Abstract
Objective
To investigate the macular morphological and visual outcomes of combined idiopathic epiretinal membrane (iERM) removal with triamcinolone acetonide (TA) injection based on consideration of the ectopic inner foveal layer (EIFL) staging scheme.
Methods
Retrospective case–control study. The clinical data of 84 eyes of 84 patients who underwent vitrectomy for iERM between 2018 and 2022 were reviewed. The enrolled subjects were divided into the TA and non-TA groups. Fifty-one eyes received intravitreal TA injection following vitrectomy and ERM peeling (TA group), and 33 were only treated by standard vitrectomy and ERM peeling (non-TA group). Preoperative and postoperative EIFL stages, central foveal thickness (CFT), and best-corrected visual acuity (BCVA) were compared between both groups.
Results
After a mean follow-up of 7.69 ± 3.68 months, both groups exhibited significant improvement in EIFL stages (P < 0.01), with no discernible advantage observed in the TA group. The TA and non-TA groups demonstrated improvement in the EIFL stages in 56.86 and 63.64% of eyes, respectively (P = 0.43). The CFT and BCVA significantly improved in both groups at the final visit (P < 0.01). However, CFT in the non-TA group displayed a more significant reduction during the follow-up (P < 0.03). Subgroup analysis revealed no significant differences in postoperative CFT and BCVA between the two groups in cases with or without continuous EIFL (P > 0.10).
Conclusion
Our findings indicate that combined intravitreal TA injection following ERM removal conferred no significant benefits in alleviating macular thickening or improving visual acuity in iERM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epiretinal membrane (ERM) is a prevalent retinal disease characterized by fibrocellular proliferation at the retinal interface. The reported prevalence of ERM ranges from 7 to 11.8%, with increasing age being the most prominent risk factor [1]. While patients may remain asymptomatic at early stages, they often have visual impairment and metamorphopsia as the disease progresses. Vitrectomy with ERM peeling has emerged as a viable therapeutic approach for ERM, and it can effectively improve the macular architecture and visual acuity [2, 3].
The contraction of ERM leads to alterations in the normal retinal architecture [4], and the architecture of the inner retina has been identified as a predictor of ERM surgeries [5, 6]. Govetto et al. [7] reported that the continuous ectopic inner foveal layer (EIFL) was associated with preoperative visual acuity and postoperative outcomes of ERM and considered that the development of ectopic inner foveal layers may result from the combination of both physical displacement of the inner retinal layers and Müller cell–driven proliferation. Moreover, their research introduced the EIFL staging system for ERM, which was valuable in predicting surgical outcomes [8,9,10,11].
Macular edema is a prominent feature of ERM and is associated with unfavorable prognostic outcomes after surgery [12, 13]. Persistent microcystic macular edema further worsens the visual outcome [14,15,16]. The corticosteroids have been shown to inhibit inflammation and proliferation of the Müller cell [17]. Intravitreal corticosteroid injection was reported to be beneficial in managing postoperative persistent macular edema by suppressing inflammation [18]. Prior studies suggested that intravitreal TA injection following ERM removal improved retinal architecture by reducing the central foveal thickness (CFT) [19]. However, the advantages of combined ERM removal with intravitreal TA injection on macular architecture and function improvement remain controversial [20,21,22]. The severity of macular edema varies at different stages of ERM [7, 11]. Nevertheless, previous investigations paid less attention to the impact of EIFL stages when evaluating the effects of intravitreal TA injection on macular architectural and visual recovery following ERM removal. Moreover, little research has investigated the improvements in the EIFL stages of this combined intervention.
This study investigated the impact of combined ERM removal and intravitreal TA injection on postoperative macular architecture and visual acuity for iERM based on consideration of the EIFL staging scheme.
Methods
Study population
This retrospective case–control study adhered to the principles of the Declaration of Helsinki and received approval from the Joint Shantou International Eye Center Ethics Committee. The data from eyes that underwent vitrectomy for iERM between January 2018 and May 2022 were reviewed.
The inclusion criteria included patients having Stage 2 or advanced iERM, with a follow-up period of at least three months after vitrectomy. We excluded eyes with secondary ERM, vitreomacular traction syndrome, macular holes, retinal detachment, proliferative diabetic retinopathy, retinal vein occlusion, and glaucoma. Additionally, eyes with postoperative data deficiency, poor OCT imaging quality, preoperative and postoperative OCT device inconsistency, and eyes receiving further intravitreal injection therapy were excluded.
Data collection
Preoperative and postoperative data collected from medical records included age, gender, BCVA, intraocular pressure (IOP), and administration of intravitreal TA injection. The subjects were further divided into the TA and non-TA groups based on whether concomitant intravitreal TA injection was administered at the end of surgery.
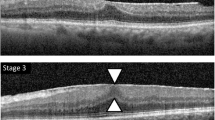
Optical coherence tomography (3D OCT-2000 or Triton DRI OCT, Topcon, Japan) was employed to assess macular architecture using a macular cube 512×128 scan pattern and radial scan protocol. According to the EIFL staging scheme reported by Govetto et al. [7], the ERM classification was performed by the same ophthalmologist (H. Lin) using the horizontal B-scan image via the fovea. The EIFL staging scheme involved four stages: Stage 1 referred to a mild ERM with the foveal pit and well-defined retinal layers; Stage 2 exhibited well-defined retinal layers, but the foveal depression was lost; Stage 3 was characterized by continuous ectopic inner foveal layers with still discernible retinal layers; Stage 4 presented with continuous ectopic inner foveal layers and disrupted retinal layers (Fig. 1).
Optical coherence tomography images of ectopic inner foveal layer (EIFL) stages before and after epiretinal membrane (ERM) removal. A, B: A sixty-four-year-old male with preoperative best-corrected visual acuity (BCVA) of 0.22 logMAR. (Panel A) The preoperative scan indicated morphological changes of Stage 2 ERM with intraretinal cysts (white arrow). (Panel B) Six months after surgery, the foveal pit recovered, and the macular architecture improved to Stage 1. C, D: A sixty-three-year-old female with preoperative BCVA of 1.00 logMAR. (Panel C) The preoperative scan displayed a Stage 4 ERM, which presented with continuous EIFL and disruption of retinal layers. (Panel D) After four months, the postoperative retinal layers became recognizable, and the macular architecture improved to Stage 3
The CFT was defined as the distance from the inner to the outer surface of the neural retina at the fovea, and it was measured by the same ophthalmologist (H. Lin) using the caliper tool on the OCT machine. The amount of CFT reduction was calculated as the difference between preoperative and last follow-up. The BCVA was measured using Snellen charts and converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. The non-contact tonometer (TX-20P, Canon, Japan) was employed to measure the IOP.
Surgical technique
All eyes underwent standard 23-gauge 3-port pars plana vitrectomy, most of which received concurrent phacoemulsification with intraocular lens implantation. Following core and peripheral vitrectomy, 40 mg/mL suspension of TA (Xianju Pharmaceutical Co., Ltd, Zhejiang, China) was used to dust the macula region and excess particles were removed with a flute needle. Visible ERM in the macular region was carefully removed using an ILM forceps without further removal of the internal limiting membrane. At the end of the surgical procedure, about 0.5 mg/0.05 ml of TA was injected into the vitreous cavity through the 23-gauge cannulas in the TA group at the surgeon's discretion. All the patients received tapering antibiotic eye drops and 1.0% Prednisolone acetate eye drops for four weeks after surgery.
Statistical analysis
The primary outcomes in our study were the EIFL stages, CFT, and BCVA. Comparison of the preoperative, one month later, and last follow-up EIFL stages, CFT, and BCVA were used the Kruskal–Wallis test. According to the normality test (Shapiro–Wilk test), the Student’s-t or Mann–Whitney U test assessed the differences between the TA and non-TA groups regarding EIFL stages, CFT, and BCVA. The statistical analysis was performed using SPSS (SPSS Inc, Chicago, Illinois, USA). P values of less than 0.05 were considered statistically significant.
Results
Eighty-four eyes of 84 patients were enrolled in the study, and the mean follow-up duration was 7.69 ± 3.68 months. This cohort included 51 eyes in the TA group and 33 eyes in the non-TA group. Furthermore, 86.90% of cases (73 out of 84) underwent concurrent phacoemulsification and intraocular lens implantation, and no statistical difference in the proportion of phacovitrectomy was observed between the two groups (P = 0.65). The baseline characteristics of the subjects demonstrated no significant differences between the groups, as shown in Table 1 (P > 0.05).
Figure 2 shows both groups' remarkable postoperative improvement in EIFL stages during the first month after surgery and the final visit (P < 0.01). However, a statistical difference in the EIFL stages was discovered between the two groups at the final follow-up (P = 0.04), as detailed in Table 2. At the last follow-up, 56.86% and 63.64% of eyes in the TA and non-TA groups exhibited improvement in the EIFL stages, respectively. Nevertheless, there was no significant difference between the two groups (P = 0.43).
The preoperative and postoperative proportion of different ectopic inner foveal layer (EIFL) stages in two groups. A: The postoperative EIFL Stages significantly improved in the non-TA group (P < 0.01). The preoperative proportions of Stage 1 to Stage 4 were 0, 36.36, 51.52, and 12.12%, respectively. Stage 1 to Stage 4 proportions were 6.06, 57.58, 36.36, and 0% one month after surgery. The proportions of Stage 1 to Stage 4 became 18.18, 60.61, 21.21, and 0% at the final follow-up. B: EIFL Stages significantly improved after surgery in the TA group (P < 0.01). The preoperative proportions of Stage 1 to Stage 4 were 0, 19.61, 62.74 and 17.65%, respectively. Stage 1 to Stage 4 proportions were 3.92, 43.14, 52.94, and 0% one month after surgery. The proportions of Stage 1 to Stage 4 became 3.92, 60.78, 35.30, and 0% at the last visit
The postoperative CFT experienced significant reductions in both groups. At the last follow-up, the CFT decreased from 467.80 ± 106.96 µm to 382.02 ± 73.94 µm in the TA group and from 443.52 ± 91.89 µm to 344.76 ± 78.71 µm in the non-TA group (all P < 0.01). Table 2 exhibited significant differences in the CFT between the two groups in the first month after surgery (P = 0.02) and the final follow-up (P = 0.03). Notable improvements in BCVA were observed in both groups during the follow-up (all P < 0.05). However, no significant difference was noted between the TA and non-TA groups.
Subgroup analysis was conducted based on the presence of a continuous ectopic inner foveal layer. The ratio of Stages 3 and 4 showed no statistical difference between the two groups (P = 0.76). There was no significant difference between the TA and non-TA groups regarding postoperative CFT and BCVA (P > 0.10) at either one month after surgery or the last follow-up, as detailed in Table 3.
There were twelve eyes in the TA group and six eyes in the non-TA group presenting with preoperative intraretinal cysts. At the final follow-up, seven eyes in the TA group and five eyes in the non-TA group still had intraretinal cysts. Moreover, 27.45% (14/51) and 24.24% (8/33) of eyes showed ERM recurrences on OCT images in the TA and non-TA groups during the follow-up period without significant difference (P = 0.74).
Discussions
Our study first investigated the anatomical and visual outcomes of combined epiretinal membrane removal with intravitreal TA injection utilizing the EIFL staging scheme. The results indicated that concomitant intravitreal TA injection produced no significant advantage in improving the EIFL stages, macular thickness reduction, and visual improvement at neither early nor advanced EIFL stages.
Numerous studies have investigated the effect of intravitreal TA injection or Dexamethasone implants to treat persistent macular edema after vitrectomy [19, 21,22,23,24,25]. Nevertheless, the advanced EIFL stages were associated with worse postoperative anatomical and visual recovery [8, 11]. Evaluating the effect of concurrent intravitreal TA injection after iERM peeling utilizing the EIFL staging system would be more comprehensive.
In our study, the postoperative EIFL stages significantly improved in both groups. At the last follow-up, 56.86% and 63.64% of eyes in the TA and non-TA groups showed improvement in the EIFL stages, respectively. However, the group with concomitant intravitreal TA injection showed no more advantage in improving the EIFL stages. González-Saldivar et al.[10] reported that 70.80% of eyes with Stage 2 improved in the EIFL stages, but 68.00% of eyes with Stage 3 and 4 remained the same after vitrectomy with ERM peeling. The postoperative ectopic inner foveal layers of most eyes with advanced stages of ERM could persist for a long time [9]. The traction at the retinal interface was relieved after ERM removal so that the distortion of the inner retina recovered gradually. However, the severe traction in the cases with advanced stages might significantly reduce the retinal structural resilience. Only a few cases that did not restore foveal depression at one month postoperatively continued to recover over the long-term follow-up period [8]. Concomitant intravitreal TA injection effectively improved anatomical outcomes after ERM peeling, according to some studies [19, 23, 26]. However, our study observed no significant difference between the TA and non-TA groups regarding the postoperative CFT and BCVA at different EIFL stages. This result was consistent with previous studies [20, 21, 28]. Persistent macular thickening in iERM might result from mechanical traction and inflammation. The eyes with advanced iERM were more likely to develop postoperative macular edema [29]. However, the advanced stages were associated with worse anatomical recovery after the operation [8, 9, 11], which indicated that the structural changes caused by long-term ERM traction might play a more significant role in postoperative non-cystoid macular thickening. It seemed that the intraretinal cysts were alleviated better in the group with TA injection in our study, and a dexamethasone implant might aid in faster retinal thickness reduction [30]. Nevertheless, intravitreal corticosteroid injection had a limited effect in reducing macular thickness after ERM removal [24].
At the last follow-up, the EIFL stages revealed statistical differences between the TA and non-TA groups. Furthermore, the CFT was reduced more in the non-TA group than in the TA group. A recent multicenter study also found that no adjuvant therapy showed better macular thickness reduction and BCVA improvement than intravitreal TA injection [22]. One reasonable explanation for this result was that the non-TA group had more cases of early EIFL stage at baseline, and postoperative anatomical abnormalities might persist longer in the cases with advanced stages. González-Saldivar et al. [10] found that surgeries at the early stages of ERM resulted in a more likely chance of reversibility in macular architecture and better visual outcomes. Govetto et al. [9] also reported that the ectopic inner foveal layers in 91% of ERM with Stages 3 and 4 still existed after 1-year follow-up. In the subgroup analysis considering the early and advanced EIFL stages, the difference in CFT and BCVA between the two groups was insignificant, which could support this hypothesis.
There were several limitations in our study. First, it was a retrospective cases control study with a small sample size. With a retrospective nature, this study inevitably faced additional surgeon-induced bias, which included the option of intravitreal TA injection. Secondly, not all patients received combined cataract and vitreoretinal surgery, which might have affected the visual results. Another limitation of this study was the absence of a longer follow-up duration. A longer follow-up might be helpful to evaluate both the differences in CFT reduction and the changes in visual acuity. However, a three-month follow-up period also revealed important information at early and late stages after surgery because measurable TA concentrations would last less than three months after a single intravitreal injection of 4 mg in the presence of a vitrectomy [27]. Furthermore, most changes in postoperative macular architecture and visual acuity occurred during the first three months after surgery [8, 31].
In conclusion, our study indicated that concurrent TA injection after ERM removal provided no additional advantage to postoperative macular thickness reduction and visual acuity improvement for patients with early or advanced stages of iERM. Prospective cohort studies are warranted to understand better whether concomitant TA injection has an advantage in improving intraretinal cysts in iERM.
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Fung AT, Galvin J, Tran T (2021) Epiretinal membrane: a review. Clin Exp Ophthalmol 49:289–308. https://doi.org/10.1111/ceo.13914
Kim M, Park YS, Lee DH et al (2015) Comparison of surgical outcome of 23-gauge and 25-gauge microincision vitrectomy surgery for management of idiopathic epiretinal membrane in pseudophakic eyes. Retina 35:2115–2120. https://doi.org/10.1097/IAE.0000000000000598
Lubiński W, Gosławski W, Podborączyńska-Jodko K et al (2020) Comparison of 27-gauge versus 25-gauge vitrectomy results in patients with epiretinal membrane: 6-month follow-up. Int Ophthalmol 40:867–875. https://doi.org/10.1007/s10792-019-01250-1
Council MD, Shah GK, Lee HC et al (2005) Visual outcomes and complications of epiretinal membrane removal secondary to rhegmatogenous retinal detachment. Ophthalmology 112:1218–1221. https://doi.org/10.1016/j.ophtha.2005.01.051
Zur D, Iglicki M, Feldinger L et al (2018) Disorganization of retinal inner layers as a biomarker for idiopathic epiretinal membrane after macular surgery-the dream study. Am J Ophthalmol 196:129–135. https://doi.org/10.1016/j.ajo.2018.08.037
Cho KH, Park SJ, Cho JH et al (2016) Inner-retinal irregularity index predicts postoperative visual prognosis in idiopathic epiretinal membrane. Am J Ophthalmol 168:139–149. https://doi.org/10.1016/j.ajo.2016.05.011
Govetto A, Lalane RA 3rd, Sarraf D et al (2017) Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol 175:99–113. https://doi.org/10.1016/j.ajo.2016.12.006
Yang X, Wang Z, Yu Y et al (2022) Effects of ectopic inner foveal layers on foveal configuration and visual function after idiopathic epiretinal membrane surgery. Retina 42:1472–1478. https://doi.org/10.1097/IAE.0000000000003495
Govetto A, Virgili G, Rodriguez FJ et al (2019) Functional and anatomical significance of the ectopic inner foveal layers in eyes with idiopathic epiretinal membranes: surgical results at 12 months. Retina 39:347–357. https://doi.org/10.1097/IAE.0000000000001940
González-Saldivar G, Berger A, Wong D et al (2020) Ectopic inner foveal layer classification scheme predicts visual outcomes after epiretinal membrane surgery. Retina 40:710–717. https://doi.org/10.1097/IAE.0000000000002486
Mavi Yildiz A, Avci R, Yilmaz S (2021) The predictive value of ectopic inner retinal layer staging scheme for idiopathic epiretinal membrane: surgical results at 12 months. Eye (Lond) 35:2164–2172. https://doi.org/10.1038/s41433-021-01429-w
Frisina R, Pinackatt SJ, Sartore M et al (2015) Cystoid macular edema after pars plana vitrectomy for idiopathic epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 253:47–56. https://doi.org/10.1007/s00417-014-2655-x
Fang IM, Hsu CC, Chen LL (2016) Correlation between visual acuity changes and optical coherence tomography morphological findings in idiopathic epiretinal membranes. Graefes Arch Clin Exp Ophthalmol 254:437–444. https://doi.org/10.1007/s00417-015-3069-0
Cicinelli MV, Post M, Brambati M et al (2022) Associated factors and surgical outcomes of microcystoid macular edema and cone bouquet abnormalities in eyes with epiretinal membrane. Retina 42:1455–1464. https://doi.org/10.1097/IAE.0000000000003492
Lee DH, Park SE, Lee CS (2021) Microcystic macular edema and cystoid macular edema before and after epiretinal membrane surgery. Retina 41:1652–1659. https://doi.org/10.1097/IAE.0000000000003087
Leisser C, Hirnschall N, Hackl C et al (2018) Risk factors for postoperative intraretinal cystoid changes after peeling of idiopathic epiretinal membranes among patients randomized for balanced salt solution and air-tamponade. Acta Ophthalmol 96:e439–e444. https://doi.org/10.1111/aos.13635
Gallina D, Zelinka C, Fischer AJ (2014) Glucocorticoid receptors in the retina, Müller glia and the formation of Müller glia-derived progenitors. Development 141:3340–3351. https://doi.org/10.1242/dev.109835
Whitcup SM, Cidlowski JA, Csaky KG et al (2018) Pharmacology of corticosteroids for diabetic macular edema. Invest Ophthalmol Vis Sci 59:1–12. https://doi.org/10.1167/iovs.17-22259
Angermann R, Zehetner C, Sidoroff P et al (2018) Triamcinolone in small-gauge vitrectomy for epiretinal membrane peeling. Can J Ophthalmol 53:632–636. https://doi.org/10.1016/j.jcjo.2018.01.023
Lai CC, Wang NK, Wu WC et al (2011) The long-term anatomical and visual effect of intravitreal triamcinolone injection during vitrectomy for the treatment of idiopathic macular epiretinal membrane. Cutan Ocul Toxicol 30:292–297. https://doi.org/10.3109/15569527.2011.568031
Ahn JH, Park HJ, Lee JE et al (2012) Effect of intravitreal triamcinolone injection during vitrectomy for idiopathic epiretinal membrane. Retina 32:892–896. https://doi.org/10.1097/IAE.0b013e318229b1f7
Mandelcorn ED, Al-Falah M, Zhao LD et al (2022) A prospective randomized clinical trial comparing nepafenac, intravitreal triamcinolone and no adjuvant therapy for epiretinal membrane. Acta Ophthalmol 100:e297–e303. https://doi.org/10.1111/aos.14873
Sella R, Gal-or O, Goh YW et al (2015) Role of concomitant triamcinolone acetonide injection in small-gauge vitrectomy for idiopathic epiretinal membrane peel. Asia Pac J Ophthalmol (Phila) 4:204–207. https://doi.org/10.1097/APO.0000000000000049
Guidi G, Casini G, Ripandelli G et al (2018) Residual intraretinal edema after 25-gauge vitrectomy and macular pucker removal: Is intraoperative sustained-release dexamethasone a real treatment option? Retina 38:993–999. https://doi.org/10.1097/IAE.0000000000001627
Savastano A, Bitossi A, Giansanti F et al (2021) Evaluation of intraoperative slow-release dexamethasone implant combined with idiopathic epiretinal membrane removal. Graefes Arch Clin Exp Ophthalmol 259:379–385. https://doi.org/10.1007/s00417-020-04911-5
Konstantinidis L, Berguiga M, Beknazar E et al (2009) Anatomic and functional outcome after 23-gauge vitrectomy, peeling, and intravitreal triamcinolone for idiopathic macular epiretinal membrane. Retina 29:1119–1127. https://doi.org/10.1097/IAE.0b013e3181ac23da
Beer PM, Bakri SJ, Singh RJ et al (2003) Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology 110:681–686. https://doi.org/10.1016/S0161-6420(02)01969-3
Chen HJ, Hsiao CH, Chang CJ (2022) Efficacy of combined vitrectomy with intravitreal corticosteroid injection for idiopathic epiretinal membrane removal on anatomical and functional outcomes: a meta-analysis. Ophthalmologica 245:218–229. https://doi.org/10.1159/000522263
Iuliano L, Cisa di Gresy G, Fogliato G et al (2021) Increased risk of postsurgical macular edema in high stage idiopathic epiretinal membranes. Eye Vis (Lond) 8:29. https://doi.org/10.1186/s40662-021-00252-4
Sane SS, Ali MH, Kuppermann BD et al (2020) Comparative study of pars plana vitrectomy with or without intravitreal dexamethasone implant for idiopathic epiretinal membrane. Indian J Ophthalmol 68:1103–1107. https://doi.org/10.4103/ijo.IJO_1045_19
Kim J, Rhee KM, Woo SJ et al (2010) Long-term temporal changes of macular thickness and visual outcome after vitrectomy for idiopathic epiretinal membrane. Am J Ophthalmol 150(701–709):e1. https://doi.org/10.1016/j.ajo.2010.05.037
Acknowledgements
Not applicable.
Funding
This work was supported by The Medical Scientific Research Foundation of Guangdong Province (NO: B2021009) and the Intramural Grant of Joint Shantou International Eye Center (NO: 20–018).
Author information
Authors and Affiliations
Contributions
The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. DZZ performed the data analyses and wrote the manuscript. HJL contributed to collecting the data. WQC, GHZ, and DGH performed the surgeries. ZJH contributed significantly to the manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no proprietary or commercial interest in any materials discussed in this article.
Ethical approval
This study protocol was reviewed and approved by the Ethics Committee of the Joint Shantou International Eye Center, with the designated approval number EC 20201124(11)-P04.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not Applicable. There is no information or images that could lead to identification of a study participant in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, Dz., Lin, Hj., Zhang, Gh. et al. Evaluation of combined epiretinal membrane removal with intravitreal triamcinolone injection utilizing ectopic inner foveal layer staging scheme. Int Ophthalmol 44, 249 (2024). https://doi.org/10.1007/s10792-024-03188-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03188-5