Abstract
Limited research has explored the experiences of caregivers and their children with autism spectrum disorder (ASD) in medical settings. A qualitative meta-synthesis of studies published between 2000 and 2020 was conducted to understand and summarize the challenges faced by caregivers, their positive experiences, and suggestions for improving medical care. Themes were generated related to caregiver challenges, positive experiences, and suggestions to improve medical care. We suggest additional training of medical professionals, an interdisciplinary approach to care, more support for caregivers, and increased adaptability of the medical environment. Implications for practice, limitations, and future research directions are discussed to ensure the highest quality care to support the needs of children with ASD and their caregivers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) causes a wide variety of symptomatology including social, communication, and behavioral challenges. Children with ASD often experience comorbid conditions, including epilepsy, gastrointestinal disorders, and attention deficit hyperactivity disorder (ADHD), that can increase their need for and complicate medical treatment. Children and young adults with ASD are more likely to need medical interventions than their typically developing peers due to comorbidities and behavioral challenges (Wu et al., 2015) and have been found to utilize emergency department services four times more often than individuals without ASD (Liu et al. 2017). Similarly, children with ASD have more hospitalizations, longer hospital stays, and more physician visits (Wu et al., 2015). As a result, children with ASD have higher healthcare expenses than children without ASD, with estimates ranging from $1,163 to $5,272 increased healthcare expenditures annually (Liptak et al. 2008; Wu et al., 2015). In addition to general health, children with ASD tend to have poorer oral health and a higher need for dental intervention (Bartolomé-Villar et al., 2016).
The unique neurological differences of children with ASD, along with their increased rates of medical care, can bring unique challenges for caregivers when medical care is needed. However, research is only now emerging to gain insight into the experiences of caregivers when seeking medical care for children with ASD. Both practitioners and caregivers face challenges providing care to children with ASD in medical settings. Practitioners such as physicians, nurses, dentists, child life specialists, and therapists have been the subject of recent research on this topic. Common challenges reported across studies include limited practitioner knowledge and experience working with children with ASD, the challenging characteristics of children with ASD, and the medical setting being a difficult place for children with ASD (Jensen et al., 2020; Morris et al., 2019; Quiban, 2020; Zwaigenbaum et al., 2016). Practitioners cite the importance of utilizing an individualized care approach, as well as the need for collaboration and communication among various providers and between providers and caregivers, to improve care (Jensen et al. 2020; Morris et al., 2019; Quiban, 2020; Zwaigenbaum et al., 2016).
Caregivers have also reported a variety of challenges in medical settings with their children with ASD. Parents indicate that medical environments can be very challenging for children with ASD, citing the fast pace, long wait times, and sensory overload as common behavioral triggers (Kopecky et al., 2013; Wilson & Peterson, 2018). Additionally, Wilson and Peterson (2018) noted that caregivers perceive that healthcare providers lack compassion and respect for parental expertise, leading to low confidence in physician capability and low caregiver satisfaction. Caregivers viewed accessing quality care for their children as a “fight,” emphasizing how challenging it is to navigate the healthcare system (Hodgetts et al., 2013). Caregivers state that providers would benefit from increased training to work with patients with ASD as well as utilizing shared decision-making (Parker & Killian, 2020; Wilson & Peterson, 2018).
There are many existing theoretical frameworks in studies regarding families of children with disabilities. Such theoretical frameworks include resiliency/adaptation theories (The Resilience Model of Family Stress, Adjustment and Adaptation; McCubbin et al., 1996) and family management theories (Family Management Style Framework [FMSF]; Knafl et al., 2012). The Resiliency Model examines families of children with chronic conditions/disabilities and methods that can be used to adapt, manage, and minimize the intrusiveness of the chronic condition on family life. Utilizing a systems approach while combining both family stress theory and family resiliency theory, the model highlights the complex meaningful role the family system plays in the variability of family outcomes and the well-being of individual family members, such as parental caregivers (McCubbin et al., 1996). The FMSF provides a structure for understanding a family’s response to a child’s chronic health-related condition and challenges (Knafl et al., 2012). According to the FMSF, individuals in the family can contribute to developing a family management style or pattern of response that can influence both individual and family outcomes (Knafl et al., 2012; Knafl & Deatrick, 2003).
To date, no summary of the literature exists to understand the medical experiences of caregivers as they seek medical care for children with ASD. Yet, synthesizing the unique challenges and general patterns of perceptions for caregivers of children with ASD when seeking medical care can allow us to construct new knowledge, perspective, and theory. Accumulating evidence in qualitative research surrounding a particular phenomenon assists with broader applications, extensions, and generalizability of theories and frameworks in research to transference in clinical practice and policies (Finfgeld-Connett 2010; Hoon, 2013). Therefore, a qualitative meta-synthesis was conducted to explore and summarize the collective experiences of caregivers as they seek medical care for children with ASD. Specifically, we asked the following research questions: (1) What challenges do caregivers face when seeking medical care for individuals with ASD?; (2) What positive experiences do caregivers note and what suggestions do caregivers have for improving medical care for individuals with ASD?
Method
To address the aforementioned research questions, we utilized a qualitative meta-synthesis approach. This approach allowed us to interpret, integrate, compare, and synthesize existing qualitative studies (Sandelowski and Barroso 2007) as well as identify important gaps within the literature (Major & Savin-Baden, 2010). We employed a systematic approach to identify studies, conducted quality appraisal to ensure rigor of the included studies, and analyzed data within studies with an aim to better understand the medical experiences of caregivers of children with ASD.
Search and Screening Procedures
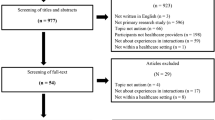
We followed the recommended reporting for systematic reviews and syntheses of the literature (Moher et al. 2010). First, we conducted searches in the following databases to identify relevant studies: (a) ProQuest, (b) PubMed, (c) Scopus, and (d) CINAHL. Search terms included the following: autism spectrum disorder or autism or autistic or ASD AND medical or doctor or hospital or inpatient or outpatient or acute care or emergency care or dentist or dental or primary care AND family or parent or mother or father or caregiver or guardian AND qualitative or perception or experience or view. Studies were included if they (a) reported caregiver (e.g., parent and guardian) perspectives of medical experiences of children ages 0–22 with ASD within various medical settings in developed countries including primary care, hospital, dental, and the emergency department; (b) included qualitative research methods (e.g., interviews and case studies); and (c) were published in a peer-reviewed journal between 2000 and 2020. We chose to focus on the past 20 years given the drastic changes in awareness of ASD in the medical field during this time period (Morris et al., 2019; Volkmar et al., 2006). Next, a hand search was conducted within journals where at least two potential studies were located in the database searches. We used the same search and inclusion criteria to identify and searched (a) Journal of Pediatric Health Care, (b) Pediatrics, (c) Pediatric Dentistry, (d) Journal of Developmental and Behavioral Pediatrics, and (e) Social Work in Healthcare. Finally, an ancestral search of relevant studies found in previous searches was conducted to identify any additional studies. Each study found within searches was first screened at the abstract level to determine if they might meet inclusion criteria. Studies that appeared to meet inclusion criteria or could not be determined with just information in the abstract were screened at the full-text level. Results from our search process are included in Fig. 1. The search resulted in 25 studies (one article included two study phases, two articles reported data from the same participants). See Table 1 for details of included studies.
PRISMA diagram of search and screening process. Note. *Studies were excluded if they did not include qualitative data, caregiver perspectives, or medical experiences, or if they were a literature review, not in peer-reviewed journal, or not published in English. Data were also excluded if they included caregiver perspectives and other participant perspectives, but data were reported in such a way that caregiver data could not be extracted.
Data Analysis, Extraction, and Quality Appraisal
The first step of our data analysis process included extracting descriptive data from each eligible study using detailed instructions and examples for each category of extraction (i.e., country where study took place, study purpose, key findings, methods, medical settings reported, and demographic information about caregivers and children with ASD). During this stage, the first author provided training to the second and third authors to ensure clarity in the process and answer questions. The second author then extracted all data, and the third author checked all extraction. Extracted data were recorded in a spreadsheet. Any disagreements about recorded data were discussed between the two research assistants until consensus was reached. If data were not reported within the study, the research assistant indicated it was not reported.
Next, we conducted a quality appraisal of each using the guidelines outlined by Lockwood et al. (2015). This included creating a spreadsheet with cells for each quality indicator outlined in the JBI critical appraisal checklist for qualitative studies (see https://jbi.global/sites/default/files/2020-08/Checklist_for_Qualitative_Research.pdf). Quality appraisal was conducted by the second author and checked by the first author. The detailed instructions with the JBI checklist were used to score each category. Quality appraisal was recorded in the spreadsheet and included ratings of yes, no, or unclear with detailed explanations of why the rating was included for each quality indicator. Any disagreements about quality indicators were discussed between the first and second authors until consensus was reached. Results of the quality appraisal are provided in the supplementary materials. No studies were excluded based on the quality appraisal.
Then, the studies were randomly split between the three authors and each author independently read their assigned studies to familiarize themselves with the data and develop a draft of emerging themes. The authors then met to compare themes/subthemes and combine and refine a draft of the themes/subthemes through continuous discussion. The themes/subthemes were then tested by all three authors with new studies randomly split between them. The authors met to discuss and refine themes based on this coding. At this stage, codes were finalized, and all three authors were randomly assigned studies to code independently using the finalized codes, first as primary and then as secondary coders. Any disagreements between primary and secondary coding were discussed until consensus was reached. The themes that emerged from the study are provided in Table 2 along with representative quotes and outlined in the “Results” section in detail.
Results
Results from this meta-synthesis provide important insights into the experiences of caregivers when seeking medical care (e.g., hospital, primary care, dental, and emergency) for individuals with ASD. Within original studies, caregivers detailed the challenges they faced obtaining medical care, positive experiences, and suggestions related to medical care for individuals with ASD.
Caregiver Challenges Obtaining Medical Care for Individuals with ASD
In the literature, caregivers noted a number of challenges when obtaining medical care for individuals with ASD. Challenges included frustration with providers, lack of provider knowledge, caregiver roles in supporting medical care, characteristics of ASD that make medical care challenging, and barriers to obtaining medical care.
Frustration with Providers
Caregivers in the included studies discussed feeling frustrated with providers. One primary area in which caregivers expressed frustration with providers was related to the judgment they received regarding their child’s behaviors. One caregiver said, “I think sometimes dentists put the pressure on the parents too much as in, you know, ‘it’s your job to make sure they brush their teeth.’ Yes but, you know, if you’ve got a child that uh violently hits you because you’re trying to do it, you, after a while...you tend to not bother” (Thomas et al., 2018, p. 230). Caregivers also felt judgment related to their treatment choices. Often, they did not want medical providers to know they were seeking alternative treatments for their child. When they did seek alternative treatments, they had no medical support. One caregiver described their experience implementing a gluten-free diet with their child with ASD: “I had no help; there was no support for that” (Carbone et al., 2010, p. 321). In addition, caregivers felt that medical professionals did not respect their expertise. A parent illustrated this point: “But when we’re not listened to...and they might not even say that but it’s their demeanor or the way that they speak to you or not speak to you” (Johnson et al. 2013, p. 390). As a result of these negative experiences, caregivers often mistrusted providers. A caregiver in the study by Stein Duker et al. (2017) said, “We went through a couple of physicians because they didn’t really recognize autism...I probably wouldn’t have trusted their recommendations” (p. 5).
Provider Lack of Knowledge/Training
Parents and caregivers perceived that often, providers lacked knowledge and training regarding ASD. Parents felt providers were not sensitive to the challenges posed by having a child with ASD. When reflecting on lack of sensitivity, one participant said “[The nurse’s] confidence and arrogance in her training and her ability as a nurse really clouded her judgment...I think she’s probably a phenomenal nurse...but I think that unfortunately hindered her in the situation [of interacting with the child with ASD] because her confidence was so clouding” (Nicholas et al., 2016, p. 415). Caregivers also felt that providers lacked training regarding ASD. A caregiver in Stein Duker et al. (2019) experienced dentists with “no awareness of how to handle a special needs kid” (p. 4) and a caregiver in Cheak-Zamora and Teti (2015) stated, “I’m more educated on autism than my doctor” (p. 996). Finally, parents felt providers lacked knowledge regarding specific treatments for children with ASD. One participant was quoted saying: “The times I have asked about treatment, I am kind of met with a blank stare” (Levy et al., 2016, p. 574). Caregivers also noted a lack of provider understanding related to the child’s specific needs and how to best assess and relay information in a developmentally appropriate way. One parent said “I’d like someone to say to me, is there a trigger, you know a fear that’s going to make him recoil and cry or try escape...How does he respond to people putting their hands on him that he doesn’t know?” (Davignon et al., 2014, p. 211).
Caregiver Roles in Medical Care
Caregivers provided insight into the important and challenging roles they hold related to medical care of children with ASD. Some of these roles included coordinating care between providers, making appointments, managing and dispensing medication, and brushing teeth. While some roles were similar to caregivers of typically developing children, caregivers of individuals with ASD often had roles above and beyond either in duration of the role or intensity of the role. A caregiver highlighted the intensity of their role. “I had to brush his teeth for the first 9 years of his life, and every single time it was a battle” (Stein et al. 2012, p. e74). Many caregivers had to coordinate numerous medical services for their child with ASD. One father commented, “My wife is the medical home—she gets referrals and coordinates between physicians, two OTs [occupational therapists], two SLPs [speech language pathologists], teachers at school, consultant, a behavioral specialist” (Carbone et al., 2010, p. 319). A mother talked about her role in medical care even when her child was in school: “I am literally on call even when she’s at school. Even though she has an aide and there’s a nurse, they will still call me to come help take care of her on a daily basis” (Oser et al., 2020, phase 2, Table 3).
Characteristics of ASD that Make Medical Care Challenging
Caregivers noted characteristics of ASD that make medical care more challenging. This included their child’s extreme reactions to procedures, sensory overload, different expressions of pain, anxiety, and communication difficulties, and environmental and timing challenges. One caregiver explained: “He has a high pain tolerance, for some reason, sometimes pain is delayed. He can’t tell you what’s hurting, because he doesn’t sign, you have to guess pretty much, or check everything in the hospital to see what’s going on” (Benich et al., 2018, p. 39). These challenges were exacerbated when the child also had additional medical diagnoses. One caregiver of a child with ASD and type 1 diabetes said: “She doesn’t show any signs of being low [blood sugar] until she is on the brink of losing consciousness and then all of a sudden she is almost passing out” (Oser et al., 2020 phase 2, Table 3).
Barriers to Medical Care
In addition to the challenges mentioned by caregivers, specific barriers to care were also noted, which made it especially challenging for families of children with ASD to find quality care. Barriers included systemic challenges such as obtaining and coordinating care, waitlists, referrals, insurance, and finding quality providers with experience. One caregiver explained:
You don’t know what to do or how to do it? You don’t know who to talk to. The doctor referred me but did not give me an appointment. The system is too hard. I called and they told me I had to wait half a year because there are so many people. They told me I had to fill out a form in order to receive a first appointment. (Sakai et al., 2019, p. 15)
Financial barriers were also noted including the cost of medical care, socioeconomic status, and parents having to remove themselves from the workforce to care for their child. One mother said: “[I] paid privately for a psychologist, and even then, finding someone who would make the diagnosis was extremely difficult. I ended up having to beg the person who did it” (Minnes & Steiner, 2009, p. 253). Other barriers were more personal in nature, such as cultural and language barriers, traveling for appointments, and feeling overwhelmed. A mother compared going to the dentist with her child in the USA to “walking into the arms of La Migra” (immigration and customs enforcement agents) because she was worried that healthcare workers would reveal her immigration status to authorities (Floríndez et al., 2019, p. 5).
Positive Caregiver Experiences when Seeking Medical Care for Individuals with ASD
Despite the challenges caregivers noted in obtaining medical care for individuals with ASD, positive experiences were also shared. Positive experiences were most common when providers (a) adapted to the child, (b) had a flexible practice environment, and (c) had formal resources and experience.
Adapted to the Child
Caregivers indicated that positive experiences were facilitated when healthcare providers adapted to the behaviors and interests of the individual with ASD. For example, a mother stated: “When we left, we were like, ‘that doctor’s amazing.’ I think [it was] how he spoke to [the child] ... He really...met the kid where he was at” (Nicholas et al., 2020, p. 95). Another caregiver shared, “I am really pleased with the way our dentist works. The dentist started with a really, really slow routine to make him comfortable…then they said, ‘let’s look in your mouth and count your teeth’” (Lewis et al., 2015 p. e100). Another caregiver stated, “After a couple of hours...of him reading books and us playing [a game] and him playing on the video games, he was comfortable in that environment...He was allowing things to progress that needed to be done to him” (Nicholas et al., 2020, p. 96).
Flexible Practice Environment
Caregivers provided insight into the importance of flexible and modifiable medical environments surrounding individuals with ASD to improve experiences. Parents indicated that an “autism-friendly” environment would assist with counteracting the stress of the medical setting (Bultas et al., 2016; Nicholas et al., 2016; Nicholas et al., 2020). One parent stated, “having them really listened to, really looked at, focusing, that people look at the positives, and that there aren’t really limitations. It’s just figuring out a different way of doing things for them” (Russell & McCloskey, 2016, p. 25). A mother noted, “Anything with animals comforts him…and if they ever had...any kind of service animal that would totally help” (Benich et al., 2018, p. 39). Additionally, caregivers mentioned that productive interactions with providers are best when the pace of the encounter is led by the individual with ASD. For example, one mother described her daughter’s electroencephalogram (EEG) experience: “People that were putting [the leads on her head] didn’t really understand…why she was so scared. [They] just wanted to get the procedure done. Instead of restraining her, if we would have went about it a little more slowly and maybe put the TV on, it wouldn’t have been as much of an ordeal” (Davignon et al., 2014, p. 211).
Formal Resources and Experience
Additionally, caregivers indicated that the use of more formal resources, such as tool kits, videos, and child life specialists, facilitated positive medical experiences for individuals with ASD. One father emphasized the value of formal resources for providers to reference when caring for an individual with ASD, “to have at their disposal, to help them plan...and even to understand what are some of the issues for kids on the spectrum” (Muskat et al., 2015, p. 487). Additionally, caregivers suggested providers “make step by step videos like the ‘how to’ videos seen on YouTube” (Oser et al., 2020, phase 2, Table 3) to provide advanced preparation for individuals with ASD. A mother noted, “With all the technology now, it’s becoming really easy, like with the iPhone, we take a picture of the doctor, oh, we’re going to see doctor so and so…we work real hard to break down tasks for him” (Johnson et al. 2013, p. 389). Caregivers also provided insight into the use of specialized professionals to guide the medical experience for individuals with ASD and their families. One mother said: “electronic devices can occupy our kids…but now they have child life specialists that can give our kids a lot of things” (Johnson et al. 2013, p. 390).
Caregiver Suggestions for Improving Medical Care for Individuals with ASD
Caregivers provided numerous suggestions for improving medical care for individuals with ASD. These recommendations broadly fell into four categories and included (a) caregivers also need support, (b) providing adaptations and accommodations, (c) desired provider characteristics, and (d) the importance of collaboration.
Caregivers also Need Support
The first suggestion provided by caregivers was the need for caregivers to also be supported within the context of medical care for individuals with ASD. Caregivers described a desire for empathy and respect. One caregiver said, “I want them to be knowledgeable, but I also want them to be genuine and empathetic, and I want them to come more from a positive [place]” (Russell & McCloskey, 2016, p. 26), while another noted: “Dignity and respect...respecting the fact I know my child better than anyone else” (p. 25). Caregivers also expressed a desire for social support from other caregivers. “It is a matter of having more activities for our children to be together, and for us, [the parents] to be together. We can share experiences, exchange advice on how to do things, and what is available” (Sakai et al., 2019, p. 8). Caregivers also expressed a need for support to prepare individuals with ASD for medical events. One mother shared:
He tends to do best with well-practiced activities and activities that he does within the context of a structure and with people and an environment that he’s familiar with. When he doesn’t have that, when it’s not a practiced skill or he’s not given that structure, and/or he doesn’t understand what’s going on, then we will see a spike in sort of negative behavioral issues. (Johnson et al. 2013, p. 389)
To carry out their roles in medical care related to individuals with ASD, caregivers noted the importance of becoming an advocate. One caregiver said: “Don’t be afraid to articulate your wants and needs in reference to your child being different, and requiring different care” (Nicholas et al., 2016, p. 421).
Adaptations and Accommodations
Caregivers also suggested the need for adaptations and accommodations to support the medical care of individuals with ASD. This included timing considerations such as minimizing wait time, reducing the number of interactions, scheduling procedures first thing in the morning, approaching the child with patience, and limiting transitions in the environment. For example, one mother said: “Being the first appointment...we found that that’s really, really helpful in decreasing a lot of anxiety” (Johnson et al. 2013, p. 389). Another noted the difference that was made when their child was approached with patience and understanding.
He was really nervous about the gas on his face, so there was a person who helped him decorate it with stickers, and put like a scent on it, with like a Hershey ChapStick-type thing, and that really helped him a lot. (Benich et al., 2018, p. 38)
Making accommodations related to the environment was also recommended by caregivers. This included providing locations with reduced sensory input (e.g., private or quiet waiting areas, calm lighting, comfortable bedding, and loose-fitting clothes), availability of sensory or other toys, using the child’s interests to occupy their mind, and the use of electronic devices. One mother talked about how helpful “the iPad and the coloring books” were for her child (Johnson et al. 2013, p. 390). Caregivers noted avoiding changes and transitions in environments was important: “going from room to room to room, I don’t think really works …” and “autism is most obvious when he has to face change or transitions” (Muskat et al., 2015, p. 486).
Desired Provider Characteristics
Caregivers detailed numerous provider characteristics that they found beneficial. This included providers who were good communicators and listened to both parents and children, held relevant knowledge related to ASD, and were flexible in their approach with children with ASD. Related to communication, one mother stated:
Listen. I want them to listen to me. Don’t be afraid to offer advice. It is okay. I need it. Don’t worry about offending me. Honestly. Be honest with me. Don’t give me some run-around because I will know if you are just telling me what I want to hear. Be real. (Levy et al., 2016, p. 575)
-
Another noted a desire for providers
[who use] layman’s terms for the kid’s benefit. They’ve got to speak at the level that the child understands. Especially when it comes to areas [in which] they’re not going to be comfortable, like anal thermometers, needles, all the rest of that stuff that they might have to do. They’ve got to literally make it ‘Elmo speak’ for younger children. (Nicholas et al., 2016, p. 422)
Caregivers indicated providers’ knowledge about ASD should not be a one-size-fits-all approach when caring for individuals with ASD (Johnson et al. 2013; Stein Duker et al., 2019).
Importance of Collaboration
Caregivers also noted the importance of collaboration to support the medical care of individuals with ASD. Caregivers discussed the importance of collaborating with them in their child’s medical care. A caregiver highlighted the importance of collaboration with them. “Well, I suppose it’s more of ‘we’, as parents need to actually give them what works for our child...maybe it’s more, the practice is saying ‘well let us know what we can do for you – what do you think is going to work for you?’” (Thomas et al., 2018, p. 234). Partnering and collaborating with parents was seen as especially important to support children with ASD as they transitioned to adulthood and parents considered what would happen if they were no longer able to care for their child. One caregiver said: “I think how it differs is that I don’t think she [the doctor] worries about my biggest worry...what is going to happen to her if she is not able to live independently after we are gone” (Levy et al., 2016, p. 574). Caregivers also talked about the importance of collaborating with providers to coordinate services within and outside of the healthcare system. Caregivers hoped for a system that would be “seamless and work and support the families with the individual holistically” (Minnes & Steiner, 2009, p. 253). As another parent indicated:
When we take our child in for a dental visit, it feels so good to be welcomed by a team who really knows us, is prepared for us, and partners with us. This has taken years to find and shape, but I am confident has led to an easier time for staff, less stress for me, and better outcomes for my child. It is not an exaggeration to say that they are heroes to our family. (Lewis et al., 2015 p. e102)
Discussion
This meta-synthesis provided important insights into the medical experiences of caregivers and their children with ASD. Our findings point to important adjustments needed within medical systems to meet the needs of children with ASD and their caregivers. We discuss key findings, implications for practice including recommendations for adjustments in medical settings to meet the needs of children with ASD, limitations, and future research directions.
Key Findings
Several key findings were uncovered within this meta-synthesis. First, it is apparent that caregivers provide a high level of support in relation to the medical care needed for their children with ASD. Caregivers repeatedly emphasized the management, time, and level of attention that was needed to support their child’s health. Many indicated being unable to work in order to support their child’s medical needs. Second, our findings highlight the negative experiences that children with ASD face when obtaining medical care, which if left unaddressed within the field might lead to instances of pediatric medical trauma stress (PMTS) for these children (Marsac et al., 2014; Price et al., 2016). These negative experiences may be due in part to the defining characteristics of ASD that make medical care challenging (e.g., social and communication deficits, and distress when an environment is unpredictable; see Jensen et al., 2020; Morris et al., 2019; Quiban, 2020; Zwaigenbaum et al., 2016). However, the lack of child-centered care and communication with caregivers also seems to contribute to negative medical experiences and adds additional stress to caregivers and the child (Hodgetts et al., 2013). There is a need for partnership between practitioners and caregivers to improve the medical care of children with ASD. These findings are consistent with current trends in the literature, highlighting the challenges faced by these children and families, the need for increased training for medical professionals regarding working with children with ASD, and the importance of adapting the medical environment for children with ASD (Kopecky et al., 2013; Wilson & Peterson, 2018).
Implications and Recommendations
Based on the experiences of caregivers uncovered within this meta-synthesis, we provide numerous suggestions to improve medical care for individuals with ASD. First, caregivers need additional support related to their role in the medical care of children with ASD. This is especially true in cases where the child has co-occurring medical conditions (e.g., seizures, diabetes, and anxiety). This might include increased respite services with providers trained in the medical supports needed by the child, so primary caregivers are able to get a break from their demanding caretaking responsibilities (Whitmore, 2016). Second, caregivers indicated the desire for social supports from other caregivers who were experiencing similar caregiving demands for their children. Such supports are more critical for caregivers of children with extensive support needs (Lai & Oei, 2014) and have been shown to support caregiver coping as well as provide important benefits for caregivers (e.g., improved mental health; Lai & Oei, 2014; Schiller et al., 2021).
Third, caregivers stressed the importance of specific characteristics for medical providers and medical settings. Specifically related to medical providers, caregivers indicated valuing providers with good communication skills, who collaborate well with caregivers and other medical providers, are flexible and child/family-centered in their approach, and are knowledgeable about ASD. One caregiver said: “I want them to ask: ‘what is the best way to proceed with your son?’” (Lewis et al., 2015, p. E102). Caregivers also indicated a need for flexibility within the medical system such as adjustments to scheduling, adaptations specific to the child’s needs, and access to supportive services for caregivers and families (e.g., child life specialist). Such supports have been shown in the literature to improve the quality of interpersonal relationships with healthcare providers and allow caregivers to more actively engage in their child’s healthcare (Gage-Bouchard, 2017). To ensure medical providers and settings are appropriate for children with ASD, training is essential. This should include training for physicians, nurses, physician assistants, nurse practitioners, and other healthcare professionals throughout their undergraduate, graduate, and medical school/residency education journey. Training should also be continued throughout the careers of these professionals and content related to ASD should become part of the continuing education requirements within these professions. Practice and training in caring for children and individuals with ASD is complex. Therefore, training should include utilizing simulation teaching methods to provide active engagement, realistic experiences, and debriefing opportunities for medical professionals (McIntosh & Thomas, 2020). Emerging training models (e.g., ECHO autism and Autism Case Training) for medical providers should be implemented, evaluated, and improved upon to support this effort (Mazurek et al., 2017).
Limitations and Future Research Directions
Although this meta-synthesis provides important insights into the experiences of caregivers of children with ASD, several limitations should be noted as well as areas for future research. First, this meta-synthesis only explored the perspectives of caregivers of children with ASD. However, it is critical that we also understand the voices of individuals with ASD themselves (e.g., Iezzoni & Long-Bellil, 2012) and their medical providers (e.g., Warfield et al., 2015) in order to inform the best medical practices moving forward for individuals with ASD. This should include additional research and/or meta-syntheses to understand the perspectives and experiences of these stakeholders using a variety of qualitative approaches (e.g., interviews, focus groups, and observations). Additionally, the studies included in our meta-synthesis report the perspectives of caregivers who have obtained medical care for children with ASD primarily in hospital, primary care, and dental settings. We recognize that finding medical care for children with ASD can be challenging (Brewer, 2018) and as a result, note that the perspectives of caregivers represented in this meta-synthesis may not be inclusive of caregivers who were unsuccessful in obtaining medical care for their child with ASD or those who seek medical care in other settings. There is a need to explore the experiences of caregivers in medical settings not currently explored within the existing literature (e.g., psychological, psychiatric, and outpatient therapy). Next, within this meta-synthesis, we did not analyze the specific research questions of each study. Although all studies addressed the medical experiences of caregivers of children with ASD, we recognize that the research questions may have guided the ultimate findings within the studies, and thus the conclusions of this meta-synthesis. Future research should continue to explore caregiver experiences to confirm or clarify our findings.
Finally, our quality appraisal of included studies also highlighted some patterns of limitations within the existing literature. The included studies rarely provided information about participant race/ethnicity, socioeconomic, or insurance status. These characteristics of caregivers and their children with ASD may be important to consider, especially with emerging research suggesting differences in medical care for minority groups (Smith et al., 2020). Future research should include this information about participants and explore how caregiver and child characteristics might influence medical experiences. Additionally, many studies did not include information related to philosophical perspective, or positionality (i.e., cultural or theoretical perspective). We believe this may be a reflection of page limitations within journals, rather than a purposeful omission or methodological limitation. As such, we encourage journal editors to consider the importance of including this information within publications and consider page requirements in light of this finding. We also urge authors to include this information within published studies to improve transparency in research. Furthermore, ongoing research should explore other methodological approaches to seek ways to improve the medical care of individuals with ASD. This might include the use of quantitative methods to measure the outcomes from implementing recommendations outlined in this meta-synthesis (e.g., social support, training to medical providers, adjustments to the medical system to improve flexibility, child/family centeredness, and access to social and support systems for caregivers). Additionally, previous research has proposed biological-psychological-social/environmental models focusing on pediatric medical trauma stress (Marsac et al., 2014; Price et al., 2016). Medical personnel recognize that children receiving medical care may be traumatized by invasive, painful, or even frightening medical procedures (Kazak et al., 2005). Hence, research in this area should extend to include children with ASD and perspectives from their caregivers. Additionally, examining evidence-based interventions, such as play or play therapy, as a vehicle for children with ASD to process feelings and create distractions to generate positive outcomes when seeking assistance in medical settings (Locatelli, 2019; Nabors et al., 2013).
Conclusion
This study uncovered important information about caregiver experiences related to medical care for children with ASD. Given these collective experiences, and the areas outlined for improvements, there is a need for continued research and advocacy to ensure that medical systems are prepared and ready to support the needs of individuals with ASD. The innovation of new knowledge in the area of refining medical care of children with ASD lies in a multi-pronged approach by engaging diverse professionals from interdisciplinary teams to assist and tailor interventions to improve outcomes for children with ASD and their caregivers.
References
*References marked with an asterisk indicate studies included in the meta-synthesis.
Bartolomé-Villar, B., Mourelle-Martínez, M. R., Diéguez-Pérez, M., & de Nova-García, M. J. (2016). Incidence of oral health in paediatric patients with disabilities: Sensory disorders and autism spectrum disorder. Systematic review II. Journal of Clinical and Experimental. Dentistry, 8(3), e344–e351. https://doi.org/10.4317/jced.52923
*Benich, S., Thakur, S., Schubart, J. R., & Carr, M. M. (2018). Parental perception of the perioperative experience for children with autism. AORN Journal, 108(1), 34-43. https://doi.org/10.1002/aorn.12274
Brewer, A. (2018). “We were on our own”: Mothers’ experiences navigating the fragmented system of professional care for autism. Social Science & Medicine, 215, 61–68. https://doi.org/10.1016/j.socscimed.2018.08.039
*Bultas, M. W. (2012). The health care experiences of the preschool child with autism. Journal of Pediatric Nursing, 27(5), 460-470. https://doi.org/10.1016/j.pedn.2011.05.005
*Bultas, M. W., McMillin, S. E., & Zand, D. H. (2016). Reducing barriers to care in the office-based health care setting for children with autism. Journal of Pediatric Health Care, 30(1), 5-14. https://doi.org/10.1016/j.pedhc.2015.08.007
*Carbone, P. S., Behl, D. D., Azor, V., & Murphy, N. A. (2010). The medical home for children with autism spectrum disorders: Parent and pediatrician perspectives. Journal of Autism and Developmental Disorders, 40(3), 317-324. https://doi.org/10.1007/s10803-009-0874-5
*Cheak-Zamora, N. C., & Teti, M. (2015). “You think it’s hard now… It gets much harder for our children”: Youth with autism and their caregiver’s perspectives of health care transition services. Autism, 19(8), 992-1001. https://doi.org/10.1177/1362361314558279
*Davignon, M. N., Friedlaender, E., Cronholm, P. F., Paciotti, B., & Levy, S. E. (2014). Parent and provider perspectives on procedural care for children with autism spectrum disorders. Journal of Developmental & Behavioral Pediatrics, 35(3), 207-215. https://doi.org/10.1097/DBP.0000000000000036
*Ferguson, A., & Vigil, D. C. (2019). A comparison of the ASD experience of low-SES Hispanic and non Hispanic White parents. Autism Research, 12(12), 1880-1890. https://doi.org/10.1002/aur.2223
Finfgeld-Connett, D. (2010). Generalizability and transferability of meta-synthesis research findings. Journal of Advanced Nursing, 66(2), 246–254. https://doi.org/10.1111/j.1365-2648.2009.05250.x
*Floríndez, L. I., Floríndez, D. C., Floríndez, F. M., Como, D. H., Pyatak, E., Baezconde-Garbanati, L., Polido, J., & Cermak, S. A. (2019). Oral care experiences of Latino parents/caregivers with children with autism and with typically developing children. International Journal of Environmental Research and Public Health, 16(16), 2905. https://doi.org/10.3390/ijerph16162905
Gage-Bouchard, E. A. (2017). Social support, flexible resources, and health care navigation. Social Science & Medicine, 190, 111–118. https://doi.org/10.1016/j.socscimed.2017.08.015
Hodgetts, S., Nicholas, D., Zwaigenbaum, L., & McConnell, D. (2013). Parents’ and professionals’ perceptions of family-centered care for children with autism spectrum disorder across service sectors. Social Science & Medicine, 96, 138–146.
Hoon, C. (2013). Meta-synthesis of qualitative case studies: An approach to theory building. Organizational Research Methods, 16(4), 522–556. https://doi.org/10.1177/1094428113484969
Iezzoni, L. I., & Long-Bellil, L. M. (2012). Training physicians about caring for persons with disabilities: “Nothing about us without us!”. Disability and Health Journal, 5(3), 136–139. https://doi.org/10.1016/j.dhjo.2012.03.003
Jensen, E. J., Geisthardt, C., & Sarigiani, P. A. (2020). Working with children with autism spectrum disorder in a medical setting: Insights from certified child life specialists. Journal of Autism and Developmental Disorders, 50(1), 189–198. https://doi.org/10.1007/s10803-019-04245-0
*Johnson, N. L., Bekhet, A., Robinson, K., & Rodriguez, D. (2014). Attributed meanings and strategies to prevent challenging behaviors of hospitalized children with autism: Two perspectives. Journal of Pediatric Health Care, 28(5), 386-393. https://doi.org/10.1016/j.pedhc.2013.10.001
Kazak, A., Kassam-Adams, N., Schneider, S., Zelikovsky, N., Alderfer, M., & Rourke, M. (2005). An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology, 31(4), 343–355. https://doi.org/10.1093/jpepsy/jsj054
Knafl, K., & Deatrick, J. (2003). Further refinement of the family management style framework. Journal of Family Nursing, 9(3), 232–256. https://doi.org/10.1177/1074840703255435
Knafl, K., Deatrick, J., & Havill, N. (2012). Continued development of the family management style. Journal of Family Nursing, 18(1), 11–34. https://doi.org/10.1177/1074840711427294
Kopecky, K., Broder-Fingert, S., Iannuzzi, D., & Connors, S. (2013). The needs of hospitalized patients with autism spectrum disorders: A parent survey. Clinical Pediatrics, 52(7), 652–660. https://doi.org/10.1177/0009922813485974
Lai, W. W., & Oei, T. P. S. (2014). Coping in parents and caregivers of children with autism spectrum disorders (ASD): A review. Review Journal of Autism and Developmental Disorders, 1(3), 207–224. https://doi.org/10.1007/s40489-014-0021-x
*Levy, S. E., Frasso, R., Colantonio, S., Reed, H., Stein, G., Barg, F. K., Madell, D. S., & Fiks, A. G. (2016). Shared decision making and treatment decisions for young children with autism spectrum disorder. Academic pediatrics, 16(6), 571-578. https://doi.org/10.1016/j.acap.2016.04.007
*Lewis, C., Vigo, L., Novak, L., & Klein, E. J. (2015). Listening to parents: A qualitative look at the dental and oral care experiences of children with autism spectrum disorder. Pediatric Dentistry, 37(7), 98e-104e.
Liptak, G. S., Stuart, T., & Auinger, P. (2008). Health care utilization and expenditures for children with autism: Data from U.S. national samples. Journal of Autism and Developmental Disorders, 36, 871–879. https://doi.org/10.1097/DBP.0b013e318165c7a0
Liu, G., Pearl, A. M., Kong, L., Leslie, D. L., & Murray, M. J. (2017). A profile on emergency department utilization in adolescents and young adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 47(2), 347–358. https://doi.org/10.1007/s10803-016-2953-8
Locatelli, M. (2019). Play therapy treatment of pediatric medical trauma: A retrospective case study of a preschool child. International Journal of Play Therapy, 29(1), 33–42. https://doi.org/10.1037/pla0000109
Lockwood, C., Munn, Z., & Porritt, K. (2015). Qualitative research synthesis: Methodological guidance for systematic reviewers utilizing meta-aggregation. International Journal of Evidence-Based Healthcare, 13(3), 179–187. https://doi.org/10.1097/XEB.0000000000000062
Major, C. H., & Savin-Baden, M. (2010). Qualitative research synthesis. In New approaches to qualitative research: Wisdom and uncertainty. Routledge.
Marsac, M., Kassam-Adams, N., Delahanty, D., Widaman, K., & Barakat, L. (2014). Posttraumatic stress following acute medial trauma in children: A proposed model of bio-psycho-social processes during the peri-trauma period. Clinical Child and Family Psychology Review, 17, 399–411. https://doi.org/10.1007/s10567-014-0174-2
Mazurek, M. O., Brown, R., Curran, A., & Sohl, K. (2017). ECHO autism: A new model for training primary care providers in best-practice care for children with autism. Clinical Pediatrics, 56(3), 247–256. https://doi.org/10.1177/0009922816648288
McCubbin, M. A., Thompson, A., & McCubbin, H. I. (1996). Family assessment: Resiliency, coping and adaptation. University of Wisconsin-Madison.
McIntosh, C., & Thomas, C. (2020). Improving safety of patients with autism spectrum disorder through simulation. Clinical Simulation in Nursing, 45, 1–5. https://doi.org/10.1016/j.ecns.2019.11.010
*Minnes, P., & Steiner, K. (2009). Parent views on enhancing the quality of health care for their children with fragile X syndrome, autism or Down syndrome. Child: Care, Health and Development, 35(2), 250-256. https://doi.org/10.1111/j.1365-2214.2008.00931.x
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Prisma Group. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8, 336–341. https://doi.org/10.1016/j.jisu.2010.02.007
Morris, R., Greenblatt, A., & Saini, M. (2019). Healthcare providers’ experiences with autism: A scoping review. Journal of Autism and Developmental Disorders, 49, 2374–2388. https://doi.org/10.1007/s10803-019-03912-6
*Muskat, B., Burnham Riosa, P., Nicholas, D. B., Roberts, W., Stoddart, K. P., & Zwaigenbaum, L. (2015). Autism comes to the hospital: The experiences of patients with autism spectrum disorder, their parents and health-care providers at two Canadian paediatric hospitals. Autism, 19(4), 482-490. https://doi.org/10.1177/1362361314531341
*Muskat, B., Greenblatt, A., Nicholas, D. B., Ratnapalan, S., Cohen-Silver, J., Newton, A. S., Craig, W. R., & Kilmer, C., & Zwaigenbaum, L. (2016). Parent and health care provider perspectives related to disclosure of autism spectrum disorder in pediatric emergency departments. Autism, 20(8), 986-994. https://doi.org/10.1177/1362361315621520
Nabors, L., Bartz, J., Kichler, J., Sievers, R., Elkins, R., & Pangallo, J. (2013). Play as a mechanism of working through medical trauma for children with medial illnesses and their siblings. Issues in Comprehensive Pediatric Nursing, 36(3), 212–224. https://doi.org/10.3109/01460862.2013.812692
*Nicholas, D. B., Muskat, B., Zwaigenbaum, L., Greenblatt, A., Ratnapalan, S., Kilmer, C., Craig, W., Roberts, W., Cohen-Wilver, J., Newton, A., & Sharon, R. (2020). Patient-and family-centered care in the emergency department for children with autism. Pediatrics, 145(Supplement 1), S93-S98. https://doi.org/10.1542/peds.2019-1895L
*Nicholas, D. B., Zwaigenbaum, L., Muskat, B., Craig, W. R., Newton, A. S., Kilmer, C., Greenblat, A., Roberts, W., & Cohen-Silver, J. (2016). Experiences of emergency department care from the perspective of families in which a child has autism spectrum disorder. Social Work in Health Care, 55(6), 409-426. https://doi.org/10.1080/00981389.2016.1178679
*Oser, T. K., Oser, S. M., Parascando, J. A., Grisolano, L. A., Krishna, K. B., Hale, D. E., Litchman, M., Majidi, S., & Haidet, P. (2020). Challenges and successes in raising a child with type 1 diabetes and autism spectrum disorder: Mixed methods study. Journal of Medical Internet Research, 22(6), e17184. https://doi.org/10.2196/17184
Parker, M. L., & Killian, M. (2020). Autism spectrum disorder and complex healthcare needs: The role of healthcare experiences. Research in Autism Spectrum Disorders, 73(March), 101535. https://doi.org/10.1016/j.rasd.2020.101535
Price, J., Kassam-Adams, N., Alderfer, M., Christofferson, J., & Kazak, A. (2016). Systematic review: A reevaluation and update of the integrative (trajectory) model of pediatric medical traumatic stress. Journal of Pediatric Psychology, 41(1), 86–97. https://doi.org/10.1093/jpepsy/jsv074
Quiban, C. (2020). Addressing needs of hospitalized patients with autism: Partnership with parents. Critical Care Nursing Quarterly, 43(1), 68–72. https://doi.org/10.1097/CNQ.0000000000000292
*Russell, S., & McCloskey, C. R. (2016). Parent perceptions of care received by children with an autism spectrum disorder. Journal of Pediatric Nursing, 31(1), 21-31. https://doi.org/10.1016/j.pedn.2015.11.002
*Sakai, C., Mulé, C., LeClair, A., Chang, F., Sliwinski, S., Yau, Y., & Freund, K. M. (2019). Parent and provider perspectives on the diagnosis and management of autism in a Chinese immigrant population. Journal of Developmental & Behavioral Pediatrics, 40(4), 257-265. https://doi.org/10.1097/DBP.0000000000000660
Sandelowski, M., & Barroso, J. (2007). Searching for and retrieving qualitative research reports. Handbook for Synthesizing Qualitative Research, 35–74.
Schiller, V. F., Dorstyn, D. S., & Taylor, A. M. (2021). The protective role of social support sources and types against depression in caregivers: A meta-analysis. Journal of Autism and Developmental Disorders, 51, 1304–1315. https://doi.org/10.1007/s10803-020-04601-5
*Shyu, Y. I. L., Tsai, J. L., & Tsai, W. C. (2010). Explaining and selecting treatments for autism: Parental explanatory models in Taiwan. Journal of Autism and Developmental Disorders, 40(11), 1323-1331. https://doi.org/10.1007/s10803-010-0991-1
Smith, K. A., Gehricke, J. G., Iadroia, S., Wolfe, A., & Kuhlthua, K. A. (2020). Disparities in service use among children with autism: A systematic review. Pediatrics, 145(1), 35–46. https://doi.org/10.1542/peds.2019-1895G
*Stein Duker, L. I., Floríndez, L. I., Como, D. H., Tran, C. F., Henwood, B. F., Polido, J. C., & Cermak, S. A. (2019). Strategies for success: A qualitative study of caregiver and dentist approaches to improving oral care for children with autism. Pediatric Dentistry, 41(1), 4e-12e.
*Stein Duker, L. I., Henwood, B. F., Bluthenthal, R. N., Juhlin, E., Polido, J. C., & Cermak, S. A. (2017). Parents’ perceptions of dental care challenges in male children with autism spectrum disorder: An initial qualitative exploration. Research in Autism Spectrum Disorders, 39, 63-72. https://doi.org/10.1016/j.rasd.2017.03.002
*Stein, L. I., Polido, J. C., Mailloux, Z., Coleman, G. G., & Cermak, S. A. (2011). Oral care and sensory sensitivities in children with autism spectrum disorders. Special Care in Dentistry, 31(3), 102-110. https://doi.org/10.1111/j.1754-4505.2011.00187.x
*Taghizadeh, N., Heard, G., Davidson, A., Williams, K., & Story, D. (2019). The experiences of children with autism spectrum disorder, their caregivers and health care providers during day procedure: A mixed methods study. Pediatric Anesthesia, 29(9), 927-937. https://doi.org/10.1111/pan.13689
*Thomas, N., Blake, S., Morris, C., & Moles, D. R. (2018). Autism and primary care dentistry: Parents’ experiences of taking children with autism or working diagnosis of autism for dental examinations. International Journal of Paediatric Dentistry, 28(2), 226-238. https://doi.org/10.1111/ipd.12345
Volkmar, F. R., Wiesner, L. A., & Westphal, A. (2006). Healthcare issues for children on the autism spectrum. Current Opinion in Psychiatry, 19(4), 361–366. https://doi.org/10.1097/01.yco.0000228754.64743.66
Warfield, M. E., Crossman, M. K., Delahaye, J., Der Weerd, E., & Kuhlthau, K. A. (2015). Physician perspectives on providing primary medical care to adults with autism spectrum disorders (ASD). Journal of Autism and Developmental Disorders, 45(7), 2209–2217. https://doi.org/10.1007/s10803-015-2386-9
Whitmore, K. (2016). Respite care and stress among caregivers of children with autism spectrum disorder: An integrative review. Journal of Pediatric Nursing, 31, 630–652. https://doi.org/10.1016/j.pedn.2016.07.009
Wilson, S. A., & Peterson, C. C. (2018). Medical care experiences of children with autism and their parents: A scoping review. Child: Care, Health and Development, 44(6), 807–817. https://doi.org/10.1111/cch.12611
Wu, C. M., Kung, P. T., Li, C. I., & Tsai, W. C. (2015). The difference in medical utilization and associated factors between children and adolescents with and without autism spectrum disorders. Research in Developmental Disabilities, 36, 78–86. https://doi.org/10.1016/j.ridd.2014.09.019
Zwaigenbaum, L., Nicholas, D. B., Muskat, B., Kilmer, C., Newton, A. S., Craig, W. R., Ratnapalan, S., Cohen-Silver, J., Greenblatt, A., Roberts, W., & Sharon, R. (2016). Perspectives of health care providers regarding emergency department care of children and youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(5), 1725–1736. https://doi.org/10.1007/s10803-016-2703-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Douglas, S.N., Jensen, E.J. & West, P. Barriers and Benefits Experienced by Caregivers Seeking Medical Care for Their Children with Autism Spectrum Disorders: a Qualitative Meta-synthesis. Rev J Autism Dev Disord 10, 492–504 (2023). https://doi.org/10.1007/s40489-022-00306-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40489-022-00306-w