Abstract
Sluggish cognitive tempo (SCT) is characterized by behavioral symptoms reflecting slowness and lethargy (e.g., sluggishness, appearing sleepy) and inconsistent alertness/mental confusion (e.g., daydreaming, fogginess). SCT is substantially correlated with the inattentive symptoms of attention-deficit/hyperactivity disorder (ADHD) and may be part of that domain, but in cross-sectional data, SCT is also strongly associated with both inattention and depression. To date, no study has examined the prospective associations of SCT symptoms in childhood/adolescence with symptoms of ADHD and internalizing problems in adulthood. Using a sample of 449 twin children and adolescent pairs, prospective multiple regression analyses examined whether self- and parent-reported SCT, depression, and parent-reported symptoms of ADHD predicted symptoms in adulthood 12 years later. SCT and depression at time one were strongly correlated (self-reported SCT and depression r = 0.84; parent-reported SCT and depression r = 0.78). When adult outcomes were separately regressed on each youth symptom dimension, self-reported SCT (β = 0.26, p < 0.0001) and depression (β = 0.13, p < 0.0001) each predicted adult symptoms of depression and self-reported SCT predicted inattention (β = 0.12, p = 0.0026). Parent-reported depression, but not parent-reported SCT, predicted self-reported adult depression symptoms (β = 0.17, p = 0.0003). In contrast, when each adult outcome was regressed simultaneously on youth self-reported SCT and depression, neither predicted adulthood inattention or depression. These findings indicate that SCT in childhood and adolescence is strongly associated concurrently and predictively with both inattention and depression. Theoretical and clinical applications of the construct of SCT must take its robust association with both inattention and depression into account.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The construct of sluggish cognitive tempo (SCT), characterized by excessive daydreaming, slowed behavior/thinking, and mental confusion, is not currently included in a diagnostic nosology (Becker et al., 2016), despite the frequent presence of such symptoms in the clinical literature. The study of SCT began as part of an attempt to determine if there was an additional domain of attention-deficit/hyperactivity disorder (ADHD) (e.g., Carlson et al., 1986). However, there is strong evidence that SCT and ADHD are at least partly distinct constructs (Becker et al., 2016). Indeed, although ADHD is a core externalizing disorder, recent work has suggested SCT may be better viewed as part of internalizing psychopathology (Becker et al., 2016; Becker & Willcutt, 2019; Servera et al., 2018; Smith et al., 2018; Ward et al., 2019). Consistent with this idea, SCT is associated with depression and anxiety even when controlling for inattentive symptoms (Becker et al., 2016; McBurnett et al., 2014; Smith & Langberg, 2017). Interestingly, SCT has been moderately to strongly associated with both externalizing (e.g., ADHD) and internalizing disorders (e.g., depression; Becker et al., 2016; Becker & Willcutt 2019; Servera et al., 2018; Smith & Langberg, 2017).
There is growing evidence that SCT is strongly associated with depression and that childhood SCT symptoms predict adolescent depressive symptoms (Becker & Willcutt, 2019; Becker et al., 2018). In a large, nationally representative sample of children ages 4–13, found that in a parent-reported high SCT group, 35% of youth met criteria for a clinical cutoff of depression and SCT was uniquely associated with depression at a higher rate than ADHD inattentive symptoms. However, no study has examined whether SCT in childhood predicts later psychopathology in adulthood. A recent body of research has found SCT to be partly distinct from other groups of internalizing symptoms (Becker et al., 2018; Becker et al., 2015; McBurnett et al., 2014; Smith et al., 2019; Willcutt et al., 2014). Although a myriad of studies have examined the discriminant validity of SCT and ADHD, only a handful have found discriminant validity between SCT and depression (Becker et al., 2018; Becker et al., 2014; Lee et al., 2014; McBurnett et al., 2014; Smith et al., 2019; Willcutt et al., 2014). However, only two of these studies used self-report of SCT, which is essential to the assessment of internalizing psychopathology. Using factor analyses, these two studies found self-reported SCT and depression to be distinct, but strongly correlated factors (Becker et al., 2015; Smith et al., 2018). Becker et al. (2015) used exploratory structural equation modeling with a sample of 124 children ages 8–13 to examine the distinctiveness of the factors of depression, anxiety, ADHD, and SCT. The best fitting model found that the construct of child-rated SCT was a distinct factor from child-rated depression and anxiety and teacher-rated ADHD. Self-reported SCT was strongly correlated with depression (r = 0.68) and anxiety (r = 0.55). Building upon this work, Smith et al. (2019) used confirmatory factor analysis with a sample of 262 adolescents with ADHD, finding SCT, depression, anxiety, and daytime sleepiness all to be distinct factors. Although distinct factors, SCT was strongly associated with depression (r = 0.51), anxiety (r = 0.51), and daytime sleepiness (r = 0.55). Both studies found strong associations between SCT and internalizing factors, but showed that SCT and depression form two distinct factors.
Currently, only ten studies from four samples have examined youth self-reported SCT (Becker et al., 2020), finding SCT to be uniquely associated with internalizing symptoms, academic impairment, and social difficulties (Becker, 2014; Becker et al., 2015, 2020; Holdaway & Becker, 2018; Sáez et al., 2019; Smith et al., 2019; Smith & Langberg, 2017). Further cross-sectional work has shown SCT to account for 23–30% of the variance in depression and to be negatively associated with externalizing factors such as ODD, CD, and hyperactivity-impulsivity (Becker et al., 2016; McBurnett et al., 2014; Smith & Langberg, 2017; Willcutt et al., 2014). Only one study to date (Becker et al. 2020) has examined different factors associated with depression (i.e., rumination, suicidal ideation, emotion dysregulation). Using a sample of 302 young adolescents with (n = 162) and without (n = 140) ADHD, they found SCT to be correlated with aspects of rumination (i.e., brooding r = 0.50, reflection r = 0.39), suicidal ideation (r = 0.35), and six aspects of emotion dysregulation (rs range 0.13–0.50). Additionally, SCT was uniquely associated with greater self-reported internalizing symptoms and suicidal ideation when controlling for ADHD inattentive symptoms, further suggesting the strong, but distinct, relationship between SCT and aspects of depression.
Very few studies have examined SCT longitudinally, with no study examining how childhood SCT predicts psychopathology in adulthood. One longitudinal study found parent-reported SCT in early childhood (ages 4–9), but not ADHD inattentive symptoms, uniquely predicted higher anxiety and depression in ninth grade (ages 14–16; Becker et al., 2018). This built on Servera and colleagues (2015) and Bernad et al. (2016) work that found SCT and ADHD inattentive symptoms both uniquely predicted depression in Spanish, school age children 1 year later. It would appear that SCT contributes more to later depression symptoms from childhood to adolescence than ADHD inattentive symptoms. However, these studies did not account for childhood depressive symptoms at the first time point in their analyses. Additionally, Becker et al. (2019) used cross-lagged panel analyses for teacher-reported SCT and teacher- and child-reported depression symptoms across 6-months. Time one SCT predicted increases in both teacher- and child-reported depressive symptoms 6 months later, but depression at time one did not predict SCT at time two. Thus, SCT may be a developmental precursor for risk of later depression, not the reverse (Becker et al., 2019). This emphasizes the importance of understanding whether SCT in childhood predicts later depressive symptoms, as youth with higher levels of SCT may be at risk for depression later in life.
In the present study, we examined SCT longitudinally including both parent- and self-report of SCT in a sample of 449 twin pairs initially assessed as youth ages 6–17. Importantly, this is the first study that used an interview format to assess SCT, which is described in more detail below. This sample was part of a larger study, the Tennessee Twin Study, which recruited twins to allow future comparative tests of shared and unique genetic and environmental dimensions of psychopathology, although this was out of the scope of the current analyses. We included both parent and self-report to address the lack of inclusion of self-report in the previously described studies. As parent- and self-report of SCT are not invariant across reporters (Smith et al., 2018), we anticipated a relatively weak correlation between the constructs as each provides unique information and previous work has found only weak associations (e.g., r = 0.16; Smith & Langberg, 2017). In order to address the impact of SCT longitudinally, we examined the ability of childhood symptoms of SCT, as well as associated constructs of inattention, hyperactivity-impulsivity, and depression to predict adult psychopathology 12 years later. We expected SCT to be strongly associated with concurrent depression, moderately associated with inattentive symptoms, and weakly associated with symptoms of hyperactivity-impulsivity. We hypothesized that self-reported SCT would predict depression and ADHD-inattentive symptoms in adulthood, with a weaker association with the ADHD inattentive domain. By contrast, we expected ADHD symptom domains would not predict later depression when including childhood SCT. As SCT is typically not associated with hyperactivity-impulsivity (Becker et al., 2016; Lee et al., 2014), we hypothesized that SCT would not predict later hyperactivity-impulsivity. If these hypotheses are supported, this would suggest the validity of SCT as a construct of importance in predicting psychopathology. If SCT both predicts depression, part of the internalizing nosology, and inattention, part of externalizing or its own domain (Laceulle et al., 2015; Lahey et al., 2017; Noordhof et al., 2015), this would provide further evidence that SCT is substantially correlated with both domains (Becker & Willcutt, 2019).
Method
Participants and Procedures
Wave one and Wave two participants from the Tennessee Twin Study (TTS; Lahey et al., 2008) were used in this sample. Study procedures were approved by the Vanderbilt University and University of Chicago Institutional Review Boards. All participants provided consent/assent at first visit through interview. See Lahey et al. (2008) for more information on sample and procedures.
Wave One Sample
The Wave one sample is representative of all 6–17-year-old twins in Tennessee’s five metropolitan statistical areas (MSAs) in 2000–2001, which includes the 28 urban, suburban, and rural counties surrounding the cities of Nashville, Memphis, Knoxville, Chattanooga, and Bristol. The Tennessee Department of Health identified all twin pairs born in Tennessee in the eligible age range, from which we recruited the sample. A total of 7968 households were initially identified, but 2431 households were eliminated because they lived outside an MSA in Tennessee at the time recruitment began. A random sample was selected from the remaining families, stratified by age and geographic subareas, proportional to the number of families. Of 4012 selected households, 3592 (89.5%) were located and screened, with 2646 of screened families being eligible (co-residence with the caretaker at least half time during the past 6 months and twins and caretakers spoke English). Interviews were completed with 2063 adult caretakers (90.8% biological mothers), with a 70% response rate. When caretakers were interviewed, 98% of both twins were interviewed. After excluding pairs in which either twin had been given a diagnosis of autism, psychosis, or seizure disorder, the sample consisted of 3990 twins in 1995 complete pairs. Caretakers classified 71% of the twins as non-Hispanic white, 24% African American, 2% as Hispanic, and 3% as other racial identities, which were representative of the broader twin population in Tennessee.
Wave One Measures
Adult caretakers and youth participants were interviewed separately using the Child and Adolescent Psychopathology Scale, which is a structured interview (CAPS; Lahey et al. 2004). The CAPS item pool covers all DSM-IV symptoms of ADHD and major depressive disorder (MDD) in DSM-IV and ICD-10 and includes 11 symptoms of SCT. CAPS items covering DSM-IV symptoms were based on the “stem questions” in Version IV of the Diagnostic Interview Schedule for Children (DISC-IV; Shaffer et al., 2000), modified from “yes or no” questions to fit a four-point response scale: “1. Not at all, 2. Just a little, 3. Pretty much, 4. Very much.” Interviewers read each item aloud to the respondent from a lap-top computer and entered responses using the computer. The program routed the interviewer from question to question, skipped age-inappropriate questions, used correct sex terms to refer to girls and boys, referred to “other children” or “other people your age” for youth <11 years or >11 years in some items, used the correct wording for children who did or did not attend school or work, and disallowed out-of-range responses. Participants were asked to respond by thinking about how well each item described the youth’s emotion or behavior, how often it occurred, and how serious it was during the last 12 months. Caretakers and youth were interviewed separately in private after caregivers provided signed consent and youth provided assent, typically by the same trained lay interviewer.
This is the first study to use an interview-based format to assess SCT. Currently, there is no gold standard for measuring SCT, though a recent meta-analysis suggested 13 items best represent SCT and are distinct from ADHD inattentive symptoms (Becker et al., 2016). This was confirmed in a sample of adolescents with and without ADHD, finding convergent validity of the SCT factor (13 items) and discriminant validity with the ADHD inattentive symptoms (Becker et al., 2020). The SCT construct in this study was created by selecting symptoms that fit the SCT factor found to have convergent and discriminant validity by Becker et al. (2020). We were able to include 11 of the 13 symptoms, as we did not have all the symptoms included in the CAPS interview (i.e., foggy, stare off, sleepy, daydream, lost in my thoughts, tired easily, confused, space out, thinking slowed; Becker et al., 2016, 2020). The additional two symptoms that were included in this study have also been found to be consistent with SCT (i.e., “sluggish” and “low energy”; Penny et al., 2009; Smith et al., 2018). Additionally, the SCT interview has proven to be internally consistent with parent-report alpha at 0.83 and self-report at 0.85. As Smith et al. (2018) found self- and parent-report to not be invariant across reporters, both respondents were included in separate analyses. Importantly, the factors of SCT and depression did not have overlapping items in this study.
In a representative sample of 1382 4–17 year olds (Lahey et al., 2004), a subset of the participants were selected for participation in a second interview 7–14 days following the initial interview to assess test–retest reliability of the CAPS. The test–retest intra-class correlations (ICCs) for unit-weighted mean ratings of the symptoms of ADHD symptom domains, MDD, and SCT on caretaker reports were inattention = 0.89, hyperactivity-impulsivity = 0.88, MDD = 0.82, and SCT = 0.84. The ICCs based on youth reports of symptoms were MDD = 0.69 and SCT = 0.77.
Wave Two Sample
Twin pairs for Wave two assessments were recruited in four replicates in reverse order of their age in Wave 1 (16–17, 14–15, 12–13, and 10–11 years) to minimize the age distribution in Wave two. Twin pairs were eligible if the last known address of both twins was within 300 miles of Vanderbilt University (95.2% of twins). Wave two participants were selected by oversampling based on greater ratings of psychopathology symptoms from parent- or youth-report at Wave one. High-risk pairs were selected with certainty if either twin had symptom ratings on the total number of internalizing, attention-deficit/hyperactivity disorder, or the combination of ODD and CD symptoms in the top 10% of that age range. In addition, 19–23% of the remainder of each replicate was randomly selected with two constraints: (a) monozygotic pairs were oversampled by randomly excluding 40% of the randomly selected dizygotic pairs, and (b) the number selected from the remainder of the sample varied slightly to equate replicate sizes (100–105 pairs). Three pairs of twins could not be located and 37 pairs refused screening. Eighteen selected pairs of twins across replicates were declared out of scope due to previous participation in a pilot study, mental or physical incapacity, residence outside the United States, imprisonment, or death. Interviews regarding psychopathology were completed for 72% of the screened sample during 2013–2016, including 248 complete twin pairs (49.5% monozygotic; 66.9% high risk) and 3 individuals without their twin.
The 499 interviewed participants were 23–31 years of age (median 26 years); 52.1% female; and self-identified as 71.5% Non-Hispanic white, 25.2% African American, and 3.2% other racial-ethnic groups. Twenty-six percent were still in school and the mean years of education was 14.3. Consistent with oversampling participants based on Wave one psychopathology, 50.3% met criteria for at least one Wave two mental disorder (46.2% of females; 54.8% of males) in the past year and 26.8% met criteria for ≥2 diagnoses. For the outcomes of interest, 5.0% met criteria for ADHD and 11.4% met criteria for Major Depressive Disorder.
Wave Two Measures
Psychopathology symptoms in adulthood were assessed using self-report on the young adult version of the Diagnostic Interview for Children (YA-DISC; Abram et al., 2015; Shaffer et al., 2008; Witkiewitz et al., 2013). The modules used in these analyses queried diagnostic criteria for adult ADHD and MDD over the past 12 months. Participants were asked about all symptoms of depression, however, only individuals that endorsed dysphoria and anhedonia were asked about frequency and duration of their depressive symptoms over the past 12 months. This may have resulted in higher prevalence of endorsed depression symptoms than if frequency and duration threshold were considered.
Data Analysis
Regression analyses were conducted using SURVEYREG procedure in the Statistical Analysis System (SAS) version 9.4, accounting for stratification and clustering with twin pairs and using weights to account both for the inverse of the probability of participation in Wave two based on selection and for nonresponse. These weights corrected any biases due to nonresponse relative to demographic characteristics (i.e., age at both time points, maternal education, race, sex) and Wave one measures of psychopathology. These weights allow valid parameter estimates when weighted back to the full Wave one TTS sample and, by extension, to the population from which the Wave one sample was drawn (Korn & Graubard, 1999).
In separate analyses for parent- and self-report of SCT in Wave one, we tested predictions that adult depression and inattention in Wave two, but not hyperactivity-impulsivity, would be independently predicted by Wave one SCT. First, each self-reported predictor variable at Wave one (i.e., self-reported SCT and depression, as self-reported inattention and hyperactivity-impulsivity were not collected at Wave one) and parent-reported predictor variable (i.e., SCT, depression, inattention, hyperactivity-impulsivity) were separately run to predict adult outcomes (i.e., depression, inattention, hyperactivity-impulsivity). Next, we included self-reported depression, parent-reported inattention, and parent-reported hyperactivity-impulsivity with self-reported SCT to predict adult outcomes. We did the same for parent-reported SCT, including parent-reported depression, inattention, and hyperactivity-impulsivity with parent-reported SCT to predict self-reported adult outcomes (i.e., depression, inattention, hyperactivity-impulsivity). Age in Wave one, the number of years since Wave one, gender, non-Hispanic white versus other race-ethnic group, the log of the total income of the family of origin, and the number of years of education of the twins’ mothers were covariates of no interest in all analyses. We corrected for multiple testing using a 5% false discovery rate (FDR) applied to two-tailed tests.
Results
Bivariate Associations
Bivariate correlations are displayed in Table 1. As expected, inter-rater correlations were stronger than cross-rater associations. Self-reported SCT and depression were strongly correlated (r = 0.84) at Wave one, while parent-reported hyperactive/impulsive, inattentive symptoms, depression, and SCT respectively were weakly correlated with self-reported SCT (r = 0.12, r = 0.23, r = 0.27, r = 0.21). This weak correlation between parent- and self-reported SCT was expected since the two are not invariant across reporters and is in line with previous work (e.g., Smith et al., 2018; Smith & Langberg, 2017). For parent-reported SCT, parent-reported depression was strongly associated with SCT (r = 0.78) and inattention was moderately correlated with SCT (r = 0.66). In contrast, hyperactive/impulsive, self-reported depression, and self-reported SCT were weakly associated with parent-reported SCT (r = 0.15, r = 15, r = 0.21). Between time points, all bivariate associations of the variables of interest were nonsignificant or weakly associated. See Table 1.
Prospective Multiple Regression Analyses
Analyses were run with each variable separately predicting later psychopathology, continuing to control for age, race, log of family income, gender, and maternal education (See Tables 2 and 3).
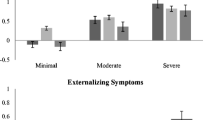
Predictor Variables Regressed Separately
When accounting for FDR, self-reported SCT (β = 0.26, 95% confidence interval (CI) [0.15, 0.37], p < 0.0001) and depression (β = 0.13, 95% CI [0.08, 0.18], p < 0.0001) separately predicted later adult depression. When separately regressed on adult inattentive symptoms, self-reported SCT also predicted adult inattentive symptoms (β = 0.12, 95% CI [0.04, 0.19], p = 0.0026). For parent-report, the findings when variables were separately regressed held, with parent-reported hyperactivity-impulsivity predicting adulthood hyperactivity-impulsivity (β = 0.06, 95% CI [0.03, 0.09], p = 0.0005) and depression predicting adulthood depression (β = 0.11, 95% CI [0.05, 0.17], p = 0.0004) respectively.
Predictor Variables Regressed Simultaneously
When adult outcomes were regressed simultaneously for youth symptoms dimensions and included self-reported SCT, only parent-reported hyperactivity-impulsivity symptoms predicted adult self-reported hyperactivity-impulsivity (β = 0.05, 95% CI [0.01, 0.09], p = 0.0017) when controlling for age, race, log of family income, gender, and maternal education and accounting for the FDR. Similarly, parent-reported hyperactivity-impulsivity predicted later self-reported adult hyperactivity-impulsivity (β = 0.06, 95% CI [0.03, 0.10], p = 0.0007) and parent-reported depression predicted later self-reported adult depression (β = 0.17, 95% CI [0.08, 0.27], p = 0.0003) when parent-report of SCT was simultaneously regressed on hyperactivity-impulsivity and depression respectively. See Tables 4 and 5 for more details. The strong associations between depression and SCT for both raters suggested that multicollinearity may have contributed to the nonsignificant finding of SCT and depression predicting adult depressive symptoms when both were included in analyses.
Discussion
Only a handful of studies have assessed SCT longitudinally, with no prior study examining whether SCT in childhood and adolescence predicts adulthood psychopathology. Additionally, no longitudinal study has used self-report of SCT to predict internalizing outcomes despite the fact that SCT may be considered an internalizing construct. As SCT has showed strong associations with both the externalizing and internalizing domains (Becker & Willcutt, 2019), we sought to examine its concurrent relationship to ADHD and depressive symptoms in childhood and whether it provides an independent prediction of adult psychopathology. When SCT and depression were run in separate analyses, both predicted adulthood depression, with the exception of parent-reported childhood SCT. According to parent-reported depression and SCT at time one, depression in childhood, but not SCT, predicted higher levels of depression in adulthood. However, when accounting for both self-reported SCT and depression at time one, neither predict later psychopathology. Our findings indicate that SCT in childhood and adolescence is associated concurrently and predictively with both depression and inattention.
Depression
When simultaneously regressing adult symptom dimensions on SCT and depression, only parent-reported depression predicted later adulthood depression (β = 0.17, p = 0.0003), which held when depression was run separately. Importantly, depression and SCT did not have overlapping items in this study. SCT and depression were strongly correlated (self-report r = 0.84, parent-report r = 0.78) in childhood and there is a degree of conceptual overlap between SCT and depression, with aspects of sleepiness, slowed behaviors, and apathy characterized in both constructs (Becker & Willcutt, 2019; Smith et al., 2019). However, there are also non-shared symptoms, including excessive daydreaming, losing train of thought, and staring blankly for SCT, and suicidal ideation, hopelessness, excessive guilt, and feelings of worthlessness for depression (American Psychological Association, 2013; Becker et al., 2016, 2020). Having shared symptoms between constructs is often the rule, not the exception, with psychopathology, particularly when both constructs are in the same higher-order domain (i.e., internalizing; Lahey et al., 2017). This may, however, increase multicollinearity, which can make variables statistically insignificant due to inflated standard errors (Daoud, 2017; Nimon et al., 2010). Thus, running predictor analyses separately for strongly correlated factors can show the true magnitude of the results (Daoud, 2017; Nimon et al., 2010). When run separately, each one standard deviation (SD) unit increase in self-reported SCT was associated on average with 0.26 SD higher depression scores and 0.12 SD higher inattentive scores in adulthood, while self-reported depression predicted 0.13 SD higher depression scores in adulthood. Interestingly, self-reported SCT had a higher association with later depression than childhood depressive symptoms.
The strong associations found in this study are consistent with the view that SCT is closely aligned with depression. When assessing for both SCT and depression, the current findings, however, suggest that SCT does not provide additional prediction of depression when regressed simultaneously with youth depressive symptoms. This is in contrast to the one longitudinal that found SCT in childhood (pre-school to second grade) uniquely predicted depression in adolescence (ninth grade; Becker et al., 2018). However, that study did not include childhood depression symptoms when regressing internalizing symptoms on SCT. The findings in the current study show the importance of simultaneous regression with both SCT and depressive symptoms when examining later internalizing psychopathology. Becker et al. (2019) suggested SCT may be a precursor to depression; however, this study only examined SCT and depression across a 6-month interval. There is a clear need for further longitudinal studies examining the relationship between SCT and depression.
Inattention
Despite SCT originating from ADHD research, more and more evidence has accumulated to conclude they are distinct, though related constructs. When accounting for FDR, SCT did not predict later inattentive symptoms when inattentive symptoms were simultaneously regressed on SCT and inattention, though when regressed separately, self-reported SCT predicted a 0.12 SD higher rate of inattentive symptoms in adulthood. This suggests a small, but significant association and continues to move the field towards the possibility of SCT as a distinct construct that may affect, but is not part of, ADHD symptoms. Very little work has examined what the underlying mechanisms are behind SCT, with one neuroimaging study finding SCT symptoms were more strongly associated with abnormal activity in posterior networks related to impaired orienting and shifting of attention, which is different than the frontal-parietal networks often evident in ADHD (Fassbender et al., 2015). This supports the differentiation between SCT and ADHD. In addition, Moruzzi et al. (2014) found that a small set of SCT items were genetically and environmentally correlated to ADHD symptom domains, but were distinct domains. From the little evidence gathered about the etiology of SCT, it is clear there are distinctions between SCT and ADHD as constructs, though further work is needed to not only understand these distinctions, but to also further understand SCT.
Hyperactivity-Impulsivity
Unsurprisingly, SCT in youth did not predict later hyperactivity-impulsivity symptoms in adulthood. This follows a long line of evidence showing that SCT and externalizing behaviors, like hyperactivity and impulsivity, are not associated and even negatively associated when accounting for inattentive symptoms (Becker et al., 2016; Lee et al., 2014). SCT was significantly correlated with hyperactivity-impulsivity, but this was a weak association for self-report of SCT. Surprisingly, parent-reported SCT and hyperactivity-impulsivity were moderately correlated (r = 0.40). Parent- and self-report of SCT are not invariant across reporters, and it has been suggested that parents may report more behavioral symptoms (e.g., sleepiness, slow behaviors) while self-report may better encapsulate the internalizing aspects (e.g., daydreaming, mental confusion, apathy; Smith et al., 2018). Still, it is unexpected that slow behaviors would be associated with hyperactivity-impulsivity and may be due to the large sample size and common method variance. Additionally, parent-reported SCT did not predict later hyperactivity-impulsivity, though the most consistent finding across analyses was that parent-reported hyperactivity-impulsivity in childhood and adolescence predicted higher levels of self-reported hyperactivity-impulsivity in adulthood despite the cross-rater aspect of these analyses.
SCT Through an Internalizing Lens
While the above data demonstrate that SCT in childhood is predictive of later depression, it does not provide evidence that SCT is a necessary additional construct in the internalizing domain independent of depression. Of course, the present work is not an ideal test for that. Given that homotypic continuity (construct predicting the same construct) is typically greater than heterotypic continuity (construct predicting a different construct; Lahey et al. 2014) it is not surprising that childhood depression was a better predictor of adult depression than childhood SCT. Currently SCT is not included in a diagnostic nosology and one might argue that the strong correlation between SCT and depression supports the belief that SCT may be part of the internalizing domain of psychology (Becker & Willcutt, 2019). SCT has also consistently been associated with inattention, which has been considered part of the externalizing domain (Lahey et al., 2017). Thus, SCT is an example of a symptom group that is positively associated with both internalizing and externalizing and may contribute to the frequently observed positive correlation between internalizing and externalizing disorders. The field of psychology had historically used categorical taxonomy to define and understand psychopathology, however, a growing body of research is suggesting that psychopathology should be understood in a dimensional, hierarchical approach (Kotov et al., 2017; Lahey et al., 2017). This work indicates that psychopathology is structured hierarchically with a general psychopathology factor that contributes to higher-order externalizing and internalizing dimensions that subdivide into more specific dimensions (Kotov et al., 2017; Lahey et al., 2017). Correlations between psychopathological constructs are due to the shared etiology of these dimensions or hierarchy of causal influences (Kotov et al., 2017; Lahey et al., 2017). This occurs both within and across internalizing and externalizing domains.
Previous work suggests that SCT may constitute a first-order dimension that could prove to be part of the higher order internalizing factor, as there are strong correlations between SCT and depression, as well as associations with internalizing behaviors such as withdrawal, rumination, suicidal ideation, emotion dysregulation, and isolation (Becker et al., 2017, 2018, 2020; Ward et al., 2019). Additionally, when controlling for ADHD, SCT is negatively associated with externalizing symptoms while ADHD inattentive symptoms are consistently associated with higher externalizing behaviors, further suggesting that the two constructs should be included on the internalizing and externalizing domains respectively (Becker & Barkley, 2018; Becker et al., 2016). When using the hierarchical model of psychopathology, correlations across domains is expected, though first-order dimensions within a higher-order factor have stronger correlations with each other (Lahey et al., 2017). This fits with the current findings, as SCT is strongly associated with depression and weakly to moderately associated with inattention and hyperactivity-impulsivity. As such, researchers should evaluate SCT within hierarchical models of psychopathology to understand whether SCT is indeed part of the internalizing domain of psychopathology and how it is associated within this framework with inattentive symptoms. The extent to which SCT shows unique predictive validity of other internalizing symptoms remains an open question.
Limitations and Future Directions
Several limitations should be considered. First, we did not collect parent-report of adult symptoms so could not run cross-rater analyses for self-reported SCT and depression. The estimates with self-reported SCT and depression found in this study may be partially inflated due to common method variance. This also may contribute to the fact that parent-reported inattentive symptoms in childhood did not predict self-reported inattentive symptoms in adulthood. The Wave two sample over-selected participants who had higher rates of psychopathology at Wave one. Therefore, it is possible that the psychopathology ratings at Wave two might have regressed toward the mean, possibly biasing the results. It is important to note, however, that the rates of ADHD (5.0%) and depression (11.4%) were both in the normative range. Additionally, as is common across psychopathology, SCT and depression share similar items. In this study, although items may be conceptually similar, SCT and depression did not have overlapping items, though the similarity in their conceptualization likely increase the associations between the factors. Further work should assess the association and distinction of SCT from low physiological arousal, negative affect, anhedonia, and related constructs to further understand the association and distinction between SCT and depression.
Importantly, although a strength of this study is the use of both parent- and self-report of SCT, future work should include teacher ratings of SCT as they may have a unique perspective and ability to assess how SCT affects behavior. For example, previous research has shown teacher-reported SCT was associated with shyness while parent- and self-reported SCT were not (Sáez et al., 2019). Shyness may be a behavior better captured in the school-setting as teachers often see children interacting with peers and is important to assess as this may be associated with withdrawal and depressive symptoms. The effects found in this sample are small, which we may have been able to detect due to our large sample size. To account for this, we adjusted for statistical significance at a 5% false discovery rate. Despite the smaller effect sizes, these findings are clinically meaningful and build upon prior research suggesting SCT may be more related to internalizing domains like depression than previously thought.
Twins tend to have somewhat higher levels of ADHD symptoms, possibly because of lower birth weights (Ehringer et al., 2006). However, correlations among symptoms of psychopathology are similar for twins and non-twins, suggesting a small difference between twins and singletons (Rutter & Redshaw, 1991). It is important to note the many future directions that are possible with twin data, including examination of shared and non-shared genetic and environmental variance associated with SCT. Becker et al., 2016 has called for further study of the etiology of SCT and the use of twin data in future studies would help with this call.
This was the first study to use an interview format to assess SCT symptoms. Although it is still unclear whether SCT should be considered a psychological disorder, there are many strengths to assessing psychological constructs through interview instead of a rating scale. Although this interview did not include all 13 items of SCT found in a recent metanalysis (Becker et al., 2016), we were able to include 11 of the 13 symptoms. Additionally, the interviewer was able to assure the respondent (parent or self) endorsed symptoms based on impairment, frequency, and severity.
Conclusions
This was the first study to examine whether SCT in childhood and adolescence predicted psychopathology in adulthood. As excepted, SCT and depression were strongly correlated concurrently in childhood and adolescence, with both separately predicting adulthood depressive symptoms. These findings are consistent with the hypothesis that SCT may be considered under the internalizing domain of psychology, but this has not been tested using hierarchical models of psychopathology. Further work is needed to assess etiology, impairment from a prospective perspective, prevention, and treatment of SCT. Importantly, these future studies need to do so with multiple reporters, particularly self-report if SCT is indeed an internalizing construct, and with a longitudinal perspective.
References
Abram, K. M., Zwecker, N. A., Welty, L. J., Hershfield, J. A., Dulcan, M. K., & Teplin, L. A. (2015). Comorbidity and continuity of psychiatric disorders in youth after detention: A prospective longitudinal study. Journal of the American Medical Association Psychiatry, 72, 84–93. https://doi.org/10.1001/jamapsychiatry.2014.1375.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Association.
Barkley, R. A. (2014). Sluggish cognitive tempo (concentration deficit disorder?): Current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42, 117–125. https://doi.org/10.1007/s10802-013-9824-y.
Becker, S. P., & Barkley, R. A. (2018). Sluggish cognitive tempo. In T. Banaschewski, D. Coghill, & A. Zuddas (Eds.), Oxford textbook of attention deficit hyperactivity disorder (pp. 147–153). Oxford: Oxford University Press.
Becker, S. P., & Willcutt, E. G. (2019). Advancing the study of sluggish cognitive tempo via DSM, RDoC, and hierarchical models of psychopathology. European Child & Adolescent Psychiatry, 28, 603–613.
Becker, S. P., Luebbe, A. M., Fite, P. J., Stoppelbein, L., & Greening, L. (2014). Sluggish cognitive tempo in psychiatrically hospitalized children: Factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. Journal of Abnormal Child Psychology, 42, 49–62.
Becker, S. P., Luebbe, A. M., & Joyce, A. M. (2015). The child concentration inventory (CCI): Initial validation of a child self-report measure of sluggish cognitive tempo. Psychological Assessment, 27, 1037–1052. https://doi.org/10.1037/pas0000083.
Becker, S. P., Leopold, D. R., Burns, G. L., Jarrett, M. A., Langberg, J. M., Marshall, S. A., McBurnett, K., Waschbusch, D. A., & Willcutt, E. G. (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 163–178.
Becker, S. P., Garner, A. A., Tamm, L., Antonini, T. N., & Epstein, J. N. (2017). Honing in on the social difficulties associated with sluggish cognitive tempo in children: Withdrawal, peer ignoring, and low engagement. Journal of Clinical Child Adolescent Psychology, 48, 228–237. https://doi.org/10.1080/15374416.2017.1286595.
Becker, S. P., Burns, G. L., Leopold, D. R., Olson, R. K., & Willcutt, E. G. (2018). Differential impact of trait sluggish cognitive tempo and ADHD inattention in early childhood on adolescent functioning. Journal of Child Psychology and Psychiatry, 59, 1094–1104.
Becker, S. P., Webb, K. L., & Dvorsky, M. R. (2019). Initial examination of the bidirectional associations between sluggish cognitive tempo and internalizing symptoms in children. Journal of Clinical Child & Adolescent Psychology. Advanced online publication. https://doi.org/10.1080/15374416.2019.1630836.
Becker, S. P., Burns, G. L., Smith, Z. R., & Langberg, J. M. (2020). Sluggish cognitive tempo in adolescents with and without ADHD: Differentiation from adolescent-reported ADHD inattention and unique associations with internalizing domains. Journal of Abnormal Child Psychology, 48, 391–406. https://doi.org/10.1007/s10802-019-00603-9.
Bernad, M., Servera, M., Becker, S. P., & Burns, G. L. (2016). Sluggish cognitive tempo and ADHD inattention as predictors of externalizing, internalizing, and impairment domains: A 2-year longitudinal study. Journal of Abnormal Child Psychology, 44, 771–785. https://doi.org/10.1007/s10802-015-0066-z.
Carlson, C. L., Lahey, B. B., & Neeper, R. (1986). Direct assessment of the cognitive correlates of attention deficit disorders with and without hyperactivity. Journal of Behavioral Assessment and Psychopathology, 8, 69–86.
Daoud, J. (2017). Multicollinearity and regression analysis. Journal of Physics: Conference Series, 949, 012009. https://doi.org/10.1088/1742-6596/949/1/012009.
Ehringer, M. A., Rhee, S. H., Young, S., Corley, R., & Hewitt, J. K. (2006). Genetic and environmental contributions to common psychopathologies of childhood and adolescence: A study of twins and their siblings. Journal of Abnormal Child Psychology, 34, 1–17.
Fassbender, C., Krafft, C. E., & Schweitzer, J. B. (2015). Differentiating SCT and inattentive symptoms of ADHD using fMRI measures of cognitive control. NeuroImage: Clinical, 8, 390–397.
Holdaway, A. S., & Becker, S. P. (2018). Sluggish cognitive tempo and student-teacher relationship quality: Short-term longitudinal and concurrent associations. School Psychology Quarterly, 33, 537–546.
Korn, E. L., & Graubard, B. I. (1999). Analysis of health surveys. New York: Wiley. https://doi.org/10.1002/9781118032619.
Kotov, R., Krueger, R. F., Watson, D., Achenbach, T. M., Althoff, R. R., Bagby, R. M., Brown, T. A., Carpenter, W. T., Caspi, A., Clark, L. A., Eaton, N. R., Forbes, M. K., Forbush, K. T., Goldberg, D., Hasin, D., Hyman, S. E., Ivanova, M. Y., Lynam, D. R., Markon, K., Miller, J. D., Moffitt, T. E., Morey, L. C., Mullins-Sweatt, S. N., Ormel, J., Patrick, C. J., Regier, D. A., Rescorla, L., Ruggero, C. J., Samuel, D. B., Sellbom, M., Simms, L. J., Skodol, A. E., Slade, T., South, S. C., Tackett, J. L., Waldman, I. D., Waszczuk, M. A., Widiger, T. A., Wright, A. G. C., & Zimmerman, M. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. https://doi.org/10.1037/abn0000258.
Laceulle, O. M., Vollebergh, W. A. M., & Ormel, J. (2015). The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS study. Clinical Psychological Science, 3, 850–860.
Lahey, B. B., Applegate, B., Waldman, I. D., Loft, J. D., Hankin, B. L., & Rick, J. (2004). The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology, 113, 358–385. https://doi.org/10.1037/0021-843X.113.3.358.
Lahey, B. B., Rathouz, P. J., Van Hulle, C., Urbano, R. C., Krueger, R. F., et al. (2008). Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology, 36, 187–206.
Lahey, B. B., Zald, D. H., Hakes, J. K., Krueger, R. F., Rathouz, P. J. (2014). Patterns of Heterotypic Continuity Associated With the Cross-Sectional Correlational Structure of Prevalent Mental Disorders in Adults. JAMA Psychiatry, 71, 989
Lahey, B. B., Krueger, R. F., Rathouz, P. J., Waldman, I. D., & Zald, D. H. (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 2, 142–186.
Lee, S. Y., Burns, G. L., Snell, J., & McBurnett, K. (2014). Validity of sluggish cognitive tempo symptom dimension in children: Sluggish cognitive tempo and ADHD-inattention as distinct symptom dimensions. Journal of Abnormal Child Psychology, 42, 7–19.
McBurnett, K., Villodas, M., Burns, G. L., Hinshaw, S. P., Beaulieu, A., & Pfiffner, L. J. (2014). Structure and validity of sluggish cognitive tempo using an expanded item pool in children with attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 42, 37–48. https://doi.org/10.1007/s10802-013-9801-5.
Moruzzi, S., Rijsdijk, F., & Battaglia, M. (2014). A twin study of the relationships among inattention, hyperactivity-impulsivity, and sluggish cognitive tempo problems. Journal of Abnormal Child Psychology, 42, 63–75.
Nimon, K., Henson, R., & Gates, M. (2010). Revisiting interpretation of canonical correlation analysis: A tutorial and demonstration of canonical commonality analysis. Multivariate Behavioral Research, 45, 702–724.
Noordhof, A., Krueger, R. F., Ormel, J., Oldehinkel, A. J., & Hartmanm, C. A. (2015). Integrating autism-related symptoms into the dimensional internalizing and externalizing model of psychopathology. The TRAILS study. Journal of Abnormal Child Psychology, 43, 577–587. https://doi.org/10.1007/s10802-014-9923-4.
Penny, A. M., Waschbusch, D. A., Klein, R. M., Corkum, P., Eskes, G. (2009). Developing a measure of sluggish cognitive tempo for children: Content validity, factor structure, and reliability. Psychological Assessment, 21, 3, 380–389
Rutter, M., & Redshaw, J. (1991). Growing up as a twin: Twin–singleton differences in psychological development. Journal of Child Psychology and Psychiatry, 32, 885–895.
Sáez, B., Servera, M., Burns, G. L., & Becker, S. P. (2019). Advancing the multi-informant assessment of sluggish cognitive tempo: Child self-report in relation to parent and teacher ratings of SCT and impairment. Journal of Abnormal Child Psychology, 47, 35–46.
Servera, M., Bernad, M. D. R., Carrillo, J. M., Collado, S., Burns, L. G. (2015). Longitudinal Correlates of Sluggish Cognitive Tempo and ADHD-Inattention Symptom Dimensions with Spanish Children. Journal of Clinical Child & Adolescent Psychology, 45, 632–641.
Servera, M., Sáez, B., Burns, G. L., & Becker, S. P. (2018). Clinical differentiation of sluggish cognitive tempo and attention-deficit/hyperactivity disorder in children. Journal of Abnormal Psychology, 127, 818–829. https://doi.org/10.1037/abn0000375.
Shaffer, D., Fisher, P., Lucas, C. P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 28–38. https://doi.org/10.1097/00004583-200001000-00014.
Shaffer, D., Fisher, P., Piacentini, J. C., & Lucas, C. (2008). Young adult diagnostic interview schedule for children. New York: Columbia University.
Smith, Z. R., & Langberg, J. M. (2017). Predicting academic impairment and internalizing psychopathology using a multidimensional framework of sluggish cognitive tempo with parent- and adolescent-report. Journal of European Child and Adolescent Psychiatry, 27, 1141–1150. https://doi.org/10.1007/s00787-017-1003-1.
Smith, Z. R., Becker, S. P., Garner, A. A., Rudolph, C. W., Molitor, S. J., Oddo, L. E., & Langberg, J. M. (2018). Evaluating the structure of sluggish cognitive tempo using confirmatory factor analytic and bifactor modeling with parent and youth ratings. Assessment, 25, 99–111.
Smith, Z. R., Eadeh, H. M., Breaux, R. P., & Langberg, J. M. (2019). Sleepy, sluggish, worried, or down? The distinction between self-reported sluggish cognitive tempo, daytime sleepiness, and internalizing symptoms in youth with attention-deficit/hyperactivity disorder. Psychological Assessment, 31, 365–375. https://doi.org/10.1037/pas0000671.
Ward, A. R., Sibley, M. H., Musser, E. D., Campez, M., Bubnik-Harrison, M. G., Meinzer, M. C., & Yeguez, C. E. (2019). Relational impairments, sluggish cognitive tempo, and severe inattention are associated with elevated self-rated depressive symptoms in adolescents with ADHD. ADHD Attention Deficit and Hyperactivity Disorders, 11, 289–298.
Willcutt, E. G., Chhabildas, N., Kinnear, M., DeFries, J. C., & Pennington, B. F. (2014). The internal and external validity of sluggish cognitive tempo and its relation with DSM-IV ADHD. Journal of Abnormal Child Psychology, 42, 21–35.
Witkiewitz, K., King, K., McMahon, R. J., Wu, J., Luk, J., Bierman, K. L., et al. (2013). Evidence for a multi-dimensional latent structural model of externalizing disorders. Journal of Abnormal Child Psychology, 41, 223–237. https://doi.org/10.1007/s10802-012-9674-z.
Funding
Supported by Grant MH098098 from the National Institute of Mental Health and CTSA Grants UL1-TR000445 and UL1-TR000430.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smith, Z.R., Zald, D.H. & Lahey, B.B. Sluggish Cognitive Tempo and Depressive Symptoms in Children and Adolescents Predict Adulthood Psychopathology. J Abnorm Child Psychol 48, 1591–1601 (2020). https://doi.org/10.1007/s10802-020-00692-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-020-00692-x