Abstract
This study examined the characteristics of the support networks of 106 mothers of children with ASD and their relationship to perceived social support, depressed mood, and subjective well-being. Using structural equation modeling, two competing sets of hypotheses were assessed: (1) that network characteristics would impact psychological adjustment directly, and (2) that network effects on adjustment would be indirect, mediated by perceived social support. Results primarily lent support to the latter hypotheses, with measures of network structure (network size) and function (proportion of network members providing emotional support) predicting increased levels of perceived social support which, in turn, predicted decreased depressed mood and increased well-being. Results also indicated that increased interpersonal strain in the maternal network was directly and indirectly associated with increased maternal depression, while being indirectly linked to reduced well-being. Study limitations and implications are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Research indicates that mothers of children with disabilities are at greater risk for mental health problems than are mothers of typically developing children (Singer 2006), with mothers of children with autism spectrum disorder (ASD) generally reporting higher levels of distress than mothers of children with other disabilities (Abbeduto et al. 2004; Blacher and McIntyre 2006; Olsson and Hwang 2001). However, it is also well established that mothers of children with ASD evidence wide variability in mental health outcomes, a fact that has encouraged research aimed at identifying possible risk and protective factors associated with maternal psychological adjustment, including child behavior problems, family socioeconomic resources, and parental psychological characteristics such as self efficacy, optimism, and coping style (Benson 2010; Ekas et al. 2010; Emerson 2003; Hastings and Brown 2002).
Among the various protective factors studied by investigators, social support has been consistently identified as one of the most powerful predictors of psychological adjustment among parents raising children with ASD and other disabilities (for reviews, see Beresford 1994; Boyd 2002; Glidden and Schoolcraft 2007). In particular, maternal perceptions of the availability and quality of social support, especially as provided by close family and friends, has repeatedly been linked to reduced distress among mothers of children with ASD. For example, in one study of mothers of children with autism, Weiss (2002) found maternal perceptions of received social support to be significantly related to both increased self-efficacy and decreased depressed mood, while in a second, more recent study, Ekas et al. (2010) found maternal perceived support to be directly and indirectly linked to maternal distress and well-being. These and similar findings (e.g., Benson 2006; Benson and Karlof 2009; Bromley et al. 2006; White and Hastings 2004) are consistent with nearly four decades of research demonstrating the beneficial effects of social support on emotional and physical health (for reviews, see Antonucci 2001; Thoits 1995; Turner and Brown 2010).
Given that social networks serve as the conduit through which social support flows, it is surprising that so little research to date has examined the social networks of parents of children with ASD. Indeed based on our review of the literature, we could find only one study to do so. In that study, Smith et al. (2011) found both quantity of support (number of social network members) and valence of support (positive and negative support) to be associated with improvements in maternal mental health outcomes over an 18-month period. No overall description of support network characteristics was provided in that study, which focused on mothers of adolescent and adult children with ASD.
In the present study, we describe the characteristics of social networks utilized by mothers of children with ASD for purposes of social support (i.e., their “support networks”) and examine the impact of network characteristics on perceived social support, depressed mood, and subjective well-being. Before detailing the current study, however, we turn to a brief review of the theoretical and research literatures linking social networks to social support and mental health, a body of work emanating largely from outside the disability field.
Network Characteristics, Social Support, and Psychological Adjustment
While the two concepts are related, it is important to separate social networks and social support, both analytically and empirically, and treat them as distinct phenomena. Social networks are the interpersonal environments that are constituted by individuals and their social relationships, while social support consists of the material, instrumental, and socio-emotional resources transferred within these interpersonal environments (Haines et al. 2002, 2008; Hartwell and Benson 2007).
But how do social networks and social support interrelate to influence mental health? The convoy model of social relations (Antonucci 2001) offers a useful theoretical framework for understanding this relationship. According to this model, convoys constitute ‘…an assembly of family, friends (and others) who surround the individual and are available as resources in times of need’ (Ajrouch et al. 2005: S311). As such, convoys provide individuals with a protective base that is both dynamic and stable over time and include both objective (e.g., network structure, composition, function) and subjective elements (i.e., perceptions of relational quality and supportiveness). According to the convoy model, the structure, composition, function, and perceived quality of individuals’ social relationships interact to jointly impact mental health outcomes, including depression and well-being.
Over the past several decades, the central tenets of the convoy model have been empirically validated as researchers have identified specific network characteristics that influence the social support received by individuals, their perceptions of the availability and adequacy of that support, and their mental health. Characteristics of network structure such as network size and density (i.e., the extent to which network members are closely interconnected), for example, have been found to be positively related to perceived social support and to favorable mental health outcomes (Seeman and Berkman 1988; Beggs et al. 1996; Haines et al. 2008; Wellman and Wortley 1990). Research also suggests that network composition matters, with individuals embedded in networks with a higher percentage of kin (i.e., parents, children, and siblings), females, and experientially similar others generally reporting higher levels of support and well-being compared to those in networks with a lower percentage of members with these characteristics (Antonucci and Akiyama 1987; Peek and Lin 1999; Suitor and Pillemer 2002; Wellman and Frank 2001). Network availability has also been found to be associated with increased social support and reduced psychological distress (Marsden and Campbell 1984; Wellman et al. 2003), though some studies suggest that it is primarily the availability of strong intimate ties, not ties in general, that fosters high levels of perceived support and positive adjustment (Brown and Harris 1978; Kessler and McLeod 1984),
Although research has clearly demonstrated the important role played by social networks in enhancing mental health, questions still remain regarding the mechanisms through which networks exert their influence. While some researchers posit that network characteristics affect psychological adjustment directly by increasing social participation and engagement (Pescosolido and Georgianna 1989), others suggest that the impact of social networks on adjustment is primarily indirect, mediated by intervening psychosocial resources such as self-esteem, mastery, and perceived social support (Berkman et al. 2000; Lin and Peek 1999; Thoits 2011). In this latter instance, network characteristics are hypothesized to increase psychological resources, such as perceived support, which, in turn, increases psychological adjustment (e.g., decreased depression, increased subjective well-being). While evidence for this indirect effect has been found in a number of studies (Chan and Lee 2006; Fiori et al. 2006; Haines et al. 2008; Tausig 1992), it has yet to be examined in research involving parents of children with ASD.
Finally, it is important to note that social ties can have negative as well as positive effects on mental health, with research indicating that negative social interaction, particularly involving close family and friends, decreases perceived support and increases psychological distress (for reviews, see Burg and Seeman 1994; Lincoln 2000; Rook et al. 2003). Evidence of the psychologically damaging effects of negative interactions has been observed in both longitudinal and cross-sectional studies across a wide array of social settings, including families of children with ASD and other disabilities. In recent study of parents of children with ASD using daily diary methods, for example, Pottie et al. (2009) found parents who experienced more negative interactions experienced higher levels of negative mood and lower levels of positive mood (see also Ekas et al. 2010; Smith et al. 2011). Existing research thus indicates that network ties can affect psychological adjustment in a variety of direct and indirect ways, for example, by increasing perceived social support and favorable mental health outcomes as well as by heightening interpersonal strain, reducing perceived support, and increasing distress.
The Present Study
In the present study we systematically examine the characteristics of the support networks of mothers of children with ASD in middle childhood and relate those characteristics to maternal social support and mental health. In our analyses, we focused attention on characteristics associated with network structure, composition, and availability found to be related to perceived social support and psychological adjustment in prior studies. In addition, we also examined the functional aspects of maternal support networks, specifically the proportion of network members engaged in supportive and strain-induced interactions with mothers in our sample.
Based on our review of the literature, several hypotheses regarding the impact of maternal network characteristics on perceived social support and psychological adjustment were posited. Specifically, in regard to network structure, we hypothesized that network size and density would be directly related to increased perceived support. In terms of network composition, we expected that increased support would be directly related to mothers being embedded in networks with a higher proportion of kin and females, as well as in networks with higher numbers of “experientially similar others” (i.e., other parents of children with ASD). Similarly, we expected increased perceived support would be directly linked to increased network availability (proximity and frequency of contact). Lastly, in regard to network function, we hypothesized that increased perceived support would be directly linked to maternal involvement in networks where a higher proportion of members were reported as providing instrumental and emotional assistance to the mother. Conversely, we expected that decreased perceived support would be directly linked to mothers being embedded in networks where a higher proportion of members were reported as a source of interpersonal strain.
Turning to expectations regarding the relationships between network characteristics and maternal psychological adjustment (depressed mood and subjective well-being), two competing sets of hypotheses were assessed: (1) that network characteristics (structure, composition, availability, and function) would impact maternal psychological adjustment directly; and (b) that network characteristics would impact maternal adjustment indirectly via their effects on perceived social support. As noted above, past studies utilizing non-ASD samples suggest that network characteristics may affect mental health outcomes in both a direct and indirect fashion.
Methods
Participants
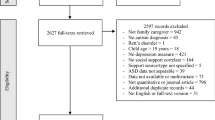
Data for the present study were drawn from an ongoing longitudinal study of children with ASD and their families (Benson et al. 2008; Benson and Karlof 2008; 2009; Benson 2010). The full sample of 142 parents was recruited into the study from a variety of public and private schools, multi-system special needs programs, and autism service organizations located in Massachusetts. The current study utilizes data collected in 2006 from a subsample of 106 mothers whose children had been identified with ASD based on the child’s medical records and an independent assessment by study staff using the Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994).
In terms of parent and family characteristics, the mean age of mothers participating in the study at Year 5 was 42.1 years (SD = 5.2). Most (80 %) were married at the time of the study and 40 % were employed, at least on a part-time basis, outside the home. The educational level of mothers in the sample was generally high, with two-thirds having obtained an undergraduate or post-graduate college degree. Total annual family income was also high, averaging between $80,000 and $89,000 a year, but varying substantially within the sample from under $30,000 (14 %) to over $149,000 a year (14 %). Finally, in terms of race/ethnicity, 85 % of participating mothers identified themselves as Caucasian.
In regard to the characteristics of the children with ASD, most were male (86 %), with a mean age of 8.6 years (SD = 1.5) at Year 5. Approximately 33 % of the child sample was diagnosed with autism, 29 % with PDD-NOS, 14 % with Asperger syndrome, and 24 % with an unspecified ASD. The primary mode of communication of 18 % of the children in the sample was through nonverbal means (signing, picture icons, etc.). In terms of school programs, 70 % attended public schools, while the remainder attended either a private or a multi-district collaborative special needs program. Three-fourths of the children attended an inclusive classroom for all or most of the school day, while one-fourth attended a self-contained special needs classroom.
Procedures
Data were gathered from participating mothers using questionnaires and in-home interviews. Study questionnaires included items on child and family characteristics, parent coping, social support, and other topics, while in the interviews, mothers were asked to talk about a variety of issues, including whom they utilized for various form of assistance, both in general and specifically in terms of caring for their child with ASD.
Specific information on mothers’ support networks was assessed using a modified version of the hierarchical mapping procedure developed by Antonucci (1986). Employing a diagram of three concentric circles with the word “you” at the center, mothers were asked to identify the “important people in your life right now whom you count on for support and assistance.” Following the enumeration of all network members (the respondent’s “total” support network), participating mothers were asked to identify the 10 “most important” people in their network (their “core” support network), placing each in the inner, middle, or outer circle of the diagram to indicate their overall importance and closeness to the respondent. Mothers were then asked a series of close-ended questions concerning the characteristics of core network members, including their age, gender, relationship to the respondent, frequency of contact, geographic proximity, and whether they were the parent of a child diagnosed with ASD. Mothers were also asked to identify network members who provided them with eight different types of support (coded 1 = yes; 0 = no): having someone to confide in; having someone who will make them feel respected; having someone to reassure them; having someone to talk to when upset, nervous, or depressed; having someone who provides advice; having someone to care for them when ill, having someone to care for their child with ASD when they were ill, and having someone to care for their child with ASD on an ongoing basis. Mothers were also asked to identify members of their network who were a source of interpersonal strain (by being critical, creating tensions or arguments, or making excessive demands on them). While somewhat tedious to implement, this mapping procedure generates detailed support network data and, for that reason, has been used in a variety of studies of networks, social support, and physical and mental health (e.g., Antonucci and Akiyama 1987; Ashida and Heaney 2008; Levitt et al. 1993; Peek and Lin 1999; Smith et al. 2011).
Measures
Network Characteristics
Employing the mapping technique described above, 10 maternal support network characteristics were assessed. These included two measures of network structure: (1) network size (the number of people identified as members of the mother’s total network) and (2) network density (the percentage of total network members in the mother’s inner circle). Three measures of network composition were also included: (3) proportion of kin; (4) proportion of females; and (5) number of parents of children with ASD in the maternal core network (excluding the respondent’s spouse). Two measures of network availability were also assessed: (6) geographic proximity (the mean distance of core network members to the mother assessed on 5-point scale ranging from 1 = less than a five-minute drive away to 5 = more than one day’s drive away); and (7) frequency of contact (the mean frequency of contact between core network members and the respondent assessed on a 5-point scale ranging from 1 = several times daily to 5 = once monthly or less.). Finally, based on the results of an exploratory factor analysis (results available from the author), three indices assessing functional aspects of the maternal network support were calculated and included in the analyses. The first two measures, proportion providing emotional support and proportion providing instrumental support, were obtained by calculating the mean percentage of core network members providing emotional support (i.e., confides in, provides reassurance, provides advice, respects, and talks to when upset) or instrumental support to the mother (i.e., provides care for mother if ill, provides childcare if mother is ill, and provides ongoing childcare). A third index, proportion engendering interpersonal strain, was obtained by calculating the mean percentage of network members engaged stressful interactions with the mother (i.e., being critical, making excessive demands, or creating tensions or arguments). Based on these calculations, the proportion of core network members providing emotional support was 0.60 (SD = 0.20), 0.42 for instrumental support (SD = 0.18), and 0.12 for interpersonal strain (SD = 0.10). Cronbach’s alphas for the three network function indices were 0.88, 0.90, and 0.92 for emotional support, instrumental support, and interpersonal strain, respectively.
Perceived Social Support
Mothers’ perception of social support was assessed using the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al. 1988). Using a 7-point scale (1 = very strongly disagree to 7 = very strongly agree), the index includes 12 items asking about social support available from family members, friends, and a significant other (e.g., “I can talk about problems with my family,” “My friends really try to help me, ““I have someone I can count on”). Possible scores on the MSPSS range from 12 to 84, with higher scores indicating greater perceived social support (mean = 61.2; SD = 13.8). Reliability for the MSPSS in the current sample was 0.89.
Depressed Mood
Mothers’ level of depressed mood was measured using a seven-item short form of the Center for Epidemiologic Studies-Depression Scale (CES-D; Radoff 1977; Ross and Mirowsky 1984). Using the CES-D short form, respondents were asked on how many days (0–7) during the past week they had experienced seven common depressive symptoms (e.g., “felt lonely,” “felt sad”, “felt that everything was an effort”). Responses on the items were then added to produce an index score ranging from of 0–49 (mean = 15.1; SD = 12.2). The short form correlates 0.92 with the full 20-item CES = D (Ross and Mirowsky 1984) and has been used extensively in prior research (e.g., Longmore and Demaris 1997; Mirowsky and Ross 1992; Pillemer et al. 2010). As is common with count variables, the distribution of responses on the CES-D short form were positively skewed and so were square-root transformed in order to correct for non-normality. Cronbach’s alpha for the CES-D was 0.84.
Subjective Well-Being
Defined as “a general sense of enjoying life, feeling happy (and) hopeful about the future” (Mirowsky and Ross 2003: 26), maternal subjective well-being was assessed using a three-item index developed by Ross (1996). Using this measure, respondents were asked on how many days (0–7) during the past week they had (a) enjoyed life? (b) felt happy? (c) felt hopeful about the future? Responses were summed to create an index of 0–21(mean = 12.4; SD = 6.7). In the present study, Cronbach’s alpha for the well-being measure was 0.91.
Parent, Child, and Family Characteristics
In addition to the measures noted above, several other parent, family, and child characteristics were included for use as potential covariates in the multivariate analyses reported below, including maternal marital status (coded 1 = currently married; 0 = other), maternal race (coded 1 = Caucasian; 0 = other), maternal education (coded on a 7- point scale, 1 = high school graduate or less” to 7 = doctoral degree), child autism symptom severity, and presence of additional children with ASD in the household (coded 1 = yes; 0 = no). Child symptom severity was assessed using the parent-report version of the Social Responsiveness Scale (SRS; Constantino et al. 2003), a 65-item index that ascertains quantitative data on the frequency of a wide array of autistic symptoms and traits (coded on a 4-point scale: 1 = not true to 4 = almost always true). Because nearly one-fifth of children with ASD in the present study were nonverbal, 12 SRS items assuming verbal language use by the child were excluded from the measure, resulting in a 53-item autism symptom severity scale (mean = 148.1; SD = 22.9). Cronbach’s alpha for the modified SRS was 0.93.
Data Analysis Plan
In the first stage of the analysis, descriptive statistics (means and percentages) were used to describe the characteristics of mothers’ support networks. This was followed by an examination of the bivariate relationships between network characteristics and our three outcomes of interest, perceived social support, depressed mood, and subjective well-being. In addition, correlations between outcomes and parent, child, and family characteristics were examined in order to determine whether any of these latter variables needed to be included as covariates in our multivariate analyses.
In the third stage of our analysis, structural equation modeling (SEM) was used to estimate the direct and indirect pathways between network characteristics, perceived social support, and psychological adjustment (depressed mood and subjective well-being). All models were estimated employing the maximum likelihood method in the Amos 19.0 program (Arbukle 2010). Following the recommendations of Hu and Bentler (1999), multiple indices are reported to assess model fit, with a good fit to the data being indicated by a statistically nonsignificant chi-square statistic (p > .05), a χ2/df ratio of close to 1, a comparative fit index (CFI) greater than 0.95, and a root mean square error of approximation (RMSEA) of <0.06. Following the estimation of full and trimmed models, utilizing a SPSS macro developed by Preacher and Hayes (2008), bias-corrected and accelerated bootstrapping procedures were used to test for the presence of significant indirect effects, with confidence intervals being set at 0.95 with 2,000 resamples. Prior to all multivariate analyses, study data were checked diagnostically for violations of standard SEM assumptions, with no serious violations being detected.
Results
Descriptive Analyses
Turning first to our descriptive findings, mothers named 1,640 individuals as members of their “total” support network (mean = 15.5; SD = 6.2), with 1,017 (62 %) of these individuals named as members of mothers’ “core” network (mean = 9.6; SD = 3.9). Not surprisingly, core networks included a substantially higher percentage identified as close network members, with 50 % of those in core networks being placed in the mother’s inner circle, compared to 36 % of those in mothers’ total networks.
Additional information on the characteristics of mothers’ core support networks is presented in Table 1. In terms of sociodemographic characteristics, most network members were identified as female (61 %), immediate or extended family members (52 %) or friends (29 %), with a mean age of 47 years (SD = 13.5). In addition, most network members were college graduates (64 %). In regard to network availability, most network members were reported as living within a 30 min drive of the respondent’s home (65 %), while nearly half (47 %) were in contact with the mother several times a week or more. Finally, 8 % of maternal networks were reported as including at least one non-spouse parent of a child diagnosed with ASD.
Table 2 presents data on the mean number of core network members reported as engaging in specific supportive or strain-inducing interactions with the mother, broken down by circle placement. As indicated, a substantially higher mean number of network members were reported as providing emotional support (mean = 5.8, SD = 2.6) and instrumental support (mean = 4.3, SD = 2.3) to mothers than were reported as fostering interpersonal strain (mean = 1.1, SD = 1.1). Inner circle network members were also named by mothers as the most frequent source of instrumental and emotional support, as well as interpersonal strain.
Bivariate Relationships
Turning next to an examination of the bivariate relationships between network characteristics and maternal outcomes, as shown in Table 3, one measure of network structure, network size, was found to be significantly related to perceived social support and maternal well-being, but not to depressed mood, while network density (i.e., proportion of network members in the mother’s inner circle) was unrelated to any maternal outcome. In terms of our measures of network function, proportion providing instrumental support, emotional support, and engendering interpersonal strain, were each found to be significantly associated with perceived social support, depressed mood, and subjective well-being in the expected direction. Contrary to expectations, however, none of our measures of network composition (proportion female, proportion kin, number of parents of children with ASD) or availability (proximity, frequency of contact) were significantly correlated with any maternal outcome.
Additional correlational analyses were also conducted to assess the relationship between maternal outcomes and parent, child, and family characteristics (maternal education, marital status, race, child gender, child symptom severity, and presence of additional children with ASD in the household). Only two variables were found to be significantly correlated with any outcome, with maternal education being positively related to perceived social support (r = 0.23, p = .016), while child symptom severity was negatively associated with maternal well-being (r = −0.25, p = .011). Based on these results, maternal education was included as a covariate in the model predicting maternal depression, while maternal education and child symptom severity were included as covariates in the model predicting well-being. Table 4 presents the zero-order correlations for all variables included in the multivariate analyses.
Multivariate Analyses
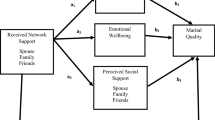
Utilizing predictor variables found to be significant in our bivariate analyses, SEM was then used to estimate the direct and indirect paths between network characteristics, perceived social support, and maternal mental health outcomes, As shown in Fig. 1, two hypothetical models were estimated, one predicting maternal depressed mood, the other predicting maternal well-being. Initial estimation of the full hypothesized models indicated that both were a good fit to the data [hypothetical depression model: χ2 (6, n = 106) = 6.03, p = .42; χ2/df = 1, CFI = 1, RMSEA = .01 (90 % CI: 0–.13); hypothetical well-being model: χ2 (11, n = 106) = 8.37, p = .68; χ2/df = .76, CFI = 1, RMSEA = 0 (90 % CI: 0–.81)]. Next, nonsignificant paths (p < .10) were dropped from the models and each was re-estimated. The resulting trimmed models also indicated a good fit to the data [trimmed depression model: χ2 (10, n = 106) = 8.87, p = .54; χ2/df = .89, CFI = 1, RMSEA = 0 (90 % CI: 0–.1); trimmed well-being model: X 2 (16, n = 106) = 12.9, p = .80; χ2/df = .81, CFI = 1, RMSEA = 0 (90 % CI: 0–.07)]. For both models, the difference in fit between the hypothesized and trimmed model was not significant [trimmed depression model: ∆χ2(3) = 2.84, p = .58; trimmed well-being model: ∆χ2(5) = 4.51, p = .48], indicating that, in each case, the more parsimonious trimmed model was not a worse fit than the hypothesized model. Figure 2 presents the final trimmed models used to predict maternal depressed mood and well-being, along with their path coefficients.
SEM results assessing direct and indirect relationships between network characteristics, perceived social support, and maternal psychological adjustment outcomes. Model A predicts maternal depressed mood. Model B predicts maternal subjective well-being. Numbers represent unstandardized path coefficients (standardized path coefficients in parentheses). + p < .10, *p < .05, **p < .01, ***p < .001
As shown in Fig. 2 (Model A), several significant direct and indirect pathways were found in the first trimmed model between network characteristics, perceived social support, and maternal depressed mood. In terms of direct effects, as expected, network size and proportion providing emotional support were each found to exert a significant positive effect on perceived social support, while proportion engendering interpersonal strain exerted a significant negative effect on this outcome, Also, as expected, perceived social support was found to be directly and negatively linked to maternal depressed mood, while interpersonal strain was negatively linked to depression. In addition, several significant indirect effects of network characteristics on depressed mood were found, with bootstrapped confidence intervals indicating that network size (point estimate = −0.015; 95 % CI: −0.037, −004), emotional support (point estimate = −0.644; 95 % CI: −1.614, −0.170), and interpersonal strain (point estimate = 0.810; 95 % CI: 0.053, 2.353), each exerted a significant indirect effect on depressed mood via its impact on perceived social support. In addition, maternal education was indirectly linked to depression via its effect on perceived social support (point estimate = −0.052; 95 % CI: −176, −0.004).
Turning to the second trimmed model in Fig. 2 (Model B), several significant pathways between network characteristics and maternal well-being were also found. Duplicating findings from the previous model, network size, emotional support, and interpersonal strain were each found to exert a significant direct effect on perceived social support. In addition, while no network factors were directly linked to well-being in this model, a direct positive path between perceived social support and well-being was found as well as a direct negative path between child symptom severity and well-being. As in the prior depression model, several significant indirect effects linking network characteristics to maternal well-being were uncovered, with bootstrapped confidence intervals indicating that perceived social support mediated the effects of network size (point estimate = 0.078; 95 % CI: 0.013, 0.164), emotional support (point estimate = 3.060; 95 % CI: 0.735, 6.027), and interpersonal strain (point estimate = −0.643; 95 % CI: −1.410, −0.095) on maternal well-being. Finally, as in the model predicting depression, maternal education was found to exert a significant indirect effect on well-being via its impact on perceived support (point estimate = 0.300; 95 % CI: 0.023, 0.752).
Discussion
Despite a large literature detailing the effects of social support on mental health, to date, very little research has examined the support networks of parents of children with ASD. The aim of the present study was to add to our knowledge in this area by systematically describing the characteristics of the support networks of a sample of mothers of children with ASD and assessing the relationship of those characteristics to perceived maternal social support and two related, but distinct, dimensions of maternal psychological adjustment, depressed mood and subjective well-being.
In regard to descriptive study findings, the 106 mothers in our sample identified 1,640 individuals in their “total” support networks, an average of approximately 15 members per network. Although we could find no other research reporting on the network size of mothers of children with ASD, this figure is larger than those found in studies of mothers of children with non-ASD disabilities (Kazak 1987; Kazak and Marvin 1984; Kazak and Wilcox 1984; Trute and Hauch 1988), while being generally comparable in size to those found in studies of mothers of nondisabled children (Levitt et al. 1986; Jennings et al. 1991; Lindblad-Goldberg and Dukes 1985). Thus, on the basis of size alone, it appears that the mothers of children with ASD in this study had fairly robust support networks.
In terms of the proportion of network members involved in supportive and stressful interactions with the mothers in our study, significant differences by closeness (circle placement) were noted, with more inner circle members, on average, providing instrumental and emotional support compared to network members placed in mothers’ middle and outer circles. Inner circle network members were also reported to be the most frequent source of interpersonal strain, although substantially fewer close network members were named as sources of interpersonal strain than of instrumental and emotional support. These findings are noteworthy given prior research suggesting that the benefits and costs of social ties may be greatest when network members are perceived as particularly close or important to the respondent (Antonucci 2001; McLaughlin et al. 2002; Thoits 1995).
Aside from describing mothers’ support networks, a major goal of this study was to examine the relationship between maternal network characteristics, perceived social support, and psychological adjustment. Based on our review of the literature, we expected that perceived support and adjustment (depressed mood and subjective well-being) would be significantly related to measures of network structure, composition, availability, and function. We also expected that at least some of the effects of network characteristics on adjustment would be mediated by perceived social support.
In terms of study findings regarding the impact of network characteristics on perceived social support, evidence was mixed. Consistent with our hypotheses and prior research with non-ASD samples (Lin and Peek 1999; Turner and Brown 2010), increased network size and network emotional support were found to be directly linked to increased perceived support, while increased network interpersonal strain was found to exert a direct negative effect on this outcome. At the same time, it is noteworthy that our network density measure (proportion of inner circle network members) as well as all of our measures of network composition (proportion female, proportion kin, number of parents of children with ASD) and availability (proximity, frequency of contact) were found not to be significantly correlated to perceived support in our bivariate analyses. Furthermore, an additional measure of network function (proportion providing instrumental support) was found not to be significantly related to perceived support in our multivariate analyses. Because this pattern of nonsignificant findings is generally inconsistent with the results flowing from prior network studies using non-ASD samples (e.g., Antonucci and Akiyama 1987; Suitor and Pillemer 2002; Wellman and Frank 2001), additional research is clearly needed to validate our results and to further explicate the relationship between network characteristics and social support in the families of children with ASD.
Turning to findings regarding network effects on maternal adjustment (depressed mood and well-being), our results indicate greater support for the view that networks affect mental health indirectly (Berkman et al. 2000; Thoits 2011) than for the view that they impact adjustment directly (Pescosolido and Georgianna 1989). In our SEM analyses, only one significant direct network effect on maternal adjustment was observed, with interpersonal network strain exerting a significant negative effect on depressed mood. On the other hand, several features of network structure (size) and function (proportion providing emotional support and interpersonal strain) exerted significant indirect effects on maternal depressed mood and well-being via their direct effects on perceived social support. Thus, consistent with research emphasizing the interplay of objective and subjective aspects of network support (Berkman et al. 2000), study findings suggest that network ties and the emotional support they provide increase mothers’ perception of support which, in turn, reduces depressed mood and increases well-being. At the same time, consistent with research on the potentially negative effects of social relationships (Rook et al. 2003), study results also indicate that stressful interactions with network members can damage one’s sense of being supported, leading to increased depression and decreased subjective well-being.
When considering study findings, it is important to note study limitations as well. The size of the sample, while larger than that used in many family studies, is still relatively small, thus limiting our ability to detect potentially meaningful relationships among study variables. In addition, our measurement of network characteristics was not always optimal. For example, our measures of network support were limited to assessments of emotional and instrumental support only, leaving out other potentially important elements of social support, including informational support and companionship (Lakey and Cohen 2000). Our measure of perceived social support also did not take into account professional sources of social support such as those provided by therapists, teachers, and physicians. In addition our measure of network density was less than ideal, given that it assessed only the strength of mothers’ network ties, not the ties between other network members.
It is also important to note that the mothers in our sample were largely Caucasian, well-educated, and economically well off; this limiting the generalizability of study findings to non-white and lower SES populations, as well as to fathers and other caregivers. The exclusion of fathers from the study sample is a particularly important limitation. Research indicates that the social networks of men and women differ significantly from one another and often have differing effects on social support and mental health (Ajrouch et al. 2005; Haines et al. 2008; Fuhrer et al. 1999). Because the present study included only mothers, we were unable to assess these potentially important gender differences.
Furthermore, it is useful to recall that our analysis primarily made use of a subsample of “core” network members rather than the full sample of “total” network members identified by respondents. While restricting core network membership to the 10 “most important” members was necessary in order to limit interview length and respondent fatigue (and is common practice in network surveys; see Brissette et al. 2000), it unavoidably introduced bias into the selection of network members, potentially leading to an overrepresentation of “close” network members (particularly family and friends) and an underrepresentation of “peripheral” network members such as coworkers, neighbors, and treatment professionals.
Finally, our use of cross-sectional data constitutes another important study limitation. Researchers have clearly demonstrated the need for longitudinal data to establish causal connections between characteristics of the social environment and mental health outcomes. The need for longitudinal data may be particularly critical in studies such as our own where depressive symptoms can affect both respondents’ social networks and their perception of available social support.
Despite these limitations, the present study enhances our understanding of the crucial role played by social networks in promoting positive psychological adjustment in the parents of children with ASD. As has prior research, we found perceived social support to be significantly related to decreased depression and increased maternal well-being. We also found perceived support to be directly linked to features of the mothers’ support networks, including network size and the extent to which network members engaged in supportive and stressful exchanges with the mother. These latter findings suggest that further research is needed aimed at increasing our understanding the social processes through which social network support is generated, maintained, and at times, hindered or disrupted. In particular, research is needed which closely examines the types, magnitude, and sources of negative social interactions experienced by mothers and fathers of children with ASD and their impact on parental mental health. As have other studies, findings from the present study indicate that problematic interactions, even with a very small proportion of network members, can exert substantial negative effects on individual support and adjustment.
Finally, taken together, study findings point to the potential utility of interventions aimed at enhancing parents’ support networks. Unfortunately, while a wide variety of parent and family support interventions are employed within the autism field (Hastings and Beck 2004; Marcus et al. 2005; Mandell and Salzer 2007), very little is known about how these various interventions affect participants’ social networks, their real and perceived levels of social support, and their overall psychological health. Existing research with non-ASD populations, however, suggests that, in order to be effective, support interventions must be closely aligned with participants’ needs and resources, including the strengths and weaknesses of preexisting social networks (Helgeson and Gottlieb 2000). Thus it may be useful to include network assessments as part of the intervention planning process (Heaney and Israel 2008). In addition, since not all network ties are beneficial, it is important for evaluators to take into account both the positive and potentially negative consequences of network change when assessing program effectiveness and impact.
References
Abbeduto, L., Seltzer, M. M., Shattuck, P., Krauss, M. W., Orsmond, G., Murphy, M. M., et al. (2004). Psychological well-being and coping in mothers of youths with autism, Down syndrome, or fragile X syndrome. American Journal on Mental Retardation, 109, 237–254.
Ajrouch, K. J., Blandon, A. Y., & Antonucci, T. C. (2005). Social networks among men and women: The effects of age and socioeconomic status. Journal of Gerontology, 60B, S311–S317.
Antonucci, T. C. (1986). Social support networks: Hierarchical mapping technique. Generations, 10, 1–12.
Antonucci, T. C. (2001). Social relations: An examination of social networks, social support, and sense of control. In K. E. Birren & K. W. Schaie (Eds.), Handbook of psychology of aging (pp. 427–453). New York: Academic Press.
Antonucci, T. C., & Akiyama, H. (1987). Social networks in adult life and a preliminary examination of the convoy model. Journal of Gerontology, 42, 519–527.
Arbukle, J. L. (2010). IBM SPSS Amos 19 user’s guide. Chicago: Amos Development Corporation.
Ashida, S., & Heaney, C. A. (2008). Differential association of social support and social connectedness with structural features of social networks and the health status of older Americans. Journal of Aging and Health, 20, 872–893.
Beggs, J. J., Haines, V. A., & Hurlbert, J. S. (1996). Situational contingencies surrounding the receipt of social support. Social Forces, 75, 201–222.
Benson, P. R. (2006). The impact of symptom severity of depressed mood among parents of children with ASD: The mediating role of stress proliferation. Journal of Autism and Developmental Disorders, 36, 685–695.
Benson, P. R. (2010). Coping, distress, and well-being in mothers of children with autism. Research in Autism Spectrum Disorders, 4, 217–228.
Benson, P. R., & Karlof, K. L. (2008). Child, parent, and family predictors of latter adjustment in siblings of children with autism. Research in Autism Spectrum Disorders, 2, 583–600.
Benson, P. R., & Karlof, K. L. (2009). Anger, stress proliferation, and depressed mood among parents of children with ASD: A longitudinal replication. Journal of Autism and Developmental Disorders, 39, 350–362.
Benson, P. R., Karlof, K. L., & Siperstein, G. N. (2008). Maternal involvement in the education of young children with autism spectrum disorders. Autism, 12, 47–63.
Beresford, B. A. (1994). Resources and strategies how parents cope with the care of a disabled child. Journal of Child Psychology and Psychiatry, 35, 171–209.
Berkman, L. F., Glass, T., Brissette, I., & Seeman, T. (2000). From social integration to health: Durkheim in the new millennium. Social Science and Medicine, 51, 843–857.
Blacher, J., & McIntyre, L. L. (2006). Syndrome specificity and behavioral disorders in young adults with intellectual disability: Cultural differences in family impact. Journal of Intellectual Disability Research, 50, 184–198.
Boyd, B. A. (2002). Examining the relationship between stress and lack of social support in mothers of children with autism. Focus on Autism and Other Developmental Disabilities, 17, 208–215.
Brissette, I., Cohen, S., & Seeman, T. E. (2000). Measuring social integration and social networks. In S. Cohen, L. H. Underwood, & B. H. Gottlieb (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 53–85). New York: Oxford University Press.
Bromley, J., Hare, D. J., Davidson, K., & Emerson, E. (2006). Mothers supporting children with autism spectrum disorders: Social support, mental health status, and satisfaction with services. Autism, 8, 409–423.
Brown, G. W., & Harris, T. O. (1978). The social origins of depression: A study of psychiatric disorder in women. New York: Free Press.
Burg, M. M., & Seeman, T. E. (1994). Families and health: The negative side of social ties. Annals of Behavioral Medicine, 16, 109–115.
Chan, Y. K., & Lee, R. P. L. (2006). Network size, social support, and happiness in later life: A comparative study in Beijing and Hong Kong. Journal of Happiness Studies, 7, 87–112.
Constantino, J. N., Davis, S. A., Todd, R. D., Schindler, M. K., Gross, M. M., Brophy, S. L., et al. (2003). Validation of a brief quantitative measure of autistic traits: Comparison of the social responsiveness scale with the autism diagnostic interview-revised. Journal of Autism and Developmental Disorders, 33, 427–433.
Ekas, N. V., Lickenborck, D. M., & Whitman, T. L. (2010). Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 40, 1274–1284.
Emerson, E. (2003). Mothers of children and adolescents with intellectual disability: Social and economic situation, mental health status, and the self-assessed social and psychological impact of the child’s difficulties. Journal of Intellectual Disability Research, 47, 385–399.
Fiori, K. L., Antonnucci, T. C., & Cortina, K. S. (2006). Social network typologies and mental health among older adults. Journal of Gerontology, 61B, P25–P32.
Fuhrer, R., Stansfield, S. A., Dhemali, J., & Shipley, M. J. (1999). Gender, social relations, and mental health: Prospective findings from an occupational cohort (Whitehall II study). Social Science and Medicine, 48, 77–87.
Glidden, L. M., & Schoolcraft, S. A. (2007). Family assessment and social support. In J. W. Jacobson, J. A. Mulick, & J. Rojahn (Eds.), Handbook of intellectual and developmental disabilities (pp. 391–422). New York: Springer.
Haines, V. A., Beggs, J. J., & Hurlbert, J. S. (2002). Exploring the structural contexts of the support process: Social networks, social statuses, social support, and psychological distress. In J. Levy & B. A. Pescosolido (Eds.), Social networks and health (pp. 269–292). New York: Elsevier.
Haines, V. A., Beggs, J. J., & Hurlbert, J. S. (2008). Contextualizing health outcomes: Do effects of network structure differ for woman and men? Sex Roles, 59, 164–175.
Hartwell, S. W., & Benson, P. R. (2007). Social integration: A conceptual overview and two case studies. In B. A. Pescosolido, J. D. McLeod, & W. R. Avison (Eds.), Mental health, social mirror (pp. 329–353). New York: Springer.
Hastings, R. P., & Beck, A. (2004). Practitioner review: Stress interventions for parents of children with intellectual disabilities. Journal of Child Psychology and Psychiatry and Allied Disciplines, 45, 1338–1349.
Hastings, R. P., & Brown, T. (2002). Child behavior problems of autistic children, parental self-efficacy, and mental health. American Journal of Mental Retardation, 107, 222–232.
Heaney, C. A., & Israel, B. A. (2008). Social networks and social support. In K. Glantz, B. Rimer, & K. Vaswaneth (Eds.), Health behavior and health education: Theory, research, and practice (4th ed., pp. 189–212). San Francisco: Jossey-Bass.
Helgeson, V. S., & Gottlieb, B. H. (2000). Support groups. In S. Cohen, L. G. Underwood, & B. H. Gottlieb (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 221–245). New York: Oxford University Press.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55.
Jennings, K. D., Stagg, V., & Connors, R. E. (1991). Social networks and mothers’ interaction with their preschool children. Child Development, 62, 966–978.
Kazak, A. E. (1987). Families with disabled children: Stress and social networks in three samples. Journal of Abnormal Child Psychology, 15, 137–146.
Kazak, A. E., & Marvin, R. S. (1984). Differences, difficulties, and adaptation: Stress and social networks in families with a handicapped child. Family Relations, 33, 67–77.
Kazak, A. E., & Wilcox, D. I. (1984). The structure and function of social support networks in families with handicapped children. American Journal of Community Psychology, 12, 646–661.
Kessler, R. C., & McLeod, J. D. (1984). Sex differences in vulnerability to undesirable life events. American Sociological Review, 49, 620–631.
Lakey, B., & Cohen, S. (2000). Social support theory and measurement. In S. Cohen, L. G. Underwood, & B. H. Gottlieb (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 29–52). New York: Oxford University Press.
Levitt, M. J., Guacci-Franco, N., & Levitt, J. L. (1993). Convoys of social support in childhood and early adolescence: Structure and function. Developmental Psychology, 29, 811–818.
Levitt, M. J., Weber, R. A. S., & Clark, M. C. (1986). Social network relationships as sources of maternal support and well-being. Developmental Psychology, 22, 310–316.
Lin, N., & Peek, K. (1999). Social networks and mental health. In A. V. Horwitz & T. L. Schneid (Eds.), A handbook for the study of mental health: Social contexts, theories, and systems (1st ed., pp. 241–258). New York: Cambridge University Press.
Lincoln, K. D. (2000). Social support, negative social interactions, and psychological well-being. Social Service Review, 74, 231–252.
Lindblad-Goldberg, M., & Dukes, J. L. (1985). Social support in black, low-income, ingle parent families. Journal of Orthopsychiatry, 55, 42–58.
Longmore, M. A., & Demaris, A. (1997). Perceived inequality and depression in intimate relationships: The moderating effect of self-esteem. Social Psychology Quarterly, 60, 172–184.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24, 659–685.
Mandell, M. S., & Salzer, D. S. (2007). Who joins support groups among parents of children with autism. Autism, 11, 111–122.
Marcus, L. M., Kunce, L., & Scholpler, E. (2005). Working with families. In F. R. Volkmar, R. Paul, A. Klin, & D. Cohen (Eds.), Handbook of autism and pervasive developmental disorder (pp. 1055–1086). New York: Wiley.
Marsden, P. V., & Campbell, K. E. (1984). Measuring tie strength. Social Forces, 63, 482–501.
McLaughlin, J., Horwitz, A. V., & White, H. R. (2002). The differential importance of friend, relative, and partner relationships for the mental health of young adults. In J. A. Levy & B. A. Pescosolido (Eds.), Social networks and health (pp. 223–246). New York: Elsevier.
Mirowsky, J., & Ross, C. E. (1992). Age and depression. Journal of Health and Social Behavior, 33, 187–205.
Mirowsky, J., & Ross, C. E. (2003). Social causes of psychological distress. Chicago: Aldine.
Olsson, M. B., & Hwang, C. P. (2001). Depression in mothers and fathers of children with intellectual disability. Journal of Intellectual Disability Research, 45, 535–543.
Peek, K. M., & Lin, N. (1999). Age differences in the effects of network composition on psychological distress. Social Science and Medicine, 49, 621–636.
Pescosolido, B. A., & Georgianna, S. (1989). Durkheim, suicide, and religion: Toward a network theory of suicide. American Sociological Review, 54, 33–48.
Pillemer, K., Suitor, J. J., Pardo, S., & Henderson, C. (2010). Mother’s differentiation and depressive symptoms among adult children. Journal of Marriage and the Family, 72, 333–345.
Pottie, C. G., Cohen, J., & Ingram, K. M. (2009). Parenting a child with autism: Contextual factors associated with enhanced daily parental mood. Journal of Pediatric Psychology, 34, 419–429.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891.
Radoff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401.
Rook, K., Sorkin, D., & Zettel, L. (2003). Stress in social relationships: Coping and adaptation across the life span. In F. R. Long (Ed.), Growing together: Personal relationships across the life span (pp. 210–239). New York: Cambridge University Press.
Ross, C. E. (1996). Work, family, and well-being in the United States, 1990. Champaign, IL: Survey Research Laboratory, University of Illinois.
Ross, C. E., & Mirowsky, J. (1984). The components of depressed mood in married men and women: The Center for Epidemiological Studies Depression Scale. American Journal of Epidemiology, 119, 997–1004.
Seeman, T. E., & Berkman, L. F. (1988). Social characteristics of social networks and their relationship with social support in the elderly: Who provides support? Social Science and Medicine, 26, 737–749.
Singer, G. H. S. (2006). Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. American Journal of Mental Retardation, 111, 155–169.
Smith, L. E., Greenberg, J. S., & Seltzer, M. M. (2011). Social support and well-being at mid-life among mothers of adolescents and adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. doi:10.1007/s10803-011-1420-9.
Suitor, J. J., & Pillemer, K. (2002). Gender, social support, and experiential similarity during chronic stress. Advances in Medical Sociology, 8, 247–266.
Tausig, M. (1992). Caregiver network structure, support, and caregiver distress. American Journal of Community Psychology, 20, 81–96.
Thoits, P. A. (1995). Stress, coping, and social support processes: Where are we? What’s next? Journal of Health and Social Behavior, 36, 72–82.
Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52, 145–161.
Trute, B., & Hauch, S. (1988). Social network attributes of families with positive adaptation to the birth of a developmentally disabled child. Canadian Journal of Community Mental Health, 7, 5–16.
Turner, R. Jay., & Brown, R. L. Brown. (2010). Social support and mental health. In A. V. Horwitz & T. L. Schneid (Eds.), A Handbook for the study of mental health: Social contexts, theories, and systems (2nd ed., pp. 200–212). New York: Cambridge University Press.
Weiss, M. J. (2002). Hardiness and social support as predictors of stress in mothers of typical children, children with autism, and children with mental retardation. Autism, 6, 115–130.
Wellman, B., & Frank, K. A. (2001). Network capital in a multilevel world: Getting support from personal communities. In N. Lee, K. Cook, & R. S. Burt (Eds.), Social capital: Theory and research (pp. 23–273). New York: Aldine De Gruyter.
Wellman, B., Potter, S., & Gulia, M. (2003), Where does social support come from? The interpersonal resources for coping with stress [electronic version]. In A. Manley, & J. Ramos (Eds.), Socioeconomic conditions, stress, and mental disorder: Toward a new synthesis of research and public policy (Chap. 15) Rockville, MD: National Institute of Mental Health. Retrieved August 15, 2011 from http://www.mhsip.org/nimhdoc/ socioeconmh_home2.htm.
Wellman, B., & Wortley, S. (1990). Different strokes from different folks: Community ties and social support. American Journal of Sociology, 96, 558–588.
White, N., & Hastings, R. P. (2004). Social and professional support for parents of adolescents with severe intellectual disabilities. Journal of Applied Intellectual Disabilities, 17, 181–190.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52, 30–41.
Acknowledgments
Special thanks are extended to the mothers who participated in this study and to Kristie Karlof, Dorothy Robison, and Zach Rossetti for their invaluable assistance in data collection. The research on which this study is based was supported by the U.S. Department of Education, Grant No. H324C040092 (A Longitudinal Study of Children with ASD and Their Families During the Elementary School Years).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Benson, P.R. Network Characteristics, Perceived Social Support, and Psychological Adjustment in Mothers of Children with Autism Spectrum Disorder. J Autism Dev Disord 42, 2597–2610 (2012). https://doi.org/10.1007/s10803-012-1517-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-012-1517-9