Abstract
Gaps in research knowledge exist regarding patient-provider interactions with individuals with autism in healthcare settings. To address this, a scoping review was conducted focusing on the experiences of healthcare professionals working with individuals with autism. A systematic search and screen of the literature resulted in 27 relevant studies. Six key themes were found across these 27 studies including (1) complexity beyond usual role, (2) limited knowledge and resources, (3) training/prior experience, (4) communication and collaboration, (5) need for information and training, and (6) need for care coordination and systemic changes. The results of this review have implications for future research and practice and should be considered when reflecting on opportunities to enhance research and service provision with individuals with autism.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
With rates of autism diagnoses on the rise internationally (Christensen et al. 2016; Elsabbagh et al. 2012), it is imperative that service providers across health sectors are prepared and equipped to meet the needs of this population. Autism has been significantly associated with a number of co-occurring medical and mental health conditions that contribute to high rates of utilization and repeated contact with the healthcare system (Cummings et al. 2016; Kogan et al. 2008; Lynch et al. 2014; Peacock et al. 2012; Tint et al. 2017; Weiss et al. 2018), increasing the need for healthcare systems to be prepared to provide effective and multi-faceted supports for this population.
The patient-provider relationship has been highlighted as integral to improving patient confidence and agency in self-management of health even among high-risk populations (Cerier et al. 2018; Mattingly et al. 2017). While some positive experiences have been shared (Muskat et al. 2015; Nicolaidis et al. 2015; Wilson and Peterson 2018), healthcare service users with autism and their family members frequently report challenges associated with the patient-provider relationship in the healthcare system; citing communication barriers, perceived limited knowledge and skill of healthcare providers related to autism, and limited recognition of the parental and family role (e.g., Chiri and Warfiled 2012; Dern and Sappok 2016; Nicolaidis et al. 2013, 2015; Raymaker et al. 2017; Strunk et al. 2014; Vogan et al. 2017; Wilson and Peterson 2018).
Individuals with autism and their caregivers report communication barriers stemming from both patients and providers. Personal difficulties that have been noted include the ability to confidently and clearly express concerns and needs as a result of autism (Dern and Sappok 2016; Lum et al. 2014; Nicolaidis et al. 2015). Difficulties associated with providers include a perception of being unheard, stigmatized, and/or excluded from participation in assessment and treatment conversations (Dern and Sappok 2016; Nicolaidis et al. 2013; Solomon et al. 2016; Strunk et al. 2014; Wilson and Peterson 2018). Similarly, limitations in knowledge and skills training of health professionals have been identified by individuals with autism and their caregivers as resulting in unmet healthcare needs (Baldwin and Costley 2015; Barber 2017; Levy et al. 2016; Nicolaidis et al. 2015; Vogan et al. 2017). Many individuals and families report particular difficulty finding and accessing healthcare providers who are willing and able to provide care for adults with autism (Joseph-Kent 2016; Lewis 2017).
Additionally, parents and family members across studies repeatedly note a limited recognition of their potential role and expertise as collateral information sources and ongoing supports for their family member with autism (Carbone et al. 2010; Hubner et al. 2016; Levy et al. 2016; Wilson and Peterson 2018).
Gaps in the patient-provider relationship experienced by individuals with autism may be exacerbated by a well-documented lack of autism relevant knowledge and skills training among healthcare professionals across disciplines (Atun-Einy and Ben-Sasson 2018; Elmensdorp 2011; Heidgerken et al. 2005; Zerbo et al. 2015).
While service user experiences and healthcare provider knowledge of autism have received research attention, the experiences of healthcare providers in these interactions are far less clearly understood. It is possible that healthcare providers themselves may hold some insight into the factors that support or obstruct the development and maintenance of therapeutic rapport in the patient-provider relationship, and there may be value in incorporating the perspectives of front-line healthcare professionals into the research on healthcare interactions with this population. Some studies have been conducted seeking healthcare provider input (see for example Warfield et al. 2015; Zerbo et al. 2015), but a review exploring thematic patterns across studies has yet to be conducted. A review of research literature to date will highlight recurring themes relevant to barriers and facilitators impacting service provision with this population, and may yield important implications for enhancing practice and research in this area.
This paper reports the results of a scoping review that was conducted by the research team to consolidate published research literature exploring healthcare provider experiences of interactions with clients with autism in the healthcare system (The Joanna Briggs Institute 2015). The goal of this scoping review was to reveal gaps in knowledge about healthcare service provision with this population, as well as to highlight areas requiring further research and knowledge development. Findings of this review may be used to inform future research in this area.
Methods
A scoping review methodology was chosen as it provided a framework to implement a systematic information retrieval strategy to search the literature, summarize themes and gaps across research, and highlight opportunities for future research and practice that can move the field forward (Anderson et al. 2008; Arksey and O’Malley 2005; The Joanna Briggs Institute 2015).
Search Strategy
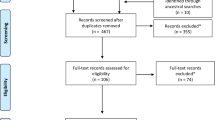
A systematic search of the literature was conducted in November 2017 and updated in April 2018 across four electronic databases: Ovid MEDLINE, CINAHL, PsycINFO, and Social Work Abstracts. Search terms related to healthcare and autism were utilized across all four databases (see Table 1). The search terms were refined with the assistance of a university research librarian to expand the comprehensiveness of resulting materials. During the first search a total of 1640 articles were found, of which 663 were duplicates, leaving 977 remaining articles for review.
A review of titles and abstracts was based on the inclusion criteria of (1) English language, (2) primary research study (3) topic was autism (4) healthcare professionals as participants, (5) primary focus was provider experiences (i.e., excluding studies that only explored amount or level of knowledge related to autism), (6) studies were based in a healthcare context (i.e., primary, secondary, or tertiary care). An iterative approach to study screening and selection was employed to emphasize a more inclusive final list of studies, and team member discussion erred on the side of inclusion whenever possible. Screening of titles and abstracts was conducted in order of the inclusion criteria as listed above and reasons for exclusion at this level included a clear identification within title or abstract that the study did not meet one or more of the inclusion criteria (see Fig. 1). This first screen eliminated 923 articles, with 54 articles remaining to undergo a screen of full-text.
A full-text screen of the 54 remaining articles was conducted separately by two members of the research team based on the same inclusion criteria above, with a 75% agreement rate. All disagreements were brought forward for further discussion by the entire research team of authors, and a consensus was reached to include three of these nine discussed articles in the final study. Based on the inclusion criteria stated above, the final decision was to exclude 29 of the 54 articles put forward for full-text review (see Fig. 1). The remaining 25 relevant articles were included in the synthesis.
During the analysis phase in April 2018 a second identical database search was conducted in order to update the search findings to include any studies that had been published since the original search. This search and screen resulted in the addition of two articles, increasing the number of included articles to N = 27 (13 quantitative, 10 qualitative, and 4 mixed-methods). The full screening process is outlined in Fig. 1.
Data Extraction and Analysis
The final 27 studies were extracted and analyzed for key thematic content and patterns. As per scoping review methodology (The Joanna Briggs Institute 2015), the results of all 27 articles were grouped by methodological approach (i.e., quantitative, qualitative, or both), and an iterative approach was taken by the team to extract demographic (i.e., country of origin, sample size), quantitative, and thematic information and to systematically review and update the results. Team members met regularly to discuss emerging themes and reduce researcher bias in interpreting the results. In accordance with the scoping review methodology, an analysis of methodological rigour of the included studies was not conducted (Anderson et al. 2008; Arksey and O’Malley 2005; The Joanna Briggs Institute 2015). This review instead provides a summary of themes found across the research literature, as well as areas of difference or gaps in knowledge that may assist with the formulation and design of future research studies in this area.
Results
The majority of the 27 included studies were conducted in the United States (n = 17), followed by Canada (n = 5), Australia (n = 2), United Kingdom (n = 2), India (n = 1), Nigeria (n = 1), and Palestine (n = 1). A total of 6537 health professionals contributed as participants across 13 quantitative, 10 qualitative, and 4 mixed-methods studies. Study participants represented a variety of healthcare provider disciplines across the 27 studies, including nurses (n = 5), allied health (i.e., psychology, social work, speech-language pathology, and/or occupational therapy) (n = 7), pediatricians or pediatric residents (n = 5), primary care physicians (n = 6), ‘physicians’ defined broadly (n = 5), psychiatrists (n = 2), dentists (n = 2), pharmacists (n = 1), and paramedics (n = 1). The majority of studies included solely primary or community care practitioners (n = 15); while the remainder included solely tertiary/hospital practitioners (n = 4), practitioners across a variety of practice settings (n = 5), or the authors didn’t inquire about or specify the practice location of participants (n = 2). Four studies also included service user and/or family members as participants (Carbone et al. 2010, 2013; Levy et al. 2016; Muskat et al. 2015), but any references to information collected from service users was excluded from the current review.
Most of the participants across studies identified working with at least one patient with an autism diagnosis, and 10 studies specified this experience with at least one patient with autism as inclusion criteria for participation (Bruder et al. 2012; Halpin 2016; Holmes et al. 2014; James et al. 2014; Kuhlthau et al. 2015; Muskat et al. 2015; Trembath et al. 2016; Warfield et al. 2015; Weil et al. 2011; Zwaigenbaum et al. 2016). Three studies specifically sought participants with specialized training or extensive experience working with autism (Halpin 2016; Kuhlthau et al. 2015; Trembath et al. 2016). Nine studies did not identify the level of experience their participants had in working with autism (Carbone et al. 2010; Fenikile et al. 2015; Kalb et al. 2017; Levy et al. 2016; Shawahna et al. 2017; Wachob and Pesci 2017; Will et al. 2013; Zuckerman et al. 2013; Zerbo et al. 2015).
The majority of studies in this review (n = 20) specifically explored provider experiences working with children and youth with autism (Broder-Fingert et al. 2014; Carbone et al. 2010, 2013; Eseigbe et al. 2015; Fenikile et al. 2015; Garg et al. 2014; Halpin 2016; Holmes et al. 2014; James et al. 2014; Kalb et al. 2017; Kuhlthau et al. 2015; Levy et al. 2016; Morris et al. 2018; Muskat et al. 2015; Shawahna et al. 207; Trembath et al. 2016; Weil et al. 2010; Will et al. 2013; Zuckerman et al. 2013; Zwaigenbaum et al. 2016). Three studies were specific to care of adults with autism (Bruder et al. 2012; Warfield et al. 2015; Zerbo et al. 2015), and the other four studies either noted both children and adults or did not specify an age frame (Daley and Sigman 2002; Unigwe et al. 2017; Wachob and Pesci 2017; Weil et al. 2011).
The key themes that were emphasized across studies included (1) complexity beyond usual role, (2) limited knowledge and resources, (3) training/prior experience, (4) communication and collaboration, (5) need for information and training, and (6) need for care coordination and systemic changes (see Table 2). All six themes remained present when controlling for provider practice location and age range of patient population.
A summary of included studies with country of origin, role of healthcare professional participants, and themes addressed organized by number in the order as listed above is provided in Table 3.
Complexity Beyond Usual Role
Many of the healthcare professionals across studies in this review referred to the complexity of working with patients with autism who often require additional services or supports beyond that which is typically provided in their role as a healthcare provider. This theme at times was directly labelled and at times came across in participants responses in studies that explored the role of healthcare professionals when working with patients with autism.
Seven of the 17 quantitative and nine of the 14 qualitative studies revealed themes related to the complexity beyond their usual role (Bruder et al. 2012; Carbone et al. 2010, 2013; Daley and Sigman 2002; Eseigbe et al. 2015; Fenikile et al. 2015; Garg et al. 2014; James et al. 2014; Levy et al. 2016; Morris et al. 2018; Unigwe et al. 2017; Warfield et al. 2015; Will et al. 2013; Zerbo et al. 2015).
Specifically, the seven quantitative studies focused on the lack of confidence and clarity around roles of healthcare providers when working with individuals with autism (Bruder et al. 2012; Carbone et al. 2013; Eseigbe et al. 2015; Garg et al. 2014; James et al. 2014; Unigwe et al. 2017; Will et al. 2013). Family physicians in particular across several studies noted frequently referring patients with autism to other healthcare professionals, such as pediatricians or psychiatrists (Eseigbe et al. 2015; Garg et al. 2014; Unigwe et al. 2017).
Across qualitative studies with physician and pediatrician participants in particular, many endorsed the perception that patients with autism were particularly complex, which limited their ability to provide comprehensive care services (Carbone et al. 2010; Daley and Sigman 2002; Fenikile et al. 2015; Levy et al. 2016; Unigwe et al. 2017). For instance, pediatricians in two qualitative studies noted that they rarely see their clients with autism beyond annual check-ups or acute illness visits, and they prefer to refer to specialists for comprehensive treatment such as initiation of medications (Carbone et al. 2010; Levy et al. 2016). Similarly family physicians in the study by Fenikile et al. (2015) preferred to refer to specialists for assessment and management of autism-related symptoms. One family physician participant noted “even with appropriate training, GPs do not have the resources properly to diagnose or look after patients/carers with autism” (Unigwe et al. 2017, p. 3450). Physicians in Warfield et al.’ (2015) study noted that when they did provide care, they were required to put in extra effort and time for activities such as care coordination, which they were not reimbursed for. Similarly, social workers in Morris et al. (2018) study noted that a lack of clarity regarding the scope of their role within the healthcare team presented a challenge related to working with the complexity of autism in particular.
Limited Knowledge and Resources
All of the studies in this review highlighted specific factors that significantly and negatively impacted service provision with patients with autism and their families, and/or contributed to the complexity of serving this population. Many studies noted particular gaps related to limited provider knowledge and/or skills (n = 27) and limited awareness or access to resources (n = 19).
Limited Knowledge
Limited knowledge related to care provision for patients with autism was a recurring theme across 16 of the quantitative and 11 of the qualitative studies (Broder-Fingert et al. 2014; Bruder et al. 2012; Carbone et al. 2010, 2013; Daley and Sigman 2002; Eseigbe et al. 2015; Fenikile et al. 2015; Garg et al. 2014; Holmes et al. 2014; James et al. 2014; Levy et al. 2016; Morris et al. 2018; Muskat et al. 2015; Shawahna et al. 2017; Unigwe et al. 2017; Wachob and Pesci 2017; Warfield et al. 2015; Weil et al. 2010, 2011; Will et al. 2013; Zerbo et al. 2015; Zuckerman et al. 2013; Zwaigenbaum et al. 2016),
A number of quantitative studies particularly emphasized limitations with regards to clinically addressing the complex needs that individuals with autism may present with (Broder-Fingert et al. 2014; Eseigbe et al. 2015; Garg et al. 2014; Holmes et al. 2014; Unigwe et al. 2017; Zerbo et al. 2015), communicating effectively with clients with autism (Broder-Fingert et al. 2014; Holmes et al. 2014), and establishing clarity with regards to diagnostic criteria and symptomatology of autism (Daley and Sigman 2002; James et al. 2014; Shawahna et al. 2017; Zerbo et al. 2015; Zuckerman et al. 2013). Navigating the high incidence of co-occurring diagnoses and behavioural challenges that can accompany autism also revealed to be particularly challenging (Eseigbe et al. 2015), as was prescribing and monitoring medications (Garg et al. 2014; Shawahna et al. 2017; Unigwe et al. 2017), working with adults (Zerbo et al. 2015), working with cultural and language differences (Zuckerman et al. 2013), and limited knowledge of available resources (Broder-Fingert et al. 2014; Carbone et al. 2013; Garg et al. 2014; Shawahna et al. 2017; Wachob and Pesci 2017; Zerbo et al. 2015; Zuckerman et al. 2013).
A general lack of knowledge of autism etiology, symptom presentation, and diagnostic criteria was similarly noted across many of the qualitative studies (Fenikile et al. 2015; Garg et al. 2014; Levy et al. 2016; Warfield et al. 2015; Zerbo et al. 2015). This was noted to be further exacerbated by many changes in diagnostic criteria (Carbone et al. 2010; Fenikile et al. 2015). Specific aspects of service provision with this population that were noted as being especially challenging across qualitative studies included management of complex behaviours (Carbone et al. 2010; Zwaigenbaum et al. 2016), medication initiation and management (Carbone et al. 2010; Garg et al. 2014), and management of co-occurring medical and mental health conditions (Zerbo et al. 2015).
Limited Resources
Limited awareness or availability of autism-related resources and specialized supports was highlighted across eight quantitative and twelve qualitative studies (Broder-Fingert et al. 2014; Carbone et al. 2010; Daley and Sigman 2002; Eseigbe et al. 2015; Fenikile et al. 2015; Garg et al. 2014; Halpin 2016; Kalb et al. 2017; Kuhlthau et al. 2015; Levy et al. 2016; Morris et al. 2018; Muskat et al. 2015; Unigwe et al. 2017; Wachob and Pesci 2017; Warfield et al. 2015; Will et al. 2013; Zerbo et al. 2015; Zuckerman et al. 2013; Zwaigenbaum et al. 2016).
Participants across four quantitative and four qualitative studies noted that individuals with autism often required a longer time commitment during and outside of visits, and a lack of reimbursement for this time was a resource barrier to service provision (Carbone et al. 2010; Eseigbe et al. 2015; Unigwe et al. 2017; Warfield et al. 2015; Weil et al. 2010, 2011; Will et al. 2013; Zwaigenbaum et al. 2016). One physician in a qualitative study stated “gosh how do I even tell you how much time I spend with this, it’s a problem, that’s why nobody wants to see people. It’s not compensated” (Warfield et al. 2015, p. 2213). Many participants across studies spoke about limited time and/or resources to coordinate care (Carbone et al. 2010; Daley and Sigman 2002; Garg et al. 2014; Halpin 2016; Muskat et al. 2015; Warfield et al. 2015).
Sparsity of community-based services was noted across six qualitative studies as a challenge to service provision, particularly for adolescent children and adults and in rural communities (Carbone et al. 2010; Daley and Sigman 2002; Fenikile et al. 2015; Garg et al. 2014; Unigwe et al. 2017; Warfield et al. 2015). One family physician endorsed a hesitation to routinely screen for autism, and stated “if there are resources to refer them to, sure. But I don’t want to screen for something I can’t get services for” (Fenikile et al. 2015, p. 361). Another physician noted “the relatively few services for children and adults [on the autism spectrum] are in a constant state of flux and impossible to keep up with” (Unigwe et al. 2017, p. e450).
Training/Prior Experience
A number of studies reported themes related to autism-specific training and prior experience with autism on a professional or personal basis. This theme was brought up from the perspective of being a barrier to care when training and experience is limited (n = 11), and being a facilitator to care among professionals who had participated in training or had prior experience with individuals with autism both on a professional and personal level (n = 6).
Training
Nine quantitative and two qualitative studies referred to autism-specific training as a current or potential facilitator to care (Carbone et al. 2013; Daley and Sigman 2002; Halpin 2016; Holmes et al. 2014; Unigwe et al. 2017; Wachob and Pesci 2017; Warfield 2015; Weil et al. 2010, 2011; Zerbo et al. 2015).
Healthcare providers across many of the quantitative studies reported limited access to education, training, and experience working with clients with autism in their role (Daley and Sigman 2002; Holmes et al. 2014; Unigwe et al. 2017; Wachob and Pesci 2017; Weil et al. 2010, 2011; Zerbo et al. 2015). Similarly, physician participants in two qualitative studies noted that their training was self-directed and required personal initiative and motivation, which was usually driven by a personal connection to autism outside of the professional setting (Warfield et al. 2015; Zerbo et al. 2015). One participant in a qualitative study noted the importance of initiative in seeking out training when it is not offered formally, and stated:
I didn’t find a lot in the way of formal programs. I ended up working with people one-on-one actually; found a mentor who was great to connect me to specific people who are doing projects or who could teach me things. So it was more of a one-to-one basis on my own initiative (Warfield et al. 2015, p. 2214).
Prior Experience
Four quantitative and two qualitative studies noted that healthcare providers valued prior experience with autism, both on a professional and personal level as facilitating continued quality of care with this population (Carbone et al. 2013; Muskat et al. 2015; Unigwe et al. 2017; Wachob and Pesci 2017; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Many healthcare providers in the qualitative study by Zwaigenbaum et al. (2016) noted that past experiences working with children with autism was more valuable than any training they had received in informing their practice. In the study by Muskat et al. (2015), healthcare providers reinforced the value of ‘knowing the child’, as each child and family may present with unique needs and may benefit from individualized care.
Communication and Collaboration
Nine of the 17 quantitative and all of the 14 qualitative studies in this review made reference to communication and collaboration factors as being relevant to service provision with this population. In particular, communication with patients with autism (n = 4) and their families (n = 12) and the need to utilize unique communication strategies and/or make accommodations for communication or sensory differences were noted across studies to facilitate effective service provision with this population. Several of the qualitative studies in this review reported collaboration as a factor facilitating service provision with patients with autism, which includes collaboration with families (n = 11) and with professionals (n = 6) within the internal healthcare team as well as external or community service providers and supports. Collaboration was not addressed in any of the quantitative studies.
Communication with Patient
Barriers to communication with individuals with autism was addressed across four quantitative and four qualitative studies (Broder-Fingert et al. 2014; Carbone et al. 2010; Holmes et al. 2014; Fenikile et al. 2015; Garg et al. 2014; Levy et al. 2016; Muskat et al. 2015; Unigwe et al. 2017; Warfield et al. 2015; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Feelings of discomfort with communication of treatment options was identified as a barrier to care across several qualitative studies, particularly among physicians and pediatricians (Carbone et al. 2010; Fenikile et al. 2015; Garg et al. 2014; Levy et al. 2016; Muskat et al. 2015; Unigwe et al. 2017; Warfield et al. 2015; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Additional challenges related to communication highlighted across qualitative studies included ability of client to articulate experiences of pain or internal physical changes, need for non-verbal means of communication, and difficulty establishing rapport (Muskat et al. 2015; Warfield et al. 2015; Zerbo et al. 2015; Zwaigenbaum et al. 2016).
One quantitative and three qualitative studies addressed effective or helpful communication strategies that healthcare providers used when working with patients with autism and their families (Morris et al. 2018; Unigwe et al. 2017; Zerbo et al. 2015; Zwaigenbaum et al. 2016). For example, participants in the qualitative study by Zwaigenbaum et al. (2016) identified helpful strategies for communicating with patients with autism such as slowing the speed of communication, attending to non-verbal forms of communication, and maintaining an ongoing assessment of symptoms of stress and anxiety. One physician in the study by Zerbo et al. (2015) spoke of her unique approach when communicating with adults with autism and stated:
Well, [conversation] is kind of focused on how are they doing today. How are you right now? Are you comfortable? I try to build rapport and set patients at ease, and try to be with them where they are. Whether it’s more personal space or less personal space, sometimes I sit beside the patient, so I am not looking directly at them, I’m not facing them…. And then, I focus on what brought them in today (Zerbo et al. 2015, p. 4009).
Participants in two qualitative studies (Morris et al. 2018; Zwaigenbaum et al. 2016) endorsed some sensory and environmental accommodations that may help to reduce stress and subsequently increase opportunity to effectively communicate with patients with autism, including scaffolding medical procedures and providing private rooms, child-friendly décor, and distractions such as toys and video games.
Communication with Caregivers
Limited ability to engage in effective communication with caregivers was noted in five quantitative and seven qualitative studies as a challenge to service provision with this population (Carbone et al. 2010; Daley and Sigman 2002; Eseigbe et al. 2015; Fenikile et al. 2015; Holmes et al. 2014; Levy et al. 2016; Shawahna et al. 2017; Trembath et al. 2016; Unigwe et al. 2017; Warfield et al. 2015; Will et al. 2013; Zerbo et al. 2015; Zuckerman et al. 2013).
Specific barriers to effective caregiver communication noted across quantitative studies included navigating caregiver perspectives that differ from provider perspectives (Eseigbe et al. 2015; Holmes et al. 2014; Will et al. 2013; Zuckerman et al. 2013), awareness of how to help families navigate treatment options (Shawahna et al. 2017), and perceived resistance from parents to understand diagnosis or engage in discussions related to treatment (Eseigbe et al. 2015; Holmes et al. 2014; Will et al. 2013; Zuckerman et al. 2013). In the quantitative study by Unigwe et al. (2017), physicians noted the aspect of their role that they felt most comfortable to carry out was “identifying stress in the parents and carers of my patients with autism”, which resulted in a mean rating of 6.3 on a likert scale ranging from 1 (“not at all confident”) to 10 (“extremely confident”).
Participants across qualitative studies also spoke of challenges related to navigating caregiver perspectives and beliefs that differ from those of the provider (Daley and Sigman 2002; Fenikile et al. 2015; Levy et al. 2016). Of the pediatricians in the study by Levy et al. (2016), only a few reported challenges with engagement in discussions with families regarding treatment options and resources. One study noted that cultural differences were seen to potentially impact family perspectives and acknowledgement of autism symptoms and treatment (Daley and Sigman 2002), and another noted that parent motivation and confidence, mental health, language differences, and learning disabilities of parents can impact communication and provide relationships with families/caregivers (Trembath et al. 2016). Pediatricians in a study by Carbone et al. (2010) identified a desire to support parents who are experiencing stress, but acknowledged having limited skills in addressing and supporting caregiver stress.
Physicians in the qualitative study by Zerbo et al. (2015) noted that visits take more time when caregivers are present, and that this can also introduce challenges to privacy and topics of discussion during the visit, such as sexual activity and substance use. Similarly, physicians in the qualitative study by Warfield et al. (2015) spoke of the complexity of family members attending appointments which one participant summarized by stating:
Well, they are much more likely, almost 100% likely to have someone with them. Which is different. You know, most adults tend to come to the doctors by themselves. Or at least if they bring someone with them the other person really isn’t participating in the visit. So right away you have two patients. You have the patient and then you have the patient’s significant others. So that’s very different. And that’s something that a lot of internists aren’t used to (Warfield et al. 2015, p. 2213).
Collaboration with Families
No quantitative but eleven qualitative studies highlighted collaboration with families as being a facilitator to effective healthcare service provision (Carbone et al. 2010; Daley and Sigman 2002; Halpin 2016; Kuhlthau et al. 2015; Levy et al. 2016; Morris et al. 2018; Muskat et al. 2015; Trembath et al. 2016; Unigwe et al. 2017; Zerbo et al. 2015; Zwaigenbaum et al. 2016).
Eight qualitative studies noted an emphasis on collaboration with families as being an integral aspect of the healthcare provider role with this population (Carbone et al. 2010; Halpin 2016; Kuhlthau et al. 2015; Morris et al. 2018; Muskat et al. 2015; Unigwe et al. 2017; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Physicians in the qualitative study by Zerbo et al. (2015) noted that office visits tended to be longer when family members or caregivers were present, but one physician noted that this is not unique to autism and that working alongside families is part of their role. Nurses in Halpin (2016) and social workers in Morris et al. (2018) perceived family collaboration and family-centered care as central to their role on the healthcare team, One social worker in Morris et al. (2018, p. 9) summarized this by stating:
I’d say the biggest thing I do to help is educating others. And listening to families, letting them know I get it. I get that this is an issue and it’s going to be more challenging. I’ve listened to that and I believe it and I’m going to do my best to put whatever into place that can make it go a little bit more smoothly for you.
Several of the participants across qualitative studies identified the need to prioritize parent and caregiver concerns during visits and incorporate family input and expertise into the assessment and treatment plan (Carbone et al. 2010; Halpin 2016; Kuhlthau et al. 2015; Morris et al. 2018; Muskat et al. 2015; Zwaigenbaum et al. 2016). One healthcare provider in the study by Muskat et al. (2015) stated “[these parents are] very helpful in telling me how to best care for their child; they know their child the best and I very much look for their expertise with their child” (p. 487). Several studies also reinforced the importance of providing information to parents to empower the parental role in care coordination and decision making (Daley and Sigman 2002; Kuhlthau et al. 2015; Halpin 2016; Levy et al. 2016; Morris et al. 2018; Trembath et al. 2016).
Collaboration with Professionals
No quantitative but six qualitative studies noted collaboration with other professionals as facilitating service provision with individuals with autism (Carbone et al. 2010; Kuhlthau et al. 2015; Morris et al. 2018; Warfield et al. 2015; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Three studies reinforced the value of working with an inter-professional team, which allowed for care coordination and holistic service provision (Carbone et al. 2010; Morris et al. 2018; Warfield et al. 2015; Zwaigenbaum et al. 2016). In the study by Zwaigenbaum et al. (2016), social workers in particular were recognized as helpful for complex situations and supporting families in navigating the hospital and community service systems. The healthcare providers in this study also recognized the value of non-medical members of the healthcare team such as Child Life specialists who can provide an opportunity for distraction and parent respite, and volunteers who can provide general assistance as needed (Zwaigenbaum et al. 2016).
Three qualitative studies spoke of collaboration with professionals external to the localized team (Kuhlthau et al. 2015; Morris et al. 2018; Warfield et al. 2015). Pediatric healthcare providers in the study by Kuhlthau et al. (2015) noted helpful strategies such as a centralized resource of information that could be passed on to the next healthcare provider as youth transition into adult services. They also spoke of generating a list of resources, maintaining communication with other providers that the child works with, and generating cross-professional partnerships (Kuhlthau et al. 2015).
Need for Information and Training
A number of studies highlighted themes related to the needs of professionals to support enhanced quality of service provision with patients with autism. Many healthcare providers across studies in this review identified a need for access to up-to-date information and research (n = 7) and skills training relevant to diagnosis, assessment, and intervention for individuals with autism who enter the healthcare system (n = 14).
Need for Information
Participants across three quantitative and four qualitative studies highlighted a need for access to information and research relevant to autism, including websites and/or lists of community resources, and evidence-based guidelines or checklists for care coordination (Carbone et al. 2010; Daley and Sigman 2002; Garg et al. 2014; James et al. 2014; Unigwe et al. 2017; Warfield et al. 2015; Zerbo et al. 2015). The occupational therapists in the quantitative study by James et al. (2014) identified preferred methods of receiving information, which included research updates (85%), autism screening methods (81%), and reading material for families (76%). A list of community resources was identified as the greatest need by participants in Zerbo et al. (2015).
Need for Training
Seven quantitative and ten qualitative studies reported that healthcare providers identified a need for opportunities to participate in training opportunities relevant to working with clients with autism as a necessary component to effective service provision with this population (Bruder et al. 2012; Carbone et al. 2010; Daley and Sigman 2002; Fenikile et al. 2015; Garg et al. 2014; Kuhlthau et al. 2015; Levy et al. 2016; Muskat et al. 2015; Shawahna et al. 2017; Unigwe et al. 2017; Warfield et al. 2015; Weil et al. 2010; Will et al. 2013; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Participants across two quantitative studies noted that they were more likely to indicate a desire for continuing education if they were already working with clients with autism diagnoses in their care (Bruder et al. 2012; Weil et al. 2010). When asked what type of training would be most useful, 70% of physicians in the quantitative study by Zerbo et al. (2015) selected “training on effective communication strategies with ASD patients” (p. 4005).
Participants across qualitative studies requested training on autism more broadly including diagnostic criteria, symptomatology, co-morbidities, treatment options, and practice strategies (Carbone et al. 2010; Daley and Signman 2002; Fenikile et al. 2015; Garg et al. 2014; Kuhlthau et al. 2015; Levy et al. 2016; Muskat et al. 2015; Unigwe et al. 2017; Zwaigenbaum et al. 2016). In one study, physicians who work with adults requested education on working with adults specifically, as well as training on relevant but non-medical information such as guardianship policies and housing issues (Warfield et al. 2015). Healthcare providers in Zwaigenbaum et al. (2016) specifically requested pragmatic training that only required a small time commitment.
Need for Care Coordination and Systemic Changes
Seven qualitative studies highlighted a professional need for systemic supports and changes including access to care coordination services (n = 6) and environmental or procedural changes that may contribute to increased accessibility and efficiency of care, such as financial compensation for time, access to specialized supports, and resources to provide to families (n = 5). This theme was not found across any of the quantitative studies.
Care Coordination
Six qualitative studies highlighted a need for care coordination when working with this population (Carbone et al. 2010; Fenikile et al. 2015; Kuhlthau et al. 2015; Warfield et al. 2015; Zerbo et al. 2015; Zwaigenbaum et al. 2016). Care coordination was defined differently across studies, but common conceptualizations included having a specific person who can facilitate communication among all involved parties (individual, families, and healthcare providers), provide case management, service navigation and referrals, and/or information to families to empower them to coordinate care for their child/youth (Carbone et al. 2010; Fenikile et al. 2015; Kuhlthau et al. 2015). Two studies specifically noted a need to increase communication between primary care physicians and pediatricians (Warfield et al. 2015; Zerbo et al. 2015). Healthcare providers in Zwaigenbaum et al. (2016) recommended implementation of a personalized ‘life plan’ to be shared among service professionals.
Systemic Changes
Five qualitative studies acknowledged a need for systemic changes in order to support healthcare services provision with this population (Fenikile et al. 2015; Kuhlthau et al. 2015; Muskat et al. 2015; Warfield et al. 2015; Zwaigenbaum et al. 2016).
The need to consider adaptations to the healthcare environment was advocated for by healthcare professionals across three studies who recognized the rigidity of the healthcare environment as a barrier to care (Muskat et al. 2015; Warfield et al. 2015; Zwaigenbaum et al. 2016). One healthcare provider noted “a hospital is a very inflexible place, it doesn’t adapt itself to the people who are in it…we’re just not that type of place or organization that serves the children well because that’s not the way we work” (Muskat et al. 2015, p. 486). Healthcare providers working in the emergency room recommended the implementation of strategies to expedite triage of care, reduce sensory stimulation, and provide additional methods of distraction (Zwaigenbaum et al. 2016).
In addition, the provision of financial incentives for healthcare providers to spend more time with clients with autism and their families was identified as a means of enticing healthcare providers to work with this population (Fenikile et al. 2015; Kuhltahu et al. 2015; Warfield et al. 2015). Participants in two studies emphasized a need for specialized supports within their healthcare settings that could provide support and consultation related to working with clients with autism (Muskat et al. 2015; Zwaigenbaum et al. 2016).
Discussion
This manuscript presents an overview of key themes across quantitative and qualitative studies related to the experience of healthcare providers caring for individuals with autism. The six themes highlighted in this review included (1) complexity beyond usual role, (2) limited knowledge and resources, (3) training/prior experience, (4) communication and collaboration, (5) need for information and training, and (6) need for care communication and systemic changes. These findings support and corroborate the aforementioned research with individuals with autism and their families identifying difficulties accessing knowledgeable providers with autism-relevant skills in effective patient-provider communication and collaboration (Chiri and Warfield 2012; Dern and Sappok 2016; Nicolaidis et al. 2013, 2015; Raymaker et al. 2017; Strunk et al. 2014; Vogan et al. 2017; Wilson and Peterson 2018). These two perspectives together fortify a critical need to enact change across healthcare systems worldwide.
In addition to providing a clear overview of themes related to healthcare providers’ experiences caring for this population, these themes can be applied to other populations encountered by providers. For instance, communication and collaboration with patients, caregivers, and professionals are critical skills when caring for any population within the healthcare system. Zerbo et al. (2015) note this in their assertion that collaboration with families and caregivers is not unique to populations of individuals with autism but, instead, a part of the physician role with all patients. A lack of specialized training is another theme that has been identified in the literature with other populations: Social work participants in Muskat et al.’s (2017) study described a lack of previous training providing end-of-life care to children in an acute -care hospital setting, leading them to independently seek out learning opportunities or work with a “trial by fire” approach (p. 510).
A conceptualization of autism as a complex/ambiguous diagnosis requiring comprehensive and specialized care seemed to underlie many of the studies in this review. Healthcare providers perceived that they were limited in their ability to provide the supports that these clients and families need, and identified a need for collaboration with other professionals, access to specialists, and concrete and practical guidelines for how to effectively work with this population.
If healthcare providers continue to feel limitations in their abilities and scope of practice they may increasingly defer to specialists for assessment and treatment of patients with autism. This could create ongoing strain on the healthcare system and reduce multi-systemic capacity to meet the health needs of this population. Ambiguity on the part of health care professionals may be attributed to the diagnosis of autism itself, which has not only been reformed and changed multiple times since its inception, but also remains open to clinical interpretation. Healthcare professionals often note this as a significant barrier to consistent assessment and intervention practices (Cerier et al. 2018; Lord et al. 2012; Silverman 2011; Verhoeff 2013).
Themes noted across studies relating to facilitators to service provision included provider knowledge and experience, communication and collaboration with families, and collaboration across professionals. Some training programs have been developed for healthcare providers working with individuals with autism, with resulting improvements in provider knowledge and skill particularly noted with those that provide exposure to real-life or case study experiences (Elmensdorp 2011; Havercamp et al. 2016; Lucarelli et al. 2018; Mazurek et al. 2016; McGonigle et al. 2014). Provider preparedness, self-efficacy, and confidence may allow space for initiative and creativity in adapting healthcare practices to more effectively meet the needs of patients with autism.
All of the reviewed studies revealed themes related to challenges to service provision. This may be because themes related to challenges and barriers are particularly relevant to healthcare provider practice with this population, but it is worth considering the ways that research design and questions may implicitly frame autism as an especially complex diagnosis that is expected to generate barriers to care. If researchers themselves believe that autism is challenging, and that these clients may be especially hard to provide services for, then research question, data collection methods, and attention to themes may be influenced by this perception.
Future Research Considerations
The reviewed studies were conducted across various programs in healthcare. Future research would benefit from a comparison of differences among specific programs and/or focus on a particular program for deeper analysis of themes. For example, research indicates that autism is highly correlated with mental health difficulties (Bradley et al. 2004; Buck et al. 2014; Moseley et al. 2011), therefore, focus on service provision for individuals with co-morbid autism and mental health concerns may be valuable.
Future studies may also consider attempts to incorporate diversity of factors that have not been comprehensively included in research to date, for example country of origin, culture and ethnicity. A focus on care provision to specific sub-populations of individuals with autism, specifically adults and women, is needed. In addition, research would benefit from an increased focus on facilitators to care, including provider approaches that contribute to care for this population. Lastly, increased inclusion of the perceptions and experiences of both service users and service providers will allow for a more robust exploration of opportunities to enhance healthcare services with this population.
Methodologically speaking the majority of the studies in this review collected either quantitative or qualitative data. Only four studies in this review employed a mix of methods for data collection. Future researchers may consider the merits of contributing works that obtain both quantifiable and subjective data. Quantitative researchers may wish to consider using the results of this review as a basis for rational-theoretical approach to survey design that captures thematic constructs commonly associated with the experiences of healthcare providers working with autism. We also recommend that forthcoming qualitative studies richen the knowledge base by delving deeper into the findings and limitations identified in this current project.
Limitations
There are a number of notable limitations both in the included studies and in the current research design. Of the 27 studies, 17 were conducted in the United States. As a result, the themes and findings may not be as relevant when considered on an international scale. This may be exacerbated by the vast diversity in healthcare system frameworks across nations. Many studies did not collect demographic information (i.e., Bruder et al. 2012; Carbone et al. 2010, 2013; Daley and Sigman 2002; Halpin 2016; Kuhlthau et al. 2015; Muskat et al. 2015; Warfield et al. 2015; Zerbo et al. 2015). Of the studies that inquired about ethnicity, a significant proportion identified as “white/Caucasian” (Holmes et al. 2014; James et al. 2014; Kalb et al. 2017; Levy et al. 2016; Morris et al. 2018; Unigwe et al. 2017). It is unclear how cultural or ethnic factors may have played a role in healthcare provider perceptions and experiences.
While the majority of participants across studies had experience with at least one patient with autism, only three of the reviewed studies specifically explored the perspectives of healthcare providers with specialized training and experience in autism. The themes in this study thus may not be representative of the experiences of providers with specialized training or extensive experience working with autism. In addition, across most of the reviewed studies participants were specifically speaking to their experiences with children and youth, which may have impacted the presence of some themes such as those related to parents and caregivers.
With regards to this current review, a scoping review methodology does not incorporate an analysis of methodological rigour of studies included in the synthesis. It may be appropriate for future research to consider a systematic review of the research as the literature in this area builds. In addition, the participants across the reviewed studies represented diverse disciplinary professions. Analysis of between-group differences may be relevant for future clinical practice and research.
Conclusion
While the experiences of people with autism and their families should continue to be captured to inform best practices, an understanding of the gaps in healthcare service provision with this population may be more holistically understood by incorporating the perceptions and experiences of professionals providing care. This review allows for a robust understanding of themes related to challenges and facilitators to service provision, and professional needs that may be translated into clinical practice and future research considerations. This review supports a push from policy makers, researchers, clinicians, and community members for research attention to be directed towards the assessment of healthcare interventions and service provision with this population (Pellicano et al. 2014). The results of this review should be considered when reflecting on opportunities to enhance healthcare practices and future research with patients with autism and their families, in order to support and maintain the provision of patient- and family-centered practices with this population.
References
Anderson, S., Allen, P., Peckham, S., & Goodwin, N. (2008). Asking the right questions: Scoping studies in the commissioning of research on the organization and delivery of health services. Health Research Policy and Systems, 6, 7–19.
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32.
Atun-Einy, O., & Ben-Sasson, A. (2018). Pediatric allied healthcare professionals’ knowledge and self-efficacy regarding ASD. Research in Autism Spectrum Disorders, 47, 1–13.
Baldwin, S., & Costley, D. (2015). The experiences and needs of female adults with high-functioning autism spectrum disorder. Autism, 20(4), 483–495.
Barber, C. (2017). Meeting the healthcare needs of adults on the autism spectrum. British Journal of Nursing, 26(7), 420–425.
Bradley, E., Summers, A., Wood, H. L., & Bryson, S. E. (2004). Comparing rates of psychiatric and behaviour disorders in adolescents and young adults with severe intellectual disability with and without autism. Journal of Autism and Developmental Disorders, 34(2), 151–161.
Broder-Fingert, S., Ferrone, C. F., Giauque, A., & Connors, S. L. (2014). Residents’ knowledge and comfort with caring for children with autism spectrum disorder. Clinical Pediatrics, 53(14), 1390–1392.
Bruder, M. B., Kerins, G., Mazzarella, C., Sims, J., & Stein, N. (2012). Brief report: The medical care of adults with autism spectrum disorders: Identifying the needs. Journal of Autism and Developmental Disorders, 42(11), 2498–2504.
Buck, T. R., Viskochil, J., Farley, M., Coon, H., McMahon, W. M., Morgan, J., & Bilder, D. A. (2014). Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 3063–3071.
Carbone, P. S., Behl, D. D., Azor, V., & Murphy, N. A. (2010). The medical home for children with autism spectrum disorders: Parent and pediatrician perspectives. Journal of Autism and Developmental Disorders, 40(3), 317–324.
Carbone, P. S., Murphy, N. A., Norlin, C., Azor, V., Sheng, X., & Young, P. C. (2013). Parent and pediatrician perspectives regarding the primary care of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(4), 964–972.
Cerier, E., Beal, E. W., Chakedis, J., Chen, Q., Paredes, A., Sun, S., … Pawlik, T. M. (2018). Patient-provider relationships and health outcomes among hepatopancreatobiliary patients. Journal of Surgical Research, 228(3), 290–298.
Chiri, G., & Warfield, M. E. (2012). Unmet need and problems accessing core health care services for children with autism spectrum disorder. Maternal and Child Health Journal, 16(5), 1081–1091.
Christensen, D. L., Baio, J., Braun, K. V., Bilder, D., Charles, J., Constantino, J. N., … Yeargin-Allsopp, M. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR, 65(3), 1–23.
Cummings, J. R., Lynch, F. L., Rust, K. C., Coleman, K. J., Madden, J. M., Owen-Smith, A. A.,… Croen, L. A. (2016). Health services utilization among children with and without autism spectrum disorders. Journal of Autism and Developmental Disorders, 46(3), 910–920.
Daley, T. C., & Sigman, M. D. (2002). Diagnostic conceptualization of autism among Indian psychiatrists, psychologists, and pediatricians. Journal of Autism and Developmental Disorders, 32(1), 13–23.
Dern, S., & Sappok, T. (2016). Barriers to healthcare for people on the autism spectrum. Advances in Autism, 2(1), 2–11.
Elmensdorp, S. T. (2011). Training physicians on the early behavioral characteristics of autism: The use of a brief, group didactic training module. Doctoral dissertation. Proquest (3456129).
Elsabbagh, M., Divan, G., Koh, Y., Kim, Y. S., Kauchali, S., Marcin, C.,… Fombonne, E. (2012). Global prevalence of autism and other pervasive developmental disorders. Autism Research, 5(3), 160–179.
Eseigbe, E. E., Nuhu, F. T., Sheikh, T. L., Eseigbe, P., & Olisah, V. O. (2015). Knowledge of childhood autism and challenges of management among medical doctors in Kaduna State, Northwest Nigeria. Autism Research and Treatment, 2015(892301), 1–6.
Fenikile, T. S., Ellerbeck, K., Filippi, M. K., & Daley, C. M. (2015). Barriers to autism screening in family medicine practice: A qualitative study. Primary Health Care Research & Development, 16(4), 356–366.
Garg, P., Lillystone, D., Dossetor, D., Kefford, C., & Chong, S. (2014). An exploratory survey for understanding perceptions, knowledge, and educational needs of general practitioners regarding autistic disorders in New South Wales (NSW), Australia. Journal of Clinical and Diagnostic Research, 8(7), PC01–PC09.
Halpin, J. (2016). What do nurses think they are doing in pre-school autism assessment. British Journal of Nursing, 25(6), 319–323.
Havercamp, S. M., Ratliff-Schaub, K., Macho, P. N., Johnson, C. N., Bush, K. L., & Souders, H. T. (2016). Preparing tomorrow’s doctors to care for patients with autism spectrum disorder. Intellectual and Developmental Disabilities, 54(3), 202–216.
Heidgerken, A. D., Geffken, G., Modi, A., & Frakey, L. (2005). A survey of autism knowledge in a health care setting. Journal of Autism and Developmental Disorders, 35(3), 323–330.
Holmes, L. G., Himle, M. B., Sewell, K. K., Carbone, P. S., Strassberg, D. S., & Murphy, N. A. (2014). Addressing sexuality in youth with autism spectrum disorders: Current pediatric practices and barriers. Journal of Developmental & Behavioral Pediatrics, 35(3), 172–178.
Hubner, L. M., Feldman, H. M., & Huffman, L. C. (2016). Parent-reported shared decision making: Autism spectrum disorder and other neurodevelopmental disorders. Journal of Developmental & Behavioral Pediatrics, 37(1), 20–32.
James, L. W., Pizur-Barnekow, K. A., & Schefkind, S. (2014). Online survey examining practitioners’ perceived preparedness in the early identification of autism. The American Journal of Occupational Therapy, 68(1), e13–e20.
Joseph-Kent, K. E. (2016). Autism spectrum disorders and the healthcare experiences of aging adults. Doctoral dissertation. Proquest (10306806).
Kalb, L. G., Stuart, E. A., Mandell, D. S., Olfson, M., & Vasa, R. A. (2017). Management of mental health crises among youths with and without ASD: A national survey of child psychiatrists. Psychiatric Services, 68(10), 1039–1045.
Kogan, M. D., Strickland, B. B., Blumberg, S. J., Singh, G. K., Perrin, J. M., & van Dyck, P. (2008). A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics, 122(6), e1149–e1158.
Kuhlthau, K. A., Warfield, M. E., Hurson, J., Delahaye, J., & Crossman, M. K. (2015). Pediatric provider’s perspectives on the transition to adult health care for youth with autism spectrum disorder: Current strategies and promising new directions. Autism, 19(3), 262–271.
Levy, S. E., Frasso, R., Colantonio, S., Reed, H., Stein, G., Barg, F. K., Mandell, D. S., & Fiks, A. G. (2016). Shared decision making and treatment decisions for young children with autism spectrum disorder. Academic Pediatrics, 16(6), 571–578.
Lewis, L. F. (2017). A mixed methods study of barriers to formal diagnosis of autism spectrum disorder in adults. Journal of Autism and Developmental Disorders, 47(8), 2410–2424.
Lord, C., Petkova, E., Hus, V., Gan, W., Lu, F., Martin, D. M.,… Risi, S. (2012). A multisite study of the clinical diagnosis of different autism spectrum disorders. Archives of General Psychiatry, 69(3), 306–313.
Lucarelli, J., Welchons, L., Sideridis, G., Sullivan, N. R., Chan, E., & Weissman, L. (2018). Development and evaluation of an educational initiative to improve hospital personnel preparedness to care for children with autism spectrum disorder. Journal of Developmental & Behavioral Pediatrics, 39(5), 358–364.
Lum, M., Garnett, M., & O’Connor, E. (2014). Health communication: A pilot study comparing perceptions of women with and without high functioning autism spectrum disorder. Research in Autism Spectrum Disorders, 8(12), 1713–1721.
Lynch, F., Cummings, J., Rust, K., Owen-Smith, A., Coleman, K., Madden, J., Yau, V., … Croen, L. (2014). PS1-39: Health care utilization for children with and without autism spectrum disorders in five large health systems. Clinical Medicine and Research, 12(1–2), 83.
Mattingly, T. J., Tom, S. E., Stuart, B., & Onukwugha, E. (2017). Examining patient-provider relationship (PPR) quality and patient activation in the Medicare population. Aging Clinical and Experimental Research, 29(3), 543–548.
Mazurek, M. O., Brown, R., Curran, A., & Sohl, K. (2016). ECHO Autism: A new model for training primary care providers in best-practice care for children with autism. Clinical Pediatrics, 56(3), 247–256.
McGonigle, J. J., Migyanka, J. M., Glor-Scheib, S. J., Cramer, R., Fratangeli, J. J., Hegde, G. G.,… Venkat, A. (2014). Development and evaluation of educational materials for pre-hospital and emergency department personnel on the care of patients with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(5), 1252–1259.
Morris, R., Muskat, B., & Greenblatt, A. (2018). Working with children with autism and their families. Pediatric social worker perceptions of family needs and the role of social work. Social Work in Health Care, 57(7), 483–501.
Moseley, D. S., Tonge, B. J., Brereton, A. V., & Einfeld, S. L. (2011). Psychiatric comorbidity in adolescents and young adults with autism. Journal of Mental Health Research in Intellectual Disabilities, 4(4), 229–243.
Muskat, B., Brownstone, D., & Greenblatt, A. (2017). The experiences of pediatric social workers providing end-of-life care. Social Work in Health Care., 56(6), 505–523.
Muskat, B., Burnham Riosa, P., Nicholas, D. B., Roberts, W., Stoddart, K., & Zwaiganbaum, L. (2015). Autism comes to the hospital: Experiences of hospital care from the perspectives of children and adolescents with Autism Spectrum Disorders, their parents and health care providers. Autism, 19(4), 482–490.
Nicolaidis, C., Raymaker, D., McDonald, K., Dern, S., Boisclair, W. C., Ashkenazy, E., & Baggs, A. (2013). Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic-community partnership. Journal of General Internal Medicine, 28(6), 761–769.
Nicolaidis, C., Raymaker, D. M., Ashkenazy, E., McDonald, K. E., Dern, S., Baggs, A. E. V., Kapp, S. K., Weiner, M., & Boisclair, W. C. (2015). “Respect the way I need to communicate with you”: Healthcare experiences of adults on the autism spectrum. Autism, 19(7), 824–831.
Peacock, G., Amendah, D., Ouyang, L., & Grosse, S. D. (2012). Autism spectrum disorders and health care expenditures: The effects of co-occurring conditions. Journal of Developmental and Behavioral Pediatrics, 33(1), 2–8.
Pellicano, E., Dinsmore, A., & Charman, T. (2014). What should autism research focus upon? Community views and priorities from the United Kingdom. Autism, 18(7), 756–770.
Raymaker, D. M., McDonald, K. E., Ashkenazy, E., Gerrity, M., Baggs, A. M., Kripke, C.,… Nicolaidis, C. (2017). Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism, 21(8), 972–984.
Shawahna, R., Fahed, B., Qadri, D., Sharawi, L., Soroghli, M., & Dweik, M. (2017). Awareness and knowledge of autism spectrum disorders among pharmacists: A cross-sectional study in Palestinian pharmacy practice. Journal of Autism and Developmental Disorders, 47(6), 1618–1627.
Silverman, C. (2011). Understanding autism: Parents, doctors, and the history of a disorder. Princeton: Princeton University Press.
Solomon, O., Heritage, J., Yin, L., Maynard, D. W., & Bauman, M. L. (2016). ‘What brings him here today?’: Medical problem presentation involving children with autism spectrum disorders and typically developing children. Journal of Autism and Developmental Disorders, 46(2), 378–393.
Strunk, J. A., Pickler, R., McCain, N. L., Ameringer, S., & Myers, B. J. (2014). Managing the health care needs of adolescents with autism spectrum disorder: The parents’ experience. Families, Systems, & Health, 32(3), 328–337.
The Joanna Briggs Institute. (2015). The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI scoping reviews. https://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v2.pdf. Accessed 1 Nov 2017.
Tint, A., Weiss, J. A., & Lunsky, Y. (2017). Identifying the clinical needs and patterns of health service use of adolescent girls and women with autism spectrum disorder. Autism Research, 10(9), 1558–1566.
Trembath, D., Hawtree, R., Arciuli, J., & Caithness, T. (2016). What do speech-language pathologists think parents expect when treating their children with autism spectrum disorder? International Journal of Speech-Language Pathology, 18(3), 250–258.
Unigwe, S., Buckley, C., Crane, L., Kenny, L., Remington, A., & Pellicano, E. (2017). GPs confidence in caring for their patients on the autism spectrum: An online self-report study. British Journal of General Practice, 67(659), e445–e452.
Verhoeff, B. (2013). Autism in flux: A history of the concept from Leo Kanner to DSM-5. History of Psychiatry, 24(4), 442–458.
Vogan, V., Lake, J. K., Tint, A., Weiss, J. A., & Lunsky, Y. (2017). Tracking health care service use and the experiences of adults with autism spectrum disorder without intellectual disability: A longitudinal study of service rates, barriers and satisfaction. Disability and Health Journal, 10(2), 264–270.
Wachob, D., & Pesci, L. J. (2017). Brief report: Knowledge and confidence of emergency medical service personnel involving treatment of an individual with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(3), 887–891.
Warfield, M. E., Crossman, M. K., Delahaye, J., Weerd, D., E., & Kuhlthau, K. A. (2015). Physician perspectives on providing primary medical care to adults with autism spectrum disorders (ASD). Journal of Autism and Developmental Disorders, 45(7), 2209–2217.
Weil, T. N., Bagramian, R. A., Inglehart, M. R., & Habil, P. (2011). Treating patients with autism spectrum disorder—SCDA members’ attitudes and behavior. Special Care Dentistry, 31(1), 8–17.
Weil, T. N., Inglehart, M. R., & Habil, P. (2010). Dental education and dentists’ attitudes and behavior concerning patients with autism. Journal of Dental Education, 74(12), 1294–1307.
Weiss, J. A., Isaacs, B., Diepstra, H., Wilton, A. S., Brown, H. K., McGarry, C., & Lunsky, Y. (2018). Health concerns and health service utilization in a population cohort of young adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(1), 36–44.
Will, D., Barnfather, J., & Lesley, M. (2013). Self-perceived autism competency of primary care nurse practitioners. The Journal for Nurse Practitioners, 9(6), 350–355.
Wilson, S. A., & Peterson, C. C. (2018). Medical care experiences of children with autism and their parents: A scoping review. Child: Care, Health and Development, 44(6), 807–817.
Zerbo, O., Massolo, M. L., Qian, Y., & Croen, L. A. (2015). A study of physician knowledge and experience with autism in adults in a large integrated healthcare system. Journal of Autism and Developmental Disorders, 45(12), 4002–4014.
Zuckerman, K. E., Mattox, K., Donelan, K., Batbayar, O., Baghaee, A., & Bethell, C. (2013). Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics, 132(3), 445–453.
Zwaigenbaum, L., Nicholas, D. B., Muskat, B., Kilmer, C., Newton, A. S., Craig, W. R.,… Sharon, R. (2016). Perspectives of health care providers regarding emergency department care of children and youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(5), 1725–1736.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
RM conceived of the study; participated in its design and coordination; participated in collection, interpretation and analysis of data; and drafted the manuscript. AG participated in the design, interpretation and analysis of the data, and helped to draft the manuscript. MS participated in interpretation of data, and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morris, R., Greenblatt, A. & Saini, M. Healthcare Providers’ Experiences with Autism: A Scoping Review. J Autism Dev Disord 49, 2374–2388 (2019). https://doi.org/10.1007/s10803-019-03912-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-019-03912-6