Abstract
The current study utilized mediation analyses to examine how parental symptoms of depression and anxiety impact child emotion regulation (ER) and emotion stability (ES) through parent emotion functioning, parenting, and the coparent relationship. 564 parents of children between 3 and 17 years (Mage = 9.47; 54.4% male) were recruited via Amazon’s Mechanical Turk across three time points: baseline (Wave 1), 4 months (Wave 2), 8 months (Wave 3). Mediation results demonstrated that symptoms of parent depression at Wave 1 predicted worse coparent relationships and decreases in parents’ ability to identify their own emotions at Wave 2. Symptoms of parental anxiety at Wave 1 predicted decreases in positive parenting and an increased tendency to have negative secondary emotional responses, impulse-control difficulties, and difficulty accessing emotion-regulation strategies at Wave 2. Additionally, symptoms of parental anxiety at Wave 1 directly predicted lower child ER and ES at Wave 3. However, no significant indirect pathways were identified between parent symptoms and child ER and ES. Sensitivity analyses examined the effects of three youth developmental stages (i.e., early and middle childhood and adolescence), as well as parent gender (i.e., mother and father), and found no significant differences across groups. Thus, even at non-clinical levels, parental symptoms of anxiety and depression may negatively impact parenting, parent regulation, and the coparent relationship, while parental anxiety symptoms may contribute to lower child ER and ES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Emotion regulation (ER) and emotion stability (ES) are critical constructs in understanding and predicting mental health outcomes in children. Both domains of emotion span across areas of functioning, with deficits in each creating serious physical and mental health problems lasting into adulthood [1, 2]. Therefore, understanding how ER and ES develop is critical in identifying risk and protective factors to inform prevention and intervention efforts. Although research has identified potential pathways to ER, such as parenting behaviors [3], significant gaps still exist. Most of the literature has focused solely on ER, with limited studies examining potential developmental pathways to ES. In addition, it is less clear if previously proposed pathways (e.g., parent dysregulation) to ER and ES are the same in parents with symptoms of anxiety or depression. Given the negative consequences of parental anxiety and depression, it is important to understand how these symptoms may impact children’s ER and ES. Lastly, much of this work has been cross-sectional, limiting causal inferences over time [4]. Therefore, the current study looks to fill these gaps by examining how parental symptoms of depression and anxiety impact child ER and ES through multiple pathways (i.e., parent emotion functioning, parenting behaviors, coparent relationship) in children and adolescents.
Emotion Regulation
ER, defined as extrinsic and intrinsic processes responsible for monitoring, evaluating, and modulating emotional arousal to generate and sustain emotions to accomplish one’s goal [5], is a precursor to the development of healthy psychosocial functioning later in life [6]. Maladaptive ER (or emotion dysregulation) early in life triggers a cascade of negative outcomes, such as poor school readiness, obesity, and aggression, which can persist throughout development [7, 8]. Given the transdiagnostic properties of ER, emotion dysregulation has been suggested to underlie multiple disorders such as attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety, and depression [9,10,11]. Research also points to emotion dysregulation as the potential underlying mechanism of heterotypic comorbidity [12] which can interfere with response to treatment and confers risk for a number of adverse outcomes [13]. Further, difficulties related to ER become more pronounced as children become older, underscoring the need to identify early prevention and intervention targets [1, 2].
The pioneering model for parental socialization of child emotion and self-regulation suggested that emotion-related socialization behaviors, such as parental reaction to child emotion and parents’ own emotional expressiveness, leads to the formation of child self-regulation, including emotion regulation [14]. Building on that model, Morris et al. (2007) proposed the tripartite model which outlines multiple pathways specific to the development of child ER: (1) children’s observation of parents’ ER (e.g., modeling emotion regulation, social referencing), (2) emotion-related parenting practices (e.g., parenting behaviors, reactions to emotions), and (3) the emotional climate of the family (e.g., emotional expressivity, family relationships). A recent review by Morris et al., (2017) presented findings across studies that support this model, yet as the authors point out, much of this literature has been cross-sectional with more studies focused on parenting and less on other factors (e.g., marital conflict, parent dysregulation).
Emotion Stability
ES, defined as an individual’s rapidity in responding to emotion eliciting stimuli, including the threshold, intensity, and duration of affective arousal for both positive and negative emotions [15, 17], is another important construct for children’s functioning. This construct has also been referred to in the literature as emotion negativity, emotion lability, emotion reactivity, and emotional impulsivity. The term “ES” and current definition were chosen based on a recent review which synthesizes the literature on emotion constructs to provide clear terminology and definitions [17]. Individuals with poor ES experience low frustration tolerance, higher levels of irritability, quickness to anger, and emotional excitability. Youth with better ES have lower levels of aggression and better social skills [16, 18, 19], while poor ES has been shown to predict internalizing and externalizing disorders [20, 21]. Unlike ER, there is no widely accepted model on the development of ES, with limited studies examining developmental pathways to ES. One of the few studies to examine ES investigated how multiple pathways based on Morris’s 2007 model (i.e., positive parenting, positive and negative family expressiveness, maternal sensitive guidance during reminiscing) were related to ER and ES in maltreated children [22]. They found that positive parenting, positive expressiveness, and maternal sensitive guidance uniquely predicted higher child ER. On the other hand, sensitive guidance was associated with better ES, and negative expressiveness was associated with worse ES. While this is an important step in examining ER and ES in an at-risk population, this study only examined parenting behaviors and did not assess for other potential pathways such as parents’ emotional functioning or family dynamics.
Parent Internalizing Symptoms
Children of parents with mental health problems are at an increased risk for later psychiatric problems [23]. Yet, not all children go on to develop psychopathology, highlighting the importance of examining who is at greatest risk. Examining the differential pathways of how parental symptoms of depression (e.g., hopelessness, fatigue, rumination) and anxiety (e.g., excessive worry, hypervigilance) lead to deficits in child ER and ES may give insight into risk and protective factors for these at-risk children. Specifically, parental symptoms of depression and anxiety may influence child ER and ES through parents’ own emotional functioning.
When parents experience symptoms of depression and anxiety, their overall emotion functioning and ability to regulate their own, and therefore their child’s emotions, can become compromised [24, 25]. Specifically, depression and/or anxiety have been shown to impact individuals’ access to adaptive emotion-regulation strategies (i.e., strategies), the tendency to experience negative emotions in response to one’s own emotional reactions or tendency to have negative secondary emotional responses to one’s negative emotions (i.e., non-acceptance), correct understanding of emotions one is experiencing (i.e., clarity), the ability to attend to and acknowledge emotions (i.e., awareness), impulse-control difficulties (i.e., impulse), and difficulties engaging in goal-directed behavior when emotionally aroused (i.e., goals) [26].
For example, compared to healthy adults, parents with depression or anxiety had fewer effective regulation strategies and greater difficulties in communication of emotions [25, 27]. For depression, symptoms of fatigue, problems with sleep, and rumination can lead to decreased adaptive ER strategies and increased maladaptive strategies [24, 28]. Relatedly, adults with anxiety may experience emotions as aversive and use worry and maladaptive interpersonal behaviors as defensive ER strategies [29]. Additionally, both symptoms of depression and anxiety can lead to non-acceptance of one’s distress [30].
Specific to depression, adults with depressive symptoms have been shown to have worse clarity and awareness compared to healthy controls on emotion-specific recognition in others and themselves [30, 31], which may be due to their low introspective abilities combined with attentional bias to sad faces when compared to healthy controls [32, 33]. These deficits may also be caused by anomalies in brain regions associated with the limbic and paralimbic systems, which are involved in emotional processing [34]. On the other hand, anxiety is typically marked by hyperarousal to environmental or internal stimuli and increased emotional reactivity, leading to ineffective decreased arousal or over-arousal in response to evocative stimuli [35]. Therefore, adults with symptoms of anxiety can be more liable and impulsive in their emotional reactions [36, 37] and have a harder time completing goals when emotionally aroused [38].
Although some research has examined these components of emotion functioning together, utilizing a total score, a recent measurement review illuminated the limitations with such analyses [17]. For example, while many studies call the total score of these scales a measure of “emotion dysregulation,” some scales assess other domains than emotion regulation/dysregulation such as emotion reasoning (i.e., clarity) and emotion stability (i.e., impulse). Further, as mentioned above, while some of these emotion domains demonstrated equifinality for depression and anxiety, other emotion domains relate more to symptoms of anxiety or depression. Therefore, it is important to examine these different domains of emotion functioning separately, without the use of a total score.
Parents with symptoms of depression or anxiety also may influence their children’s ER and ES through their parenting behaviors. These internalizing symptoms can make it difficult for parents to respond to their children in calm or emotionally supportive ways, leading to increases in negative parenting (e.g., increased hostility and ineffective discipline) and decreases in positive parenting (e.g., less positive reinforcement and warmth). For example, research has shown that maternal depression is associated with diminished emotional reciprocity and impaired parent-child bonding [39, 40], which can lead to decreases in positive reactions toward their child and increases in negative parenting behaviors such as disengagement and yelling [41, 42]. On the other hand, parental anxiety has been associated with more overcontrolling parenting and decreases in warmth [43,44,45]. While these associations between parenting and child outcomes may look slightly different based on the child’s developmental stage, research has shown that parental depression and anxiety can lead to decreases in positive parenting and increases in negative parenting from early childhood through adolescence [44, 46,47,48]. Lastly, symptoms of anxiety and depression may also influence family dynamics, such as within the coparenting relationship (i.e., the way parental figures cooperate in parenting) [49]. For example, individuals with depression can become more withdrawn, unpredictable, and have a diminished ability to use positive problem solving strategies [50], leading to decreased coparenting perceptions and increased marital discord [51, 52]. Additionally, symptoms of anxiety have been shown to increase undermining of the other parent and coparent conflict, leading to worse coparenting relationships [53, 54]. As children observe and model their parents’ own emotional functioning, parents’ interactions, and their reactions to children’s behaviors and emotions, these parent behaviors have the potential to influence the development of children’s emotional functioning, such as ER and ES.
The Current Study
Seminal theories by Eisenberg et al. (1998) and Morris et al. (2007) propose multiple pathways to the development of child emotion socialization and regulation, respectively. Yet, there is a lack of comprehensive, longitudinal evaluations of theoretically driven models investigating unique contributions to child ER and ES. While research supports these models in ER, it is less clear how parental depression or anxiety symptoms influence these proposed pathways or how these proposed pathways lead to the development of ES. Based on the previously proposed models of emotion [3, 14], the current study will examine how parental symptoms of depression or anxiety impact multiple pathways (i.e., parent emotion functioning, coparent relationship, parenting behaviors) to ER and ES in children and adolescents.
Based on previous research, we expect that symptoms of depression will influence ER and ES through positive parenting, negative parenting, and quality of the coparent relationship. Specific to emotion functioning, depressive symptoms will influence ER and ES through the awareness, clarity, non-acceptance, and strategies scales [25, 55, 56], on the Difficulties in Emotion Regulation Scale Short Form (DERS-18; [57]. In addition, based on previous research, we predict that anxiety symptoms will impact ER and ES through quality of the coparenting relationship, positive parenting, and negative parenting. In regard to emotion functioning, anxiety will impact ER and ES through impulse, goals, non-acceptance, and strategies scales on the DERS [27, 43]. Lastly, we expect that parental anxiety will directly impact ER and ES, while depression will only directly impact ES [25, 27].
Method
Procedure
With approval from the University of Vermont’s IRB, parents of youth 3-17-years-old were recruited via Amazon’s Mechanical Turk (MTurk) as part of a larger study on parenting. Parents were asked to fill out questions about their child at baseline, 4 months (Wave 2), and 8 months (Wave 3). The study was listed separately for three age groups to ensure roughly equal sample sizes in the following age ranges: early childhood (3 to 7 years old), middle childhood (8 to 12 years old), and adolescence (13 to 17 years old). For families with multiple children in the target age range, one child was randomly selected through a computer algorithm and measures were asked in reference to parenting specific to this child and her/his behavior. To participate, parents had to be a resident of the United States and have a task approval rating of 95% or higher on MTurk. These criteria ensured a high-quality participant pool as workers with better reputations (i.e., approval rating) with more tasks tend to pass attention checks at a high rate, respond with less socially desirable answers, show less midpoint bias in scale responses, and, overall, provide responses to questionnaires that match the reliability of traditional samples [58].
Parents consented online prior to beginning the survey and were compensated for completion of the survey at each Wave. Participants were excluded if their demographic data was not consistently entered across Waves or if they missed more than 2 out of 10 attention checks throughout each survey. MTurk is currently the most widely used internet-based crowdsourcing application in the social sciences [59] and has been suggested to be reliable and valid in child and family research [60].
Participants
Data from 564 parents of children between the ages of 3 and 17 years (M = 9.57, SD = 4.45) were included in the current study (see Table 1 for full demographics). Approximately half of youth were males (54.4%), with 38.5% being an only child. Overall, parents were on average 36.35 years old (SD = 8.13) and approximately 40% were fathers. Participants were predominately White (79.0%), with an additional 9.8% who identified as Black, 5.7% as Latino/a, 4.5% as Asian, and 1.0% as American Indian, Alaska Native, or other Pacific Islander. Parents’ education level ranged from not completing high school or the H.S. equivalent (0.4%), obtaining a H.S. degree or GED (12.8%), attending some college (30.5%), earning a college degree (40.6%), and attending at least some graduate school (15.9%). Most parents were employed full-time (61.7%) with 19.5% reporting employment at a part-time level, and 18.8% reporting unemployment. Reported family income was 21.7% for less than $30,000 per year, 28.7% between $30,000 and $50,000, 19.5% between $50,000 and $70,000, 16.8% between $70,000 and $100,000, and 13.3% at least $100,000. Parent marital status was organized into three categories with 17.1% reporting being single, 64.6% being married, and 18.3% being in a cohabiting relationship. Retention rates for parents were 68% at the 4-month time points (Wave 2) and 61% at the 8-month time point (Wave 3).
Measures
Parent Anxiety and Depression
The Brief Symptom Inventory-18 (BSI-18; 61) was used to assess parental symptoms of anxiety and depression at Wave 1. The BSI-18 is an 18- item self-report checklist measure developed as a brief screener for psychological symptoms and has demonstrated good psychometric properties across clinical and non-clinical samples [62, 63]. The items describe symptoms to be rated by respondents along a five-point scale according to how much they have been bothered by the symptom in the prior week. For the purpose of this study, the sum scores of the depression (6 items; a = 0.91) and anxiety (6 items; a = 0.91) scales were used, with higher scores indicating worse depression and anxiety.
Coparenting Relationship
The Coparenting Relationship Scale - Brief (CRS-Brief; 64) was used to assess the coparenting relationship at Wave 1 and Wave 2. The CRS-Brief is a 14-item self-report measure of the quality of coparenting in a family on a seven-point scale, which has demonstrated very strong associations to the original measure. The CRS-Brief assesses multiple subdomains within coparenting, including support, undermining, agreement, endorsement of partner’s parenting, closeness, division of labor, and child exposure to conflict. For the current study, a total overall sum score was used, with higher scores indicating a better coparenting relationship. Previous research has demonstrated the CRS-Brief (a = 0.79) is a reliable and valid measure of coparenting [64, 65].
Parent Emotion Functioning
The DERS-18 was used to assess six different domains of parent emotion functioning at Wave 1 and Wave 2. The DERS is one of the most commonly used self-report measures to assess emotion functioning, with a particular emphasis on negative emotions [66, 67], and higher scores indicating worse emotion functioning. The first scale, Nonacceptance (a = 0.89), focuses on the acceptance of emotions, which includes a tendency to have negative secondary emotional responses to initial negative emotions or to not accept one’s reactions to distress. The second scale, Awareness (a = 0.81), assesses lack of emotional awareness and understanding of emotions, or the ability to attend to and acknowledge emotions. The third scale, Strategies (a = 0.88), assesses an individual’s access to emotion-regulation strategies perceived as effective. The fourth scale, Goals, assesses difficulties engaging in goal-directed behavior when emotionally aroused. The fifth scale, Impulse (a = 0.89), assesses an individual’s impulse-control difficulties. Lastly, the sixth scale, Clarity (a = 0.82), assesses lack of emotional clarity, which includes the ability to identify the emotions one is experiencing. The DERS-18 has well-established psychometric properties [57, 68]. A sum score of each subscale was used.
Parenting Behaviors
The Multidimensional Assessment of Parenting Scale (MAPS; 69) was used to assess broadband positive and negative parenting practices at Wave 1 and Wave 2. The 16-item positive parenting subscale (a = 0.90) included items representing proactive parenting, positive reinforcement, warmth, and supportiveness (e.g., “I express affection by hugging, kissing, and holding my child”). The 18-item negative parenting subscale (a = 0.88) included items representing hostility, lax control, and physical control (e.g., “I spank my child with my hand when he/she has done something wrong”). Item responses were on a five-point Likert scale with 1 being “never” and 5 being “always,” such that higher scores reflected greater positive parenting and negative parenting, based upon the respective subscale. A mean score was used. The MAPS has demonstrated strong psychometric properties [69,70,71].
Child ER and ES
To assess children’s emotion functioning at Wave 1 and Wave 3, the Emotion Regulation Checklist (ERC; 72) was used. The ERC is one of the most commonly used parent-report measures to assess ER and ES. The overall measure has 24 questions and creates two subscales: ER and emotion negativity/lability (used to assess ES). Items were on a four-point Likert scale (1 = “never” to 4 = “almost always”), with higher scores indicating greater regulation (ER subscale) and stability (ES subscale). However, when examining the individual items that represent each subscale, some items did not align with our definitions for ER and ES or assessed other constructs such as empathy (e.g., “Is empathic towards others; shows concern when others are upset or distressed”). This is in line with a recent review that noted the low face validity of these scales [73]. Therefore, using questions from the ERC, we adjusted each subscale to be more in line with our definitions of ER and ES and removed some questions that assessed other domains (see Table S1 for the composite of the updated scales). The edited subscales had improved alphas across all time points (original a’s = 0.679-0.797, new a’s = 0.728-0.826), except for the ES scale at Wave 1 (a = 0.852 on the original and a = 0.838 on the new scale). Additionally, the new scales had improved overall model fit, based on confirmatory factor analyses, at both Waves (see Table S2 for more detail). A mean score for each subscale was created using the newly formed composites.
Data Analytic Plan
Path analyses were conducted using Mplus version 8.3 to test the hypothesized longitudinal model examining the link between parental symptoms of anxiety and depression and child ER and ES through parent and family variables. Variables at each Wave were covaried. Little’s Missing Completely at Random (MCAR) test revealed the data were missing completely at random, χ2 = 23.23, p = .332, and full information maximum likelihood estimation techniques were used for inclusion of all available data. The following fit statistics were used to evaluate model fit: Chi-square (χ2 > 0.05 excellent), comparative fit index (CFI; >0.90 acceptable, > 0.95 excellent), root mean square error of approximation (RMSEA; <0.08 acceptable; <0.05 excellent), and the standard root mean square residual (SRMR; <0.08 acceptable, < 0.05 excellent). The Model Indirect command with 500 bootstrapped samples in Mplus was utilized to calculate a standardized indirect effect parameter and bias-corrected bootstrap confidence intervals. Mediation will be tested when an “a” path (depression and anxiety to mediators) and “b” path (mediators to ER/ES) involving the same mediator are significant.
Covariates
Parent gender can influence parent psychopathology [74] and parenting behaviors [75], and child gender can influence parenting behaviors [76] and may impact the manifestation of emotional expression [77]. Therefore, parent gender and child gender were covaried at every time point. Further, it may also be the case that children model emotional expression from their siblings [78]. As the current dataset did not have any assessments on siblings, we covaried all time points for number of children in the home as a proxy for the presence of other children from whom to model emotional expression/behavior. As some studies show that child age may impact the proposed pathways [79, 80], child age at Wave 1 was controlled for at every time point. Lastly, for all measures examined at Wave 2 and Wave 3, their Wave 1 timepoint will be included as a covariate (see Table S3).
Sensitivity Analyses
Although some research has shown developmental differences across the proposed pathways [79, 80], other research has shown similar associations from early childhood to adolescence [44, 46,47,48]. Therefore, child age was removed from the model and the multiple-group function in Mplus was used to determine model fit across all three developmental stages ([early childhood: 3–7, n = 192], [middle childhood: 8–12; n = 176], [adolescence: 13–17; n = 195]). Three models were run separately examining model fit for the “a”, “b”, and “c” paths. Chi square difference tests were used to determine whether these paths significantly differed by developmental stage.
Furthermore, some literature has shown males and females may differ in their presentations of mental health symptoms, emotion functioning, and parenting practices. Therefore, parent gender was removed from the model and the multiple-group function in Mplus was used to determine model fit across all parent gender (1 = female, 2 = male). Similar to analyses above, three models were run separately examining model fit for the “a”, “b”, and “c” paths and chi square difference tests were used to determine whether these paths significantly differed by parent gender. Additionally, it is important to note that that 81% of parents reported having a coparent and a measure of coparenting was included in the model. Therefore, a separate model will also be run only including parents who reported having a coparent to examine potential differences.
Results
Bivariate associations and descriptive statistics are presented in Table 2. Overall, the covariates had mixed associations with primary study variables. Parent gender was associated with positive parenting and parent emotional awareness, child gender was associated with positive parenting, child age was associated with positive parenting, and child emotion stability, and number of children in the household was associated with positive parenting, negative parenting, child emotion regulation, and child emotion stability. Additionally, all primary study variables were correlated in expected directions. Finally, 28% of parents reported clinical levels of depression and 15% reported anxiety severity in the clinical range. The final model demonstrated excellent fit: χ2 (154) = 321.57, p < .001, CFI = 0.96, RMSEA = 0.044 (90% CI = 0.037 − 0.051), SRMR = 0.042.
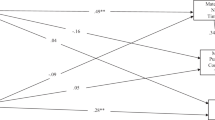
Regarding prediction of parenting and family mechanisms, symptoms of parental depression at Wave 1 significantly predicted the coparent relationship and clarity scale of the DERS at Wave 2 above and beyond stability of levels from baseline, such that greater levels of depression led to a worse coparent relationship and harder time identifying the emotions one is experiencing (see Fig. 1). Symptoms of parental anxiety at Wave 1 were significantly associated with positive parenting and the non-acceptance, impulse and strategies scales of the DERS at Wave 2. More specifically, greater levels of parental anxiety led to decreases in positive parenting, an increased tendency to have negative secondary emotional responses to initial negative emotions, increased impulse-control difficulties, and increased difficulty accessing emotion regulation strategies perceived as effective.
Model results. Bolded lines represent significant pathways. Dashed gray lines represented non-significant pathways. Paths not depicted: All variables at each time point are covaried; all variables at wave 2 are controlled for at wave 1; all variables at wave 3 are controlled for at wave 1; all variables at each timepoint are controlled for parent gender, child gender, child age, and number of children in the household. *p < .05, **p < .01, ***p < .001
Regarding prediction of child ER and ES outcomes, symptoms of parental depression at Wave 1 did not directly predict lower ER or ES at Wave 3 (see Table 3). However, higher symptoms of parental anxiety at Wave 1 significantly predicted worse ER and ES at Wave 3 after controlling for baseline levels. Positive parenting and the strategies scale of the DERS at Wave 2 predicted child ER outcomes at Wave 3, such that higher positive parenting led to better child ER, while parents’ difficulty accessing emotion regulation strategies led to decreased child ER. Negative parenting at Wave 2 significantly negatively predicted ES at Wave 3, indicating that increases in negative parenting predicted decreases in child ES.
The indirect effect of symptoms of anxiety at Wave 1 on child ER at Wave 3 through the strategies scale at Wave 2 was not significant (β = − 0.03, SE = 0.02, p = .126, [CI 95% − 0.08, 0.00]). In addition, the indirect effect of symptoms of anxiety at Wave 1 on child ER at Wave 3 through positive parenting at Wave 2 was also not significant (β = − 0.01, SE = 0.01, p = .100, [CI 95% − 0.03, 0.00]).
Sensitivity Analyses
The original model was run only including parents who reported having a coparent. Results demonstrated that significant findings did not change (see Table S4). Next, to examine if pathways are moderated by child developmental stage, the multiple-group function in Mplus was used to determine model fit across all three developmental stages. Utilizing the chi square difference tests, allowing the “a” paths (Δχ2[44] = 58.19, p = .074), “b” paths (Δχ2[44] = 39.45, p = .667, and “c” paths (Δχ2[44] = 58.19, p = .074) to vary by developmental stage led to a decrement in model fit, with all significant and non-significant paths the same across developmental stages (see Tables S5-S7). Next, to examine if pathways are moderated by parent gender, the multiple-group function in Mplus was used to determine model fit across parent gender (i.e., female and male). Utilizing the chi square difference tests, allowing the “a” paths (Δχ2[18] = 12.77, p = .805, “b” paths (Δχ2[18] = 13.44, p = .999, and “c” paths (Δχ2[26] = 20.93, p = .745) to vary by parent gender did not improve model fit, with all significant and non-significant paths the same across parent gender (see Tables S5-S7). Therefore, the results are interpreted in the context of the original model.
Discussion
Consistent with our hypotheses, parental symptoms of anxiety and depression uniquely negatively impacted the family environment, parenting practices, and both children’s and parents’ abilities to effectively manage their own emotions. Even more, specific disruptions in parenting and parental emotion regulation abilities impacted youth ER and ES. Taken together, these findings promote the need for universal screening and prevention efforts for youth that specifically assess and target effective ER and ES, for both for child and parent. Additionally, this work sets the stage for future examination of these pathways within a clinical sample.
While baseline parental depression symptoms did not directly impact parenting or child ER and ES, these symptoms did predict reduced quality of the coparent relationship and difficulties identifying experienced emotions at Wave 2. This is in line with previous work that found parental depression leads to decreases in perceived quality of the coparent relationship over time [52] and impaired emotion specific recognition [26, 27], as well as ability to recognize facial emotional expressions [81, 82]. Surprisingly, parental depressive symptoms were not associated with the DERS strategies or non-acceptance subscales as would be expected based on prior work [24, 25, 30]. Despite established associations between parental depression and parenting, as well as parental depression and child emotional functioning through parenting, significant associations among these constructs were not identified within the current study [83]. Importantly, parents within the current study sample reported lower levels of depression (28% in clinical range), suggesting that even non-clinical levels can affect the coparent relationship and parental emotion identification. Given that reduced emotional clarity can lead to other impaired facets of emotion regulation and overall wellbeing [84] and that the coparenting relationship is crucial to child psychological adjustment [85], early prevention is key to disrupt potential negative outcomes. It is possible that the lack of significant associations between parental depressive symptoms and parenting, as well as child ER and ES, in the current study may be attributed to symptoms being too low or the study assessment intervals and/or overall timeframe being too short in duration to observe an effect [86]. Additionally, it may be that the nature of depressive symptoms (e.g., withdrawal) hold more influence over the individual parent’s relationships and regulatory abilities than their child’s emotional functioning.
Baseline parental anxiety symptoms were associated with less positive parenting, increased likelihood of a poor secondary emotional response to a negative emotion, as well as difficulties with access to effective regulatory strategies and impulse control at Wave 2. These findings were expected as prior work has shown that adults with anxiety exhibit greater difficulty with accepting and managing their emotions compared to non-anxious adults [35, 87]. Further, individuals experiencing symptoms of anxiety are more prone to accessing fewer effective ER strategies [24, 25], exhibiting impulsive [28, 29], negative [30] emotional reactions, and engaging in fewer positive parenting practices [87, 88]. Contrary to our hypotheses and prior work, anxiety did not predict reduced goal-directed outcomes [27] or having poor coparent relations [53, 54]. These associations may not have been elucidated due to low levels of internalizing symptoms in this sample.
Additionally, baseline parental anxiety symptoms were directly associated with disruptions in child ER and ES at Wave 3. Prior work has shown that parents of school-aged youth with anxiety are more likely to exhibit over-control and are less likely to grant autonomy to their child [89]. The presence of these factors may have impeded upon children’s development of ER and ES in the current study, as youth may not have been exposed to a full range of positive and negative experiences crucial for the development of these skills. Children may also fail to develop effective ER and ES skills through observation of their parents’ anxious behaviors (i.e., emotion contagion, social referencing and modeling; 3).
Future work should assess for these factors along with parental symptoms of anxiety in order to best pinpoint the specific parental behaviors that contribute to either child ER or ES. Similar to parental depressive symptoms, parental anxiety symptoms were endorsed at low levels in the current study (15.1% in clinical range). Nonetheless, the presence of non-clinical levels of parental anxiety symptoms predicted later impairment in parenting practices, several domains of parent emotion regulation, and child emotional expressivity and regulation. Given that parent anxiety was assessed in tandem with depression, it appears that there is something unique about anxiety that contributes to parenting, as well as child ER and ES over time.
With respect to parenting behavior, positive parenting at Wave 2 was associated with improved child ER at Wave 3, whereas greater negative parenting was associated with worse child ES. This suggests a divergence in child emotional functioning based on the valence of parenting practices, aligning with previous research showing that positive parental behaviors foster the development of child ER, whereas negative parental behaviors increase child distress and emotional intensity due to unsuccessful attempts at suppression [90].
At Wave 2, parents’ inability to access effective regulatory strategies when feeling distressed was also associated with lower child ER abilities at Wave 3. Given that parents often serve as a model for their children with respect to regulating emotions [3], it appears that some parents experience difficulties using effective strategies when needed, and thus, are not modeling effective strategies for their child. Contrary to our hypotheses, only the strategies scale was associated with child ER and none of the DERS subscales were associated with child ES. While lack of parental emotional awareness and goal-setting have been associated with reduced interest in and certainty of their child’s mental state [91], certain facets of parental emotion regulation (e.g., awareness, goal-setting) may not be as salient to the development of child ER and ES in non-clinical samples. Additionally, the current study did not examine the influence of child factors on child ES. Oddo and colleagues (2020) found that the association between maternal emotion dysregulation and child emotional lability was moderated by ADHD symptom severity 92. This suggests that both child and parental factors should be assessed to monitor the development of child ES.
Importantly, the current study found no significant differences in results across developmental stages. Some prior work has shown age effects with respect to youth emotion functioning [79, 80]; however, these studies did not examine parental factors. Additionally, other studies have suggested bidirectional parent-child effects across development [93], which were not assessed in this study. Further, despite previous findings that women may be more prone to experiencing internalizing symptoms and that mothers and fathers may present differential parenting styles, no significant differences by parent gender were identified in this study. In fact, parental internalizing symptoms and positive and negative parenting practices were similar across parent genders, which may be due to the non-clinical nature of the sample.
Limitations and Future Directions
These findings should be considered within the context of the study’s limitations. First, the recruited sample predominantly ethnically identified as non-Latino and racially identified as White, limiting the generalizability of our findings. Prior work has shown that rates of psychiatric disorders, as well as the reported chronicity and severity of mental health difficulties, may vary based on ethnic and racial identity [94, 95]. Further, the majority of the sample was highly educated and there were a limited number of parents coming from single parent households. Prior work has shown that higher parental education level is typically associated with better youth mental health outcomes [96], whereas single parent status may confer risk for youth emotion regulation [97]. As this was secondary data analysis, we were limited in the diversity of our sample. Thus, future research is needed to examine the effects of parental factors on child ER and ES across more diverse groups.
Second, the original study was not aimed at recruiting clinically anxious or depressed parents and the symptom rates within the current sample were low; however, parents in the current sample may be more reflective of the general population. It should be noted that despite the non-clinical nature of the sample, significant associations between parental depressive symptoms and parental dysregulation (e.g., reduced emotion identification), as well as parental anxiety symptoms and later emotion dysregulation of both parent (e.g., poorer emotional responding, reduced access to effective regulation strategies) and child (e.g., lower ER and ES), were identified. Thus, the presence of these symptoms, even at low levels, contributed to worsened ER and ES outcomes. Future research should examine these relations within a clinical sample.
While the longitudinal nature of the current study was advantageous for examining parent-child pathways to emotion regulation development over time, which has been noted as a limitation in previous work [4], the non-experimental design of this study prevented the ability to draw definitive conclusions. Even more, there is evidence that youth emotion functioning influences parental factors and that this association is bidirectional across development [98]; thus, future longitudinal work should consider these pathways. Additionally, there was the possibility of shared method bias due to data being collected through MTurk from only one parent respondent. Although the current study did not recruit a clinical sample, research has demonstrated that parents with psychiatric symptoms may not be the best reporters of their child’s symptoms [99]. Therefore, future research should utilize multiple informants, including coparent and teacher report, as well as observational coding. Observational coding may also provide a context in which to better measure child modeling of parental ER behaviors, compared to parent-report measures from which the number of behaviors observed and/or modeled by the child cannot be determined. A broad measure of depression and anxiety symptoms was also used. Future work should examine whether different symptoms of depression (e.g., withdraw, anhedonia) or anxiety (e.g., generalized anxiety disorder versus obsessive compulsive disorder) differentially impact these pathways.
Lastly, in line with previous work demonstrating the high comorbidity of anxiety and depression symptoms [100], scores of parent depression and anxiety were highly associated in the current sample. While the current study may have obtained different results if models for parent anxiety and depression were run separately, that may not reflect real-world functioning. The unique results for depression and anxiety found in the current study are also more robust, as they demonstrate the unique variance predicting the Wave 1 and Wave 2 constructs, above and beyond the other parenting symptom.
Summary
The current study identified significant associations between parental symptoms of anxiety and depression, disruptions in the family environment, parenting, and parental emotion regulation, and child difficulties with regulating emotions, particularly negatively valenced emotions, within a non-clinical sample. Overall, the current study provided useful knowledge regarding the development of child ER and ES difficulties as influenced by parental behaviors (i.e., negative parenting), emotion regulation difficulties (i.e., lack of access to effective strategies), and symptoms of anxiety. Although parental factors may present differently across youth developmental stages, these parent-child associations remained salient among youth from preschool-age to adolescence. Expanding upon limited extant work on child ES, the current study identified several significant predictors of child ES; however, future research is needed to create a valid model of ES in children and adolescents. As parental anxiety and negative parenting were significant predictors of child ES, it will be important for future research to probe these associations and test different mediated pathways.
Emerging work has shown the effectiveness of a universal prevention program for parents, which incorporates parental emotion coaching components, on young children’s behavioral outcomes [101]. Findings of the current study raise the importance of identifying and mitigating potential risk factors for youth ES even in non-clinical samples through universal screening and prevention measures. Given that disruptions in ER and ES can result in a negative long-term trajectory for youth, understanding the processes that lead to their development and identifying both risk and resilience factors is imperative for the prevention of later psychopathology. Specifically, parental anxiety, as well as emotional functioning affected in this study (i.e., access to strategies, emotion identification, impulse control, poor secondary reactions to negative emotional stimuli) may be beneficial to target in emotion-focused prevention programs. While parental depressive symptoms were not associated with child ER or ES in this study, they were associated with reduced quality of the co-parenting relationship and parents’ own emotion functioning (i.e., emotion identification). A recent review shows support for emotion-focused parenting interventions, particularly those that assist parents with building their own emotion regulation skills prior to teaching their children about emotions [102]. Even more, these interventions may mitigate parental internalizing symptoms and improve parents’ ability to effectively respond to their child’s negative emotions [103]. As the current study assessed a non-clinical sample, future work should examine these longitudinal parent-child pathways within clinical, high-risk and more diverse samples to better inform risk and resilience trajectories. In all, the current study provides valuable information regarding development of child ER and ES in a non-clinical sample, while offering a foundation from which to build a valid model of child ES and explore similar associations among high-risk youth.
References
Heffer T, Willoughby T (2018) The role of emotion dysregulation: a longitudinal investigation of the interpersonal theory of suicide. Psychiatry Res 260:379–383
Masters MR, Zimmer-Gembeck MJ, Farrell LJ (2019) Transactional associations between adolescents’ emotion dysregulation and symptoms of social anxiety and depression: a longitudinal study. J Early Adolescence 39(8):1085–1109
Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR (2007) The role of the family context in the development of emotion regulation. Soc Dev 16(2):361–388
Morris AS, Criss MM, Silk JS, Houltberg BJ (2017) The impact of parenting on emotion regulation during childhood and adolescence. Child Dev Perspect 11(4):233–238
Thompson RA (1994) Emotion regulation: A theme in search of definition. Monographs of the society for research in child development. :25–52
Troy AS, Mauss IB (2011) Resilience in the face of stress: emotion regulation as a protective factor. Resil mental health: Challenges Lifesp 1(2):30–44
Eisenberg N, Valiente C, Eggum ND (2010) Self-regulation and school readiness. Early Educ Dev 21(5):681–698
Herts KL, McLaughlin KA, Hatzenbuehler ML (2012) Emotion dysregulation as a mechanism linking stress exposure to adolescent aggressive behavior. J Abnorm Child Psychol 40(7):1111–1122
Heleniak C, Jenness JL, Vander Stoep A, McCauley E, McLaughlin KA (2016) Childhood maltreatment exposure and disruptions in emotion regulation: a transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cogn therapy Res 40(3):394–415
Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK (2017) Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev 57:141–163
Brenning K, Soenens B, Vansteenkiste M, De Clercq B, Antrop I (2021) Emotion regulation as a transdiagnostic risk factor for (non) clinical adolescents’ internalizing and externalizing psychopathology: investigating the intervening role of psychological need experiences.Child Psychiatry & Human Development. :1–13
Aldao A, Gee DG, De Los Reyes A, Seager I (2016) Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: current and future directions. Dev Psychopathol 28(4pt1):927–946
Walczak M, Ollendick T, Ryan S, Esbjørn BH (2018) Does comorbidity predict poorer treatment outcome in pediatric anxiety disorders? An updated 10-year review. Clin Psychol Rev 60:45–61
Eisenberg N, Cumberland A, Spinrad TL (1998) Parental socialization of emotion. Psychol Inq 9(4):241–273
Derryberry D, Rothbart MK (1988) Arousal, affect, and attention as components of temperament. J Personal Soc Psychol 55(6):958
Hare M, Parent J, Trucco E (2022) The Emotional Competence in Children (ECIC) Scale: A parent-report measure. PsyArXiv.
Hare M, Parent J (2022) Child Emotional Competence: A Unified Framework and Assessment Review of Emotion Reasoning, Emotion Stability, Emotion Regulation, and Empathy.
Dvorak RD, Pearson MR, Kuvaas NJ (2013) The five-factor model of impulsivity-like traits and emotional lability in aggressive behavior. Aggress Behav 39(3):222–228
Eisenberg N, Fabes RA, Murphy B, Maszk P, Smith M, Karbon M (1995) The role of emotionality and regulation in children’s social functioning: a longitudinal study. Child Dev 66(5):1360–1384
Reyes NM, Factor R, Scarpa A (2020) Emotion regulation, emotionality, and expression of emotions: a link between social skills, behavior, and emotion problems in children with ASD and their peers. Res Dev Disabil 106:103770
Rosen PJ, Walerius DM, Fogleman ND, Factor PI (2015) The association of emotional lability and emotional and behavioral difficulties among children with and without ADHD. Atten Defic Hyperact Disord 7(4):281–294
Speidel R, Wang L, Cummings EM, Valentino K (2020) Longitudinal pathways of family influence on child self-regulation: the roles of parenting, family expressiveness, and maternal sensitive guidance in the context of child maltreatment. Dev Psychol 56(3):608
Plass-Christl A, Otto C, Klasen F, Wiegand-Grefe S, Barkmann C, Hölling H et al (2018) Trajectories of mental health problems in children of parents with mental health problems: results of the BELLA study. Eur Child Adolesc Psychiatry 27(7):867–876
Martin RC, Dahlen ER (2005) Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Pers Indiv Differ 39(7):1249–1260
Maliken AC, Katz LF (2013) Exploring the impact of parental psychopathology and emotion regulation on evidence-based parenting interventions: a transdiagnostic approach to improving treatment effectiveness. Clin Child Fam Psychol Rev 16(2):173–186
Gratz KL, Roemer L (2004) Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 26(1):41–54
Hughes EK, Gullone E (2008) Internalizing symptoms and disorders in families of adolescents: a review of family systems literature. Clin Psychol Rev 28(1):92–117
Aldao A, Nolen-Hoeksema S (2010) Specificity of cognitive emotion regulation strategies: a transdiagnostic examination. Behav Res Ther 48(10):974–983
Mennin DS, Heimberg RG, Turk CL, Fresco DM (2002) Applying an emotion regulation framework to integrative approaches to generalized anxiety disorder.
Bourke C, Douglas K, Porter R (2010) Processing of facial emotion expression in major depression: a review. Australian & New Zealand Journal of Psychiatry 44(8):681–696
Rubinow DR, Post RM (1992) Impaired recognition of affect in facial expression in depressed patients. Biol Psychiatry 31(9):947–953
Gotlib IH, Krasnoperova E, Yue DN, Joormann J (2004) Attentional biases for negative interpersonal stimuli in clinical depression. J Abnorm Psychol 113(1):127
Krause FC, Linardatos E, Fresco DM, Moore MT (2021) Facial emotion recognition in major depressive disorder: a meta-analytic review. J Affect Disord 293:320–328
Phillips ML, Drevets WC, Rauch SL, Lane R (2003) Neurobiology of emotion perception I: the neural basis of normal emotion perception. Biol Psychiatry 54(5):504–514
Mennin DS, Heimberg RG, Turk CL, Fresco DM (2005) Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behav Res Ther 43(10):1281–1310
Moustafa AA, Tindle R, Frydecka D, Misiak B (2017) Impulsivity and its relationship with anxiety, depression and stress. Compr Psychiatr 74:173–179
Kret ME, Ploeger A (2015) Emotion processing deficits: a liability spectrum providing insight into comorbidity of mental disorders. Neurosci Biobehavioral Reviews 52:153–171
Sörman K, Garke M, Isacsson NH, Jangard S, Bjureberg J, Hellner C et al (2021) Measures of emotion regulation: convergence and psychometric properties of the difficulties in emotion regulation scale and emotion regulation questionnaire.Journal of Clinical Psychology.
Hare MM, Kroll-Desrosiers A, Deligiannidis KM (2021) Peripartum depression: does risk versus diagnostic status impact mother–infant bonding and perceived social support? Depress Anxiety 38(4):390–399
Johnson K (2013) Maternal-infant bonding: a review of literature.International Journal of Childbirth Education. ; 28(3)
Conners-Burrow NA, McKelvey L, Perry D, Whiteside-Mansell L, Kraleti S, Mesman G et al (2016) Low-level symptoms of depression in mothers of young children are associated with behavior problems in middle childhood. Matern Child Health J 20(3):516–524
Trussell TM, Ward WL, Conners Edge NA (2018) The impact of maternal depression on children: a call for maternal depression screening. Clin Pediatr 57(10):1137–1147
Ginsburg GS, Schlossberg MC (2002) Family-based treatment of childhood anxiety disorders. Int Rev Psychiatry 14(2):143–154
Johnco CJ, Magson NR, Fardouly J, Oar EL, Forbes MK, Richardson C et al (2021) The role of parenting behaviors in the bidirectional and intergenerational transmission of depression and anxiety between parents and early adolescent youth.Depression and anxiety.
Jones JD, Lebowitz ER, Marin CE, Stark KD (2015) Family accommodation mediates the association between anxiety symptoms in mothers and children. J Child Adolesc Mental Health 27(1):41–51
Feng X, Shaw DS, Kovacs M, Lane T, O’Rourke FE, Alarcon JH (2008) Emotion regulation in preschoolers: the roles of behavioral inhibition, maternal affective behavior, and maternal depression. J Child Psychol Psychiatry 49(2):132–141
Foster CJE, Garber J, Durlak JA (2008) Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. J Abnorm Child Psychol 36(4):527–537
Möller EL, Majdandžić M, Bögels SM (2015) Parental anxiety, parenting behavior, and infant anxiety: Differential associations for fathers and mothers. J Child Fam stud 24(9):2626–2637
Feinberg ME (2003) The internal structure and ecological context of coparenting: a framework for research and intervention. Parenting: Sci Pract 3(2):95–131
Du Rocher Schudlich TD, Cummings EM (2003) Parental dysphoria and children’s internalizing symptoms: marital conflict styles as mediators of risk. Child Dev 74(6):1663–1681
Du Rocher Schudlich TD, Papp LM, Cummings EM (2011) Relations between spouses’ depressive symptoms and marital conflict: a longitudinal investigation of the role of conflict resolution styles. J Fam Psychol 25(4):531
Williams DT (2018) Parental depression and cooperative coparenting: a longitudinal and dyadic approach. Fam Relat 67(2):253–269
Majdandžić M, de Vente W, Feinberg ME, Aktar E, Bögels SM (2012) Bidirectional associations between coparenting relations and family member anxiety: a review and conceptual model. Clin Child Fam Psychol Rev 15(1):28–42
Metz M, Majdandžić M, Bögels S (2018) Concurrent and predictive associations between infants’ and toddlers’ fearful temperament, coparenting, and parental anxiety disorders. J Clin Child Adolesc Psychol 47(4):569–580
Hoffman C, Crnic KA, Baker JK (2006) Maternal depression and parenting: implications for children’s emergent emotion regulation and behavioral functioning. Parenting: Sci Pract 6(4):271–295
Silk JS, Shaw DS, Forbes EE, Lane TL, Kovacs M (2006) Maternal depression and child internalizing: the moderating role of child emotion regulation. J Clin Child Adolesc Psychol 35(1):116–126
Victor SE, Klonsky ED (2016) Validation of a brief version of the difficulties in emotion regulation scale (DERS-18) in five samples. J Psychopathol Behav Assess 38(4):582–589
Hauser DJ, Schwarz N (2016) Attentive turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behav Res Methods 48(1):400–407
Chandler J, Paolacci G, Peer E, Mueller P, Ratliff KA (2015) Using nonnaive participants can reduce effect sizes. Psychol Sci 26(7):1131–1139
Parent J, Forehand R, Pomerantz H, Peisch V, Seehuus M (2017) Father participation in child psychopathology research. J Abnorm Child Psychol 45(7):1259–1270
Derogatis LR (2001) Brief symptom inventory-18. Cultural Diversity and Ethnic Minority Psychology.
Derogatis LR, Fitzpatrick M (2004) The SCL-90-R, the brief symptom inventory (BSI), and the BSI-18.
Franke GH, Jaeger S, Glaesmer H, Barkmann C, Petrowski K, Braehler E (2017) Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative german sample. BMC Med Res Methodol 17(1):1–7
Feinberg ME, Brown LD, Kan ML (2012) A multi-domain self-report measure of coparenting. Parenting 12(1):1–21
Lee Jk, Feinberg ME, Wells MB (2021) The swedish brief coparenting relationship scale: Psychometrics and Concurrent Validity among Primiparous and Multiparous fathers. Fam Relat 70(3):823–839
Neumann A, van Lier PA, Gratz KL, Koot HM (2010) Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. Assessment 17(1):138–149
Weinberg A, Klonsky ED (2009) Measurement of emotion dysregulation in adolescents. Psychol Assess 21(4):616
Hallion LS, Steinman SA, Tolin DF, Diefenbach GJ (2018) Psychometric properties of the difficulties in emotion regulation scale (DERS) and its short forms in adults with emotional disorders. Front Psychol 9:539
Parent J, Forehand R (2017) The Multidimensional Assessment of Parenting Scale (MAPS): development and psychometric properties. J Child Fam stud 26(8):2136–2151
Cordts KMP, Wilson AC, Riley AR (2020) More than mental health: parent physical health and early childhood behavior problems. J Dev Behav pediatrics: JDBP 41(4):265
Ren Y, Han ZR, Ahemaitijiang N, Zhang G (2021) Maternal mindfulness and school-age children’s emotion regulation: mediation by positive parenting practices and moderation by maternal perceived life stress. Mindfulness 12(2):306–318
Shields A, Cicchetti D (1997) Emotion regulation among school-age children: the development and validation of a new criterion Q-sort scale. Dev Psychol 33(6):906
Mazefsky CA, Conner CM, Breitenfeldt K, Leezenbaum N, Chen Q, Bylsma LM et al (2021) Evidence base update for questionnaires of emotion regulation and reactivity for children and adolescents.Journal of Clinical Child & Adolescent Psychology. :1–25
Rosenfield S (1999)
McKinney C, Renk K (2008) Differential parenting between mothers and fathers: implications for late adolescents. J Fam Issues 29(6):806–827
Mesman J, Groeneveld MG (2018) Gendered parenting in early childhood: subtle but unmistakable if you know where to look. Child Dev Perspect 12(1):22–27
Chaplin TM (2015) Gender and emotion expression: a developmental contextual perspective. Emot Rev 7(1):14–21
Cunningham SA, Kramer MR, Narayan KV (2014) Incidence of childhood obesity in the United States. N Engl J Med 370(5):403–411
Sanchis-Sanchis A, Grau MD, Moliner A-R, Morales-Murillo CP (2020) Effects of age and gender in emotion regulation of children and adolescents. Front Psychol 11:946
Theurel A, Gentaz E (2018) The regulation of emotions in adolescents: Age differences and emotion-specific patterns. PLoS ONE 13(6):e0195501
Gollan JK, McCloskey M, Hoxha D, Coccaro EF (2010) How do depressed and healthy adults interpret nuanced facial expressions? J Abnorm Psychol 119(4):804
Scibelli F, Troncone A, Likforman-Sulem L, Vinciarelli A, Esposito A (2016) How major depressive disorder affects the ability to decode multimodal dynamic emotional stimuli. Front ICT 3:16
Goodman SH, Simon HF, Shamblaw AL, Kim CY (2020) Parenting as a mediator of associations between depression in mothers and children’s functioning: a systematic review and meta-analysis. Clin Child Fam Psychol Rev 23(4):427–460
Boden MT, Thompson RJ (2017) Meta-analysis of the association between emotional clarity and attention to emotions. Emot Rev 9(1):79–85
Teubert D, Pinquart M (2010) The association between coparenting and child adjustment: a meta-analysis. Parenting: Sci Pract 10(4):286–307
Timmons AC, Preacher KJ (2015) The importance of temporal design: how do measurement intervals affect the accuracy and efficiency of parameter estimates in longitudinal research? Multivar Behav Res 50(1):41–55
McLaughlin KA, Mennin DS, Farach FJ (2007) The contributory role of worry in emotion generation and dysregulation in generalized anxiety disorder. Behav Res Ther 45(8):1735–1752
Crosby Budinger M, Drazdowski TK, Ginsburg GS (2013) Anxiety-promoting parenting behaviors: a comparison of anxious parents with and without social anxiety disorder. Child Psychiatry & Human Development 44(3):412–418
Budinger MC, Drazdowski TK, Ginsburg GS (2013) Anxiety-promoting parenting behaviors: a comparison of anxious parents with and without social anxiety disorder. Child Psychiatry & Human Development 44(3):412–418
Shipman KL, Schneider R, Fitzgerald MM, Sims C, Swisher L, Edwards A (2007) Maternal emotion socialization in maltreating and non-maltreating families: implications for children’s emotion regulation. Soc Dev 16(2):268–285
Schultheis AM, Mayes LC, Rutherford HJ (2019) Associations between emotion regulation and parental reflective functioning. J Child Fam stud 28(4):1094–1104
Oddo LE, Miller NV, Felton JW, Cassidy J, Lejuez CW, Chronis-Tuscano A (2020) Maternal emotion dysregulation predicts emotion socialization practices and adolescent emotion lability: conditional effects of youth ADHD symptoms.Research on Child and Adolescent Psychopathology. :1–14
Johnco CJ, Magson NR, Fardouly J, Oar EL, Forbes MK, Richardson C et al (2021) The role of parenting behaviors in the bidirectional and intergenerational transmission of depression and anxiety between parents and early adolescent youth. Depress Anxiety 38(12):1256–1266
Ertel KA, Rich-Edwards JW, Koenen KC (2011) Maternal depression in the United States: nationally representative rates and risks. J women’s health 20(11):1609–1617
Williams DR (2018) Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav 59(4):466–485
Yamauchi C (2010) Parental investment in children: Differential pathways of parental education and mental health. Economic Record 86(273):210–226
Shaffer A, Suveg C, Thomassin K, Bradbury LL (2012) Emotion socialization in the context of family risks: links to child emotion regulation. J Child Fam stud 21(6):917–924
Kiel EJ, Kalomiris AE (2015) Current themes in understanding children’s emotion regulation as developing from within the parent–child relationship. Curr Opin Psychol 3:11–16
Kraemer HC, Measelle JR, Ablow JC, Essex MJ, Boyce WT, Kupfer DJ (2003) A new approach to integrating data from multiple informants in psychiatric assessment and research: mixing and matching contexts and perspectives. Am J Psychiatry 160(9):1566–1577
Aina Y, Susman JL (2006) Understanding comorbidity with depression and anxiety disorders. J Am Osteopath Assoc 106(5 Suppl 2):S9–14
Zhou X, Lee RM, Ohm J (2020) Evaluating the feasibility of the incredible years attentive parenting program. as a Universal Prevention for Racially Diverse Populations
Havighurst SS, Radovini A, Hao B, Kehoe CE (2020) Emotion-focused parenting interventions for prevention and treatment of child and adolescent mental health problems: a review of recent literature. Curr Opin Psychiatry 33(6):586–601
Tonarely NA, Kennedy S, Halliday E, Sherman JA, Ehrenreich-May J (2021) Impact of Youth Transdiagnostic treatment on parents’ own emotional responding and socialization behaviors. J Child Fam stud 30(5):1141–1155
Funding
This work was supported by the NIDA under Grant number T32DA043449; and NICHD under Grant F31HD082858.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
MH, KF, and JP report no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments of comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hare, M.M., Feeney, K.E. & Parent, J. Longitudinal Pathways from Parent Internalizing Symptoms to Parent and Youth Emotion Functioning. Child Psychiatry Hum Dev 55, 1211–1224 (2024). https://doi.org/10.1007/s10578-022-01482-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-022-01482-w