 77% and 59% respectively. The recurrence-free survival progressively dropped over time and reached a plateau of 52% and 30% for paroxysmal and non-paroxysmal AF respectively at 5 years. The recurrence rate was significantly lower in patients with paroxysmal AF than non-paroxysmal AF (Fig. 3, log-rank test p = 0.006). During the last follow-up, 56 (70%) patients with paroxysmal AF and 34 (81%) patients with non-paroxysmal AF were not on any antiarrhythmic drugs. With multivariate Cox regression analysis (Table 3), the types of CB (use of second-generation CB: HR 0.49; 95% CI 0.28–0.85; p = 0.011) and size of LA (larger LA size (as a continuous variable): HR 1.52; 95% CI 1–2.14; p = 0.017) independently predicted recurrence after CB PVI. Figure 4a, b show the comparison of Kaplan-Meier curves on recurrence rates between first- and second-generation CB (log-rank test p = 0.003), and between LA size ≥ 4 cm and < 4 cm (log-rank test p = 0.044). In patients undergoing PVI with second-generation CB, the recurrence-free survival was 75% for paroxysmal AF and 45% for non-paroxysmal AF at 5-year follow-up. In patients with LA size over 5 cm, all of them suffered from recurrence (Fig. 5).
Kaplan-Meier curves for recurrence-free survival after CB PVI for AF. Panel a shows a comparison between first- and second-generation CB. Panel b shows a comparison between patients with LA size < 4 cm and ≥ 4 cm. CB: cryoballoon, PVI: pulmonary vein isolation, AF: atrial fibrillation, LA: left atrium, CB1: first-generation cryoballoon, CB2: second-generation cryoballoon
3.3 Use of CMAP and LET monitoring during CB PVI procedures
CMAP monitoring was used in 55 (45.1%, 95% CI 40.6–49.6%) patients. No significant difference was shown in the incidence of PNI (7.3 vs 6%, p = 1.0) or persistent PNI (0 vs 6%, p = 0.126) between patients with and without CMAP monitoring. LET monitoring was used in 29 (23.8%, 95% CI 19.9–27.7%) patients. Cryoablation was interrupted in 16 (55.2%, 95% CI 46–64.4%) patients due to a fall in LET to 20 °C. These interruptions occurred during ablation in left superior pulmonary veins (LSPV) in 7 (24.1%, 95% CI 16.2–32%) patients, left inferior pulmonary veins (LIPV) in 12 (41.4%, 95% CI 32.3–50.5%) patients, and right inferior pulmonary veins (RIPV) in 1 (3.4%, 95% CI 0–6.8%) patient. The median lowest CB temperatures reached on termination of cryoapplications were − 44 °C (− 27 to − 52 °C) at LSPVs, − 45 °C (− 38 to − 51 °C) at LIPVs, and − 48 °C at RIPV.
4 Discussion
4.1 Long-term efficacy of CB PVI in Chinese patients with AF
Data on very-long term outcome of radiofrequency circumferential PVI has consistently shown a progressive reduction in efficacy over time. Tilz et al. reported 32.9% recurrence-free survival in 161 patients with drug-refractory paroxysmal AF after a single circumferential PVI procedure and median follow-up of 129 months [10]. In that study, the recurrence-free survival was around 42% on 5-year follow-up. Brooks et al. studied the efficacy of circumferential PVI in 174 patients with persistent AF and during a median follow-up of 89 months found a recurrence-free survival of 25% after a single procedure [11]. Tilz et al. found a recurrence-free survival of 20.3% after a single circumferential PVI procedure in 202 patients with long-standing persistent AF and median follow-up of 56 months [12]. Similarly in our study, we observed a progressive drop in recurrence-free survival to 52% and 30% for paroxysmal and non-paroxysmal AF respectively at 5 years after a single procedure of CB PVI in a cohort of Chinese patients. Interestingly, we also observed a plateau phenomenon from 5 years onwards, which was not apparent in radiofrequency circumferential PVI procedures and has not been previously observed in CB PVI procedures. This may support the notion that, compared with a single-shot balloon-based ablation, it is technically more difficult to achieve a durable PVI by using point-by-point radiofrequency ablation. On the other hand, radiofrequency circumferential PVI may be complicated by more macro-reentrant atrial tachycardia which continues to depreciate the long-term treatment efficacy [3]. Data on the very long-term outcome in patients treated with CB PVI for AF is in contrast scarce. Heeger et al. reported recurrence-free survival of 69% for paroxysmal AF and 39% for persistent AF with a median follow-up of 38 months in a cohort of 100 patients undergoing CB PVI [13]. In another study with 178 patients enrolled, Akkaya et al. reported a higher recurrence-free survival of 61.4% for paroxysmal AF and 52.2% for persistent AF at 5-year follow-up [14]. In both studies, second-generation CB was used. As shown by our study, use of second-generation CB was an independent predictor for lower recurrence rate. With subgroup analysis on second-generation CB in our study, the recurrence-free survival was 75% for paroxysmal AF and 45% for non-paroxysmal AF at 5-year follow-up and is thus consistent with the observations by Akkaya et al.
4.2 Predictors of long-term success after CB PVI
Clinical characteristics including age, sex, coronary artery disease, number of failed antiarrhythmic drugs, and types of AF, together with LA size, have been shown to be independent predictors of recurrence after radiofrequency ablation for AF [15]. On the other hand, persistent AF and its duration, presence of cardiomyopathy and LA area > 21 cm2 have been shown to be independent predictors of recurrence after CB PVI procedures for AF [13, 14, 16, 17]. In addition, conceivably, different anatomical features of PVs were consistently found to be independent predictors of recurrence after CB ablation [18,19,20,21]. In our study, only the use of second-generation CB and LA size were identified to be independent predictors for long-term success after CB PVI procedures. Notably, the types of AF, namely paroxysmal, persistent, or long-standing persistent types, were only predictors on univariate analysis but not in a multivariate regression model. As shown in our study, LA size is therefore the most important clinical parameter for selecting a patient to undergo CB PVI for treatment of AF. When LA size is over 5 cm, all patients in our study had recurrence and therefore it may not be advisable to subject these patients to CB PVI procedures.
4.3 LET and CMAP monitoring to prevent ETL and PNI
Atrioesophageal fistula (AEF) is a rare but fatal complication associated with CB PVI procedures. The incidence was estimated to be < 0.01% and the mortality rate was reported to be over 60% [22]. In addition, all cases of AEF were associated with CB ablation at LIPVs. LET monitoring with interruption of CB ablation at a cut-off temperature has been shown to reduce the incidence of ETL which may be a precursor of AEF [23]. Furnkranz et al. showed that the incidence of ETL decreased from 7.1 to 1.5% when the temperature cut-off was increased from 12 to 15 °C. A few esophageal temperature probes have been tested [24]. To the best of our knowledge, we have reported for the first time the use of a self-expandable esophageal temperature catheter with 12 sensor probes spanning the whole length of the esophagus. We adopted a higher temperature cut-off of 20 °C for interruption of CB ablation aiming to totally avoid the occurrence of ETL. This temperature cutoff was reached in 55.2% of patients, and consistent with previous observations, it occurred most commonly during LIPV ablation (41.4%). Importantly, it also occurred during LSPV (24.1%) and RIPV (3.4%) ablation. Compared with other studies, the increased need for interruption of CB ablation was likely to be related to the adoption of a higher temperature cut-off and a more panoramic monitoring of the LET. Whether this approach leads to a lower incidence of ETL warrants further research.
PNI is the most common clinically significant adverse event complicating CB PVI. Persistent PNI beyond discharge varied from 3.5 to 11.2% [1, 3, 25]. Different techniques, namely exclusive use of a 28-mm CB [26], short cryoapplication of 3 min [27], “double-tap technique,” [28] “proximal seal technique,” [27] and CMAP monitoring have been described to reduce the incidence of PNI. Whether the use of CMAP monitoring prevents PNI remains an unanswered question. We observed no significant difference in the total incidence of PNI between patients with and without CMAP monitoring (7.3 vs 6%, p = 1.0). However, it seems that the incidence of persistent PNI may be reduced by CMAP monitoring (0 vs 6%, p = 0.126). All PNIs in the CMAP monitoring group were transient and resolved before the end of the procedure. In contrast, all PNIs in patients without CMAP monitoring persisted beyond discharge. Interestingly, Meissner et al. showed that PNI occurred significantly fewer when CMAP monitoring was used (3.8 vs 9.8%, p < 0.001) [29]. Consistent with our observations, none of the patients with CMAP monitoring had persistent PNI. Randomized-controlled studies were warranted to confirm the usefulness of CMAP monitoring in reducing the risk of persistent PNI complicating CB PVI.
4.4 Limitations
The number of patients in this study is relatively small. Over a very long-term follow-up, both the procedural techniques and operator experience may have significantly changed and confounded the outcomes. A significant proportion of patients (44%) had PVI with the first-generation CB, which is no longer applicable in current clinical practice. On the other hand, the number of patients reaching very long-term follow-up was small and future studies with larger number of patients are required to confirm our observations on very long-term outcomes after CB PVI. The follow-up methodology may not be rigorous enough, and the recurrence rate can be underestimated. Similarly the plateau phenomenon observed on recurrence pattern may also be related to the follow-up methodology. Although LET monitoring was used in our study, upper endoscopy was not performed to document ETL. Lastly, this study was performed on Chinese patients, applicability of our findings to other ethnic groups remains unknown.
5 Conclusion
In a cohort of Chinese patients undergoing CB PVI, the 1-year recurrence-free survival for paroxysmal and non-paroxysmal AF was 77% and 59% respectively. The recurrence-free survival progressively declined over time and reached a plateau of 52% and 30% for paroxysmal and non-paroxysmal AF respectively at 5 years. In patients undergoing PVI with second-generation CB, the recurrence-free survival was 75% for paroxysmal AF and 45% for non-paroxysmal AF at 5-year follow-up. The types of CB and LA size were shown to be independent predictors for recurrence.
References
Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG, et al. STOP AF Cryoablation investigators. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J Am Coll Cardiol. 2013;61:1713–23.
Vogt J, Heintze J, Gutleben KJ, Muntean B, Horstkotte D, Nolker G. Long-term outcomes after cryoballoon pulmonary vein isolation: results from a prospective study in 605 patients. J Am Coll Cardiol. 2013;61(16):1707–12.
Kuck KH, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KR, et al. FIRE AND ICE investigators. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235–45.
Kuck KH, Furnkranz A, Chun KRJ, Metzner A, Ouyang F, Schluter M, et al. Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur Heart J. 2016;37:2858–65.
Chun KRJ, Brugada J, Elvan A, Geller L, Busch M, Barrera A, et al. The impact of cryoballoon versus radiofrequency ablation for paroxysmal atrial fibrillation on healthcare utilization and costs: an economic analysis from the FIRE AND ICE trial. J Am Heart Assoc. 2017;6:e006043. https://doi.org/10.1161/JAHA.117.00043.
Mondesert B, Andrade JG, Khairy P, Guerra PG, Dyrda K, Macle L, et al. Clinical experience with a novel electromyographic approach to preventing phrenic nerve injury during cryoballoon ablation in atrial fibrillation. Circ Arrhythm Electrophysiol. 2014;7:605–11.
Miyazaki S, Nakamura H, Taniguchi H, Takagi T, Iwasawa J, Watanabe T, et al. Esophagus-related complications during second-generation cryoballoon ablation-insight from simultaneous esophageal temperature monitoring from 2 esophageal probes. J Cardiovasc Electrophysiol. 2016;27:1038–44.
Sticherling C, Marin F, Birnie D, Boriani G, Calkins H, Dan GA, et al. Antithrombotic management in patients undergoing electrophysiological procedures. A European Heart Rhythm Association (EHRA) position document endorsed by the ESC working group thrombosis, Heart Rhythm Society (HRS), and Asia Pacific Heart Rhythm Society (APHRS). Europace. 2015;17:1197–214.
Chan NY. Catheter ablation of peri-nodal and pulmonary veno-atrial substrates: should it be cool? Europace. 2015;17(Suppl 2):ii19–30.
Tilz RR, Wick A, Saguner AM, Metzner A, Rillg A, Wohlmuth P, et al. Ten-year clinical outcome after circumferential pulmonary vein isolation utilizing the Hamburg approach in patients with symptomatic drug-refractory paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol. 2018;11:e005250. https://doi.org/10.1161/CIRCEP.117.005250.
Brooks S, Metzner A, Wohlmuth P, Lin T, Wissner E, Tilz R, et al. Insights into ablation of persistent atrial fibrillation: lessons from 6-year clinical outcomes. J Cardiovasc Electrophysiol. 2018;29:257–63.
Tilz RR, Rillig A, Thum AM, Arya A, Wohlmuth P, Metzner A, et al. Catheter ablation of long-standing persistent atrial fibrillation. J Am Coll Cardiol. 2012;60:1921–9.
Heeger CH, Wissner E, Knoll M, Knoop B, Reissmann B, Mathew S, et al. Three-year clinical outcome after 2nd-generation cryoballoon-based pulmonary vein isolation for the treatment of paroxysmal and persistent atrial fibrillation- a 2-center experience. Circ J. 2017;81:974–80.
Akkaya E, Berkowitsch A, Zaltsberg S, Greiss H, Hamm CW, Sperzel J, et al. Five-year outcome and predictors of success after second-generation cryoballoon ablation for treatment of symptomatic atrial fibrillation. Int J Cardiol. 2018;266:106–11.
Winkle RA, Jarman JWE, Mead H, Engel G, Kong MH, Fleming W, et al. Predicting atrial fibrillation ablation outcome: the CAAP-AF score. Heart Rhythm. 2016;13:2119–25.
Irfan G, de Asmundis C, Mugnai G, Poelaert J, Verborgh C, Umbrain V, et al. One-year follow-up after second-generation cryoballoon ablation for atrial fibrillation in a large cohort of patients: a single-centre experience. Europace. 2016;18:987–93.
Yalin K, Abdin A, Lyan E, Sawan N, Liosis S, Elsner C, et al. Safety and efficacy of persistent atrial fibrillation ablation using the second-generation cryoballoon. Clin Res Cardiol. 2018;107(7):570–7.
Kubala M, Hermida JS, Nadji G, Quenum S, Traulle S, Jarry G. Normal pulmonary veins anatomy is associated with better AF-free survival after cryoablation as compared to atypical anatomy with common left pulmonary vein. Pacing Clin Electrophysiol. 2011;34:837–43.
Schmidt M, Dorwarth U, Straube F, Daccarett M, Rieber J, Wankerl M, et al. Cryoballoon in AF ablation: impact of PV ovality on AF recurrence. Int J Cardiol. 2013;167:114–20.
Kencht S, Kuhne M, Altmann D, Ammann P, Schaer B, Osswald S, et al. Anatomical predictors for acute and mid-term success of cryoballoon ablation of atrial fibrillation using the 28mm balloon. J Cardiovasc Electrophysiol. 2013;24:132–8.
Guler E, Guler GB, Demir GG, Kizilirmak F, Gunes HM, Barutcu I, et al. Effect of pulmonary vein anatomy and pulmonary vein diameters on outcome of cryoballoon catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol. 2015;38:989–96.
John RM, Kapur S, Ellenbogen KA, Koneru JN. Atrioesophageal fistula formation with cryoballoon ablation is most commonly related to the left inferior pulmonary vein. Heart Rhythm. 2017;14:184–9.
Furnkranz A, Bordignon S, Bohmig M, Konstantinou A, Dugo D, Perrotta L, et al. Reduced incidence of esophageal lesions by luminal esophageal temperature-guided second-generation cryoballoon ablation. Heart Rhythm. 2015;12:268–74.
Leite LR, Santos SN, Maia H, Henz BD, Giuseppin F, Oliverira A, et al. Luminal esophageal temperature monitoring with a deflectable esophageal temperature probe and intracardiac echocardiography may reduce esophageal injury during atrial fibrillation ablation procedures. Circ Arrhythm Electrophysiol. 2011;4:149–56.
Neumann T, Vogt J, Schumacher B, Dorszewski KM, Hans N, et al. Circumferential pulmonary vein isolation with the cryoballoon technique. Results from a prospective 3-center study. J Am Coll Cardiol. 2008;52:273–8.
Metzner A, Rausch P, Lemes C, Reissmann B, Bardyszewski A, Tilz R, et al. The incidence of phrenic nerve injury during pulmonary vein isolation using the second-generation 28mm cryoballoon. J Cadiovasc Electrophysiol. 2014;25:466–70.
Mugnai G, de Asmundis C, Ciconte G, Irfan G, Saitoh Y, Velagic V, et al. Incidence and characteristics of complications in the setting of second-generation cryoballoon ablation: a large single-center study of 500 consecutive patients. Heart Rhythm. 2015;12(7):1476–82.
Ghosh J, Sepahpour A, Chan KH, Singarayar S, McGuire MA. Immediate balloon deflation for prevention of persistent phrenic nerve palsy during pulmonary vein isolation by balloon cryoablation. Heart Rhythm. 2013;10(5):646–52.
Meissner A, Maagh P, Christoph A, Oernek A, Plehn G. ECG-guided surveillance technique in cryoballoon ablation for paroxysmal and persistent atrial fibrillation: a strategy to prevent from phrenic nerve palsy. Int J Med Sci. 2016;13(6):403–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Ethics Committee of the investigation centre. All patients gave written informed consent before recruitment into the study.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chan, NY., Choy, CC., Yuen, HC. et al. Long-term outcomes of cryoballoon pulmonary vein isolation for paroxysmal and persistent atrial fibrillation in Chinese patients. J Interv Card Electrophysiol 57, 425–434 (2020). https://doi.org/10.1007/s10840-019-00542-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00542-x