Abstract
Purpose
To analyze the functional impact of ectopic inner foveal layers (EIFL), along with other clinical and optical coherence tomography biomarkers, on patients with epiretinal membrane (ERM) and preserved foveal layers’ segmentation undergoing ERM removal.
Methods
Retrospective review of consecutive patients with ERM who underwent pars plana vitrectomy with ERM peeling from December 2018 to December 2019. Baseline factors including age, gender, lens status, phacoemulsification at the time of surgery, tamponade agent, dye used for ERM and internal limiting membrane (ILM) enhancement, ILM peeling, best-corrected visual acuity (BCVA) and central macular thickness (CMT), presence and thickness of EIFL, thickness of outer nuclear layer (ONL), presence of a cotton ball, subfoveal state of photoreceptors, and presence of cystoid macular edema were included in a multivariable model having the BCVA at 12 months as the main outcome. The changes in EIFL and ONL thickness over time were also analyzed.
Results
Fifty-one patients (58 eyes, 23 eyes in the no EIFL group, and 35 eyes in the EIFL group) were enrolled. The BCVA significantly improved over 12 months after surgery, regardless of the presence of EIFL (p < 0.001). Eyes with no EIFL had better BCVA at month 3 (p = 0.04), but this difference was no longer detectable at 6 and 12 months. The presence of EIFL was not associated with the final BCVA (p = 0.9), while the CMT at 12 months correlated with EIFL thickness (r = 0.8, p = 0.008).
Conclusion
Patients with EIFL could reach optimal visual acuity in the absence of disorganization of the inner retinal layers but should be warned of potentially longer healing times. None of the morphologic signs included in this study precluded good visual recovery on long-term follow-up.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epiretinal membrane (ERM) is a relatively common vitreoretinal interface disease, characterized by fibrocellular proliferation over the internal limiting membrane (ILM) [1, 2]. While early stages are often asymptomatic, advanced disease may lead to macular distortion, with consequent metamorphopsia and visual impairment. Pars plana vitrectomy (PPV) with ERM peeling is the procedure of choice for symptomatic patients and usually leads to visual improvement, anatomical restoration, and low recurrence rate [3].
Spectral-domain optical coherence tomography (SD-OCT) allows a detailed evaluation of patients with ERM and helps in preoperative prognostication of visual and anatomical outcomes. Proposed SD-OCT biomarkers of unfavorable prognosis include disruption of the ellipsoid zone (EZ) and the external limiting membrane (ELM), thinning of the outer nuclear layer (ONL), presence of cystoid macular edema (CME), and detection of a cotton ball (CB), referred to as a round, hyperreflective thickening of the external retinal layers [4]. The available literature mostly provides qualitative descriptions of these features and univariable correlations with best-corrected visual acuity (BCVA) [5, 6]; only one study analyzed the simultaneous effect of these characteristics on both baseline and 12-month postoperative BCVA [7]. A comprehensive analysis of the longitudinal BCVA changes after surgery is currently lacking.
Latest studies have been focused on the presence of ectopic inner foveal layers (EIFL), defined as a continuous hypo- or hyper-reflective inner retinal band traversing the fovea in patients with ERM. EIFL spans from negligible morphologic or anatomic disruption (stage 1) to anatomic disorganization of the macular segmentation (stage 4) [5]. Advanced EIFL has been acknowledged as a predictor of poor visual acuity before and after ERM removal [7]. On the other hand, the impact of EIFL in patients with a relatively preserved macular anatomy, which represents the majority of patients with ERM, has not been specifically addressed.
The aim of the present study is to analyze the functional impact of EIFL, along with other clinical and SD-OCT biomarkers, on patients with symptomatic ERM and preserved foveal layers’ segmentation undergoing PPV and ERM peeling. The identification of prognostic factors in this category of patients might help in better tailoring of the surgical timing and the postoperative follow-up.
Methods
Study participants
Retrospective, observational study including patients who underwent PPV and idiopathic ERM ± inner limiting membrane (ILM) peeling between December 2018 and December 2019, at S. Gerardo Hospital (Monza, Italy). The study adhered to the tenets of the Declaration of Helsinki and received the approval of the local IRB. Patients signed written consent at the time of enrollment to be included in observational clinical research studies.
Cases presenting with secondary ERM (i.e., those listed in Supplementary Table 1) and those with a history of intraocular surgery excepting uncomplicated phacoemulsification were excluded. Optic media opacity impeding good-quality imaging before or after PPV, presence of a lamellar or full-thickness macular hole, and presence of other potential causes of irreversible visual loss (e.g., advanced glaucoma, macular degeneration, optic neuropathy, corneal disease) were considered additional exclusion criteria. Both eyes of each patient were included if eligible.
The following variables were gathered at baseline: age, gender, surgeon, phacoemulsification at the time of PPV, tamponade agent at the end of PPV, and dye used for ERM and ILM enhancement. BCVA values measured on decimal charts and SD-OCT scans were collected at baseline, at 3 months, 6 months, and 12 months after surgery.
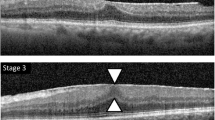
Imaging evaluation
All patients were imaged with Spectralis OCT with eye-tracking dual-beam technology and follow-up mode (Heidelberg Engineering, Heidelberg, Germany). The CMT value, corresponding to the innermost 1-mm wide circle of the ETDRS map, was automatically calculated from a 19 B-scans raster centered to the fovea. A horizontal B-scan passing through the fovea was chosen as a reference for further measurements. Macular scans were evaluated independently by two retinal specialists (EZ and APD). Patients were classified into 4 stages [5]:
-
Stage 1: mild ERM with foveal depression preservation and no anatomical distortion;
-
Stage 2: ERM with thickening of the outer nuclear layer (ONL) and loss of the foveal depression;
-
Stage 3: presence of continuous EIFL, identified as a clear foveal band extending from the inner nuclear layer and inner plexiform layer;
-
Stage 4: advanced ERM, with EIFL, no foveal depression, and complete loss of macular segmentation.
Patients bearing stage 4 EIFL were excluded from our cohort, as the study focused on eyes with a preserved macular segmentation on SD-OCT. Stages 1 and 2 were combined (no EIFL group) and compared with stage 3 (EIFL group). EIFL thickness at the presumed foveal depression was manually measured with the caliper function of the Heidelberg Spectralis by two trained investigators (EZ and APD). The measurement of EIFL spanned from the outer border of the inner nuclear layer to the inner margin of the inner limiting membrane for preoperative measurement [6] and from the outer border of the inner nuclear layer to the vitreoretinal interface postoperatively. The thickness of the ONL, defined as the width of the outer dark-gray band between the outer plexiform layer’s outer boundary and ELM, was measured similarly (Fig. 1).
Qualitative and quantitative assessment of optical coherence tomography of included study patients. Measurement of ectopic inner foveal layer (EIFL) and outer nuclear layer (ONL) were performed manually. ONL was defined as the width of the outer dark-gray band between the outer boundary of outer plexiform layer and the external limiting membrane. EIFL thickness was measured in the presence of a continuous inner nuclear layer and inner plexiform layer band at the presumed foveal depression. Measurement of EIFL spanned from the outer border of the inner nuclear layer to the inner margin of the inner limiting membrane. As the photoreceptor appeared thickened and fuzzy subfoveally, the scan was marked as positive for the presence of the cotton ball (CB) sign
Baseline SD-OCT B-scans were qualitatively evaluated for the presence of CB, defined as a roundish hyperreflective area between the EZ and the interdigitation zone in the central fovea (Fig. 1); [8] EZ and/or ELM disruption, defined as an interruption in these bands subfoveally; and CME, labeled as hyporeflective intraretinal cysts in the macular area.
Surgical procedure
PPV was performed within 2 ± 1 weeks from the baseline assessment, by one of four experienced vitreoretinal surgeons. A 3-port 25-gauge PPV with ERM peeling was performed with the Constellation 25 G+ Total Plus Vitrectomy Pack (Alcon Laboratories, Inc, Fort Worth, TX).
The ERM and ILM were stained with a 0.3-mL intravitreal dye: MembraneBlue-Dual (DORC International, Zuidland, the Netherlands; 0.15% trypan blue, 0.025% Brilliant Blue G) in 38 cases (65%); Doubledyne (Alfa Intes, Casoria, Italy; 2% soluble lutein, 0.15% trypan blue, 0.05% Brilliant Blue G) in 15 cases (26%); trypan blue 0.15% (MembraneBlue, Dutch Ophthalmic Research Center International) in 4 cases (7%); ILM Blue, DORC International, Zuidland, the Netherlands: 0.025% Brilliant Blue G) in 1 case (2%). Fine-tipped forceps (Alcon ILM forceps 25G) were used to peel the ERM up to the vascular arcades. The ILM was peeled at the discretion of the surgeon. Combined phacoemulsification and intraocular lens implantation were performed in case of visually significant lens opacity. At the end of the surgery, the eye was filled with a tamponade agent (air, fluid, or sulfur hexafluoride), and all patients received a subconjunctival injection of anti-inflammatory and antibiotics, as standard protocol.
Statistical analysis
Statistical calculations were carried out with the open-source programming language R [9]. Continuous variables were reported as mean ± standard deviation [SD], categorical variables as frequency and proportions. The BCVA was converted to LogMAR and used as a continuous variable. Differences in the baseline characteristics as a function of the presence of EIFL were explored with linear or logistic regression models, according to the nature of the dependent variable (continuous vs. categorical, respectively).
The BCVA and CMT variation over 12 months after ERM removal was investigated with linear mixed models with a repeated measures design. The differences between EIFL vs. no EIFL patients at different time points were investigated using least-square means, correcting results for multiple comparisons (Tukey’s correction).
The primary outcome was to identify the baseline factors associated with the BCVA at 12 months after surgery, including demographic data (age and gender), surgical details (phacoemulsification at the time of PPV, tamponade agent at the end of PPV, combined ILM peeling, surgeon), baseline characteristics (BCVA and CMT), and presence of SD-OCT biomarkers (CB, EZ/ELM disruption, EIFL, CME). A linear mixed model was designed, where the patient identification number was included as a random effect (to correct for the inclusion of both eyes in some participants). The variables for the final model were selected with a parsimonious approach, using a least absolute shrinkage and selection operator regression (LASSO) [10]. As a secondary outcome, the clinical factors influencing the baseline BCVA and the delta BCVA (calculated as the difference between baseline BCVA and the 12-month BCVA) were investigated. Linear regression estimates and 95% confidence intervals (CI) are provided for significant associations.
For descriptive statistics, only complete cases were used. For predictive model statistics, the missing values were handled with multiple imputations through a chain equation with the mice R package [11]. Fifteen randomly generated datasets were imputed, one set for the models having the BCVA at baseline as the dependent variable and another set for the models having the BCVA at 12 months and the delta BCVA as the dependent variables, which included only subjects who had a complete 12-month follow-up. Demographics and clinical characteristics were compared between patients with a 12-month follow-up and those who were lost to follow-up before 12 months. To test the reliability of predictive statistics with missing data imputation, all analyses were also performed on the non-imputed database, including complete cases only.
The cutoff point for statistical significance was set at p < 0.05 (two-sided).
Results
A total of 51 patients (58 eyes), mean age 73.5 ± 6.1 years, were enrolled. Demographic and clinical features are listed in Table 1. Three eyes (5.2%) had stage 1, 20 eyes (34.5%) had stage 2, and 35 eyes (60.3%) had stage 3; therefore, 23 eyes of 22 patients were included in the no EIFL group and 35 eyes of 33 patients in the EIFL group.
No differences were found between the two groups in terms of demographics, surgical technique, tamponade agent, and need for concurrent cataract surgery (Table 1). Baseline BCVA was similar in the two groups, while CMT was higher in patients with EIFL (p = 0.02) and correlated with EIFL thickness (r = 0.4, p = 0.03). Morphologic characteristics, namely, the presence of CME, CB, and EZ/ELM disruption, were evenly distributed. The ONL was thinner in patients with EIFL (p=0.004).
The percentage of missing values is presented in Supplementary Fig. 1. There were no baseline differences between patients with complete follow-up (n = 24 eyes) and those lost to follow-up before 12 months (n = 34 eyes). The BCVA and the CMT at 3 and 6 months were also similar between the two groups (Supplementary Table 2).
Visual and anatomical outcomes after surgery
The BCVA significantly improved over the 12 months after surgery, regardless of the presence of EIFL (p < 0.001) (Table 2, Fig. 2). Eyes with intact retinal inner layers had better BCVA at month 3 compared with eyes with EIFL (p = 0.04); the BCVA at 6 and 12 months was similar between the two groups. The main visual improvement was 0.43 ± 0.22 LogMAR.
Best-corrected visual acuity (BCVA, left) and central macular thickness (CMT, right) at the time of epiretinal membrane peeling and throughout a 12-month follow-up. Patients are stratified according to the presence of ectopic inner foveal layer (EL). The bolded horizontal line inside the boxplot represents the median value. Dots represent outlier data. Boxplots refer to complete cases
The CMT and ONL thickness decreased over 12 months (p < 0.001 and p = 0.002, respectively) (Table 2, Figs. 2 and 3). The CMT reduced equally in eyes with EIFL and those without EIFL (p = 0.5 at month 3, p = 0.5 at month 6, and p = 0.5 at month 12); the last CMT correlated closely with the EIFL thickness at 12 months (r = 0.8, p = 0.008). EIFL thickness progressively reduced after ERM removal, being 111.26 ± 73.42 μm at month 3 (p = 0.3), 122.69 ± 64.19 μm at month 6 (p = 0.4), and 62.6 ± 20.2 μm at month 12 (p = 0.003) (Fig. 3).
Outer nuclear layer (ONL, left) and ectopic inner foveal layer (right) thickness at the time of epiretinal membrane peeling and throughout a 12-month follow-up. In the left panel, patients are divided according to the presence of ectopic inner foveal layer (EL). The bolded horizontal line inside the boxplot represents the median value. Dots represent outlier data. Boxplots refer to complete cases
No serious intraoperative or postoperative complications were registered over the follow-up.
Clinical predictors of BCVA before and after surgery
Female gender (estimate = 0.13, 95% CI = 0.01–0.24, p = 0.04) was the only factor associated with worse baseline BCVA at the multivariable analysis (Table 3).
Among the investigated variables associated with the visual outcome at 12 months, phacoemulsification at the time of PPV was associated with better vision (estimate = −0.15, 95% CI = −0.29 – −0.01, p = 0.03) and higher visual gain (estimate = 0.15, 95% CI = 0.01–0.29, p = 0.04). On the contrary, the presence of EIFL did not affect the final BCVA in our cohort (p = 0.2), neither the BCVA improvement (p = 0.2), once corrected for the other covariates (Table 3). Finally, the magnitude of visual improvement at 12 months was strongly related to the baseline BCVA (estimate = 0.86, 95% CI = 0.61–1.11, p < 0.001) (Table 3).
Discussion
In the present study, we longitudinally analyzed patients with idiopathic, symptomatic ERM and relatively preserved macular segmentation undergoing PPV. All the eyes experienced significant visual and morphologic improvement after surgery, maintained up to 12 months. Eyes with intact retinal inner layers before surgery had better BCVA at month 3 compared with eyes with EIFL, but this difference was no longer detectable at subsequent time points. Once correcting for all clinical parameters, female gender was associated with worse visual acuity at baseline. By contrast, undergoing cataract extraction at the time of PPV was associated with better functional outcome at 12 months. The visual improvement was closely related to the baseline BCVA.
The pathogenesis of ERM is multifactorial, and the mechanisms leading to visual loss are complex and not completely understood. The introduction of state-of-the-art imaging modalities, as SD-OCT and—more recently—OCT angiography, has allowed a better understanding of the morphologic changes happening in eyes with tractional maculopathy before and after surgery [12,13,14]. A progressive displacement of the inner retinal layers towards the center of the macula has been described in eyes with ERM, reported as EIFL. The presence of EIFL, as well its thickness, has been associated with worse baseline visual acuity, suggesting a negative impact of foveal pit obliteration and loss of retinal segmentation on macular physiology [5, 15]. Most evidence derives from univariable correlations between the BCVA and the EIFL findings. By contrast, our multivariable analysis did not corroborate the association between EIFL and baseline BCVA, once patients with advanced macular pathology had been excluded. These findings are in accordance with the previous reports, in which no statistical difference was found in baseline BCVA between eyes with stage 2 ERM and those with stage 3 ERM [6].
Female gender was the only parameter significantly (and negatively) associated with baseline BCVA. Morphological and structural differences in the chorioretinal architecture have been observed between healthy men and women [16]. Different studies have reported a thicker fovea in males compared with females, and a possible role of sex hormones in maintaining retinal health has been implicated [16,17,18]. Slightly thicker inner nuclear layer (INL), outer plexiform layer, (OPL) and ONL have also been described in males, while thicker retinal nerve fiber layer characterizes female subjects [19]. Female gender has also been acknowledged as a risk factor for ERM [20]. Although the significance of anatomic differences is yet to be determined, a delay in seeking treatment among women might also contribute to explaining our results [21].
The ONL thickness at baseline was lower in eyes featuring EIFL. These results are consistent with previous evidence [5, 7]. Progressive ONL thinning may imply progressive centripetal displacement of the inner retinal layers and outer layers centrifugal shift to the perifoveal area [22]. This agrees with OCT angiography findings in EIFL, in which foveal avascular zone obliteration is more pronounced in the superficial capillary layer than the deep capillary layer [14]. A previous study demonstrated a significant association between deformation of ONL and metamorphopsia [23]; we encourage additional research to correlate the deformation of ONL in eyes with ERM with visual distortion.
EIFL thickness decreased significantly in the postoperative period but did not disappear completely after surgery. Postoperative BCVA has been inversely correlated with EIFL severity [6]. Nevertheless, a significant difference between stage 2 and stage 3 EMR has not been reported. Govetto et al. found that stage 4 ERM eyes reached a plateau in BCVA 6 months after surgery, as opposite of eyes with stage 2 and stage 3 ERM which continued improving until the last visit [7]. In this study, we found very similar results, as both stage 2 and stage 3 ERM had a positive trend in visual acuity after the surgery. At 12 months, the patients with stage 3 ERM had similar BCVA compared with stage 1 and stage 2 ERM, with functional improvement lagging slightly behind; more severe architectural changes in patients with EIFL may delay functional recovery. Finally, the magnitude of visual recovery after surgery strongly correlated with the preoperative visual acuity, as reported by the previous literature [4].
Combined phacoemulsification and PPV is a reasonable alternative in selected patients to avoid sequential surgeries; combined surgery has similar or sometimes better functional outcomes when performed at the time of PPV [24], with a similar number of complications [25] and a similar amount of postoperative refractive error [26]. The type of tamponade agent used at the time of the surgery, the dye used for membrane enhancement, and the peeling of ILM did not influence significantly the final BCVA [27, 28]. Other factors should be explored to predict the anatomical and functional outcomes after ERM removal, including the duration and the severity of preoperative symptoms (metamorphopsia) [4].
One of the novelties of this study relies on the distinction between patients with and without EIFL based solely on the presence of a continuous inner retina band at the fovea, provided that retinal segmentation was discernible. On the contrary, stage 4 ERM is characterized by notable retinal thickening and disruption of the normal retina architecture, and this may irreversibly preclude good surgical outcomes. Stage 4 patients represent around 10% of ERM eyes. The exclusion of patients with stage 4 ERM could lead to a more homogenous sample of patients in clinical practice. Accordingly, the EIFL thickness measured in our study (137.6 ± 79.3 μm) was considerably lower than EIFL thickness measured in the cohort by Govetto et al. (191.7 ± 75.5 μm) [7]; the exclusion of stage 4 patients contributes to this discrepancy. None of the other morphologic features potentially associated with ERM severity (i.e., CB sign, EIFL thickness, ONL thickness in the foveal area, CMT) clinically predicted the visual function one year after ERM removal.
This study has several limitations, including the retrospective nature of the analysis. Retrospective collections of data are inevitably more flawed than prospective analyses. First, retrospective studies are prone to selection biases; as the consequence, the enrolled sample (e.g., age and gender) and its partition (e.g., ERM stages and classification) might be non-representative of the actual population, reducing the potential application of the study to different demographic and clinical settings. Some key statistics were missing when looking back to clinical charts; we handled missing data as missing data completely at random or missing at random, but we cannot exclude the presence of data missing not at random (MNAR). For instance, eyes with very low or very high BCVA could have missed their scheduled appointments. Although potent and reliable statistical tools exist to cope with missing data (namely, multiple imputations), MNAR is difficult to predict based on the available information [29]. Like other retrospective studies, ours might also be flawed by inconsistency in clinical variable collection (for example, BCVA). Additional limitations include the number of patients lost to follow-up, the subjective interpretation and the manual measurement of the SD-OCT findings, and the lack of quantification of visual symptoms, such as metamorphopsia and contrast sensitivity, at baseline and over the follow-up.
In conclusion, we provided data about the post-operative ERM peeling outcomes in patients with EIFL and preserved macular segmentation on SD-OCT. In our study, the presence of EIFL did not affect the final outcome after surgery but was associated with a slower recovery of visual acuity. Patients with EIFL could reach good visual acuity in the absence of complete disorganization of the inner retinal layers; nevertheless, they should be warned of potentially longer healing times.
Data availability
Data are available upon request to the corresponding authors.
Code availability
Statistical software (R) and statistical packages used for this study are open access and adequate reference is provided.
References
Iuliano L, Fogliato G, Gorgoni F, Corbelli E, Bandello F, Codenotti M (2019) Idiopathic epiretinal membrane surgery: safety, efficacy and patient related outcomes. Clin Ophthalmol 13:1253–1265. https://doi.org/10.2147/OPTH.S176120
Hosoda Y, Ooto S, Hangai M, Oishi A, Yoshimura N (2015) Foveal photoreceptor deformation as a significant predictor of postoperative visual outcome in idiopathic epiretinal membrane surgery. Invest Ophthalmol Vis Sci 56(11):6387–6393. https://doi.org/10.1167/iovs.15-16679
Tsunoda K, Watanabe K, Akiyama K, Usui T, Noda T (2012) Highly reflective foveal region in optical coherence tomography in eyes with vitreomacular traction or epiretinal membrane. Ophthalmology 119(3):581–587. https://doi.org/10.1016/j.ophtha.2011.08.026
Scheerlinck LM, van der Valk R, van Leeuwen R (2015) Predictive factors for postoperative visual acuity in idiopathic epiretinal membrane: a systematic review. Acta Ophthalmol 93(3):203–212. https://doi.org/10.1111/aos.12537
Govetto A, Lalane RA 3rd, Sarraf D, Figueroa MS, Hubschman JP (2017) Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol 175:99–113. https://doi.org/10.1016/j.ajo.2016.12.006
Gonzalez-Saldivar G, Berger A, Wong D, Juncal V, Chow DR (2020) Ectopic inner foveal layer classification scheme predicts visual outcomes after epiretinal membrane surgery. Retina 40(4):710–717. https://doi.org/10.1097/IAE.0000000000002486
Govetto A, Virgili G, Rodriguez FJ, Figueroa MS, Sarraf D, Hubschman JP (2019) Functional and anatomical significance of the ectopic inner foveal layers in eyes with idiopathic epiretinal membranes: surgical results at 12 months. Retina 39(2):347–357. https://doi.org/10.1097/IAE.0000000000001940
Govetto A, Bhavsar KV, Virgili G, Gerber MJ, Freund KB, Curcio CA, Burgoyne CF, Hubschman JP, Sarraf D (2017) Tractional abnormalities of the central foveal bouquet in epiretinal membranes: clinical spectrum and pathophysiological perspectives. Am J Ophthalmol 184:167–180. https://doi.org/10.1016/j.ajo.2017.10.011
Team RDC (2010) R: a language and enviroment for statistical computing. R Foundation for Statistical Computing, Vienna
Tibshirani R (1996) Regression shrinkage and selection via the lasso. J R Stat Soc Ser B Methodol 58(1):267–288
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. 45(3):67. https://doi.org/10.18637/jss.v045.i03
Cicinelli MV, Marchese A, Bandello F, Coppola M (2019) Inner retinal layer and outer retinal layer findings after macular hole surgery assessed by means of optical coherence tomography. J Ophthalmol 2019:3821479. https://doi.org/10.1155/2019/3821479
Coppola M, Marchese A, Cicinelli MV, Rabiolo A, Giuffre C, Gomarasca S, Querques G, Bandello F (2020) Macular optical coherence tomography findings after vitreoretinal surgery for rhegmatogenous retinal detachment. Eur J Ophthalmol 30(4):805–816. https://doi.org/10.1177/1120672120911334
Cicinelli MV, Carnevali A, Rabiolo A, Querques L, Zucchiatti I, Scorcia V, Bandello F, Querques G (2017) Clinical spectrum of macular-foveal capillaries evaluated with optical coherence tomography angiography. Retina 37(3):436–443. https://doi.org/10.1097/IAE.0000000000001199
Doguizi S, Sekeroglu MA, Ozkoyuncu D, Omay AE, Yilmazbas P (2018) Clinical significance of ectopic inner foveal layers in patients with idiopathic epiretinal membranes. Eye (Lond) 32:1652–1660. https://doi.org/10.1038/s41433-018-0153-9
Ooto S, Hangai M, Yoshimura N (2015) Effects of sex and age on the normal retinal and choroidal structures on optical coherence tomography. Curr Eye Res 40(2):213–225. https://doi.org/10.3109/02713683.2014.952828
Ooto S, Hangai M, Sakamoto A, Tomidokoro A, Araie M, Otani T, Kishi S, Matsushita K, Maeda N, Shirakashi M, Abe H, Takeda H, Sugiyama K, Saito H, Iwase A, Yoshimura N (2010) Three-dimensional profile of macular retinal thickness in normal Japanese eyes. Invest Ophthalmol Vis Sci 51(1):465–473. https://doi.org/10.1167/iovs.09-4047
Song WK, Lee SC, Lee ES, Kim CY, Kim SS (2010) Macular thickness variations with sex, age, and axial length in healthy subjects: a spectral domain-optical coherence tomography study. Invest Ophthalmol Vis Sci 51(8):3913–3918. https://doi.org/10.1167/iovs.09-4189
Ooto S, Hangai M, Tomidokoro A, Saito H, Araie M, Otani T, Kishi S, Matsushita K, Maeda N, Shirakashi M, Abe H, Ohkubo S, Sugiyama K, Iwase A, Yoshimura N (2011) Effects of age, sex, and axial length on the three-dimensional profile of normal macular layer structures. Invest Ophthalmol Vis Sci 52(12):8769–8779. https://doi.org/10.1167/iovs.11-8388
Kawasaki R, Wang JJ, Mitchell P, Aung T, Saw SM, Wong TY, Singapore Malay Eye Study G (2008) Racial difference in the prevalence of epiretinal membrane between Caucasians and Asians. Br J Ophthalmol 92(10):1320–1324. https://doi.org/10.1136/bjo.2008.144626
Clayton JA, Davis AF (2015) Sex/gender disparities and women's eye health. Curr Eye Res 40(2):102–109. https://doi.org/10.3109/02713683.2014.986333
Kofod M, la Cour M (2012) Quantification of retinal tangential movement in epiretinal membranes. Ophthalmology 119(9):1886–1891. https://doi.org/10.1016/j.ophtha.2012.03.022
Takagi S, Kudo S, Yokota H, Akiba M, Mandai M, Hirami Y, Takahashi M, Kurimoto Y, Ishida M (2019) Assessment of the deformation of the outer nuclear layer in the Epiretinal membrane using spectral-domain optical coherence tomography. BMC Ophthalmol 19(1):113. https://doi.org/10.1186/s12886-019-1124-z
Port AD, Nolan JG, Siegel NH, Chen X, Ness SD, Subramanian ML (2021) Combined phaco-vitrectomy provides lower costs and greater area under the curve vision gains than sequential vitrectomy and phacoemulsification. Graefes Arch Clin Exp Ophthalmol 259(1):45–52. https://doi.org/10.1007/s00417-020-04877-4
Hamoudi H, Correll Christensen U, La Cour M (2018) Epiretinal membrane surgery: an analysis of 2-step sequential- or combined phacovitrectomy surgery on refraction and macular anatomy in a prospective trial. Acta Ophthalmol 96(3):243–250. https://doi.org/10.1111/aos.13572
Shi L, Chang JS, Suh LH, Chang S (2019) Differences in refractive outcomes between phacoemulsification for cataract alone and combined phacoemulsification and vitrectomy for epiretinal membrane. Retina 39(7):1410–1415. https://doi.org/10.1097/IAE.0000000000002153
Guber J, Pereni I, Scholl HPN, Guber I, Haynes RJ (2019) Outcomes after epiretinal membrane surgery with or without internal limiting membrane peeling. Ophthalmol Therapy 8(2):297–303. https://doi.org/10.1007/s40123-019-0185-7
Chabot G, Bourgault S, Cinq-Mars B, Tourville E, Caissie M (2017) Effect of air and sulfur hexafluoride (SF6) tamponade on visual acuity after epiretinal membrane surgery: a pilot study. Can J Ophthalmol 52(3):269–272. https://doi.org/10.1016/j.jcjo.2016.11.004
Cismondi F, Fialho AS, Vieira SM, Reti SR, Sousa JM, Finkelstein SN (2013) Missing data in medical databases: impute, delete or classify? Artif Intell Med 58(1):63–72. https://doi.org/10.1016/j.artmed.2013.01.003
Author information
Authors and Affiliations
Contributions
Michele Coppola: conceptualization, writing—original draft
Maria Vittoria Cicinelli, Maria Brambati, Alessandro Marchese: methodology, writing—review and editing
Emma Clara Zanzottera, Antonio Peroglio Deiro, Michal Post: visualization, data curation
Francesco Bandello: project administration, supervision
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received the approval of the San Gerardo ASST Monza IRB. Patients signed written consent at the time of enrollment to be included in observational clinical research studies.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Fig 1
Percentage of missing data. EIFL: ectopic inner foveal layer; ONL: outer nuclear layer; VA: visual acuity; CMT: central macular thickness (PDF 5 kb).
ESM 1
(PDF 46 kb).
ESM 2
(PDF 30 kb).
Rights and permissions
About this article
Cite this article
Coppola, M., Brambati, M., Cicinelli, M.V. et al. The visual outcomes of idiopathic epiretinal membrane removal in eyes with ectopic inner foveal layers and preserved macular segmentation. Graefes Arch Clin Exp Ophthalmol 259, 2193–2201 (2021). https://doi.org/10.1007/s00417-021-05102-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05102-6