Abstract
Adolescents with Sluggish Cognitive Tempo (SCT) exhibit symptoms of slowness, mental confusion, excessive daydreaming, low motivation, and drowsiness/sleepiness. Although many symptoms of SCT reflect internalizing states, no study has evaluated the clinical utility of self-report of SCT in an attention-deficit/hyperactivity disorder (ADHD) sample. Furthermore, it remains unclear whether SCT is best conceptualized as a unidimensional or multidimensional construct. In a sample of 262 adolescents comprehensively diagnosed with ADHD, the present study used adolescent- and parent reports of SCT to evaluate the predictive utility of a general SCT factor from a bifactor modeling approach compared the utility of three specific SCT factors (slow, sleepy, and daydreamer) for predicting academic impairment and internalizing psychopathology. Overall, a multidimensional framework of SCT was supported, with the three SCT factors differentially predicting impairment and in one case (school grades), predicting impairment when the general factor did not. Consistent with prior research, SCT slow behaviors appear to be most strongly associated with impairment, predicting both academic impairment and internalizing psychopathology. Parent report of SCT was most useful for predicting academic functioning, whereas youth self-report was important for predicting anxiety and depression. Implications of the findings for the assessment and potential treatment of SCT are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The construct of Sluggish Cognitive Tempo (SCT) includes symptoms of slowness, mental confusion or “fogginess”, excessive daydreaming, low motivation, and drowsiness [1]. Although it is becoming evident that SCT symptoms are present in a variety of populations [2], SCT has primarily been studied in youth with attention-deficit/hyperactivity disorder (ADHD; [2]). Within ADHD samples, there is compelling evidence to support the reliability of SCT and that SCT and ADHD symptoms are related but distinct [1]. Despite rapid growth of the literature on SCT in youth with ADHD, multiple key questions about the measurement of SCT remain unanswered. First, there continues to be debate about whether SCT is best conceptualized as a unidimensional or multidimensional construct, and there are factor analytic findings supporting both [3,4,5,6,7,8]. As such, it is important to understand whether conceptualizing SCT as multiple distinct factors is clinically useful, with specific factors exhibiting unique associations with impairment. Second, it remains unclear what source(s) are best for obtaining information about SCT. SCT is moderately associated with internalizing symptoms [9], and it is possible that youth self-report may be the ideal for measuring what is largely an internal state. However, to date, there has been no research on how self-report of SCT in youth with ADHD is related to impairment. In sum, research is needed to evaluate the clinical utility of assessing SCT multidimensionally and from the youth’s perspective.
Factor structure of SCT
One of the more widely used SCT measures, the 14-item Penny and colleagues [10] scale, includes three separate factors. Specifically, an exploratory factor analysis (EFA) of parent-reported SCT on this scale revealed three dimensions: slow (e.g., “is slow or delayed in completing tasks”), sleepy (e.g., “seems drowsy”), and daydreamer (e.g., “gets lost in his or her own thoughts”) [10]. Similar results were found in a clinic-referred sample with teacher report of this scale [11]. However, these analyses were conducted using exploratory methods that had no a priori hypotheses and are data driven [12, 13], so these factor structures may not generalize to other samples. Recently, Smith and colleagues [7] used confirmatory factor analysis (CFA) and bifactor modeling to compare one (total SCT score), two (slow and sleepy/daydreamer), and three (slow, sleepy, and daydreamer) factor structures for parent- and self-report using this same measure in a sample of adolescents with ADHD. The CFA with the three-factor structure was the best fitting model for both parent- and self-report of SCT. The bifactor model also demonstrated excellent fit, and suggested that the specific factors were not reliable enough to be considered separately. Smith et al. [7] concluded that given the mixed evidence supporting uni- and multidimensional factor structures for SCT, that decisions should be made based upon clinical utility, and whether the specific factors differentially and consistently predicted impairment.
Multidimensional associations with impairment
There are numerous studies showing that SCT symptoms in general (i.e., total scores) are associated with functional impairment above and beyond the impact of ADHD symptoms [8, 14,15,16]. In particular, SCT seems to be associated with internalizing problems (e.g., anxiety and depression; [4, 14, 17, 18]), as well as with the academic (e.g., homework and grades; [19]) domain. To date, two studies have evaluated whether specific SCT factors differentially predict impairment [4, 19].
Fenollar Cortés and colleagues [4] separated SCT into two dimensions; SCT-inconsistent alertness (SCT-IA, e.g., daydreaming, losing one’s train of through) and SCT slowness (SCT-S, e.g., slowed thinking, drowsiness). Fenollar Cortés et al.’s study [4] is the only study to date to evaluate associations between depression and multiple factors of SCT, finding that only SCT-S was positively associated with depression. Only one study has evaluated associations between SCT measured multidimensionally and academic impairment. In a sample of 52 adolescents diagnosed with ADHD, Langberg et al. [19] found that parent-rated SCT-slow and teacher-rated SCT-low initiation/persistence (e.g., slow movement; is apathetic; lacks motivation to complete work) predicted multiple aspects of academic impairment above and beyond ADHD and the other SCT factors (three-factor structure was used). Importantly, some of the findings were cross-rater (e.g., parent rated SCT-slow predicting teacher-rated academic impairment) and one association was with a non-rating metric (teacher-rated SCT-low initiation/persistence predicted school grades). Accordingly, in two relatively small samples, there is some evidence that viewing SCT as multidimensional may have clinical utility. However, neither of these studies included self-report of SCT in predicting impairment and none compared the utility of the specific factors to the utility of a bifactor or total score approach.
Utility of self-report
Since SCT has mainly been studied in ADHD samples, and the gold-standard measurement for ADHD relies on parent and teacher ratings [20], there has been minimal examination of self-reported SCT. However, self-report is considered the best source of information regarding internalizing conditions [21, 22], and SCT is moderately correlated with internalizing symptoms [1]. In the only study to explore how self-report of SCT is related to impairment, Becker et al. [23] found in a general school sample that self-reported SCT symptoms were significantly associated with poorer self-report of academic functioning above and beyond demographic factors and other psychopathology, but were not significantly associated with teacher-rated academic functioning [23]. However, the authors only evaluated the associations between an SCT total score and impairment, and prior evidence suggests that specific aspects of SCT are most highly associated with academic functioning [19]. In sum, important next steps include evaluating the association between impairment and SCT defined multidimensionally in an ADHD sample and with SCT assessed from both the self and parent perspective.
Present study
Accordingly, the primary goal of the present study was to evaluate associations between the general factor of SCT and the specific factors of slow, sleepy, and daydreamer as rated by both parents and youth with ratings and objective indicators of functional impairment and psychopathology. Specifically, associations with anxiety, depression, and academic functioning were examined while controlling for the influence of ADHD symptoms. This is the first study to examine associations between self-report of SCT and impairment and psychopathology in an ADHD sample. Although accumulating evidence suggests that SCT symptoms are present in a variety of populations [1], evaluation of SCT within ADHD samples remains important as SCT may be more common in ADHD samples and could have a different etiology and outcomes given the existing deficits seen with ADHD. The previously validated structure of the Penny et al. measure [7, 10, 23] was used to assess associations with impairment, including associations with both the general factor and specific factors.
The present study focused on academic outcomes because of emerging evidence that SCT symptoms are particularly impairing for academic functioning, and because the mechanisms thought to underlie SCT (e.g., slow thought processes, lack of initiative, and low motivation) seem particularly relevant for academic achievement. Consistent with Langberg et al. [19], we predicted that the SCT-daydreamer factor would predict academic functioning as measured by grades, while SCT-Slow would predict teacher-rated homework problems. This is the first study to assess associations with academic functioning from both the parent and adolescent perspective. However, Smith et al.’s [7] invariance testing with this measure suggested that both reporters could provide unique information for SCT. Accordingly, we predicted that both parent and adolescent reports of SCT would predict academic outcomes. The present study focused on internalizing psychopathology because of emerging evidence that SCT symptoms and internalizing symptoms are significantly associated and may share a common etiology. Specifically, aspects of SCT include apathy, decreased effort, and lack of interest in activities, which are also core aspects of internalizing psychopathology. Given that internalizing symptoms are often covert, self-report is considered most “accurate,” and best-practice recommendations emphasize self-report in assessing internalizing symptoms [21, 22]. As SCT includes internalizing states, we hypothesized that self-report of SCT would account for a greater proportion of the variance than parent report in predicting symptoms of anxiety and depression. Consistent with Fenollar Cortés et al. [4], we predicted that the SCT-Slow factor would be most strongly associated with higher levels of depression and anxiety.
Methods
Participants were 262 middle-school age adolescents (boys 193, girls 69) in grades 6–8 (ages 10–15; M = 11.95, SD = 1.05) who were comprehensively diagnosed with ADHD. Participants were recruited from six public middle schools in the Eastern United States. Demographics for the sample can be found in Table 1. The sample was diverse, with parents identifying 30.2% of the youth as African American (n = 79), 10.3% identified as Biracial (n = 27), 56.5% identified as White (n = 148), 2.3% identified with another race (n = 6), and two participants chose not to respond. Per procedures described next; 171 participants (65.3%) were diagnosed with ADHD Predominantly Inattentive Presentation (ADHD-IA) and 91 (34.7%) were diagnosed with ADHD Combined Presentation (ADHD-C).
Procedure
Participants who provided data for the current study were recruited as part of a larger study evaluating school-based intervention programs for adolescents with ADHD. All data evaluated in the present study were collected at baseline, prior to participants receiving any intervention. Recruitment methods included study announcement letters mailed to all parents at participating middle schools, flyers posted in each school, and direct referral by school staff. Interested parents completed a phone screen that included rating their child on each of the nine DSM-5 ADHD-IA symptoms on a 4-point Likert scale (0 = rarely, 1 = sometimes, 2 = often, 3 = very often). If a parent reported that their child had a previous diagnosis of ADHD or they endorsed the presence of at least four of nine ADHD-IA symptoms at clinically significant levels (i.e., “often” or “very often”), a full in-person evaluation was scheduled.
During the inclusion/exclusion evaluation, adolescents and parents/guardians independently were administered the Parent Children’s Interview for Psychiatric Syndromes (P-ChIPS; [24]), a structured diagnostic interview which was administered by a doctoral student supervised by a licensed clinical psychologist. In addition, parents and adolescents completed the Behavior Assessment System for Children, Second Edition (BASC-2; [25]), a measure designed to broadly screen for behavioral or mood problems in children. Parents and at least one teacher of each student also completed the Vanderbilt ADHD diagnostic rating scale ([26]), which is a 45-item measure that assesses symptoms of ADHD, oppositional defiant disorder (ODD), and conduct disorder (CD). Finally, adolescents were administered a brief battery assessing their cognitive and academic achievement abilities, including four subtests from the Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV; [27]), and seven subtests from the Wechsler Individual Achievement Test, Third Edition (WIAT-III; [28]).
Participants were considered eligible for the study if they met five criteria: (1) attended a participating middle school; (2) met full DSM-5 diagnostic criteria for ADHD-IA or ADHD-C presentation based on the combination of parent report on the P-ChIPS and teacher report; (3) experienced significant impairment due to ADHD symptoms based on parent and/or teacher report; (4) had an estimated full scale IQ (FSIQ) of at least 80 according to performance on the WISC-IV; and (5) did not meet diagnostic criteria for any bipolar disorder, psychosis, or obsessive–compulsive disorder (OCD) according to parent report on the P-ChIPS. To maximize generalizability, students with comorbid diagnoses of ODD, CD, and anxiety and mood disorders were allowed to participate in the study. Parent report on the P-ChIPS was used for externalizing comorbidities, with 30.6% meeting criteria for ODD, 3.2% for CD, while child report on the ChIPS was used for internalizing comorbidities, with 25.4% meeting for an anxiety disorder and 5.3% for depression.
Measures
Participants’ parents/guardians completed a demographics questionnaire at the study baseline that included information on sex, race/ethnicity, grade in school, parent education and income, and ADHD medication status.
Children’s interview for psychiatric syndromes (ChIPS)
The ChIPS [24] is a structured diagnostic interview for administration to parents and children (children ages 6–18) and has a parent (P-ChIPS) and child version (ChIPS). The ChIPS has shown high internal consistency and test–retest reliability [29] and high convergent validity in relation to the diagnostic interview for children and adolescents-revised-child version (DICA-R-C) [29]. A recent review of child and adolescent diagnostic interviews [30] found five separate studies documenting that the ChIPS has good concurrent validity with other validated diagnostic interviews, including the DICA-R-C and the schedule for affective disorders and schizophrenia for school aged children (K-SADS). Furthermore, the ChIPS has good construct validity, with the percent of agreement between a consensus panel of child psychopathology experts and the results from ChIPS interviews ranging from 97.5 to 100%. Sensitivity averaged 87% across diagnostic categories and specificity averaged 76%, with sensitivity and specificity for attention deficit disorder being 100 and 44%, respectively [29].
Vanderbilt ADHD diagnostic rating scale (VADRS)
The VADRS is a DSM-IV-based scale that includes all 18 DSM-IV symptoms of ADHD. Parents and teachers rate how frequently each symptom occurs on a four-point Likert scale (0 = never, 1 = occasionally, 2 = often, 3 = very often). The VADRS produces an inattention score (sum of the nine inattention items) and a hyperactivity/impulsivity score (sum of the nine hyperactive/impulsive items). The VADRS has excellent psychometric properties [26]. In the present study, internal consistencies were: ADHD inattention α = 0.87, ADHD hyperactivity-impulsivity α = 0.90, ODD/CP α = 0.87, and anxiety/depression α = 0.87.
Sluggish Cognitive Tempo scale
The parent and self-report versions of the Penny et al. [10] SCT Scale were used in this study. The SCT scale consists of 14 items that are each rated on a four-point scale from 0 = never to 3 = very often. As described above, confirmatory factor analyses have identified three factors for the parent- and self-report versions: slow, sleepy, and daydreamer [7]. CFAs were conducted on an ADHD adolescent sample. The parent-report three-factor model had adequate fit (RMSEA = 0.118, CFI = 0.928, TLI = 0.912) and was significantly better than a one- or two-factor model, while the self-report three-factor model had excellent fit (RMSEA = 0.053, CFI = 0.979, TLI = 0.970) and was significantly better than a one- or two-factor model according to Chi-square difference testing [7]. These findings suggest a three-factor model best fits the scale. Invariance testing on this same group suggests that parent- and self-report may provide unique information, as parent- and self-reports were not invariant [7]. Test–retest reliability estimates range from 0.70 to 0.87 for the parent-report version. As in Becker et al. and Smith et al. [7, 23], the parent-report scale was modified for use as a self-report measure in the present study (e.g., instead of “does your child…”, “do you…”). Each of the 14 items were changed to reflect the first person, and items were kept as similar as possible to the original parent-report version, but some words were changed to make it more understandable for children (e.g., instead of “lethargic” use “don’t have energy”). In the present study, internal consistencies for parent and child total scores were α = 0.87 and α = 0.86, respectively. Internal consistencies for the subscales were α = 0.800, α = 0.860, and α = 0.834 for parent-report, and α = 0.712, α = 0.796, and α = 0.751 for self-report, for the slow, sleepy, and daydreamer subscales, respectively.
Grades
Grade point average (GPA) is a standardized numerical measure of aggregated grades from a student’s courses within a given time period. GPA is on a four-point scale, with higher numbers indicating better grades (4.0 = A, 3.0 = B, 2.0 = C, and 1.0 = D). In the current study, grades from four core subjects (i.e., mathematics, English, science, and social studies) were collected and converted into the four-point scale. These converted grades were then averaged over the same semester that the evaluation appointment was conducted.
Homework Performance Questionnaire (HPQ)
The Homework Performance Questionnaire (HPQ; [31]) is a 22-item rating scale that assesses a student’s homework behavior. Higher scores on the HPQ indicate a better homework performance. The HPQ relies on teacher report and is, therefore, useful for cross-rater academic analyses. The HPQ has previously demonstrated high internal consistency (α = 0.85–0.91) and 2-week test–retest reliability [31]. For the current study, two teachers rated student’s homework behaviors, and scores were averaged across the teachers.
Behavior assessment system for children, second edition (BASC-2)
The BASC-2 is a widely used, multi-dimensional clinical assessment tool that includes self-report and informant-based report forms to evaluate a wide range of behavioral and emotional experiences of youth. In the current study, parents and adolescents completed the BASC-2 [25]. Some items assess the frequency of experiences (rated from 0 = never to 3 = almost always), while others are true/false questions assessing the presence of thoughts and behaviors. The BASC-2 is widely used in mental health and educational settings, and has been normed on a large representative sample [25]. T scores representing age-normed domain scores were used for this study. T scores reflect a continuous distribution within the population, with a mean of 50 and a standard deviation of 10. BASC-2 authors suggest that T scores over 60 (i.e., scores above the 86th percentile of the normative sample) represent potentially meaningful clinical elevations. In the current study, scales of particular interest were the anxiety and depression scales. For anxiety, self-report consists of 13 items (e.g., “I get nervous”). For depression, self-report consists of 12 or 13 child and adolescent versions, respectively, including items such as “I feel sad.” Given the differences across the child and adolescent versions for the interpersonal relations scale and the depression scale, T scores will be used in all analyses with the BASC to standardize across versions.
Data analysis
To assess the external validity of SCT, multiple regression analyses were conducted. Because ADHD symptoms are known to be associated with impairment, parent-rated ADHD symptoms were entered into the model as a covariate. Two regressions were conducted for each outcome (academic, anxiety, and depression): (1) including both parent- and self-reports of the general SCT factor and (2) including both parent- and self-reports of the specific factors. For the subscales on the BASC-2, T scores were used to standardize across the child and adolescent versions. In addition, the multicollinearity of these predictors (ADHD, SCT, sleepy, slow, and daydreamer) was examined. If two variables are closely related, then any potential effect of one predictor could be artificially reduced by the presence of the collinear variable in the model. To this point, it was not possible to test the predictive utility of the specific factors above and beyond the general factor of SCT due to multicollinearity. To test for multicollinearity, the variance inflation factor (VIF) was calculated for each predictor in the models, with VIFs greater than 10 indicating multicollinearity.
Results
For all data, assumptions of univariate and multivariate normality, linearity, and normally distributed errors were checked and met.
Academic functioning
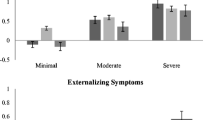
The model including ADHD symptoms and the parent- and self-report SCT general factors in predicting teacher-rated homework performance was significant, F(4, 209) = 2.96, p = 0.021, R 2 = 0.053. Parent report of SCT was the only significant individual variable in the model, β = −0.219, t(209) = −2.82, semi-partial r 2 = 0.036, p = 0.001. The regression analysis with the specific SCT factors, slow, sleepy, and daydreamer, and ADHD symptoms predicting teacher-rated homework performance was also significant, F(8, 205) = 2.56, p = 0.011, R 2 = 0.091. However, only the parent-reported slow factor β = −0.209, t(205) = −2.24, semi-partial r 2 = 0.022, p = 0.026 was a significant predictor of homework performance over and above the other subscales. The model evaluating whether the general construct of parent- and self-report SCT predicted GPA was not significant, F(4, 210) = 1.55, p = 0.19. When inputting the specific factors of Slow, Sleepy, and Daydreamer as predictors with ADHD symptoms, the model was significant, F(8, 206) = 4.60, p < 0.001, R 2 = 0.152. Two of the parent-rated specific factors, Slow β = −0.377, t(206) = −4.29, semi-partial r 2 = 0.076, p < 0.001 and daydreamer β = 0.302, t(206) = 4.06, semi-partial r 2 = 0.068, p < 0.001, were significant individual predictors. It is important to note that the slow factor was negatively associated with grades while the daydreamer factor was positively associated with grades.
Internalizing symptoms
The model with the SCT general factors and ADHD symptoms predicting anxiety was significant, F(4, 232) = 23.76, p < 0.001, R 2 = 0.291, with both parent-β = −0.174, t(232) = −2.73, semi-partial r 2 = 0.023, p = 0.007 and self-report SCT β = 0.532, t(232) = 9.49, semi-partial r 2 = 0.276, p < 0.001 significantly predicting anxiety. The model with the slow, sleepy, and daydreamer specific factors and ADHD symptoms was also significant, F(8, 228) = 12.98, R 2 = 0.313, p < 0.001. Each of the self-reported SCT factors predicted anxiety, slow, β = 0.191, t(228) = 2.58, semi-partial r 2 = 0.020, p = 0.011, sleepy, β = 0.195, t(228) = 2.65, semi-partial r 2 = 0.021, p = 0.009 and daydreamer, β = 0.251, t(228) = 3.57, semi-partial r 2 = 0.038, p < 0.001, and parent-reported sleepy β = −0.135, t(232) = −2.14, semi-partial r 2 = 0.016, p = 0.033 also predicted anxiety over the parent-reported slow and daydreamer factors. The model with the general SCT factors and ADHD symptoms predicting depression was significant, F(4, 232) = 17.99, p < 0.001, R 2 = 0.237. Only self-report of SCT significantly predicted depression, β = 0.481, t(324) = 8.28, semi-partial r 2 = 0.226, p < 0.001. The regression with the specific factors of SCT and ADHD symptoms predicting depression was also significant, F(8, 228) = 9.34, p < 0.001, R 2 = 0.247, self-reported slow, β = 0.258, t(228) = 3.34, semi-partial r 2 = .037, p = 0.001 and daydreamer β = 0.232, t(228) = 3.16, semi-partial r 2 = 0.033, p = 0.002 were the only significant individual predictors of depression over and above the Sleepy factor and parent-reported factors.
Discussion
This was the first study to evaluate how multiple factors of SCT, measured from both the self- and parent perspectives, were related to academic impairment and psychopathology in an ADHD sample. Given that two studies using bifactor modeling have found the specific factor scores unreliable statistically [7, 23], yet many studies have suggested that SCT is multidimensional (e.g., 3–4, 6, 10–11), it is important to evaluate whether the specific factors of SCT have clinical utility in predicting outcomes. It is also important to evaluate what source of information, parent- or self-reports, has the greatest predictive power. Parent but not self-report of SCT predicted academic impairment. Importantly, these associations included cross-rater findings and associations with more objective outcomes. What is perhaps most noteworthy is that the general SCT factor did not predict GPA, but taking a multidimensional approach, the parent-rated Slow factor predicted GPA impairment over the parent-reported Sleep factor and three self-reported factors. In contrast to the findings with academic functioning, youth self-report of SCT was most important in predicting anxiety and depression. Furthermore, the models accounted for relatively high levels of variance, 29.1 and 23.7%, for anxiety and depression, respectively.
Overall, the findings suggest that there is clinical utility in considering SCT as multidimensional, as the specific factors differentially predicted outcomes. This is now the second study to find that the SCT-Slow factor is uniquely related to academic impairment [19]. Although little is known about the etiology of each distinct factor of SCT, one possible explanation is underlying executive functioning (EF) deficits [1, 8, 32, 33]. In the only study to date to examine associations between specific factors of SCT and EF, the parent-reported SCT Slow factor predicted both parent- and teacher-reported metacognitive EF deficits (e.g., working memory, managing task demands, material organization, and self-monitoring) above and beyond demographics and ADHD symptoms [32]. Consistent with these findings, the slow factor includes items such as “lacks initiative to complete work” and “effort on tasks fades quickly,” which may represent the underlying metacognitive EF deficits such as planning, organization, and self-motivation, which can negatively affect academic performance [32, 33]. Furthermore, it is important to note that the general construct of SCT did not significantly predict grades, but when the model included the specific factors, the Slow factor emerged significant over and above the other factors. This finding highlights the clinical utility of the specific factors.
In contrast to predicting academic impairment, each self-reported specific factor (Slow, Sleepy, Daydreamer) predicted higher levels of anxiety, which is consistent with the moderate-to-strong bivariate associations, as shown in Table 2. Consistent with Fenollar Cortés et al. [4], the self-reported slow factor predicted higher levels of depression, though the daydreamer factor also predicted depression over and above the parent-reported factors and self-reported sleepy factor. As the slow factor may have an underlying EF deficit in motivation ([32], e.g., “I am not interested in participating in activities,” “I don’t have the drive to complete my work”), it is understandable that it would also predict depression, as depression is often associated with apathy and a lack of motivation to participate in life events.
There were also some unexpected findings with the regression analyses. For example, the parent-reported daydreamer factor predicted higher grade point averages, which was contrary to hypotheses. This may be a result of the daydreamer factor containing only three items, although the reliability for these three items was sufficient (α = 0.83 and α = 0.75 for parent and self, respectively). Interestingly, when examining bivariate associations, the daydreamer factor was not significantly associated with GPA, suggesting that the positive association is only found when included in the regression with the other factors. Overall, it is noteworthy that parent-reported daydreamer did not predict any impairment/psychopathology except for the unexpected finding, perhaps suggesting the need to return to a larger item pool to sufficiently capture the daydreaming aspects of SCT. In a recent meta-analysis, 13 items were found to best represent SCT across multiple studies [1]. Adding items from this list such as “in a fog” or “spacey” that are not included in the Penny et al. [10] measure daydreamer factor may improve fit for the parent version and prediction of impairment. One additional finding that was not consistent with hypotheses was that parent-reported slow predicted lower levels of anxiety symptoms. Anxiety has not previously been examined with specific factors of SCT, and as such, this finding needs to be replicated before drawing any conclusions. It appears that these unexpected findings were not a function of multicollinearity as all VIFs were less than 10, and the regression findings were consistent with bivariate associations. Correlations can be found in Table 2. Despite these inconsistencies, overall, the results suggest that viewing SCT as a multidimensional construct may have clinical utility.
Limitations
The present study should be interpreted in light of several limitations. The cross-sectional nature of the data does not allow conclusions to be drawn about causality or the direction of the effects regarding SCT, impairment, and psychopathology. Therefore, it is unclear if SCT caused academic impairment or anxiety and depression, vice versa, or a mix of the two. In addition, although the use of a clinical sample of young adolescents with ADHD builds on prior work, it is important to note that these findings may not generalize to younger children or to adults with ADHD. Overall, SCT research in ADHD and non-ADHD samples remains important, as there may be different etiologies and outcomes for individuals with and without ADHD and SCT symptoms. Finally, the associations between SCT and anxiety and depression should be interpreted with caution, because they are subject to within-source bias. However, depression and anxiety are best rated in adolescence with self-report [21, 22], so in this case, self-report was prioritized as other raters (e.g., parents or teachers) may have insufficient knowledge to rate certain items.
Future directions
If SCT is best conceptualized as multidimensional, latent profile analyses (LPA) may be helpful in understanding whether there are naturally occurring SCT symptom profiles or clusters. It is currently unclear whether there is variability within SCT, with youth scoring high on some factors but low on others. For example, perhaps, some individuals exhibit slow behaviors but do not appear “sleepy” or to be “daydreaming”. If multiple profiles emerge, this would have implications for intervention given the differential associations between the three SCT factors and domains of impairment. It would also be important to evaluate whether these profiles are stable across time, or if similar to ADHD symptom presentations, change occurs across development [34, 35]. The stability of the profiles created by the LPA could be analyzed using latent transition analysis (LTA).
At this point, there is compelling evidence that SCT symptoms predict multiple domains of functional impairment above and beyond ADHD symptoms, yet to date, no intervention has been created to specifically target SCT symptoms. Due to the cognitive, internal aspects of some SCT symptoms (e.g., fogginess, daydreaming and losing train of thought), a cognitive-behavioral intervention approach may be needed. Specifically, it may be difficult to take a purely behavioral approach which is common in ADHD treatment, as behavioral approaches rely on the application of contingencies for observed behaviors. Behavioral activation may also be a good strategy to incorporate, as some symptoms, such as apathy, slow movements, and sleepiness, are similar to depression, and behavioral activation could help to increase motivation for adolescents displaying these symptoms.
Conclusions
In sum, the findings from this study suggest that a multidimensional structure of SCT has clinical utility and that clinicians and researchers should incorporate self-report into the assessment of SCT. In addition, this study confirmed that the slow factor is particularly related to academic impairment, suggesting that these behaviors may be an important target for academic-skill-related interventions for adolescents with ADHD.
References
Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM et al (2016) The internal, external, and diagnostic validity of Sluggish Cognitive Tempo: a meta-analysis and critical review. J Am Acad Child Psy 55:163–178
Becker SP, Marshall SA, McBurnett K (2014) Sluggish Cognitive Tempo in abnormal child psychology: a Historical overview and introduction to the special section. J Abnorm Child Psychol 42:1–6
Barkley RA (2013) Distinguishing Sluggish Cognitive Tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. J Clin Child Adolesc 42:161–173
Fenollar Cortés J, Servera M, Becker SP, Burns GL (2014) External validity of ADHD Inattention and Sluggish Cognitive Tempo dimensions in Spanish children with ADHD. J Atten Disord. doi:10.1177/1087054714548033
Lee S, Burns GL, Snell J, McBurnett K (2014) Validity of the Sluggish Cognitive Tempo symptom dimension in children: Sluggish Cognitive Tempo and ADHD-inattention as distinct symptom dimensions. J Abnorm Child Psychol 42:7–19
McBurnett K, Villodas M, Burns GL et al (2014) Structure and validity of Sluggish Cognitive Tempo using an expanded item pool in children with attention-deficit/hyperactivity disorder. J Abnorm Child Psychol 42:37–48
Smith ZR, Becker SP, Garner AA, Rudolph CW, Molitor SJ, Oddo LE, Langberg JM (2016) Evaluating the structure of Sluggish Cognitive Tempo using confirmatory factor analytic and bifactor modeling with parent and youth ratings. Assessment. doi:10.1177/1073191116653471
Willcutt EG, Chhabildas N, Kinnear M et al (2014) The internal and external validity of Sluggish Cognitive Tempo and its relation with DSM-IV ADHD. J Abnorm Child Psychol 42:21–35
Becker SP, Langbergm JM, Luebbe AM, Dvorsky MR, Flannery AJ (2014) Sluggish Cognitive Tempo is associated with academic functioning and internalizing symptoms in college students with and without attention-deficit/hyperactivity disorder. J Clin Psychol 70:388–403
Penny AM, Waschbusch DA, Klein RM, Corkum P, Eskes G (2009) Developing a measure of Sluggish Cognitive Tempo for children: content validity, factor structure, and reliability. Psychol Assess 21:380–389
Jacobson LA, Murphy-Bowman SC, Pritchard AE et al (2012) Factor structure of a Sluggish Cognitive Tempo scale in clinically-referred children. J Abnorm Child Psychol 40:1327–1337
Farrell AD (1999) Statistical methods in clinical research. In: Kendall PC, Butcher JN, Holmbeck GN (eds) Handbook of research methods in clinical psychology, 2nd edn. Willey, New York, pp 72–106
Floyd FJ, Widaman KF (1995) Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess 7:286–299
Bernad MD, Servera M, Becker SP, Burns GL (2015) Sluggish Cognitive Tempo and ADHD inattention as predictors of externalizing, internalizing, and impairment domains: a two-year longitudinal study. J Abnorm Child Psychol. doi:10.1007/s10802-015-0066-z
Capdevila-Brophy C, Artigas-Pallares J, Navarro-Pastor JB, Garcia-Nonell K, Rigau-Ratera E, Obiols JE (2014) ADHD predominantly inattentive subtype with high Sluggish Cognitive Tempo: a new clinical entity? J Atten Disord 18:607–616
Garner AA, Marceaux JC, Mrug S, Patterson C, Hodgens B (2010) Dimensions and correlates of attention deficit/hyperactivity disorder and Sluggish Cognitive Tempo. J Abnorm Child Psychol 38:1097–1107
Bernad MD, Servera M, Grases G, Collado S, Burns GL (2014) A cross-sectional and longitudinal investigation of the external correlates of Sluggish Cognitive Tempo and ADHD-inattention symptoms dimensions. J Abnorm Child Psychol 42:1225–1236
Skirbekk B, Hjelde Hansen B, Oerbeck B, Kistrensen H (2011) The relationship between Sluggish Cognitive Tempo subtypes of attention-deficit/hyperactivity disorder, and anxiety disorders. J Abnorm Child Psychol 39:513–525
Langberg JM, Becker SP, Dvorsky MR (2014) The association between Sluggish Cognitive Tempo and academic functioning in youth with attention-deficit/hyperactivity disorder (ADHD). J Abnorm Child Psychol 42:91–103
Pelham WE, Fabiano GA, Massetti GM (2005) Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. J Clin Child Adolec 34:449–476
Klein DN, Dougherty LR, Olino TM (2005) Towards guidelines for evidence-based assessment of depression in children and adolescents. J Clin Child Adolec 34:412–432
Silverman WK, Ollendick TH (2005) Evidence-based assessment of anxiety and its disorders in children and adolescents. J Clin Child Adolec 34:380–411
Becker SP, Luebbe AM, Joyce AM (2015) The child concentration inventory (CCI): initial validation of a child self-report measure of Sluggish Cognitive Tempo. Psychol Assess 27:1037–1052
Weller EB, Weller RA, Fristad MA, Rooney MT, Schecter J (2000) Children’s interview for psychiatric syndromes (ChIPS). J Am Acad Child Psy 39:76–84
Reynolds CR, Kamphaus RW (2004) Behavior assessment system for children-second edition. Circle Pines, Minnesota
Wolraich ML, Lambert EW, Doffing MA et al (2003) Psychometric properties of the vanderbilt ADHD diagnostic parent rating scale in a referred population. J Pediatr Psychol 28:559–568
Wechsler D (2003) Wechsler intelligence scale for children—fourth edition. The Psychological Coorporation, TX
Wechsler D (2009) Wechsler individual achievement test—third edition. Pearson, TX
Fristad MA, Teare M, Weller EB, Weller RA, Salmon P (1998) Study III: development and concurrent validity of the children’s interview for psychiatric syndromes—parent version (P-ChIPS). J Child Adol Psychop 8:221–226
Leffler JM, Riebel J, Hughes HM (2015) A review of child and adolescent diagnostic interviews for clinical practitioners. Assessment 22:690–703. doi:10.1177/1073191114561253
Power TJ, Dombrowski SC, Watkins MW, Mautone JA, Eagle JW (2007) Assessing children’s homework performance: development of multi-dimensional, multi-informant rating scales. J School Psychol 45:333–348
Becker SP, Langberg JM (2014) Attention-deficit/hyperactivity disorder and Sluggish Cognitive Tempo dimensions in relation to executive functioning in adolescents with ADHD. Child Psychiatry Hum Dev 45:1–11
Jiménez EAA, Ballabriga MCJ, Bonillo Martin A, Arrufat FJ, Giacobo RS (2015) Executive functioning in children and adolescents with symptoms of Sluggish Cognitive Tempo and ADHD. J Atten Disord 19:507–514
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, VA
Willcutt EG (2012) The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 9:490–499
Acknowledgement
This research was supported by a grant awarded to Dr. Langberg from the Institute of Education Sciences (R305A130011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards statement
All human studies have been approved by the appropriate ethics committee and have, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
About this article
Cite this article
Smith, Z.R., Langberg, J.M. Predicting academic impairment and internalizing psychopathology using a multidimensional framework of Sluggish Cognitive Tempo with parent- and adolescent reports. Eur Child Adolesc Psychiatry 26, 1141–1150 (2017). https://doi.org/10.1007/s00787-017-1003-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-017-1003-1