Abstract
The quantitative study assessed subjective burden, depression, and the moderating effect of social support in mothers of children with autism spectrum disorder (ASD) in India. Seventy mothers were interviewed using a structured interview schedule, which measured their subjective burden, depression, and social support from family, friends, and significant others. Data was analyzed using descriptive statistics and multiple regression analysis with interaction terms. Half of the mothers in the study reported depression of clinical significance. Higher subjective burden significantly predicted higher depression. Of the three sources of support, only medium/high family support had a direct impact on depression and also moderated the impact of the subjective burden of depression. Implications for practice and policy are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perceived social support is an integral coping resource in the caregiving stress and adaptation process (Lazarus and Folkman 1984). Research shows perceived support from informal social networks, such as family and friends, to directly impact the mental health of mothers of children with ASD, as well as buffer the impact of negative stress-appraisal on caregivers’ mental health (Benson and Karlof 2009; Benson 2006; Boyd 2002; Falk et al. 2014). However, majority evidence on the role of social support in the stress-adaptation process of caregivers of children with ASD comes from studies in the West.
We now know that an individual’s social and cultural context determines availability and use of social support (Chun et al. 2006; Uchino 2006; Kawachi and Berkman 2001). For example, Asians and Asian Americans from East and South East Asia tend to be more reluctant to disclose personal stress, like having a child with a disability, and ask for or expect support from family or friends for fear of negative social consequences, compared to European Americans (Kim et al. 2008). This pattern of help-seeking by Asians contradicts the cultural value of ‘collectivism,’ where families are primarily relied upon for support (Chun et al. 2006; Yeh et al. 2006). However, in several collectivist Asian cultures, disability in any form is highly stigmatized (Daley 2002; Dhar 2009; for review see; Ghosh and Magaña 2009). The stigma of disability possibly challenges a parent’s ability to ‘conform to social norms’—a hallmark of collectivist Asian cultures (Triandis 1994)—and impact access and availability of social support (Ghosh and Magaña 2009; Taylor et al. 2004).
Although there is an emerging body of literature on parenting stress and coping from East Asia, our knowledge of stress and adaptation of families of children with ASD from South Asia, particularly from India is limited. It is estimated that there are 2 million children with ASD between ages 2 and 9 in India (Deshmukh et al. 2013). Our understanding of the stress process, particularly the role of social support from one’s informal network, as more of stress or support, is ambiguous and based on anecdotes that are by-products of qualitative inquiries meant to explore the overall experience of parenting a child with ASD in India. Given the ambiguity and lack of knowledge, we specifically ask, “Does perceived social support buffer the impact of subjective burden on levels of depression in Indian mothers’ caring for children with ASD?”
The study is timely and important because of the following reasons. First, ASD has recently been recognized by the Indian People with Disabilities Act (1995) as a valid disability, guaranteeing individuals with ASD equal protections and rights as those with other forms of disability listed under the Act. Macro-level policy change and empirical evidence from studies such as these can help address the unmet needs and improve the quality of life of caregivers of children with ASD. The timing of the current study is, therefore, appropriate and has much to contribute to improving services for children with ASDs as well as their parents. Second, existing ASD interventions in India are heavily centered on improving child functioning (Bannerjee and Ray 2013; Gupta 2015; Lal 2010; Malhotra et al. 2010; Nair et al. 2014; Rai et al. 2015), and less so on improving caregivers wellbeing. There is a great need to develop interventions that address caregivers’ stress appraisal and mental health status. If left unaddressed, long-term exposure to stress and depression may be deleterious to both caregiver and child development outcomes (Goodman et al. 2011; Keen et al. 2010; Moore 2009; Osborne et al. 2008). Therefore, the findings from this study, based on an empirical model may aid in developing culturally appropriate and evidence-based interventions (Shu and Lung 2005) to help parents cope and better care for their child with ASD. To the best of our knowledge, this is the first study in India to quantitatively investigate the stress-buffering role of perceived social support on mothers’ depressive symptoms using a theoretical model.
Stress: Adaptation Process: Evidence from the West
The Lazarus and Folkman’s Stress, Appraisal, and Coping Model (Lazarus and Folkman 1984) model have been extensively adapted in the West to understand the stress process of caregivers of children with ASD (Dunn et al. 2001; Benson 2010). The model forms the theoretical basis for the current study. According to the model, subjective appraisal of stress, also referred to as subjective burden (Magaña et al. 2007; Pearlin et al. 1990; Zarit et al. 1980), is an individual’s evaluation of whether one’s current and future psycho-social resources are adequate to meet the demands of care (Lazarus and Folkman; Zarit et al. 1980). It is the appraisal of a situation that differentiates heterogeneity in adaptation to stressors (Pearlin et al. 1990). In general, parents of children with ASD consistently report higher levels of stress and burden compared to parents of typically developing children (Baker-Ericzen et al. 2005; Hayes and Watson 2013; Hoffman et al. 2009; Lee et al. 2009; Rao and Beidel 2009), or children who have other disabilities or impairments (Abbeduto et al. 2004; Griffith et al. 2010; Zablotsky et al. 2013; Estes et al. 2013). Parents of children with disabilities also report higher levels of mental health problems, including depression, compared to their age-matched peers who do not have children with disabilities (Abbeduto et al. 2004; Baker-Ericzen et al. 2005; Blacher and McIntyre 2006; Singer 2006; Zablotsky et al. 2013).
The importance of subjective burden has been widely demonstrated (Manning et al. 2011; McStay et al. 2014; Khanna et al. 2011; Werner and Schulman 2013), including its negative impact on an individual’s mental health (Beach et al. 2000; Gallagher et al. 2008; Phillips et al. 2009; Pinquart and Sorensen 2003).
According to Lazarus and Folkman (1984), one can modify the impact of negative subjective appraisal of stress on adaptive outcomes by strengthening an individual’s social support. Prior research shows social support to consistently predict positive mental health and adjustment in parents of children with ASD and other disabilities (Boyd 2002; Glidden and Schoolcraft 2007). Others show social support to alleviate caregivers’ depression directly (Benson and Karlof 2009; Boyd 2002; Ekas et al. 2010; Falk et al. 2014; Glidden and Schoolcraft; Weiss 2002; for review see; Stein et al. 2011). However, evidence on the stress-buffering role of social support on the relationship between subjective burden and depression (Lin et al. 2009; Manning et al. 2011; Sawyer et al. 2010) is more tenuous. Some show social support to buffer the negative impact of caregiver stress appraisal on depression, (Dunn et al. 2001) and physiological processes (Lovell et al. 2012), whereas others have found no evidence to that effect (Benson 2006). Some of this mixed evidence may be attributed to the various ways of operationalizing social support in prior research studies.
Existing research operationalizes social support in four broad ways: quantity, role, quality, and source. The quantity of social support is assessed by analyzing network density (Boyd 2002; Smith et al. 2011), and the role of support assessed via its ability to provide emotional, informational or instrumental support (Benson 2012). Researchers evaluate the quality of social support as being either positive or negative (Smith et al.), and assess its source as being, either, formal or informal (Boyd 2002), perceived or received (Benson 2012; Gill and Harris 1991). There exists an association between each of the different forms of social support measures to caregivers depression, through direct or indirect pathways (Benson 2006, 2012; Benson and Karlof 2009; Bromley et al. 2004; Ekas et al. 2010; Weiss 2002; White and Hastings 2004).
In this study, we particularly focus on two sources of support: (1) perceived social support, or the perception that one is being cared for (Turner and Marino 1994), and (2) support received from informal networks (Boyd 2002; Ekas et al. 2010). Prior research shows perceived social support and not the quantity of support (network size) (Benson 2012; Werner and Shulman 2013) to consistently predict lower depression in mothers of children with ASD (Benson 2012; Boyd 2002; Bromley et al. 2004; Ekas et al. 2010; Gill and Harris 1991). Researchers have also demonstrated that individuals whose social networks are composed primarily of kin to report greater support as well as better mental health (Antonucci and Akiyama 1987), compared to those that do not. Further, the support from informal networks is more effective in reducing stress among mothers of children with ASD than formal support (Boyd 2002; Ekas et al. 2010). Research also shows how the different sources of perceived support, such as from friends, family, and significant others, have a distinct impact on the well-being of parents of children with ASD (Boyd 2002; Mak and Kwok 2010). Given the impact of the different types of informal social supports on caregivers’ well-being, we separately investigate both the direct and buffering effects of perceived support from family, friends, and significant others, on caregivers’ depression.
As previously suggested, all of the aforementioned research has been conducted in the West with Western populations. We know that social support, its access, and utilization to maintain positive mental health (Ng 2002) are functions of an individual’s culture and social context (Kim et al. 2008; Taylor et al. 2004). It is unknown, therefore, whether the theoretical relationships that hold true in the Western context will hold true in the Asian context. The theories developed out of the studies of stress and adaptation from the West have been the basis for empirically-based interventions. It is important to generate similar evidence if we are to develop new or adapt existing interventions from the West to low- and middle-income countries to benefit caregivers of children with ASD (Divan et al. 2015).
Current Knowledge on Stress-Process in Families Caring for a Son or Daughter with ASD in India
The literature on caregivers of children with ASD in India is new and emerging. Only twenty-one studies to date have investigated their experiences, majority of which are qualitative, sans the use of any theoretical model. Findings on stress and burden, social support, and mental health are the by-products of themes that emerged from qualitative studies, meant to investigate the experiences of parents of children with ASD. For example, in the studies reviewed, only one had a specific theme, “parents’ emotions and health” (Divan et al. 2012, p. 193), wherein a respondent reportedly felt shocked, frustrated, shaken to the point of thinking about committing suicide. In the studies reviewed, caregivers reported high levels of burden and stress, a finding supported by both qualitative (John 2012; Minhas et al. 2015), and quantitative studies Kandolkar and Kenchappanavar (2014). For example, Kandolkar used the Burden Assessment Schedule (Thara et al. 1998) and found mothers of children with ASD to have higher burden scores than the control group of mothers.
Social support was a common theme to emerge across all the qualitative studies conducted in India. However, evidence of the usefulness of social support in the lives of caregivers is mixed. While some studies found the family to be a significant source of support, others show quite the contrary or provide no conclusive evidence. For example, in studies by Daley 2004; Desai et al. 2012; Divan et al. 2012; John 2012; Krishnamurthy 2008; Ravindran and Myers 2012, caregivers simultaneously perceived spouse, grandparents, siblings or other extended family members as both sources of support as well as stress. Others point to the lack of social support or understanding (Dhar 2009) or a gradual erosion of support from the once- helpful extended family (Divan et al. 2012). Lack of perceived support and negative interactions with one’s social network is of concern, as prior research from the West shows how negative interactions with family and friends decrease or undo the positive impact of perceived social support, resulting in psychological distress (Ekas et al. 2010; Pottie et al. 2009).
We specifically focus on mothers in this study, as prior research show mothers of children with ASD to report higher levels of caregiving involvement (Tehee et al. 2009), anxiety, stress, and depression of clinical significance (Davis and Carter 2008; Herring et al. 2006), compared to fathers (Falk et al. 2014; Ozturk et al. 2014). Among Asians in general, mothers of children with intellectual disabilities experience higher levels of stigma and discrimination than fathers (Ghosh and Magaña 2009). Given the complex social context in which Indian mothers provide care to children with disabilities, there is much to know about the dynamics of social support and their role in protecting maternal mental health, to help design evidence-based interventions that are socially and culturally appropriate.
Based on the review of literature, the study has the following three aims: (Aim 1) To assess the levels of subjective burden, depression, and social support among mothers of children with ASD; (Aim 2) To assess the impact of subjective burden on depression in mothers of children with ASD; and (Aim 3) To estimate the moderating effect, if any, of the three types of social support on the relationship between subjective burden and depression. For Aim 2, we hypothesized that higher subjective burden would significantly predict higher depression in mothers of children with ASD. To test for the moderating effect of social support (Aim 3), we hypothesized that as subjective burden decreases depression also decreases. However, this decrease will be greater for mothers with higher levels of social support from family, friends, or support from significant others, compared to mothers with lower social support from family, friends, or significant others.
Methods
Participants
The study included a purposive sample of 70 mothers of children with ASD recruited from non-governmental organizations, and special schools working with children with ASD from three urban areas—Delhi (including National Capital Region), Dehradun and Mumbai. Preliminary analysis found no significant difference in socio-demographic characteristics between mothers recruited from Delhi (National Capital Region), Dehradun and Mumbai. Although The Right to Education Act (2009) has made it compulsory to make special accommodation for children with disabilities in regular schools, yet Non-Governmental Organizations are preferred and continue to be the pivotal contact points for services and special education for children with disabilities in India (Kalyanpur and Gowramma 2007).
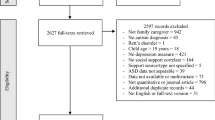
Procedure
Before approaching mothers to participate in the study, the research protocol was reviewed and approved by the Masters Research Ethics Committee of the Institute and the data collection sites. To be recruited into the study respondents had to be biological or adoptive mothers of co-residing children between ages 4 and 17 years, an age-range frequently used in academic research to investigate the experiences of parents of children with ASD (Falk et al. 2014; Giovagnoli et al. 2015; Zablotsky et al. 2013), and professionally diagnosed with ASD. Since children in India on average receive a formal diagnosis on the Pervasive Developmental Disorder (PDD) spectrum at age 4 years and 11 months (Daley 2004), we decided on a minimum cut-off age of four to qualify for the study. An upper cut-off age was set at eighteen because individuals with ASD frequently move out of the service system, hence difficult to track. It would have made recruitment difficult. For mothers who met the inclusion criteria, a date and time were set up for an interview at a place they felt convenient and safe, and in a language of their preference, i.e. Hindi or English. Before conducting the interview, all the mothers individually signed the informed consent form. Data was collected from May to October 2015. The first 70 mothers who met the inclusion criteria and gave written consent after having explained the purposes of the study were interviewed. Logistical constraints, primarily due to the nature of the hard to reach population, limited the sample size to seventy. With only eight factors and one interaction, a sample size of seventy was deemed enough to detect the effects.
Table 1 shows the demographic characteristics of the mothers and children with ASD. Mothers in the sample were in their mid-thirties. Majority mothers were not employed, and of those that did, less than half were employed full-time. The age of the children ranged between 4 and 15 years with the mean age being 8 years. Sixty-nine percent of the children were male, and thirty-one percent of the children were females. The average age of diagnosis of the child with ASD was thirty-nine months or 3 years and 3 months. Thirty-nine percent of the children had a comorbid diagnosis of ADHD along with ASD.
Measures
Along with a range of socio-demographic information, the study included three valid and reliable scales to assess subjective burden, depression and perceived social support. All the scales were translated from English to Hindi and back translated into English by reaching a consensus between two independent bilingual researchers on every item, to ensure validity. The interview schedule was pilot tested for clarity and cultural appropriateness, and necessary modifications made before the final data collection.
Subjective burden was assessed using the Zarit Burden Scale (Zarit et al. 1980). The cross-culturally valid and reliable scale has been extensively used to evaluate subjective burden or negative stress appraisal in parents of children and adolescents with developmental disabilities in the West (Gallagher et al. 2008), as well as in the context of learning disability in India (Banga and Ghosh 2016). The 30 items on this scale have responses coded as follows: 0 ‘not at all,’ 1 ‘somewhat’ and 2 ‘extremely.’ Four positively worded items are reverse coded, and the scores on all the items are summed to calculate total burden. The total scale score ranges between 0 and 60, with higher scores indicating greater subjective burden. Cronbach’s alpha was 0.86.
We used the Centre for Epidemiological Studies—Depression Scale (Radloff 1977), a widely reliable and valid to assess depression, the primary dependent variable of interest. The 20 item scale measures how often in the past week have the respondents experienced symptoms associated with depression, such as restless sleep, poor appetite or felt lonely. The response categories are, ‘rarely or none of the time,’ (0); ‘some or little of the time’ (1), ‘occasionally or moderate amount of time’ (2) and ‘most or all of the time’ (3). Four positively worded items are reverse coded. The total score ranges from 0 to 60, with higher scores indicating greater depression. A score of 16 or above identifies individuals who may be at risk of clinical depression. Scores from each statement were added to create the total score. The CES-D scale has been widely used to study caregivers from diverse backgrounds, including mothers of children with ASD in India (Seth 2011) and in the West (Taylor and Warren 2012). Scale reliability was 0.92.
Perceived Social support the moderating variable, was measured using the Multidimensional Scale of Perceived Social Support (Zimet et al. 1988). The scale has been widely used to assess the adequacy of perceived support among mothers of children with ASD in the West (Benson 2012; Khanna et al. 2011; Stuart and McGrew 2009), as well as in Asia (Mak and Kwok 2010). The 12 item scale consists of positively worded items measured on a 7 point Likert-scale, with 1 being ‘Very strongly disagree,’ 2 being ‘strongly disagree,’ 3 being ‘mildly disagree,’ 4 being ‘neutral,’ 5 being ‘mildly agree,’ 6 being ‘strongly agree’ and 7 being ‘very strongly agree.’ The 12 items assess three sources of support which are, family, friends and significant other. The three sources formed the three sub-scales, with a mean score calculated for each of the subscales (Mak and Kwok; Stuart and McGrew). The sub-scale of family enquires whether the respondent feels like the ‘family tries to help’ her; that she gets the ‘emotional help and support’ and ‘can talk about’ her problems with her family members, who are ‘willing to help’ her make decisions. The sub-scale support from friends enquired whether the mother had friends with whom she could ‘talk about’ her problems, who ‘try to help’ the mother and whether the mother ‘can count on them if things go wrong.’ The sub-scale of significant others enquired whether ‘there is a special person who is around’ to help the mother when in need, a special person with whom she could share her ‘joys and sorrows,’ or ‘who cares about her feelings’ or a ‘real source of comfort.’ The alpha reliability of the family subscale was 0.86, friends, 0.88 and significant other, 0.81.
In addition to the main study variables, other demographic variables included for analysis were the age of mother, the highest level of education she had completed, employment status, household income, and age and gender of the child.
Data Analysis
Means and standard deviations were used to assess the levels of subjective burden, depression and perceived social support among mothers of children with ASD (Aim 1). To estimate the impact of subjective burden on caregiver depression (Aim 2), we used multiple regression analysis. Prior to conducting multiple regression, we ran Pearson’s product moment correlation between the following demographic variables—age of the mothers and children, gender of the child, mothers’ years of education completed, total monthly household income as well as the multi-generational household status and the main study variables—subjective burden, depression and social support and its three subscales (support from significant other, family and friends). We selected only those variables for multiple regression analysis that correlated significantly with the primary study variables and were theoretically relevant based on prior research. Next, we analyzed the residuals of the fitted model to ensure adherence to the assumptions of regression. To ensure normality of the error distribution and to correct for heteroscedasticity, the response variable depression was transformed to its square-root. The model residuals were analyzed on all the predictor variables to test if depression exhibited a non-linear relationship with any of the predictor or control variables. Age of child exhibited a non-linear relationship with the residuals. Hence a second order term for the age of the child was added as a control variable. Other control variables were years of education completed by the mother, age, and gender of the child with ASD, and log of monthly household income.
The perceived social support measures (from family, friends and significant others) were added to the regression model, along with their interactions with subjective burden, to test the moderating effect of different types of social support on depression (Aim 3). The subjective burden measure was discretized into three levels—‘low,’ ‘medium’ and ‘high,’ by percentiles. Mothers with a score of 15 or below were in ‘low’ level, between 15 and 23 were in ‘medium’ level and those higher than 23 were in ‘high’ level of subjective burden. It was necessary to discretize subjective burden using percentiles for two reasons. First, its distribution was not symmetric, which would not have allowed using a mean +/−1 standard deviation approach. Second, the percentile approach discretized the mothers into similar sized groups. For same reasons, the three different sources of social support were each categorized into ‘low,’ ‘medium’ and ‘high’ to test if they had a moderating effect on depression. However, the average difference in depression for mothers with ‘medium’ and ‘high’ levels of support were not statistically significant. Hence, medium and high social support were merged and re-categorized into two levels—‘low’ and ‘medium/high.’ The two-step regression model included the main effects of the categorical social support and subjective burden measures in step one and the interaction terms in step two. The interaction variable was a six level factor: two levels of family support (‘low,’ ‘medium/high’) and three levels of subjective burden (‘low,’ ‘medium,’ and ‘high’). R version 3.2.4 was used for analysis of the data.
Results
The sample included 70 mothers of children with ASD. Table 1 reports results for the first aim of the study, which was to assess the levels of subjective burden, depression and social support of the mothers in the sample. Mothers reported a moderate level of subjective burden, with scores ranging between 1 and 39. The total score on the depression scale ranged between 0 and 49, with half the mothers (47.14%) having a cut-off score of 16 or above, qualifying for depression of clinical significance. Of the three forms of perceived social support, the highest support was noted from significant others, followed by support from family and then from friends.
Aim two of the study was to assess the impact of subjective burden on depression. Step 1, the correlational analysis shows (Table 2) subjective burden to be inversely correlated with the gender of the child with ASD (r = −0.24, p < 0.05), and significantly positively correlated with depression (r = 0.51, p < 0.01). Of the measures of perceived social support, support from significant other showed a negative correlation with subjective burden (r = −0.41, p < 0.01) and depression (r = −0.31, p < 0.01). Support from family was inversely correlated with subjective burden (r = −0.49, p < 0.01) and depression (r = −0.31, p < 0.01). Support from friends had no association with depression but inversely correlated with subjective burden (r = −0.25, p < 0.05).
As hypothesized in Aim 2, subjective burden was found to significantly (β = 0.118, p < 0.01) predict depression, even after controlling for the demographic variables (Table 3). Since the model was fit with a square-root transformation of the response variable, a coefficient of 0.118 for subjective burden, for example, meant that a 10 unit increase in subjective burden would result in a 1.39 (or 1.182) unit increase in depression.
Aim three of the study was to test for the moderating effect of the three forms of perceived social support on the relationship between subjective burden and depression. Table 4 shows only the direct and the moderating effect of perceived support from family, as support from friends and significant others did not exhibit any statistically significant association with depression. Step 1 of the model included the main effect of categorized subjective burden measure and family support measures, controlling for the effect of demographic factors. Results show mothers with high levels of subjective burden to report significantly higher levels of depression, compared to mothers with lower levels of subjective burden (β = 2.028, p < 0.01). There was no significant difference in depression between mothers with the medium and low levels of subjective burden. Although the main effect of perceived family support on depression was not statistically significant in step 1, the relationship became significant with the addition of interaction terms in step 2, (β = −2.151, p < 0.01), such that mothers with perceived ‘medium/high’ family support had significantly lower depression than those with ‘low’ perceived family support. Step 2 reports only the significant interaction terms between the categorical measures of stress appraisal and family support. Results show that mothers with medium level of subjective burden and medium/high family support have higher depression than mothers with low level of subjective burden and low social support (β = 2.277, p < 0.05). Similarly, mothers with high subjective burden and medium/high family support have higher depression than mothers with low subjective burden and low social support (β = 2.337, p < 0.05).
To further analyze the moderating effect of family support on depression Tukey’s HSD (Highest Significant Difference) posthoc tests were conducted (Table 5) between the six levels of the interaction term. The results showed that for mothers with low subjective burden, depression was higher for those with low family support compared to those with medium/high family support (β = 2.005, p < 0.07). However, the difference in depression was not significant for mothers with medium or high subjective burden, at low or medium/high perceived family support. Specifically, for mothers with the medium subjective burden, the difference in depression among those with low versus medium/high family support was statistically non-significant (β = 0.181, p = 0.99). Similarly, for mothers with high subjective burden, the difference in depression among those with low versus medium/high family support was statistically non-significant (β = 0.121, p = 0.999). The findings from the post hoc test support the interaction plots. The figure shows (Fig. 1) that depression decreases with declining subjective burden for mothers with medium/high family support. However, when mother perceived low family support, depression levels remain the same irrespective of the levels of stress appraisal. Figure two and three graphically shows the non-significant role of perceived support from friends and significant others to moderate the relationship between mothers level of subjective burden and depression. The interaction plots support the findings of the regression model—only family support exhibits the moderating effect of the relationship between stress appraisal and depression. Figures 2 and 3.
Discussion
Using the modified Lazarus and Folkman Stress and Coping (1984) framework, the current study investigates the stress and adaptation process in mothers of children with ASD in India. The study found subjective burden to predict depression significantly and perceived social support specifically from family to moderate the relationship between subjective burden and depression. To the best of our knowledge, the current study is the first empirical study from India to use a theoretical model and quantitatively investigate the pathway through which perceived social support moderates the relationship between subjective burden and depression in mothers of children with ASD. Using quantitative methods and a stress process model addresses potential gaps in knowledge and methodology. The study is timely and contributes to the growing body of knowledge on ASD in India, and has the potential to inform policy and intervention services to support caregivers of children with ASD in India.
The first aim of the study was to assess levels of depression, subjective burden, and perceived social support in mothers of children with ASD. Mothers in the study reported mild to moderate levels of subjective burden as opposed to previous studies that have used the Zarit scale in the context of childhood disability, such as learning disability in India (Banga and Ghosh 2016). There could be possible reasons for favorable appraisal of the caregiving situation by mothers of children with ASD. The first reason could be greater acceptance of ASD by the mothers, compared to mothers of children with a learning disability, where parents might have an ongoing expectation and hope that the child might improve academically. The second reason for favorable appraisal may be attributed to sampling characteristics. All the mothers in the study were recruited from NGOs located in urban areas. Parents of children with ASD from cities in India now have greater access to screening, diagnostic facilities, and services for their child, which implies improved knowledge and understanding of the course of the disorder. ASD is increasingly becoming a visible diagnosis. Part of it may be attributed to advocacy, policy changes, and grass-root efforts. For example, the National Trust for Autism, Cerebral Palsy, Mental Retardation, and Multiple Disabilities Act, passed by the Rehabilitation Council of India (1999), for the first time included ASD as a valid childhood developmental disability (Sect. 2 of the National Trust Act 1999). Recent legislations by the Ministry of Social Justice and Empowerment and the Union Ministry of Health and Family Welfare in April 2016 laid down clear guidelines for issuing disability certificates to individuals with ASD. It standardized the tool for the identification (Juneja et al. 2014) and assessment of severity of disability in children with ASD age six and above: an important landmark in the ASD movement. Policy changes, greater recognition, and knowledge implies greater acceptance, which may contribute to lower parenting stress and appraisal of the caregiving situation (Bitsika and Sharpley 2000). It is possible that mothers from rural or semi/peri-urban areas might have a different experience. A third possible reason for the low score on subjective burden could be ‘socially desirability’ (O’Rourke and Wenaus 1998) in response to items in the Zarit Burden Scale. As such, the mothers, in spite of being stressed were reluctant to acknowledge feeling burdened. The Zarit Scale measures “The extent to which caregivers perceive their emotional, physical health, social life, and financial status as a result of caregiving for their relative” (Zarit et al. 1986, p. 261). The original scale was designed to be self-administered. However, in this study respondents were interviewed in person. Maybe the lack of anonymity had led to response bias. Future studies may want to address these methodological challenges.
Although mothers had a low score on burden, their reported levels of depression were higher compared to findings from other studies that have used the CES-D scale in the context of caring for a child with ASD (Abbeduto et al. 2004; Smith et al. 2008; Hartley et al. 2012). Similar to Benson’s study, almost half (47.14%) of the mothers in the current sample qualified for clinically significant depression. The finding is of concern because depression is a risk factor for chronic diseases (e.g. cardiovascular diseases, osteoporosis, type 2 diabetes), through direct and indirect pathways (Kiecolt-Glaser and Glaser 2002; Lovell et al. 2012).
Of the three sources of support, mothers reported the lowest perceived support from friends, followed by families and from significant others. This finding concurs to that of Ravindran and Myers (2012), who found Indian caregivers of children with ASD to less likely list friends or support group members as sources of support compared to their Western counterparts. In a qualitative study by Divan et al. (2012), the mothers had reportedly cut off all friendships from the time the child was born, withdrew from society, or had become socially isolated or homebound, a finding also noted among Iranian parents of children with ASD (McConkey and Samadi 2013). These results are in contrast to mothers in the West, who tend to identify providers, including other parents of children with ASD, as sources of support (Mackintosh et al. 2006; Boyd 2002). There are two possible reasons why mothers tend to rate low on perceived support from friends. The first reason could be real or perceived stigma from having a child with ASD, and the second could be cultural norms, which do not support sharing worries beyond one’s immediate network. In India, disability in any form is stigmatizing and may result in ‘losing face,’ being ‘criticized,’ or ‘being disruptive to group harmony,’ or ‘bringing shame to the family.’ These norms and values are central to Asian collectivist cultural norms (Kim et al. 2008). Therefore, disclosing one’s child’s condition beyond one’s immediate family and seeking social support for the same may not be an option for these mothers. Hence dependence on family or significant others is reportedly higher.
The study found subjective burden to predict depression significantly, a finding that concurs with previous studies conducted in the West (Khanna et al. 2011; Phillips et al. 2009; Pinquart and Sorensen 2003), and lends support to the replicability of the stress-appraisal model to study the stress process of caregivers of children with ASD in India. Themes, central to the Zarit Burden Scale, such as financial distress, stigma, negative societal attributions, worry about the future of the child, or unrealistic parental expectations, when caring for the child with the disability (Brezis 2015; Daley 2004; Gupta and Singhal 2005; Minhas et al. 2015), are also common to the qualitative studies from India. However, the studies did not investigate the association of the themes to feelings of distress or depression. As such, future mixed methods studies are warranted to understand the same in greater details in the Indian context. The findings point to the need for interventions that could help mothers positively appraise the caregiving situation, so as to ensure positive mental health.
The study underscores the important role of social support in the lives of mothers of children with ASD in India. Of the three forms of social support, only perceived support from family, particularly ‘medium/high support’ had both a direct and moderating impact on the relationship between subjective burden and depression. There are two possible reasons as to why only perceived family support had a direct and moderating impact on the mental health of mothers of children with ASD. The first contributing factor could be mothers’ limited social life. Studies conducted in the West (Boyd 2002; Sanders and Morgan 1997) as well as in India (Dhar 2009; Divan et al. 2012; John 2012; Krishnamurthy 2008) point to social isolation and lack of participation in social activities by mothers of children with ASD. The limited social life has been attributed primarily to the demands of care, the behavioral challenges of the child with ASD, social stigma, fear of embarrassment, or sacrificing career and becoming homebound to care for the child with a disability (Divan et al. 2012; Krishnamurthy 2008; John 2012). Under such circumstances, it is likely that caregivers would seek support from one’s inner circle of the social network, particularly from a spouse or a relative (Bristol 1984; Divan et al. 2012), and not from friends (Bailey et al. 1999). Second, for a socially stigmatizing condition like ASD in the context of India, receiving support from the ‘family’ implies social acceptance. Perceiving support from one’s family may give these mothers a sense of ‘belonging to the in-group’ and contributing to restoring group harmony instead of burdening the family system–a collectivist cultural value (Triandis 1994). According to Triandis (1994), the impact of in-group on individuals’ social support and well-being is profound. Future mixed methods studies may want to explore in greater detail the structure, function, and quality of perceived social support networks, as well as the cultural nuances of support in mothers of children with ASD in India.
Delving deeper into family support, two findings from this study are of significance. First, results show depression to decrease with declining subjective burden for mothers with ‘medium/high’ family support, but not for a mother with ‘low’ family support. In other words, for mothers with low family support, depression levels remained the same irrespective of the levels of stress appraisal. Second, there was no significant difference in depression between mothers with ‘medium/high’ social support and ‘low’ social support when experiencing high subjective burden. The finding points to the need to address parents’ subjective stress-appraisal when designing interventions and to devise strategies to strengthen family support.
The fact that ‘medium/high’ social support from family only had a positive effect on a mother’s mental health when reporting ‘low’ levels of subjective burden and not ‘high’ levels of subjective burden have found some support from the existing literature. For example, Benson (2006) found the impact of social support on stress to be greater at low levels of the child’s ASD symptom severity, but not when the child with ASD showed high symptom severity. Similarly, a study by Hastings (2003) found high family support to predict better adjustment in siblings when the family had a child with low ASD symptom severity and not when the child had severe ASD symptoms. Extrapolating the finding in the context of the current study could imply that social support positively impacts depression only at low levels of subjective burden, but not at high levels of burden. That is, when the appraisal of a situation is very negative, perceived level of social support from family does not matter to caregivers’ psychological well-being.
The study is not without limitations. First, the study used a purposive sampling strategy, which limits the generalizability of the findings beyond the sample. In the absence of any centralized registry of children with ASD, future studies may want to select agencies/schools catering specifically to children with ASD at random, and from those select caregivers of children with ASD randomly. However, such a strategy would only include children tied to the service system in urban areas, which is also a limitation of the current study. All the mothers in the present study were selected from agencies providing services to children with ASD in urban metropolitan cities. As such, not much is known about families of children with ASD who are not tied to services and living in peri-urban and rural areas. Given that most ASD services are concentrated in cities in India, this limitation is unlikely to be resolved soon. Second, mothers of children between ages 4 and 17 were recruited. It is likely that the experiences of parents would vary by the age of the child due to different exposure to the health, education, and services system, as well as their child’s developmental challenges. Future studies may want to have a broad cross-section with sufficient respondents within each age cohort to explore how mothers’ experiences vary by the age of the child with ASD. Third, it is also possible that factors other than stress appraisal and social support may be at play which could have led to depression, which future studies could address. There is a need for a greater understanding of why mothers with high subjective burden do not benefit from high family support. Fourth concerns the measure of social support: The scale does not differentiate between mothers’ maternal versus marital family. The use of the word ‘family’ is contextual, and scales often miss out on cultural nuances or the complexity inherent in the understanding of family support, a concern raised by several respondents during data collection. Fifth, it was left up to the mothers to differentiate between support from family and that from significant others. It is possible that the same person may have been identified as a family and a significant other, e.g., for a spouse or a parent. To address the fourth and the fifth limitations, future studies on the social support may want to include social structure analysis, using Antonucci and Akiyama’s convoy model (1987) to understand mothers’ social network structures. The Sixth limitation concerns the validity of the scales. To ensure scale validity, the scales were translated and back-translated. However, the CES-D and the MSPSS scale are yet to be validated in local languages in India. Future work is needed to address these methodological challenges. Finally, the study did not include formal support as a potential source of support. It is possible that mothers may benefit from support from professionals, especially in low- and middle-income countries, where specialized services are few, and professional support is valued (McConkey and Samadi 2013). However, the limitations are offset by the fact that the study uses a theoretical model to empirically test the relationship between subjective stress-appraisal and depression and the moderating impact of perceived social support, the first one to do so in India. It opened doors to future research involving larger generalizable samples to inform policy and shape interventions and practice.
The findings from the study have the potential to inform future interventions. First, it calls for service providers to address the mental health of mothers of children with ASD in India. Half of the mothers were showing depression of clinical significance, which is of concern, given that long-term depression increases the likelihood of higher mortality and morbidity in caregivers (Kiecolt-Glaser and Glaser 2002; Lovell et al. 2012). Second, since the study found subjective burden to predict depression significantly, interventions should be targeted at improving a mother’s appraisal of the caregiving situation. Activities would involve psychoeducation, providing training and information on ASD, and streamlining the monitoring of developmental milestones to refer children to developmental pediatricians or early intervention services subsequently. Research shows that mothers of children with ASD, when involved in psychoeducational programs, report a decrease in depression (Bristol et al. 1993; McConachie and Diggle 2007). Most of the intervention studies in India tend to focus on child outcomes. Measurable parent outcomes are a rarity, although anecdotally results suggest the importance of psychoeducation on improving parents’ perception of the caregiving situation. In an intervention study on parents of children with ASD in India, Brezis et al. (2015) found parents less likely to compare their child with ASD to normal children, and to report greater acceptance and understanding of the child’s condition and behavior following the intervention. Although the intervention did not measure depression or burden pre and post activities, it is likely that such interventions may prove effective to improve caregivers’ subjective appraisal, which might ultimately impact their mental health. Practitioners in India may want to use a stress adaptation framework to design interventions that address both child and parent outcomes.
Because of the direct and moderating impact of family support on depression, family-based therapies and interventions are necessary. Interventions and therapies would improve communication, assist in better understanding of symptoms, greater acceptance of the child, and strengthen the support system, which would ultimately help in reducing stress (Kale and Landreth 1999), subjective burden, and the depression in mothers of children with ASD. Strategies could include training of the siblings and the spouse, as well as grandparents of children with ASD living in multi-generational households.
In conclusion, the study found subjective burden to predict depression in mothers of children with ASD significantly, and perceived social support, particularly from family, to moderate the relationship between stress appraisal and depression. The study calls for focusing on subjective stress appraisal and mental health of mothers of children with ASD and strengthening their support network.
References
Abbeduto, L., Seltzer, M. M., Shattuck, P., Krauss, M. W., Osmond, G., & Murphy, M. M. (2004). Psychological well-being and coping in mothers of youths with autism, Down syndrome, or Fragile X Syndrome. American Journal on Mental Retardation, 109(3), 237–254.
Antonucci, T. C., & Akiyama, H. (1987). Social networks in adult life and a preliminary examination of the convoy model. Journal of Gerontology, 42(5), 519–527.
Bailey, Jr, D. B., Skinner, D., Correa, V., Arcia, E., Reyes-Blanes, M. E., Rodriguez, P., et al. (1999). Needs and supports reported by Latino families of young children with developmental disabilities. American Journal on Mental Retardation, 104(5), 437–451.
Baker-Ericzen, M. J., Brookman-Frazee, L., & Stahmer, A. (2005). Stress levels and adaptability in parents of toddlers with and without ASDs. Research and Practice for Persons with Severe Disabilities, 30(4), 194–204.
Banerjee, M., & Ray, S. G. (2013). Development of Play Therapy Module for Children with Autism. Journal of the Indian Academy of Applied Psychology, 39(2), 245–253.
Banga, G., & Ghosh, S. (2016). The impact of affiliate stigma on the psychological well-being of mothers of children with learning disabilities in India: The mediating role of subjective burden. Journal of Applied Research in Intellectual Disabilities. DOI:10.1111/jar.12311.
Beach, S. R., Schulz, R., Yee, J. L., & Jackson, S. (2000). Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging, 15, 259–271.
Benson, P. (2012). Network characteristics, perceived social support, and psychological adjustment in mothers of children with social support. Journal for Autism and Developmental Disorders, 42(12), 2597–2610.
Benson, P. R. (2006). The impact of child symptom severity on depressed mood among parents of children with ASD: The mediating role of stress proliferation. Journal of Autism and Developmental Disorders, 36(5), 685–695.
Benson, P. R. (2010). Coping, distress, and well-being in mothers of children with autism. Research in Autism Spectrum Disorders, 4(2), 217–228.
Benson, P. R., & Karlof, K. L. (2009). Anger, stress proliferation, and depressed mood among parents of children with ASD: A longitudinal replication. Journal of Autism and Developmental Disorders, 39(2), 350–362.
Bitsika, V., & Sharpley, C. (2000). Development and testing of the effects of support groups on the well-being of parents of children with autism-II: Specific stress management techniques. Journal of Applied Health Behaviour, 2(1), 8–15.
Blacher, J., & McIntyre, L. L. (2006). Syndrome specificity and behavioural disorders in young adults with intellectual disability: Cultural differences in family impact. Journal of Intellectual Disability Research, 50(3), 184–198.
Boyd, B. A. (2002). Examining the relationship between stress and lack of social support in mothers of children with autism. Focus on Autism and Other Developmental Disabilities, 17(4), 208–215.
Brezis, R. S., Weisner, T. S., Daley, T. C., Singhal, N., Barua, M., & Chollera, S. P. (2015). Parenting a child with Autism in India: Narratives before and after a parent–child intervention program. Culture, Medicine, and Psychiatry, 39(2), 277–298.
Bristol, M. M. (1984). Family resources and successful adaptation to autistic children. In E. Schopler & G. B. Mesibov (Eds.), The Effects of Autism on the Family. Current Issues in Autism (pp. 289–310). Boston, MA: Springer.
Bristol, M. M., Gallagher, J. J., & Holt, K. D. (1993). Maternal depression in autism: Response to psychoeducational intervention. Rehabilitation Psychology, 38(1), 3–10.
Bromley, J., Hare, D. J., Davison, K., & Emerson, E. (2004). Mothers supporting children with autistic spectrum disorders: Social support, mental health status and satisfaction with services. Autism: The International Journal of Research and Practice, 8(4), 409–423.
Chun, C. A., Moos, R. H., & Cronkite, R. C. (2006). Culture: A fundamental context for the stress and coping paradigm. In P. T. Wong & L. C. Wong (Eds.), Handbook of Multicultural Perspectives on Stress and Coping (pp. 29–53). Berlin: Springer.
Daley, T. (2004). From symptom recognition to diagnosis: Children with autism in urban India. Social Science and Medicine, 58(7), 1323–1335.
Davis, N. O., & Carter, A. S. (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders, 38(7), 1278–1291.
Desai, M. U., Divan, G., Wertz, F. J., & Patel, V. (2012). The discovery of Autism: Indian parents’ experiences of caring for their child with an ASD. Transcultural Psychiatry, 49(3–4), 613–637.
Deshmukh, V.B., Mohapatra, A., Gulati, S., Nair, M.K.C., Bhutani, V.K., Silberg, D.H., et al. (2013). Program booklet. West Hartford: IMFAR; Prevalence of neuro-developmental disorders in India: poster presentation.
Dhar, R. (2009). Living with a developmentally disabled child: Attitude of family members in India. The Social Science Journal, 46(4), 738–755.
Divan, G., Hamdani, S. U., Vajartkar, V., Minhas, A., Taylor, C., Aldred, C., … & Patel, V. (2015). Adapting an evidence-based intervention for autism spectrum disorder for scaling up in resource-constrained settings: the development of the PASS intervention in South Asia. Global Health Action, 8.
Divan, G., Vajaratkar, V., Desai, M. U., Strik-Lievers, L., & Patel, V. (2012). Challenges, coping strategies, and unmet needs of families with a child with autism spectrum disorder in Goa, India. Autism Research, 5(3), 190–200.
Dunn, M. E., Burbine, T., Bowers, C. A., & Tantleff-Dunn, S. (2001). Moderators of stress in parents of children with Autism. Community Mental Health Journal, 37(1), 39–52.
Ekas, N. V., Lickenbrock, D. M., & Whitman, T. L. (2010). Optimism, social support, and well-being in mothers of children with ASD. Journal of Autism and Developmental Disorders, 40(10), 1274–1284.
Estes, A., Olson, E., Sullivan, K., Greenson, J., Winter, J., Dawson, G., & Munson, J. (2013). Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain and Development, 35(2), 133–138.
Falk, N. H., Norris, K., & Quinn, M. G. (2014). The factors predicting stress, anxiety and depression in the parents of children with autism. Journal of Autism and Developmental Disorders, 44(12), 3185–3203.
Gallagher, S., Phillips, A. C., Oliver, C., & Carroll, D. (2008). Predictors of psychological morbidity in parents of children with intellectual disabilities. Journal of Pediatric Psychology, 33(10), 1129–1136.
Ghosh, S., & Magaña, S. (2009). A rich mosaic: Emerging research on Asian families of persons with intellectual and developmental disabilities. International Review of Research in Mental Retardation, 37, 179–212.
Gill, M. J., & Harris, S. L. (1991). Hardiness and social support as predictors of psychological discomfort in mothers of children with Autism. Journal of Autism and Developmental Disorders, 21(4), 407–416.
Giovagnoli, G., Postorino, V., Fatta, L. M., Sanges, V., De Peppo, L., Vassena, L., … & Mazzone, L (2015). Behavioral and emotional profile and parental stress in preschool children with autism spectrum disorder. Research in Developmental Disabilities, 45, 411–421.
Glidden, L. M., & Schoolcraft, S. A. (2007). Family assessment and social support. In J. W. Jacobson, J. A. Mulick & J. Rojahn (Eds.), Handbook of intellectual and developmental disabilities (pp. 391–422). New York: Springer.
Goodman, S. H., Rouse, M. H., Connell, A. M., Broth, M. R., Hall, C. M., & Heyward, D. (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27.
Griffith, G. M., Hastings, R. P., Nash, S., & Hill, C. (2010). Using matched groups to explore child behavior problems and maternal well-being in children with Down syndrome and autism. Journal of Autism and Developmental Disorders, 40, 610–619.
Gupta, A., & Singhal, N. (2005). Psychosocial support for families of children with autism. Asia Pacific Disability Rehabilitation Journal, 16(2), 62–83.
Gupta, B. (2015). Theory of mind in autism: A case study. Psychological Studies, 60(3), 339–345.
Hartley, S. L., Seltzer, M. M., Head, L., & Abbeduto, L. (2012). Psychological well-being in fathers of adolescents and young adults with Down Syndrome, Fragile X Syndrome, and Autism. Family Relations, 61(2), 327–342.
Hastings, R. P. (2003). Child behaviour problems and partner mental health as correlates of stress in mothers and fathers of children with autism. Journal of Intellectual Disability Research, 47(4–5), 231–237.
Hayes, S. A., & Watson, S. L. (2013). The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(3), 629–642.
Herring, S., Gray, K., Taffe, J., Tonge, B., Sweeney, D., & Einfeld, S. (2006). Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. Journal of Intellectual Disability Research, 50(12), 874–882.
Hoffman, C. D., Sweeney, D. P., Hodge, D., Lopez-Wagner, M. C., & Looney, L. (2009). Parenting stress and closeness: Mothers of typically developing children and mothers of children with autism. Focus on Autism and Other Developmental Disabilities, 24(3), 178–787.
John, A. (2012). Stress among mothers of children with intellectual disabilities in urban India: role of gender and maternal coping. Journal of Applied Research in Intellectual Disabilities, 25(4), 372–382.
Juneja, M., Mishra, D., Russell, P. S. S., Gulati, S., Deshmukh, V., Tudu, P., ... & Arora, N. K. (2014). INCLEN diagnostic tool for Autism Spectrum Disorder (INDT-ASD): Development and validation. Indian Pediatrics, 51(5), 359–365.
Kale, A. L., & Landreth, G. L. (1999). Filial therapy with parents of children experiencing learning difficulties. International Journal of Play Therapy, 8(2), 35–56.
Kalyanpur, M., & Gowramma, I. P. (2007). Cultural barriers to South Indian families’ access to services and educational goals for their children with disabilities. Journal of the International Association of Special Education, 8(1), 69–82.
Kandolkar, A. C., & Kenchappanavar, R. N. (2014). Burden of care and parent-child relationship of parents of autistic children. Journal of Psychosocial Research, 9(2), 309–317.
Kawachi, I., & Berkman, L. F. (2001). Social ties and mental health. Journal of Urban Health, 78(3), 458–467.
Keen, D., Couzens, D., Muspratt, S., & Rodger, S. (2010). The effects of a parent-focused intervention for children with a recent diagnosis of autism spectrum disorder on parenting stress and competence. Research in Autism Spectrum Disorders, 4(2), 229–241.
Khanna, R., Madhavan, S. S., Smith, M. J., Patrick, J. H., Tworek, C., & Becker-Cottrill, B. (2011). Assessment of health-related quality of life among primary caregivers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 41(9), 1214–1227.
Kiecolt-Glaser, J. K., & Glaser, R. (2002). Depression and immune function: central pathways to morbidity and mortality. Journal of Psychosomatic Research, 53(4), 873–876.
Kim, H. S., Sherman, D. K., & Taylor, S. E. (2008). Culture and social support. American Psychologist, 63(6), 518–526.
Krishnamurthy, V. (2008). A clinical experience of autism in India. Journal of Developmental and Behavioral Pediatrics, 29(4), 331–333.
Lal, R. (2010). Effect of alternative and augmentative communication on language and social behavior of children with autism. Educational Research and Reviews, 5(3), 119–125.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer.
Lee, G. K., Lopata, C., Volker, M. A., Thomeer, M. L., Nida, R. E., Toomey, J. A., et al. (2009). Health-related quality of life of parents of children with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 24(4), 227–239.
Lin, J. D., Hu, J., Yen, C. F., Hsu, S. W., Lin, L. P., Loh, C. H., … & Wu, J. L (2009). Quality of life in caregivers of children and adolescents with intellectual disabilities: use of WHOQOL-BREF survey. Research in Developmental Disabilities, 30(6), 1448–1458.
Lovell, B., Moss, M., & Wetherell, M. A. (2012). With a little help from my friends: Psychological, endocrine and health corollaries of social support in parental caregivers of children with autism or ADHD. Research in Developmental Disabilities, 33(2), 682–687.
Mackintosh, V. H., Goin-Kochel, R. P., & Myers, B. J. (2006). Sources of information and support used by parents of children with autism spectrum disorders. Journal on Developmental Disabilities, 12(1), 41–51.
Magaña, S. M., García, J. I. R., Hernández, M. G., & Cortez, R. (2007). Psychological distress among Latino family caregivers of adults with schizophrenia: The roles of burden and stigma. Psychiatric Services, 58(3), 378–384.
Mak, W. W., & Kwok, Y. T. (2010). Internalization of stigma for parents of children with autism spectrum disorder in Hong Kong. Social Science & Medicine, 70(12), 2045–2051.
Malhotra, S., Rajender, G., Bhatia, M. S., & Singh, T. B. (2010). Effects of picture exchange communication system on communication and behavioral anomalies in autism. Indian Journal of Psychological Medicine, 32(2), 141–143.
Manning, M. M., Wainwright, L., & Bennett, J. (2011). The double ABCX model of adaptation in racially diverse families with a school-age child with autism. Journal of Autism and Developmental Disorders, 41, 320–331.
McConachie, H., & Diggle, T. (2007). Parent implemented early intervention for young children with autism spectrum disorder: A systematic review. Journal of Evaluation in Clinical Practice, 13(1), 120–129.
McConkey, R., & Samadi, S. A. (2013). The impact of mutual support on Iranian parents of children with an autism spectrum disorder: a longitudinal study. Disability and Rehabilitation, 35(9), 775–784.
McStay, R. L., Trembath, D., & Dissanayake, C. (2014). Stress and family quality of life in parents of children with autism spectrum disorder: parent gender and the double ABCX model. Journal of Autism and Developmental Disorders, 44(12), 3101–3118.
Minhas, A., Vajaratkar, V., Divan, G., Hamdani, S. U., Leadbitter, K., Taylor, C., … & Green, J (2015). Parents’ perspectives on care of children with autistic spectrum disorder in South Asia–Views from Pakistan and India. International Review of Psychiatry, 27(3), 247–256.
Moore, T. R. (2009). Adherence to behavioral and medical treatment recommendations by parents of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(8), 1173–1184.
Nair, M. K. C., Russell, P. S. S., George, B., Prasanna, G. L., Bhaskaran, D., Leena, M. L., … & Mammen, P (2014). CDC Kerala 9: Effectiveness of low intensity home based early intervention for Autism Spectrum Disorder in India. The Indian Journal of Pediatrics, 81(2), 115–119.
Ng, S. H. (2002). Will families support their elders? Answers from across cultures. In T. D. Nelson (Ed.), Ageism: Stereotyping and prejudice against older persons (pp. 295–309). Cambridge, MA: MIT Press.
O’Rourke, N., & Wenaus, C. A. (1998). Marital aggrandizement as a mediator of burden among spouses of suspected dementia patients. Canadian Journal on Aging, 17(04), 384–400.
Osborne, L. A., McHugh, L., Saunders, J., & Reed, P. (2008). Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders, 38(6), 1092–1103.
Ozturk, Y., Riccadonna, S., & Venuti, P. (2014). Parenting dimensions in mothers and fathers of children with Autism Spectrum Disorders. Research in Autism Spectrum Disorders, 8(10), 1295–1306.
Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594.
Phillips, A. C., Gallagher, S., Hunt, K., Der, G., & Carroll, D. (2009). Symptoms of depression in non-routine caregivers: The role of caregiver strain and burden. British Journal of Clinical Psychology, 48(4), 335–346.
Pinquart, M., & Sorensen, S. (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. Journal of Gerontology: Series B Psychological Sciences and Social Sciences, 58, 112–128.
Pottie, C. G., Cohen, J., & Ingram, K. M. (2009). Parenting a child with autism: Contextual factors associated with enhanced daily parental mood. Journal of Pediatric Psychology, 34(4), 419–429.
Radloff, L. S. (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Rai, S., Nizamie, S. H., & Nizamie, A. (2015). Social story in improving problem behavior in moderate autism-A case study. Journal of Indian Association for Child & Adolescent Mental Health, 11(3), 246–255.
Rao, P. A., & Beidel, D. C. (2009). The impact of children with high functioning autism on parental stress, sibling adjustment, and family functioning. Behavior Modification, 33(4), 437–451.
Ravindran, N., & Myers, B. J. (2012). Cultural influences on perceptions of health, illness, and disability: A review and focus on autism. Journal of Child and Family Studies, 21(2), 311–319.
Sanders, J. L., & Morgan, S. B. (1997). Family stress and adjustment as perceived by parents of children with autism or Down syndrome: Implications for intervention. Child & Family Behavior Therapy, 19(4), 15–32.
Sawyer, M. G., Bittman, M., La Greca, A. M., Crettenden, A. D., Harchak, T. F., & Martin, J. (2010). Time demands of caring for children with autism: What are the implications for maternal mental health? Journal of Autism and Developmental Disorders, 40(5), 620–628.
Seth, S. B. (2011). Autism: The impact on caregivers. Journal of Psychosocial Research, 6(1), 149–156.
Shu, B. C., & Lung, F. W. (2005). The effect of support group on the mental health and quality of life for mothers with autistic children. Journal of Intellectual Disability Research, 49(1), 47–53.
Singer, G. H. S. (2006). Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. American Journal of Mental Retardation, 111(3), 155–169.
Smith, L. E., Greenberg, J. S., & Seltzer, M. M. (2011). Social support and well-being at mid-life among mothers of adolescents and adults with ASD. Journal of Autism and Developmental Disorders, 42(9), 1818–1826.
Smith, L. E., Seltzer, M. M., Tager-Flusberg, H., Greenberg, J. S., & Carter, A. S. (2008). A comparative analysis of well-being and coping among mothers of toddlers and mothers of adolescents with ASD. Journal of Autism and Developmental Disorders, 38(5), 876–889.
Stein, L. I., Foran, A. C., & Cermak, S. (2011). Occupational patterns of parents of children with autism spectrum disorder: Revisiting Matuska and Christiansen’s model of lifestyle balance. Journal of Occupational Science, 18(2), 115–130.
Stuart, M., & McGrew, J. H. (2009). Caregiver burden after receiving a diagnosis of an autism spectrum disorder. Research in Autism Spectrum Disorders, 3(1), 86–97.
Thara, R., Padmavati, R., Kumar, S. & Srinivasan, L. (1998). Burden Assessment Schedule Instrument to assess burden on caregivers of chronic mentally ill. Indian Journal of Psychiatry, 40(1), 21–29.
Taylor, J. L., & Warren, Z. E. (2012). Maternal depressive symptoms following autism spectrum diagnosis. Journal of Autism and Developmental Disorders, 42(7), 1411–1418.
Taylor, S. E., Sherman, D. K., Kim, H. S., Jarcho, J., Takagi, K., & Dunagan, M. S. (2004). Culture and social support: Who seeks it and why? Journal of Personality and Social Psychology, 87(3), 354.
Tehee, E., Honan, R., & Hevey, D. (2009). Factors contributing to stress in parents of individuals with autistic spectrum disorders. Journal of Applied Research in Intellectual Disabilities, 22(1), 34–42.
Triandis, H. C. (1994). Culture and Social Behavior. New York: McGraw-Hill.
Turner, R. J., & Marino, F. (1994). Social support and social structure: A descriptive epidemiology. Journal of Health and Social Behavior, 35(3), 193–212.
Uchino, B. N. (2006). Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29(4), 377–387.
Weiss, M. L. (2002). Hardiness and social support as predictors of stress in mothers of typical children, children with autism, and children with mental retardation. Autism: The international journal of research and practice, 6(1), 115–130.
Werner, S., & Shulman, C. (2013). Subjective well-being among family caregivers of individuals with developmental disabilities: The role of affiliate stigma and psychosocial moderating variables. Research in Developmental Disabilities, 34(11), 4103–4114.
White, N., & Hastings, R. P. (2004). Social and professional support for parents of adolescents with severe intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 17(3), 181–190.
Yeh, C. J., Arora, A. K., & Wu, K. A. (2006). A new theoretical model of collectivistic coping. In P. T. Wong & L. C. Wong (Eds.), Handbook of Multicultural Perspectives on Stress and Coping (pp. 55–72). Berlin: Springer.
Zablotsky, B., Bradshaw, C. P., & Stuart, E. A. (2013). The association between mental health, stress, and coping supports in mothers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(6), 1380–1393.
Zarit, S. H., Reever, K. E., & Bach-Peterson, J. (1980). Relatives of the impaired elderly: correlates of feelings of burden. The Gerontologist, 20(6), 649–655.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41.
Funding
The study has not received any funding.
Author information
Authors and Affiliations
Contributions
PS conceived the study, collected, entered and cleaned the data and helped with writing the manuscript. SG co-conceived the study, interpreted the results and drafted the manuscript. SN performed the statistical analysis, interpreted the results and drew the figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Singh, P., Ghosh, S. & Nandi, S. Subjective Burden and Depression in Mothers of Children with Autism Spectrum Disorder in India: Moderating Effect of Social Support. J Autism Dev Disord 47, 3097–3111 (2017). https://doi.org/10.1007/s10803-017-3233-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-017-3233-y