Abstract
Sluggish Cognitive Tempo (SCT) has been defined by a constellation of caregiver-reported symptoms that includes daydreaming, difficulty initiating and sustaining effort, lethargy, and physical underactivity. These symptoms have been observed in both typically developing children and in some children with Attention-Deficit/Hyperactivity Disorder (ADHD)—especially those with the predominantly inattentive presentation. Symptoms of SCT (typically identified via rating scales) appear separable from DSM inattentive ADHD symptoms, but have also been associated with internalizing symptoms. To date, however, few studies have examined associations among ratings of SCT and speeded performance-based measures. The present study examined associations among SCT, processing speed, and internalizing symptoms in a sample of 566 clinically referred children (65% male), while also considering how these associations change with age. Findings revealed small but significant age-related differences in the strength of associations between the “Daydreamy” element of SCT and processing speed (as measured by the WISC-IV Processing Speed Index—PSI), with stronger associations observed in younger children. Importantly, this difference in strength of association was not accounted for by the change in WISC-IV test forms for PSI subtests between 6–7 year-olds and 8–16 year-olds. Conversely, the association between SCT and internalizing symptoms remained generally consistent across the age range. Findings contribute to further characterization of the “slowness” of responding seen in SCT and may have implications for behavioral intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sluggish Cognitive Tempo (SCT) has been defined by a constellation of caregiver-reported symptoms that includes daydreaming, difficulty initiating and sustaining effort, lethargy, and physical underactivity (Barkley 2012; Becker and Langberg 2013; Carlson and Mann 2002). Youth with SCT are typically described as “slow moving” and “under-responsive,” characteristics of the SCT construct that appear to be separable from both inattention and other characteristics of SCT, such as daydreaminess and low initiation/poor persistence (Hartman et al. 2004; Jacobson et al. 2012). Relative to typically-developing peers, youth with ADHD—particularly the inattentive or combined presentations—have been found to demonstrate slower cognitive processing speed (Chhabildas et al. 2001; Jacobson et al. 2011; Rucklidge and Tannock 2002; Willcutt et al. 2005) and slowed motor reaction time (Lee et al. 2012; Rucklidge and Tannock 2002; Shanahan et al. 2006; Wodka et al. 2007). As approximately 30–60% of youth with ADHD may also exhibit high levels of SCT (Barkley 2012; Garner et al. 2010; Skirbekk et al. 2011), the hypomotoric presentation seen in youth with SCT may, at least in part, contribute to this pattern of slower processing speed and reaction time. It is not yet clear, however, whether the slowed processing in SCT reflects slowed motor responding or slowed cognitive processing (e.g., “bradyphrenia”), or a combination. For the purposes of this paper, we will use the term “processing speed” to reflect the measured speed of performance, acknowledging that this generally includes both cognitive processing speed and motor response or performance speed.
The limited initial work examining neuropsychological correlates of caregiver-reported SCT has been inconsistent. An investigation in 140 Puerto Rican children recruited for ADHD symptomatology found no association between parent-rated SCT severity and performance-based processing speed, as measured by a rapid naming task (Bauermeister et al. 2012), nor was SCT significantly associated with other performance-based measures of executive control, including working memory, interference control, or problem-solving skills. Conversely, other researchers (e.g., Willcutt et al. 2014) have found that, after controlling for inattentive and hyperactive symptoms, caregiver ratings of SCT were significantly associated with weakness in sustained attention (i.e., omissions) on a continuous performance task (CPT), but not with naming speed, a composited processing speed score, or response inhibition (CPT commission errors). Notably, however, SCT in these studies was represented by a limited item pool, with either four (Bauermeister et al. 2012) or six (Willcutt et al. 2014) items. In many recent studies, investigators have relied on more comprehensive measures of SCT consisting of 14 (Penny et al. 2009) up to 44 (McBurnett et al. 2014) items. Thus, the construct of SCT may have been only partially characterized in these initial investigations, while more comprehensive characterization of SCT (beyond rating scales) may yield a differing pattern of associations. When considering expanding the assessment of SCT to performance-based measures, it is important to note that identifying meaningful associations between parent ratings and performance-based measures of a similar construct has been challenging, a fact highlighted by investigations of executive function (e.g., McAuley et al. 2010). Further examination of this putative association between SCT and processing speed is needed to clarify whether youth rated as showing greater SCT symptoms are also more likely to demonstrate slower processing or more delayed responses on performance-based measures.
SCT and Internalizing Symptoms
Given the relatively apathetic and lethargic presentation characteristic of youth with high levels of SCT, SCT symptoms have also been hypothesized to overlap with symptoms of internalizing disorders. Although some data suggest SCT may be more closely associated with inattention symptoms than with internalizing psychopathology (e.g., Lahey et al. 2004), there is growing evidence supporting the SCT-internalizing association, with a recent meta-analysis suggesting a potentially stronger association between SCT and depressive symptoms than anxiety symptoms (Becker et al. 2016). Specifically, children with higher levels of SCT symptomatology have been found to show greater unhappiness, withdrawal, anxiety/depression, and social dysfunction relative to children with lower levels of SCT symptomatology, suggesting a link between SCT and mood symptoms (Becker and Langberg 2013; Carlson and Mann 2002; Hartman et al. 2004). After controlling for symptoms of ADHD (Bauermeister et al. 2012) and Conduct Disorder (Becker and Langberg 2013), ratings of SCT remained significantly associated with internalizing symptoms in youth with ADHD. Clinically-referred children with comorbid ADHD and anxiety were found to be more likely to display SCT than those with ADHD alone (Skirbekk et al. 2011). The strength of the SCT-internalizing symptoms association has been somewhat variable across studies, with somewhat stronger correlations in non-referred versus clinically-referred samples. In a clinical sample, Garner et al. (2010) reported correlations of 0.28 and 0.20 between parent-reported SCT symptoms and ratings of anxiety/depression and aggression, respectively, whereas the bivariate SCT-internalizing association was stronger within a sample of non-referred youth (e.g., r = 0.55, and r p = 0.31 after controlling for inattention; Penny et al. 2009).
Growing evidence also suggests that observable ADHD symptomatology appears to shift as children age (Lahey et al. 2005), with fewer adolescents exhibiting primarily hyperactive symptoms relative to younger children. At the same time, data suggest a greater likelihood of preadolescent or adolescent youth presenting with mood symptomatology, relative to younger children (Kessler et al. 2001). Recent evidence from a 10-year period in a population-based sample found latent stability of the SCT construct over this period and suggested that mean levels of parent-reported SCT symptoms may actually increase over time (Leopold et al. 2016). As such, it is important to consider the role of age when considering the relationships between SCT and internalizing behaviors. Although the relation between SCT and internalizing symptoms appears to be present across both community and clinical samples, no published studies have examined the moderating effect of age or examined whether SCT is more common in younger versus older children, and the implications of age for associations between SCT, speed, and anxiety or depressive symptoms.
The present study examined the associations between SCT, processing speed, and internalizing symptoms (anxiety, depression), while also considering how these relationships may change with age. We hypothesized that those elements of SCT previously shown to be most separable from ADHD in other samples would be separable from ADHD-related inattention, and that those separable components of SCT would be associated with lower scores on performance-based measures of processing speed. In addition, we hypothesized that the relationship between SCT and internalizing symptoms (anxiety, depression) would be moderated by age, with different patterns of association (i.e., likely stronger associations) in older children, compared to those observed in younger children.
Methods
Procedures
As part of routine clinical practice at a large outpatient neuropsychology assessment center, parents of children referred to the clinic are asked to complete a set of behavioral rating scales including the Penny et al. (2009) SCT Scale, the ADHD Rating Scale-IV (ADHDRS; DuPaul et al. 1998), and portions of the Vanderbilt Parent Rating Scale (VPRS; Wolraich et al. 2003) through a secure survey web link prior to the assessment appointment. All data are then entered into a clinical database. Data from routine clinical assessments are also entered into this database by department clinicians via the hospital electronic health record, and these data are securely maintained by the hospital’s Information Systems Department. Data were collected from unique patient visits over a 2-year period.
Following approval from the hospital’s Institutional Review Board, the de-identified clinical database was queried, and a limited dataset was constructed of patients between the ages of 6 and 16 years of age for whom valid scores were available on the Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV) Processing Speed Index (PSI) and for whom parent ratings were available on the ADHDRS, the SCT Scale, and the VPRS. There were no exclusionary criteria beyond complete data on these four measures.
Measures
Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV, Wechsler 2004)
The WISC-IV is a frequently administered measure of intellectual ability. In addition to providing a Full Scale IQ (FSIQ), this measure provides four Index scores: Verbal Comprehension, Perceptual Reasoning, Working Memory, and Processing Speed. Internal consistency for the Index scores and FSIQ is good (Cronbach’s alpha [r α ] ranging from 0.81 to 0.95), with good test-retest reliability (r from 0.86 to 0.93). The Processing Speed Index (PSI) is also a reliable measure across the test-specific age span (r α ranging from 0.81 to 0.91), with a corrected test-retest reliability estimate across age groups of 0.86.
Sluggish Cognitive Tempo (SCT) Scale (Penny et al. 2009)
The SCT Scale is a 14-item teacher- or parent-report rating scale of symptoms that correspond to the SCT construct. For the purposes of the present study, only the parent report version was used. Ratings are made on a 4-point scale (0 = Never or Rarely; 1 = Sometimes; 2 = Often; 3 = Very Often). The scale was originally normed on a Canadian sample of school children, and data from parent reports in this sample demonstrated adequate internal consistency. Test-retest reliability estimates for the parent-report version were adequate (ranging from 0.70 to 0.87). Total composite score for the SCT scale is the sum of the ratings on all 14 items. In the current sample, internal consistency for the SCT scale was very good (r α = 0.88).
ADHD Rating Scale-IV, Home Version (ADHDRS; DuPaul et al. 1998)
The ADHDRS is an 18-item measure, reflecting the DSM-IV ADHD diagnostic criteria. The scale is designed to be completed by parents or teachers, although for the purposes of the current study, only the home (parent) version was used. Item content reflects DSM-IV diagnostic criteria and items were rated based on the child’s behavior over the past 6 months, using a 4-point scale (0 = Not at all; 1 = Sometimes; 2 = Often; 3 = Very Much). Subscales correspond to the DSM-IV Inattentive and Hyperactive/Impulsive criteria. Total subscale scores were obtained by adding item ratings (range: 0–27 for each). The ADHDRS has been shown to demonstrate adequate reliability and validity (DuPaul et al. 1998); internal consistency estimates for the parent-report version ranged from 0.86 for the Inattention scale to 0.88 for the Hyperactivity/Impulsivity scale, with test-retest reliability over short periods of time ranging from 0.78 for Inattention to 0.86 for Hyperactivity/Impulsivity. In the current sample, internal consistency for the ADHDRS subscales was excellent (Inattention r α = 0.90; Hyperactivity/Impulsivity r α = 0.90).
The Vanderbilt Parent Rating Scale (VPRS, Wolraich et al. 2003)
The VPRS is a parent report questionnaire designed to assess a variety of symptoms of childhood behavioral disorders; for the purposes of the present study, only the items related to internalizing symptoms were included. Specifically, the seven items designed to assess for internalizing behavior symptoms suggestive of anxiety or depression were included to provide an estimate of internalizing symptoms (e.g., is fearful, anxious, or worried; feels worthless or inferior; is sad, unhappy, or depressed). Items are rated on a 4-point scale (0 = Never; 1 = Occasionally; 2 = Often; 3 = Very Often). The anxiety/depression composite score is the sum of ratings on the three anxiety symptom items (range = 0 to 9) and the four items assessing depressive symptomatology (range = 0 to 12). In this sample, internal consistency for the Vanderbilt Anxiety/Depression composite was good (r α = 0.87).
Analysis Plan
First, associations between the primary variables of interest (age, SCT, internalizing symptoms) were examined using zero-order Pearson correlations. Second, an exploratory factor analysis (principal axis factoring with Promax rotation) was conducted including both the SCT and the inattention items of the ADHDRS, in order to identify the elements of SCT that are most unique from inattention in this clinical sample. Third, age, SCT, and the age-by-SCT interaction were then entered into a series of linear regression equations in order to determine the strongest predictors of processing speed and internalizing symptoms, and whether/how these associations are moderated by age. In these analyses, two age groups were used: younger (ages 6–9 years) and older (ages 10–16 years). Given concerns for multicollinearity, a separate set of analyses were run covarying for inattention symptom severity. When age-by-SCT interactions were observed, separate analyses of simple slopes and the associations in younger (6–9 years) and older (10–16 years) groups were completed, and compared using Fisher’s r-to-z transformations. Age 10 years as selected at the split point for three reasons: first, this provided an essentially median split, allowing for fairly even groups in each subsample; second, a split at 10 years allowed (generally) for a pre-post-pubertal split; and third, this cut point has clinical significance in that children under 10 are elementary age and those over 10 are moving into middle school and beyond, which is developmentally and clinically relevant. A secondary set of analyses were run examining age as a continuous variable.
Results
Participants
The total sample included 566 children (M Age = 10.37, SD = 2.76) referred for psychological or neuropsychological assessment in a large outpatient neuropsychology clinic (see Table 1). The majority of children were male (65.0%) and Caucasian (57.8%); 23.6% were African American, 5.7% were multi-racial, 3.4% were Asian American, and 6.8% were of unknown racial background, while 1.3% were reportedly of Hispanic ethnicity. With regard to parent characteristics, 25.6% of caregivers completing the parent-report measures had completed high school and/or at least some college coursework, 0.7% earned less than a high school education, 4.4% had completed an associate’s degree or had some type of vocational training, 32.2% graduated from college, and 25.2% earned a graduate or post graduate degree (11.8% of the sample did not report parent education level). With regard to clinical diagnoses, approximately 82% were assigned mental health diagnoses, including ADHD, disruptive behavior disorders, mood, anxiety, and learning disorders. Approximately 18% were evaluated secondary to medical diagnoses, including epilepsy, oncologic conditions, brain injury, neurofibromatosis, and spina bifida. Overall, the sample was generally of average intellectual functioning, as measured by untimed verbal reasoning ability (Table 1).
Associations Among Age, SCT, PSI, and Mood
Parent ratings of SCT (SCT Total score) were more strongly associated with ratings of inattentive symptoms, r = 0.77, p < 0.001, than hyperactive/impulsive symptoms, r = 0.33, p < 0.001; r-to-z, p < 0.001 (Table 2). SCT Total was also significantly inversely associated with performance-based measures of processing speed (WISC-IV PSI; r = −0.21, p < 0.001—such that greater SCT rating was associated with poorer performance on PSI)—and positively associated with ratings of internalizing symptomatology, including both anxiety and depression (greater SCT associated with greater anxiety and depression). In addition, parent ratings of SCT were modestly correlated with age, with older children more likely to display SCT symptoms, r = 0.20, p < 0.001.
Determining the Unique Components of SCT
To determine unique components of SCT (i.e., those that have least overlap with the inattentive symptoms of ADHD), all 14 items from the SCT scale and the nine inattention items from the ADHDRS were entered into an exploratory factor analysis, using principal axis factoring with Promax rotation. Criteria for determining the number of factors included eigenvalues >1.0 and examination of the scree plots. In terms of the item-factor loadings (as presented in Table 3), factor loadings <0.20 were suppressed for clarity and only a few cross loadings higher than this threshold were observed (and presented in the table). The analysis produced four primary factors accounting for 58% of the total variance. Eight of the nine inattention items loaded on Factor 1 (40.2% total variance) along with three of the SCT items assessing low initiation/persistence (i.e., lacks initiative, effort fades quickly, and appears unmotivated). All of the SCT items describing the “sleepy/sluggish” presentation loaded uniquely on Factor 2 (10.2% total variance). The “daydreamy” SCT items loaded on Factor 3 (4.4% total variance) along with the remaining one inattention item from the ADHDRS (i.e., is forgetful). Notably, this item also showed a substantial cross loading on Factor 1 (i.e., the DSM inattention factor). Finally, the two remaining SCT items (“low initiation/persistence”) loaded uniquely on Factor 4 (3.1% total variance), representing a construct related to slower speed of performance (i.e., needs extra time, slow completing tasks). Given the separation of variance associated with inattention symptoms, Factor 2 (Sleepy/Sluggish), Factor 3 (Daydreamy), and Factor 4 (Low Initiation) were used as variables in subsequent analyses.
Age as a Potential Moderator of Associations Between SCT and Processing Speed
To determine the associations between unique elements of SCT (i.e., those factors that diverge from inattentive symptoms in this sample) and PSI, a series of linear regression models were employed, using age group, SCT (i.e., Factors 2, 3, 4), and the age-by-SCT interaction as independent variables, and WISC-IV PSI as the dependent variable (Table 4).
There was a significant effect for age group on PSI (i.e., younger children showing higher PSI than older children; p < 0.001).
For Factor 2 (Sleepy/Sluggish), neither the effect for SCT, p = 0.195, nor the age group-by-SCT interaction, p = 0.458, were significant. This pattern of associations remained when inattention severity was included in the model.
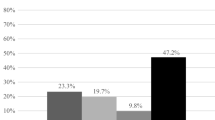
For Factor 3 (Daydreamy), the effect of SCT, p = 0.006, and the age group-by-SCT interaction, p = 0.005, were both significant predictors of PSI. The interaction remained significant when inattention was included in the model (see Table 4). The interaction effect was explored by examining associations in the younger and older groups separately. The association between SCT and PSI was larger and statistically significant in the younger group, r = −0.23, p < 0.001, compared to the older group, r = −0.01, p = 0.837, and the difference (one-tailed) between the correlations, r-to-z = 2.60, p = 0.0047, was also significant (Fig. 1). In the younger group, higher ratings of Daydreamy SCT were associated with slower processing speed scores. Examination of simple slopes across the age distribution confirmed the differential impact of Daydreamy SCT in younger, t = −2.653, p = 0.008, but not older, t = -1.085, p = 0.278, children.
Given that children 6–7 years old are administered different test forms for the WISC-IV subtests comprising the Processing Speed Index (Coding, Symbol Search) than children ages 8–16, an additional analysis, comparing associations between SCT and PSI for younger (ages 6–7) and older (ages 8-9) children in the (overall) younger age group, was employed to determine whether the significant associations observed were being driven primarily by the use of a different test form in the 6–7 year-olds. The association between SCT and PSI was actually significantly higher (one-tailed) in the 8–9 year-old group, r = −0.33; n = 138, than in the 6–7 year old group, r = −0.11; n = 137; r-to-z = 1.93, p = 0.027, suggesting that the significant association between SCT and PSI observed in the (overall) younger age group (6–9 year olds) was not being driven solely by those children who had been given Form A of Symbol Search and Coding.
For Factor 4 (Low Initiation), there was a significant main effect for SCT (i.e., higher ratings of SCT predicting lower PSI scores; p < 0.001); however, the age group-by-SCT interaction was not significant, p = 0.168. This pattern remained the same when inattention severity was included in the model.
Age as a Potential Moderator of Associations Between SCT and Internalizing symptoms
To determine the associations between unique elements of SCT (i.e., those factors that diverge from inattentive symptoms) and parent reported anxiety and depression symptoms, a series of linear regression models were employed, using age, SCT (i.e., Factors 2, 3, 4), and the age-by-SCT interaction as independent variables, and the VPRS Anxiety/Depression composite score as the dependent variable. The association between age group and VPRS Anxiety/Depression approached significance, p = 0.060, with a significant association when age was examined continuously (Table 4). For Factor 2 (Sleepy Sluggish), the effect of SCT was significant (i.e., greater report of SCT was associated with greater internalizing symptoms; p < 0.001), but the age group-by-SCT interaction was not, p = 0.782. For Factor 3 (Daydreamy), a very similar pattern emerged, such that the main effect of SCT was significant (i.e., greater report of SCT was associated with greater internalizing symptoms; p < 0.001), but not the age group-by-SCT interaction, p = 0.993. Likewise, for Factor 4 (Low Initiation), the main effect for SCT, p = 0.004, was significant but not the age group-by-SCT interaction, p = 0.732. In each case, the pattern was consistent when inattention severity was included in the model.
Discussion
In this clinically referred sample, there were age-related differences in the strength of association between parent ratings of the “Daydreamy” component of SCT (which is statistically unique from parent-rated DSM inattentive ADHD symptoms) and processing speed, with a stronger association observed in younger children. For this element of SCT both age and the age-by-SCT interaction were significantly associated with performance on WISC-IV PSI, such that younger children showed a significantly stronger association than older children for Daydreamy SCT (Factor 3) with higher ratings of Daydreamy SCT associated with slower processing speed. Importantly, this difference in strength of association was not accounted for by inattention severity or the change in measurement format between younger and older children on the WISC-IV, suggesting that younger children with Daydreamy SCT symptoms may manifest graphomotor slowing more than older children rated similarly in terms of SCT symptoms. Unlike processing speed, the association between SCT and internalizing symptoms appeared consistent across the age range, even when inattention severity was included in the model, for all three SCT factors.
A growing body of evidence suggests that SCT is significantly associated with both academic and functional impairment (Barkley 2012; Becker and Langberg 2013), as well as the lethargy and low initiation thought to be characteristic of depression. Few published studies, however, have investigated whether behavioral ratings of SCT provided by caregivers are also predictive of actual “slowing” assessed directly through performance-based measures and these findings have been inconclusive. Moreover, the moderating effects of age (known to be significant in ADHD) have not been examined in SCT. Our results indicate that SCT ratings are predictive of not only internalizing symptoms, but also slowed processing speed, and that the association between SCT symptoms and PSI may be stronger in younger (elementary school age) children.
Treatment of ADHD symptoms with stimulant medication is recommended by the AACAP (Pliszka 2007); however, response rates in ADHD are incomplete: 25–35% of individuals tend not to respond to initial treatment with stimulant medication (Pliszka 2007) and a crossover trial found that 22% did not respond to either stimulant or a non-stimulant treatment (Newcorn et al. 2008). Some data suggest this finding may be particularly true of the inattentive presentation, as up to one-third of youth with ADHD-I may not respond to stimulant medications (Barkley et al. 1991). SCT, alone or in conjunction with ADHD, appears to convey significant risk for impairment (Barkley 2012). Thus appropriate identification and clarification of co-occurring risks (e.g., low mood, slow motor speed) associated with SCT may provide appropriate targets for intervention or accommodation. Additionally, some emerging evidence suggests that children with SCT may respond to treatment with non-stimulant medication (e.g., atomoxetine; Wietecha et al. 2013); therefore, accurately identifying those children with ADHD plus SCT may be important for determining the type of medication intervention. The present data add to the growing literature on SCT by first, adding to the evidence for performance-based impact of SCT on processing speed, and second, identifying age-related differences in the association with the Daydreamy component of SCT, which is consistently separable from inattention symptomatology. Additionally, secondary analyses suggest that the pattern of findings is not due solely to the multicollinearity between SCT and inattention symptoms. Consideration of age-related changes and careful assessment of both SCT and associated internalizing symptomatology is important to ensure effective treatment and interventions for children with ADHD.
The differences in the pattern of associations across the age span examined between SCT and processing speed versus SCT and affective symptoms may reflect differences in the biological bases of these behaviors in younger children versus adolescents. Specifically, it may be that earlier motor response control is very closely tied to affective control, due to overlap in recruitment of similar brain regions for both (e.g., basal ganglia, cingulate; Mogenson et al. 1980; Shackman et al. 2011); whereas in older children (pubertal and post-pubertal), greater frontal lobe recruitment may allow for more differentiation of these regulatory mechanisms (Yurgelun-Todd 2007). It may be that this difference in neurobiological substrates underlies the age difference in the association between SCT and graphomotor processing speed. Alternatively, it may be that the observed age difference is simply a function of the referred nature of the sample in that the older children show greater impairment in processing speed relative to the younger children. Additionally, it is important to note that these findings examine two separate patterns of associations: parent ratings compared to parent ratings (SCT-internalizing symptoms) versus parent ratings compared to performance (SCT-PSI). As such, method variance may also play a role in interpretation of the pattern of findings. Further investigations will help to elucidate the nature of the observed differences. Furthermore, additional work will be needed to identify whether there is a difference in the consistency of motor slowing in youth with SCT, who may be consistently slow in responding as compared with youth with ADHD who have been shown to be slow but highly variable in responding (Jacobson et al. 2013).
Although these data provide a first examination of age-related differences in the SCT-motor processing speed association in a large sample, further work will be needed to clarify the nature of these age-related differences in children’s presentations with SCT. Limitations of the study include use of a mixed diagnostic/referred sample, in which incidence of anxiety and depression may be greater than within a community sample. In addition, medication status and past medical history were not available for review or inclusion in analyses. Furthermore, given the increased incidence of slower processing in a variety of developmental and medical conditions, the referred nature of the sample may also convey greater risk for slowed processing relative to a community sample (as suggested by the average mean VCI score, but below average mean PSI score of the overall sample). Also, given the age range of the sample and inclusion of younger children for whom self-report of symptoms has been shown to be less reliable (Ebesutani et al. 2011), particularly for specific aspects of internalizing symptoms, anxiety and depression symptoms were assessed via parent report only. However, we acknowledge that parent ratings provide a limited measure of such symptoms and, in many cases, these symptoms might be more comprehensively assessed by including self-report. Additional work should examine whether these associations remain using self-reports of mood and anxiety symptomatology. Overall, however, these data provide initial evidence for associations between ratings of SCT and performance-based motor slowing as well as for age-related differences in this SCT-motor processing speed association, which may offer targets for intervention in youth with SCT.
References
Barkley, R. A. (2012). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. Journal of Clinical Child and Adolescent Psychology, 42, 161–73.
Barkley, R. A., DuPaul, G. J., & McMurray, M. B. (1991). Attention deficit disorder with and without hyperactivity: clinical response to three dose levels of methylphenidate. Pediatrics, 87, 519–531.
Bauermeister, J. J., Barkley, R. A., Bauermeister, J. A., Martinez, J. V., & McBurnett, K. (2012). Validity of the sluggish cognitive tempo, inattention, and hyperactivity symptom dimensions: neuropsychological and psychosocial correlates. Journal of Abnormal Child Psychology, 43, 683–697.
Becker, S. P., & Langberg, J. M. (2013). Sluggish cognitive tempo among young adolescents with ADHD: relations to mental health, academic, and social functioning. Journal of Attention Disorders, 17, 681–689.
Becker, S. P., Leopold, D. R., Burns, G. L., Jarrett, M. A., Langberg, J. M., Marshall, S. A., & Willcutt, E. G. (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: a meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 163–178.
Carlson, C. L., & Mann, M. (2002). Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. Journal of Clinical Child and Adolescent Psychology, 31, 123–129.
Chhabildas, N., Pennington, B. F., & Willcutt, E. G. (2001). A comparison of the neuropsychological profiles of the DSM-IV subtypes of ADHD. Journal of Abnormal Child Psychology, 29, 529–540.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (1998). ADHD rating scale-IV. New York: Guilford Press.
Ebesutani, C., Bernstein, A., Martinez, J. I., Chorpita, B. F., & Weisz, J. R. (2011). The youth self report: applicability and validity across younger and older youths. Journal of Clinical Child and Adolescent Psychology, 40, 338–346.
Garner, A. A., Mrug, S., Hodgens, B., & Patterson, C. (2010). Do symptoms of sluggish cognitive tempo in children with ADHD symptoms represent comorbid internalizing difficulties? Journal of Attention Disorders, 17, 510–518.
Hartman, C. A., Willcutt, E. G., Rhee, S. H., & Pennington, B. F. (2004). The relation between sluggish cognitive tempo and DSM-IV ADHD. Journal of Abnormal Child Psychology, 32, 491–503.
Jacobson, L. A., Ryan, M., Martin, R. B., Ewen, J., Mostosfky, S. H., & Mahone, E. M. (2011). Working memory influences processing speed and reading fluency in ADHD. Child Neuropsychology, 17, 209–24.
Jacobson, L. A., Murphy-Bowman, S. C., Pritchard, A. E., Tart-Zelvin, A., Zabel, T. A., & Mahone, E. M. (2012). Factor structure of a sluggish cognitive tempo scale in clinically-referred children. Journal of Abnormal Child Psychology, 40, 1327–1337.
Jacobson, L. A., Ryan, M., Denckla, M. B., Mostofsky, S. H., & Mahone, E. M. (2013). Performance lapses in children with ADHD contribute to poor reading fluency. Archives of Clinical Neuropsychology, 28, 672–683.
Kessler, R. C., Avenevoli, S., & Merikangas, K. R. (2001). Mood disorders in children and adolescents: an epidemiologic perspective. Biological Psychiatry, 49, 1002–1014.
Lahey, B. B., Applegate, B., Waldman, I. D., Loft, J. D., Hankin, B. L., & Rick, J. (2004). The structure of child and adolescent psychopathology: generating new hypotheses. Journal of Abnormal Psychology, 113, 358–385.
Lahey, B. B., Pelham, W. E., Loney, J., Lee, S. S., & Willcutt, E. (2005). Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives General Psychiatry, 62, 896–902.
Lee, R. W. Y., Jacobson, L. A., Pritchard, A. E., Ryan, M. S., Yu, Q., Denckla, M. B., & Mahone, E. M. (2012). Jitter reduces response-time variability in ADHD: an ex-Gaussian analysis. Journal of Attention Disorders, 19, 794–804.
Leopold, D. R., Christopher, M. E., Burns, G. L., Becker, S. P., Olson, R. K., & Willcutt, E. G. (2016). Attention-deficit/hyperactivity disorder and sluggish cognitive tempo throughout childhood: temporal invariance and stability from preschool through ninth grade. Journal of Child Psychology and Psychiatry, 57, 1066–1074.
McAuley, T., Chen, S., Goos, L., Schachar, R., & Crosbie, J. (2010). Is the behavior rating inventory of executive function more strongly associated with measures of impairment or executive function? Journal of the International Neuropsychological Society, 16, 495–505. doi:10.1017/S1355617710000093.
McBurnett, K., Villodas, M., Burns, G. L., Hinshaw, S. P., Beaulieu, A., & Pfiffner, L. J. (2014). Structure and validity of sluggish cognitive tempo using an expanded item pool in children with attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 42, 37–48.
Mogenson, G. J., Jones, D. L., & Yim, C. Y. (1980). From motivation to action: functional interface between the limbic system and the motor system. Progress in Neurobiology, 14, 69–97.
Newcorn, J. H., Kratochvil, C. J., Allen, A. J., Casat, C. D., Ruff, D. D., Moore, R. J., & Michelson, D. (2008). Atomoxetine and osmotically releases methylphenidate for treatment of attention deficit hyperactivity disorder: acute comparison and differential response. American Journal of Psychiatry, 165, 721–730.
Penny, A. M., Waschbusch, D. A., Klein, R. M., Corkum, P., & Eskes, G. (2009). Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychological Assessment, 21, 380–389.
Pliszka, S. (2007). Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of American Academy of Child and Adolescent Psychiatry, 46, 894–921.
Rucklidge, J. J., & Tannock, R. (2002). Neuropsychological profiles of adolescents with ADHD: effects of reading difficulties and gender. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 43, 988–1003.
Shackman, A. J., Salomons, T. V., Slagter, H. A., Fox, A. S., Winter, J. J., & Davidson, R. J. (2011). The integration of negative effect, pain and cognitive control in the cingulate cortex. Nature Reviews Neuroscience, 12, 154–167.
Shanahan, M. A., Pennington, B. F., Yerys, B. E., Scott, A., Boada, R., & Willcutt, E. G. (2006). Processing speed deficits in attention deficit/hyperactivity disorder and reading disability. Journal of Abnormal Child Psychology, 34, 585–602.
Skirbekk, B., Hansen, B. H., Oerbeck, B., & Kristensen, H. (2011). The relationship between sluggish cognitive tempo, subtypes of attention-deficit/hyperactivity disorder, and anxiety disorders. Journal Abnormal Child Psychology. doi:10.1007/s10802-011-9488-4.
Wechsler, D. (2004). Weschler Intelligence Scale for Children (4th ed.). San Antonio: The Psychological Corporation.
Wietecha, L., Williams, D., Shaywitz, S. E., Shaywitz, B., Hooper, S. R., Wigal, S. B., & McBurnett, K. (2013). Atomoxetine improved attention in children and adolescents with attention-deficit/hyperactivity disorder and dyslexia in a 16 week, acute, randomized, double-blind trial. Journal of Child and Adolescent Psychopharmacology, 23, 605–613.
Willcutt, E. G., Doyle, A. E., Nigg, J. T., Faraone, S. V., & Pennington, B. F. (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biological Psychiatry, 57, 1336–1346.
Willcutt, E. G., Chhabildas, N., Kinnear, M., DeFries, J. C., Olson, R. K., Leopold, D. R., & Pennington, B. F. (2014). The internal and external validity of sluggish cognitive tempo and its relation with DSM–IVADHD. Journal of Abnormal Child Psychology, 42, 21–35.
Wodka, E. L., Mahone, E. M., Blankner, J. G., Larson, J. C., Fotedar, S., & Mostofsky, S. H. (2007). Evidence that response inhibition is a primary deficit in ADHD. Journal of Clinical and Experimental Neuropsychology, 29, 345–356.
Wolraich, M. L., Lambert, W., Doffing, M. A., Bickman, L., Simmons, T., & Worley, K. (2003). Psychometric properties of the Vanderbilt ADHD diagnostic parent rating scale in a referred population. Journal of Pediatric Psychology, 28, 559–568.
Yurgelun-Todd, D. (2007). Emotional and cognitive changes during adolescence. Current Opinion in Neurology, 17, 251–257.
Acknowledgements
This work was supported by U54 HD 079123. A portion of this work was previously presented as a published abstract in the Journal of the International Neuropsychological Society and presented as a poster at the associated International Neuropsychological Society Annual Conference.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest, financial or otherwise, to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
With IRB approval, a waiver of consent was obtained as all data represent de-identified clinical data obtained in the course of routine care.
Additional information
This work was supported by U54 HD 079123.
Rights and permissions
About this article
Cite this article
Jacobson, L.A., Geist, M. & Mahone, E.M. Sluggish Cognitive Tempo, Processing Speed, and Internalizing Symptoms: the Moderating Effect of Age. J Abnorm Child Psychol 46, 127–135 (2018). https://doi.org/10.1007/s10802-017-0281-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-017-0281-x