Abstract
Children of parents with mental health problems (CPM) have an increased risk for behavioral and psychological problems. This study investigated the age- and gender-specific course as well as predictors of mental health problems in CPM using the longitudinal data (baseline 1- and 2-year follow-ups) of a German general population sample from the BELLA study. Children and adolescents aged 11–17 years (at baseline) who had a parent with mental health problems (n = 325) were analyzed. The mental health problems of the children were assessed by the self-reported version of the strengths and difficulties questionnaire (SDQ). We used individual growth modeling to investigate the age- and gender-specific course, and the effects of risk as well as personal, familial and social protective factors on self-reported mental health problems in CPM. Additionally, data were examined differentiating internalizing and externalizing mental health problems in CPM. Results indicated that female compared to male CPM showed increasing mental health problems with increasing age. Mental health problems in CPM were associated with lower self-efficacy, worse family climate and less social competence over time. Internalizing problems were associated with lower self-efficacy, less social competence and more severe parental mental health problems. Externalizing problems were associated with lower self-efficacy, worse family climate and lower social competence. The main limitations of the study are the short time period (2 years) covered and the report of mental health problems by only one parent. Our findings should be considered in the development of treatment and prevention programs for mental health problems in CPM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children of parents with mental health problems (CPM) represent a well-known risk group for mental health problems [1, 2]. A review by Siegenthaler and colleagues revealed that about 50% of the CPM develops psychiatric disorders during childhood or adolescence [3]. Accordingly, parental mental health problems represent a significant predictor for lifetime onset of psychiatric disorders in their children. The general risk in children to develop any psychiatric disorder is 1.8–2.9 times higher if one parent is affected and 2.2–4.6 times higher if both parents suffer from mental health problems, compared to children in the general population [4]. In a population-based cross-sectional sample of the BELLA study [5], a proportion of 18.6% of the parents reported mental health problems. The risk factors for parental mental health problems like parental daily strain, parental chronic disease or stressful life events tend to cluster together in these families resulting in a high risk for mental health problems. CPM in this study reported mental health problems nearly three times more often (OR = 2.85) compared to children of parents without mental health problems. The most important risk factors for mental health problems in these children were stressful life events and parental mental health problems.
Factors associated with the course of mental health problems in CPM are analyzed in the longitudinal studies [6, 7]. These studies focus on factors that contribute to healthy development in children and adolescents even under difficult conditions. They differentiate protective factors into characteristics of the child (personal resources like high self-efficacy and optimism), of the family (familial resources like parental support and good familial climate) and of the social environment (social resources like availability of social support outside the nuclear family and social competence) [8].
Only a small number of longitudinal studies so far have investigated protective factors that may contribute to mental health development in CPM [6, 7]. Lewandowski and colleagues [6] identified easier temperament of the children, higher self-esteem, lower maternal overprotection and higher IQ as protective factors for mental development of children, if the parents suffer from depression. Pargas and colleagues [7] investigated children of mothers with depression and identified lower levels of perceived maternal psychological control and higher child IQ as protective factors for a healthy mental development of the children. A recently published cross-sectional study provided evidence that CPM particularly benefits from a combination of personal, familial, and social resources regarding mental health problems [9].
Moreover, based on longitudinal data, Garai and colleagues [10] reported that maternal sensitivity was related to child-reported externalizing symptoms, but not to internalizing symptoms of the child. Correspondingly, Reuben and Shaw [11] emphasize in their recent review that positive outcome has to be defined for circumscribed domains like, e.g., internalizing or externalizing behavior.
So far, longitudinal studies that investigate the natural course of mental health problems in CPM in Germany are lacking. At the same time, information on risk and protective factors as well as on the course of mental health problems in CPM based on data from the general population are essential for conceptualization and implementation of tailored support and prevention programs for this specific subgroup. Moreover, internalizing and externalizing symptoms may be associated differently by diverse factors. Consequently, the present study addresses the following research questions based on data of a general population sample:
-
1.
What are the age- and gender-specific trajectories of mental health problems in CPM?
-
2.
Which factors affect the course of mental health problems in CPM over time?
-
3.
Are there differences with respect to internalizing and externalizing mental health problems in CPM?
Methods
Procedures
The longitudinal BELLA study is the mental health module of the German National Health Interview and Examination Survey for children and adolescents (KiGGS). The BELLA baseline sample is a representative subsample of the KiGGS baseline sample. For the KiGGS baseline sample, 167 sample units were randomly chosen in German cities and communities and subsequently a random sample was generated using the local registration offices [12]. For the BELLA study, a sample of 2942 families with children and adolescents aged 7–17 years was randomly drawn from the KiGGS baseline sample separately for each age group [13]; out of these families, a number of 2863 (97.3%) families consented to participate in the BELLA study constituting the BELLA baseline sample. The baseline assessment of the BELLA study was conducted from 2003 to 2006. Data for the 1-year and the 2-year follow-ups of the BELLA study were gathered from 2004 to 2007 and from 2005 to 2008, respectively. Demographic information, data on mental health problems as well as on risk and protective factors were gathered by means of computer-assisted telephone interviews and subsequent questionnaires; psychometrically sound and internationally tested measures were administered, if available. Written informed consent for study participation was obtained from the parents and the children prior to data collection. Ethical approval for the BELLA study was obtained from the ethics committee of the University Hospital Charité in Berlin and the Federal Commissioner for Data Protection in Germany. Details on the design and methods of the BELLA and KiGGS studies are described elsewhere [13, 14].
Sample
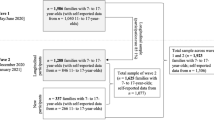
Longitudinal data of the BELLA study were analyzed focusing on children and adolescents whose biological parents had mental health problems. In the BELLA study, self-reports were only gathered from children aged at least 11 years (n = 1724). Further, we excluded participants with parental mental health data reported by step-/adoptive parents or other caregivers at any measurement point and those with parental mental health data reported by different biological parents over the included measurement points (overall n = 143). Among the remaining participants (n = 1581), we identified those with parental mental health problems at baseline (for more details, see Measures). The resulting subsample included n = 342 CPM aged 11–17 years (at baseline; 48.8% female; Mean, age = 14.09; SD = 2.024) and served to investigate the age- and gender-specific course of mental health problems in CPM. In subsequent analyses on predictors of mental health problems over time, participants could only be included, if data for at least one of the above mentioned three measurement points on mental health problems, self-efficacy, family climate and social competence, as well as information on the individual intervals between measurement points were available. This led to a slightly reduced sample of n = 325 CPM aged 11 to 17 years (at baseline; 50.5% female; Mean, age = 14.11; SD = 2.028) which could be included in the longitudinal analyses on predictors of mental health problems in CPM.
Measures
Parental mental health problems were assessed by parent-reports at each measurement point in the BELLA study using the Symptom-Check List 9-item Short-version (SCL-S-9) [15]. The decision about which parent of a child or adolescent was included in the BELLA study was primarily based on availability and willingness (parents were asked to take part during telephone interviews). The administered SCL-S-9 is an abbreviated version of the SCL-90-R [16]. Each item of the SCL-S-9 belongs to one dimension of the original SCL-90-R (i.e., somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) and is offered with a 5-point rating scale (0 = “none at all” to 4 = “very severe”). A higher total score over all 9 items of the SCL-S-9 indicates more severe psychopathologic symptoms [15]. To identify CPM within the BELLA baseline sample, we adapted the SCL-S-9 total score to the sum score of the SCL-90-R (i.e., the global severity index, GSI) and used the recommended cutoff for the GSI (T values ≥ 63 indicate mental health problems) [17]. This procedure allowed a gender-specific determination of parents with mental health problems. In our subsequent analyses on predictors of mental health problems in CPM, we used the total score of the SCL-S-9 to control for the severity of parental mental health problems.
Mental health problems of CPM were measured by self-reports in the KiGGS baseline assessment as well as in the 1- and 2-year follow-ups of the BELLA study using the Strengths and difficulties questionnaire (SDQ) [18]. The SDQ provides four problem-focused subscales with five items each, i.e., emotional symptoms (item example: “I worry a lot”), peer-related problems (“Other children or young people pick on me or bully me”), conduct problems (“I take things that are not mine from home, school or elsewhere”), and hyperactivity/inattention (“I get very angry and often lose my temper”). Items of the SDQ are offered with three response options (0 = “not true” to 2 = “certainly true”). The scores of the four problem scales are calculated by summing up the scores of the corresponding items. A total difficulties score can be calculated by summing up the scores of the four problem scales of the measure. Moreover, the SDQ allows a differentiation of mental health problems into internalizing and externalizing problems [19]. The SDQ scale on internalizing problems is calculated by summing up the scores of the subscales emotional symptoms and peer-related problems. The SDQ scale on externalizing problems is correspondingly generated by gathering the subscales that conduct problems and hyperactivity/inattention.
Self-efficacy was assessed by self-reports of CPM in the BELLA study using the General Self-Efficacy Scale (GSE) [20] at each investigated measurement point of the study. Items of the GSE (e.g., “It is easy for me to stick to my aims and accomplish my goals”) were offered with a 4-point rating scale (0 =“not at all true” to 3 = “exactly true”). Higher scores of the sum scored over all 10 items of the GSE indicate higher self-efficacy.
Family climate was measured by self-reports of CPM using the German Family Climate scale (FCS) [21] at each investigated measurement point of the study. Eight items of the FCS were administered to find out which relate to active recreational organization and cohesion (e.g., “In our family, everybody cares about each other’s worries”); items were offered with a 4-point rating scale (0 = “not true” to 3 = “exactly true”). A higher sum score over the administered items indicates better family climate.
Social competence was assessed by self-reports of CPM using five items developed in the Health Behavior in School-aged Children study [22] at each investigated measurement point of the study. Items on social competence (e.g., “I have many friends”) were offered with a 4-point rating scale (0 = “describes me not at all” to 3 = “describes me exactly”). A higher sum score over all items indicates better social competence.
SES was measured using the Winkler index [23], which includes information on education, profession as well as income of both the parents. We used the metric score of the Winkler index (ranging from 3 to 21) in our multivariate analyses; only to describe our sample, we categorized participants into groups with low (scores from 3 to 8), middle (9–14) and high SES (15–21) [24]. The SES was measured at baseline.
Migration background was determined considering the countries of birth and citizenship. Migration background was given, if (1) the CPM himself or herself immigrated to Germany and had at least one parent who was not born in Germany, or if (2) at least one of the parents immigrated to Germany or did not hold German citizenship. The migration background was measured at baseline.
Data analysis
Data were analyzed using individual growth modeling. This approach allows the simultaneous analysis of all the units of observation (i.e., data gathered at several measurement points) considering their organization within the subjects even with varying intervals between time points [25]. Correspondingly, linear mixed models were calculated using full-information maximum likelihood (FIML) estimation, which allows the inclusion of cases with missing data [26, 27]. In the first analysis, we investigated age- and gender-specific effects on mental health problems in CPM (n = 342) using data on mental health problems from all the three measurement points. We investigated the total difficulties score of the SDQ with the intercept representing the individual score at baseline and the slope reflecting the individual change per year. Further, age (at baseline), gender, the interaction between age and gender, a time variable (with individual information about the intervals between measurement points in years using three decimals, e.g., intervals from baseline to 1-year follow-up = 1.003 and from 1- to 2-year follow-up = 2.021) and a squared time variable (time × time) served as fixed effects; only time was additionally used as random effect. To investigate, if a cohort effect was given, we added the interaction between age and time to this model. Additionally, a graph was created on the age-specific course of mental health problems in male and female CPM based on estimated marginal means from the corresponding model. Moreover, we differentiated between internalizing and externalizing problems in CPM; we calculated two additional models analyzing age- and gender-specific effects on internalizing and externalizing problems using the corresponding SDQ subscales.
Predictors of mental health problems of CPM (n = 325) over time were analyzed using individual growth modeling and FIML-estimation as well. However, a number of 17 cases were still excluded from these analyses, since missing data patterns did not allow a reliable model estimation (these cases showed missing values in a level-1 predictor for each measurement point or in time variables for both intervals between measurement points). Prior to the calculations, all metric predictors except for age were centered. We investigated the total difficulties score of the SDQ with the intercept representing the individual score at baseline and the slope reflecting the individual change per year. Following a stepwise approach, we started with calculating the null model (which included the outcome, but no further predictors) [26]. In subsequent analyzing steps, we added (1) time-varying level-1 predictors with data for the three investigated measurement points (i.e., time variables, self-efficacy, family climate, social competence and parental mental health problems), (2) level 2-predictors which were only measured at baseline (i.e., age, gender, SES, migration background, as well as information on the parental rater), and (3) interaction terms (i.e., time × age, time × gender, age × gender, and age × gender × time) to our model. The included level 2-predictor indicated for each participant for which the parental rater gave information on parental mental health problems consistently throughout the study (0 = biological father; 1 = biological mother). Predictors were included as fixed effects, only time served additionally as random effect. To evaluate changes in model fit, we used the Bayesian information criterion (BIC) (smaller values indicate better model fit) and the log-likelihood difference test. To roughly evaluate the strength of significant effects, we calculated McFadden’s R 2 [28] using the log-likelihood estimates of the full model and of the full model without the predictor in question. Finally, we again differentiated between internalizing and externalizing mental health problems in CPM. We repeated the above described procedure using SDQ scales internalizing and externalizing problems as outcomes. We used IBM SPSS 22 for the presented analyses, and we determined the statistical power of our final model on mental health problems in CPM by the means of GPower.
Results
Age- and gender-specific effects on mental health problems in CPM were investigated over time (n = 342). Parent-reports indicated parental mental health problems for 88.6% of these investigated cases by biological mothers (n = 303) and for 11.4% by their biological fathers (n = 39). Based on the SCL-S-9, parents reported symptoms of depression in 48.9%, interpersonal sensitivity in 31.7%, anxiety in 24.7%, somatization in 14.9%, obsessive–compulsive in 16.1%, hostility in 22.9%, phobic anxiety in 8.2%, paranoid ideation in 12.3%, and psychoticism in 5.9% (multiple responses were possible). The results of our model indicated no direct effects of age or gender, but a significant interaction effect indicated increasing mental health problems with increasing age for female CPM (p = 0.053; y = 0.36; confidence interval (CI; 95%) − 0.01; 0.72). For internalizing difficulties, a corresponding interaction effect pointed in the same direction (p = 0.009; y = 0.30; CI (95%) = 0.07; 0.52). For externalizing problems, we found no age- or gender-specific effects. Please note that no evidence for a cohort effect was found in any investigated model. Figures 1, 2 and 3 include graphs on the age- and gender-specific courses of mental health problems as well as internalizing and externalizing problems in CPM. Descriptive means for self-reported SDQ total scores were 11.12 (SD = 4.552) at baseline [for 11–13 year-olds: M = 10.84 (SD = 4.616); for 14–17 year-olds: M = 11.30 (SD = 4.510)]. The SDQ total scores for the investigated sample were 9.18 (SD = 4.7078) at 1-year and 8.88 (SD = 4.496) at 2-year follow-ups. Descriptive mean scores for internalizing problems were 5.03 (SD = 2.958) at baseline, 4.30 (SD = 2.837) at 1-year, and 4.16 (SD = 2.946) at 2-year follow-ups. For externalizing mental health problems, a mean score of 6.09 (SD = 2.830) at baseline, 4.88 (SD = 2.852) at 1-year and 4.72 (SD = 2.667) at 2-year follow-ups were found.
Averaged age- and gender-specific course of self-reported mental health problems according to the total difficulties score of the Strengths and difficulties questionnaire (SDQ; [18]) in children of parents with mental health problems (n = 358)
Averaged age- and gender-specific course of self-reported internalizing mental health problems according to the internalizing difficulties score of the Strengths and difficulties questionnaire (SDQ; [19]) in children of parents with mental health problems (n = 358)
Averaged age- and gender-specific course of self-reported externalizing mental health problems according to the externalizing difficulties score of the Strengths and difficulties questionnaire (SDQ; [19]) in children of parents with mental health problems (n = 358)
To analyze predictors of mental health problems over time, a slightly reduced sample was used (n = 325). In this analyzed sample, a proportion of 34.2% of the cases had low (n = 111), 48.3% medium (n = 157) and 17.5% high SES (n = 57). A proportion of 9.8% of the analyzed CPM had a migration background (n = 32). Parent-reports on parental mental health problems (according to the SCL-S-9) were given for 88.9% of the investigated cases by biological mothers (n = 289) and for 11.1% by their biological fathers (n = 36). Table 1 presents descriptive means and standard deviations of scale scores for each measurement point.
Following our stepwise analyzing procedure, we started with the null model (BIC = 4471.1; − 2*log-likelihood = 4451.053); the intra class-correlation for this model indicated that 55% of the total variance in the SDQ total difficulties score could be explained by differences between the subjects. The inclusion of level 1-predictors led to a highly significant improvement in model fit according to the log-likelihood difference test (BIC = 3696.5; − 2*log-likelihood = 3624.750; χ 2 (8) = 862.303, p < 0.001). Subsequently, we included level-2 predictors, but model fit did not improve any more (BIC = 3721.5; − 2*log-likelihood = 3617.210, χ 2 (5) = 7.540, p = 0.183). Finally, model fit did not improve either, as we added interaction terms (BIC = 3745.3; − 2*log-likelihood = 3614.961, χ 2 (4) = 2.249, p = 0.490). The results of our final model indicate that the average total score of the SDQ at baseline was 11.11 in our sample (see the corresponding estimate for the intercept in Table 2, which presents an average score in the outcome for the analyzed sample, when all predictors included in the model are zero). The model results indicated a decrease in the outcome according to the estimate for the linear time variable (y = − 1.58) and an increase according to the squared time variable (y = 0.69) over time. That is, the average SDQ score of 11.11 decreased on average per year by 0.89 into scores of 10.228 and 9.33 after 1 year and after 2 years, respectively). Moreover, lower self-efficacy, worse family climate, and less social competence were associated with more mental health problems in CPM. Effects of age, gender, SES or migration status on mental health problems were not detected. We controlled for effects of parental mental health problems and for the rater reporting these problems (biological fathers vs. biological mothers) on mental health problems in CPM over time, but no corresponding effects were found. The model fit improved most by including family climate (McFadden’s R 2 = 0.13) and less by adding self-efficacy, or social competence (McFadden’s R 2 = 0.01 for each of these predictors). The correlations between subscales on internalizing and externalizing mental health problems ranged again from small to moderate across the investigated measurement points in the investigated sample (r ranging from 0.23 to 0.36). For the analyzed data, the statistical power of a small regression effect (f 2 = 0.06) is at least 90%.
The results of the final models on predictors of internalizing and externalizing mental health problems are included in Table 2. Internalizing problems were associated with lower self-efficacy, less social competence and more severe parental mental health problems in CPM. Externalizing problems were associated with lower self-efficacy, worse family climate, and less social competence. We found no effects of the parental rater (biological father vs biological mother) in any model.
Discussion
The present study investigated the course of mental health problems and analyzed risk and protective factors for mental health problems in CPM over time. Our findings indicate that female compared to male CPM showed increasing mental health problems with increasing age. Our predictor models showed that mental health problems in CPM were associated with lower self-efficacy, worse family climate and less social competence over time. Internalizing problems were associated with lower self-efficacy, less social competence and more severe parental mental health problems. Externalizing problems were associated with lower self-efficacy, worse family climate and lower social competence.
A proportion of 21.6% (n = 342) of our initial population-based sample of 1581 children and adolescents had parents with mental health problems at baseline. This result is close to the corresponding proportion of 19.1% of the parents, which we reported in our above cited cross-sectional study based on weighted data of the 6-year follow-up of the BELLA study (data were weighted based on the German microcensus with regard to the children's age and gender) [5]. Other population-based studies focused on maternal depressive symptoms. Chang et al. [29] reported that 23.4% of the mothers were depressive in a US nationally representative household sample. Pargas et al. [7] reported a proportion of nearly 14% for depressive mothers based on their Australian prospective birth cohort study of 7223 children and their mothers. Different proportions for maternal depressive symptoms reported in these two studies may be due to the differing nationalities of the investigated samples and the instruments used (Chang et al. [29] administered the 20-items CES-D scale to measure maternal depressive symptoms, while Pargas et al. [7] used the Structured Clinical Interview for DSM-IV). The descriptive means for the SDQ self-reported total score in CPM in our sample ranged from 9 to 11 points across measurement points with lower scores at follow-up measurement points. We draw our subsample of CPM by identifying children and adolescents with parents who reported mental health problems at baseline and mental health problems in these parents did not necessarily sustain or re-appear at 1-year and/or 2-year follow-ups. Moreover, our findings may have partly been influenced by effects of repeated measurements over time. Overall, the descriptive means for the SDQ total score found in our study are only slightly higher than corresponding scores based on norm samples from different countries ranging from 8 to 10 points [for a British sample of 11–15 year-olds, the mean score was 10.3 (SD = 5.2) [30]; in an Australian sample of 11–17 year-olds, the mean score was 9.0 (SD = 5.6) [31] ranging from 8.0 (SD = 6.1) in 11–13 year-old girls to 10.1 (SD = 6.0) in 14–17 year-old boys]. Although the total score in our sample was not much higher than in the above cited norm samples, we detected that CPM in the BELLA study reported nearly three times more often mental health problems (OR = 2.85; CI 1.88; 4.32) compared to children of parents without mental health problems in our previous work [5] showing that CPM represent a risk group for mental health problems.
The investigation of the age-specific course showed that internalizing mental health problems in CPM increased for girls with increasing age. This result is in line with findings of epidemiological studies for the general population assessed with clinical interviews indicating more internalizing symptoms in adolescent girls compared to boys [32] These authors also reported a high symptomatology concerning externalizing problems for boys which is decreasing with ongoing age in the years 10–15. We could not confirm the latter finding due to the age group investigated in our study. As mentioned above, we showed in a previous work [5] that CPM report more mental health problems than children of parents without mental health problems (19.1 vs. 7.7%). In summary, these results suggest that the level of symptomatology in CPM is considerably higher than in children of parents without mental health problems, but the course of mental health problems does not differ distinctly in CPM compared to children of parents without mental health problems. Future longitudinal studies are necessary to confirm these results.
Our analyses on the predictors of mental health problems in CPM over time revealed evidence that self-efficacy, family climate and social competence may serve as protective factors for mental health problems in CPM. Correspondingly, Lewandowski and colleagues [6] reported that self-esteem was the most important predictor for mental health development in children of depressed mothers; the concept of self-esteem analyzed by those authors is very close to the concept of self-efficacy which we analyzed in our study. Similar results from the longitudinal study done by Pargas and colleagues [7] showed that high self-esteem predicted mental health development in children of depressed mothers; the same was true for healthy peer social functioning, a predictor that is very close to social competence in the present study. Moreover, our findings on the association between family climate and mental health problems in CPM are in line with the findings of former studies. Parenting functioning operationalized as perceived maternal psychological control by Pargas and colleagues [7] and as lower maternal overprotection by Lewandowski and colleagues [6] predicted mental health development in the children of depressed mothers. We found that mental health problems of CPM were associated with personal (self-esteem), familial (family climate) as well as social resources (social competence); these findings indicate that the mental health development in CPM depends on resources from diverse sources, corresponding to the findings of our former cross-sectional study [9].
Increasing parental mental health problems served as a risk factor for increasing internalizing but not for increasing externalizing symptoms of CPM. To interpret this result, it has to be noticed that the parents included in the present study predominantly reported severe internalizing mental health problems like depression (48.9%), interpersonal sensitivity (31.7%) and anxiety (24.7%). Previous studies described that psychiatric disorders were transmitted specifically from parents to their offspring (e.g., concerning anxiety disorders [33, 34], substance use disorders [35], behavioral disorders [36] and major depression [37]). However, other studies with bigger samples as well as meta-analyses reported little specificity in the associations of particular parent disorders with particular offspring disorders [4, 38] and suggested a more generalized pattern for intergenerational transmission of mental disorders. These results raise the question of mechanisms of risk transmission from parents to children. The following results of the Gene-by-Environment research [39], genetic as well as environmental factors have to be considered. Genetic liability factors are associated with a wide range of internalizing or externalizing pathology [40, 41]. As important environmental factor in the transmission of parental psychopathology on children, parenting behavior may have an important influence on the mental health of children as well. Particular patterns of parenting behavior may be specifically associated with a child’s mental health problems [38]. Future research should investigate more detailed mechanisms of the transmission of mental health problems from parents to children and shed light on aspects of specific vs. unspecific transmission processes.
Family climate predicted externalizing but not internalizing symptoms in the investigated children in our study. This result is in line with the study of Luthar and Sexton [42]; these authors reported that externalizing diagnoses but not internalizing diagnoses of the children were associated with negative parenting behaviors in a sample of mothers with depression or drug abuse. Goodman and colleagues [38] showed in their review that parenting style in particular was associated with externalizing problems in children. According to Reuben and Shaw [11], externalizing problems in children substantially depend on the adequacy of parental discipline. Based on these findings, we suggest that familial as well as parental protective and risk factors are more important for the development of externalizing than for internalizing problems in CPM.
In the present study, we analyzed a risk group sample of CPM and found no association between mental health problems in CPM and SES. However, we found in our previous study based on data of the BELLA study, that families with parental mental health problems are already characterized by significantly lower SES compared to families without parental mental health problems (27.9% with low, 60.0% with medium, and 12.1% with high SES compared to 13.3% with low, 66.6% with medium, and 20.1% with high SES [5]). That is, the investigated sample of CPM in our study already had relatively low SES (low SES in 34.2%, medium SES in 48.3% and high SES in 17.5% of the investigated cases).
The present study has the following main limitations. Neither the investigated children, nor the parents received a clinical diagnose confirmed by the clinical interviews. Additionally, in the BELLA study, only information on mental health problems of one parent was assessed. However, previous studies reported substantial differences in risks for child mental health problems in CPM, if one or both parents suffered from mental health problems [4]. Future studies should consider mental health problems in both parents. Finally, the investigated time span only covered 2 years in our study. In general, longitudinal studies on children and adolescents have to deal with the transition from childhood over adolescence into adulthood, and the respective changes in symptomatologies as well as in recommended age-appropriate assessment instruments. Nevertheless, future studies should strive for assessing data over a longer time period and for describing trajectories of mental health problems in CPM based on those data.
The present study also has several strengths. We analyzed data of the general German population, whereas previous German studies on CPM have predominantly investigated clinical samples [2, 43]. The present data should thus fill an important gap in the existing literature.
Research already showed that self- and parent-reports on mental health problems in children and adolescents may differ [44, 45]. We analyzed self-reported data on mental health problems in CPM to prevent a potential bias which may have occurred if parents with mental health problems report on the mental health of their offspring. Future studies may wish to investigate predictors of parent-reported mental health problems in CPM as well as the agreement between self- and parent-reported data on mental health in this risk group. CPM represent a well-known risk group for mental health problems and thus tailored support and prevention programs are needed; corresponding programs are currently developed and progressively implemented in mental care services [46, 47]. Our findings that self-efficacy and social competence may serve as protective factors for developing mental health problems in CPM, and that family climate is a protective factor for developing externalizing symptoms in CPM can facilitate the development of adapted support and prevention programs for this risk group. Moreover, support programs should consider that female CPM with growing age may represent a subgroup with a high risk for internalizing symptoms.
References
Beardslee WR, Gladstone TRG, O’Connor EE (2011) Transmission and prevention of mood disorders among children of affectively ill parents: a review. J Am Acad Child Adolesc Psychiatry 50(11):1098–1109. https://doi.org/10.1016/j.jaac.2011.07.020
Mattejat F, Remschmidt H (2008) The children of mentally Ill parents. Deutsch Arzteblatt Int 105(23):413–418. https://doi.org/10.3238/arztebl.2008.413
Siegenthaler E, Munder T, Egger M (2012) Effect of preventive interventions in mentally ill parents on the mental health of the offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 51(1):8–17. https://doi.org/10.1016/j.jaac.2011.10.018
McLaughlin KA, Gadermann AM, Hwang I, Sampson NA, Al-Hamzawi A, Andrade LH, Angermeyer MC, Benjet C, Bromet EJ, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, de Graaf R, Florescu S, Gureje O, Haro JM, Hinkov HR, Horiguchi I, Hu CY, Karam AN, Kovess-Masfety V, Lee S, Murphy SD, Nizamie SH, Posada-Villa J, Williams DR, Kessler RC (2012) Parent psychopathology and offspring mental disorders: results from the WHO World Mental Health Surveys. Br J Psychiatry 200(4):290–299. https://doi.org/10.1192/bjp.bp.111.101253
Plass-Christl A, Haller AC, Otto C, Barkmann C, Wiegand-Grefe S, Holling H, Schulte-Markwort M, Ravens-Sieberer U, Klasen F (2017) Parents with mental health problems and their children in a German population based sample: results of the BELLA study. PLoS One 12(7):e0180410. https://doi.org/10.1371/journal.pone.0180410
Lewandowski RE, Verdeli H, Wickramaratne P, Warner V, Mancini A, Weissman M (2014) Predictors of positive outcomes in offspring of depressed parents and non-depressed parents across 20 years. J Child Fam Stud 23(5):800–811. https://doi.org/10.1007/s10826-013-9732-3
Pargas RCM, Brennan PA, Hammen C, Le Brocque R (2010) Resilience to maternal depression in young adulthood. Dev Psychol 46(4):805–814. https://doi.org/10.1037/a0019817
Masten AS, Reed M-GJ (2002) Resilience in development. In: Snyder CR, Lopez SJ (eds) Handbook of positive psychology. Oxford University Press, Oxford, pp 74–88
Plass A, Haller AC, Habermann K, Barkmann C, Petermann F, Schipper M, Wiegand-Grefe S, Holling H, Ravens-Sieberer U, Klasen F (2016) Factors promoting mental health in children of parents with mental health problems: results of the BELLA Cohort study. Kindheit und Entwicklung 25(1):41–49. https://doi.org/10.1026/0942-5403/a000187
Garai EP, Forehand RL, Colletti CJM, Reeslund K, Potts J, Compas B (2009) The relation of maternal sensitivity to children’s internalizing and externalizing problems within the context of maternal depressive symptoms. Behav Modif 33(5):559–582. https://doi.org/10.1177/0145445509342581
Reuben JD, Shaw DS (2015) Resilience in the offspring of depressed mothers: variation across risk, domains, and time. Clin Child Fam Psychol Rev 18(4):300–327. https://doi.org/10.1007/s10567-015-0195-5
Kamtsiuris P, Lange M, Schaffrath Rosario A (2007) Der Kinder- und Jugendgesundheitssurvey (KiGGS): stichprobendesign, response und nonresponse-analyse (The German Health Interview and Examination Survey for Children and Adolescents (KiGGS): sample design, response and nonresponse analysis). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50(5–6):547–556. https://doi.org/10.1007/s00103-007-0215-9
Ravens-Sieberer U, Otto C, Kriston L, Rothenberger A, Dopfner M, Herpertz-Dahlmann B, Barkmann C, Schon G, Holling H, Schulte-Markwort M, Klasen F, Grp BS (2015) The longitudinal BELLA study: design, methods and first results on the course of mental health problems. Eur Child Adolesc Psychiatry 24(6):651–663. https://doi.org/10.1007/s00787-014-0638-4
Kurth BM, Kamtsiuris P, Holling H, Schlaud M, Dolle R, Ellert U, Kahl H, Knopf H, Lange M, Mensink G, Neuhauser H, Rosario A, Scheidt-Nave C, Schenk L, Schlack R, Stolzenberg H, Thamm M, Thierfelder W, Wolf U (2008) The challenge of comprehensively mapping children’s health in a nation-wide health survey: design of the German KiGGS-study. BMC Public Health 8(1):196
Klaghofer R, Brahler E (2001) Construction and statistical testing of a short version of the SCL-90-R. Zeitschrift für Klinische Psychologie Psychiatrie und Psychotherapie 49(2):115–124
Derogatis LR (ed) (1977) SCL-90-R administration, scoring and procedures—manual-I for the Revised version. John Hopkins University School of Medicine, Baltimore
Franke GH (2002) SCL-90-R: Symptom-Checkliste von L.R. Derogatis—deutsche Version. Beltz Test GmbH, Göttingen
Goodman R (1997) The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 38(5):581–586
Goodman A, Lamping DL, Ploubidis GB (2010) When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): data from British parents, teachers and children. J Abnorm Child Psychol 38(8):1179–1191
Schwarzer R, Jerusalem M (1995) Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M (eds) Measures in health psychology: a user’s portfolio. Causal and control beliefs NFER-NELSON, Windsor, pp 35–37
Schneewind K, Beckmann M, Hecht-Jackl A (1985) Familienklima-Skalen. Bericht 8.1 und 8.2. Ludwig Maximilians Universität, Institut für Psychologie-Persönlichkeitspsychologie und Psychodiagnostik, München
Currie C, Samdal O, Boyce W, Smith R (2001) Health behaviour in school-aged children: A WHO Cross-National Study (HBSC), Research Protocol for the 2001/2002 Survey. University of Edinburgh: Child and Adolescent Health Research Unit (CAHRU)
Winkler J, Stolzenberg H (1999) Der Sozialschichtindex im Bundes-Gesundheitssurvey. Gesundheitswesen 61:S178–S183
Lange M, Kamtsiuris P, Lange C, Schaffrath Rosario A, Stolzenberg H, Lampert T (2007) Messung soziodemographischer Merkmale im Kinder- und Jugendgesundheitssurvey (KiGGS) und ihre Bedeutung am Beispiel der Einschätzung des allgemeinen Gesundheitszustands. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50(5–6):578–589
DeLucia C, Pitts SC (2006) Applications of individual growth curve modeling for pediatric psychology research. J Pediatr Psychol 31(10):1002–1023. https://doi.org/10.1093/jpepsy/jsj074
Heck R, Thomas S, Tabata L (2014) Multilevel and longitudinal modeling with IBM SPSS. Routledge, New York
Field A (2015) Discovering statistics using IBM SPSS statistics, 4th edn. Sage Publications Ltd., London
McFadden D (1974) Conditional logit analysis of qualitative choice behaviour. In: Zarembka P (ed) Frontiers in Ecnometrics. Academic Press, New York, pp 105–142
Chang JJ, Halpern CT, Kaufman JS (2007) Maternal depressive symptoms, father’s involvement, and the trajectories of child problem Behaviors in a US national sample. Arch Pediatr Adolesc Med 161(7):697–703. https://doi.org/10.1001/archpedi.161.7.697
Meltzer H, Gatward R, Goodman R, Ford T (2000) Mental health of children and adolescents in Great Britain. Stationery Office, London
Mellor D (2005) Normative data for the Strengths and Difficulties Questionnaire in Australia. Aust Psychol 40(3):215–222. https://doi.org/10.1080/00050060500243475
Costello EJ, Copeland W, Angold A (2011) Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry 52(10):1015–1025. https://doi.org/10.1111/j.1469-7610.2011.02446.x
Turner SM, Beidel DC, Costello A (1987) Psychopathology in the offspring of anxiety disorder patients. J Consult Clin Psychol 55:229–235
Biedermann J, Petty C, Faraone SV, Henin A, Hirshfeld-Becker D, Pollack MH et al (2006) Effects of parental anxiety disorders in children at high risk for panic disorder: a controlled study. J Affect Disord 94:191–197
Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang HP, O’Malley SS, Rounsaville BJ (1998) Familial transmission of substance use disorders. Arch Gen Psychiatry 55(11):973–979. https://doi.org/10.1001/archpsyc.55.11.973
Clark DB, Cornelius J, Wood DS, Vanyukov M (2004) Psychopathology risk transmission in children of parents with substance use disorders. Am J Psychiatry 161:685–691
Lieb R, Isensee B, Höfler M, Pfister H, Wittchen HU (2002) Parental major depression and the risk of depression and other mental disorders in offspring. A prospective-longitudinal community study. Arch Gen Psychiatry 59:365–374
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14(1):1–27. https://doi.org/10.1007/s10567-010-0080-1
Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE (2010) Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry 167(5):509–527. https://doi.org/10.1176/appi.ajp.2010.09101452
Kendler KS, Prescott CA, Myers J, Neale MC (2003) The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry 60(9):929–937. https://doi.org/10.1001/archpsyc.60.9.929
Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ (2004) Family transmission and heritability of externalizing disorders—a twin-family study. Arch Gen Psychiatry 61(9):922–928. https://doi.org/10.1001/archpsyc.61.9.922
Luthar SS, Sexton CC (2007) Maternal drug abuse versus maternal depression: vulnerability and resilience among school-age and adolescent offspring. Dev Psychopathol 19(1):205–225. https://doi.org/10.1017/s0954579407070113
Wiegand-Grefe S, Geers P, Halverscheid S, Petermann F, Plass A (2010) Kinder psychisch kranker Eltern. Zusammenhänge zwischen der Krankheitsbewältigung einer elterlichen psychischen Erkrankung und der Gesundheit der Kinder. Zeitschrift für klinische Psychologie und Psychotherapie 39(1):13–23
Becker A, Hagenberg N, Roessner V, Woerner W, Rothenberger A (2004) Evaluation of the self-reported SDQ in a clinical setting: do self-reports tell us more than ratings by adult informants? Eur Child Adolesc Psychiatry 13:17–24. https://doi.org/10.1007/s00787-004-2004-4
Klasen F, Petermann F, Meyrose AK, Barkmann C, Otto C, Haller AC, Schlack R, Schulte-Markwort M, Ravens-Sieberer U (2016) Trajectories of mental health problems in children and adolescents: results of the BELLA Cohort Study. Kindheit und Entwicklung 25(1):10–20. https://doi.org/10.1026/0942-5403/a000184
Brent D, Brunwasser SM, Hollon SD, Weersing VR, Clarke GN, Dickerson JF, Beardslee WR, Gladstone T, Porta G, Lynch F, Iyengar S, Garber J (2015) Effect of a cognitive-behavioral prevention program on depression 6 years after implementation among at-risk adolescents: a randomized clinical trial. JAMA Psychiatry 72(11):1110–1118. https://doi.org/10.1001/jamapsychiatry.2015.1559
Wiegand-Grefe S, Alberts J, Petermann F, Plass A (2016) Differential perspectives on family functioning and interfamilial relationships: the effect of a manualized intervention program on children of mentally Ill parents. Kindheit und Entwicklung 25(2):77–88. https://doi.org/10.1026/0942-5403/a000192
Acknowledgements
The authors thank all participants of the BELLA study and their parents for their time and involvement. We also would like to thank the Robert-Koch Institute for their ongoing support and co-operation. The baseline, 1- and 2-year follow-up assessments of the BELLA study were financed by the German Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Plass-Christl, A., Otto, C., Klasen, F. et al. Trajectories of mental health problems in children of parents with mental health problems: results of the BELLA study. Eur Child Adolesc Psychiatry 27, 867–876 (2018). https://doi.org/10.1007/s00787-017-1084-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-017-1084-x