Abstract
Relations among past maternal depressive disorder, current depressive symptoms, current maternal interaction behaviors, and children’s adjustment were examined in a sample of 204 women and their young adolescent offspring (mean age = 11.86, SD = 0.55). Mothers either had (n = 157) or had not (n = 57) experienced at least one depressive disorder during the child’s life. Mothers and children participated in a problem-solving task, video-taped for later coding. Mothers with current depressive symptoms and those with histories of chronic/severe depressive disorders displayed fewer positive behaviors toward their children; mothers with current depressive symptoms also showed more negative behaviors with their children. The relation between mothers’ depression history and their behavior during the interaction with their child was partially mediated by mothers’ current mood state. Moreover, high levels of maternal negativity and low levels of positivity during the problem-solving task were related to children’s externalizing problems. Maternal positivity partially mediated the relation between maternal depression and children’s externalizing symptoms. These findings highlight the importance of providing parenting interventions for depressed mothers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Offspring of depressed parents are at increased risk for internalizing (Wickramaratne and Weissman 1998) and externalizing problems (Kim-Cohen et al. 2005). Because depression has been shown to have deleterious effects on parenting behaviors (Lovejoy et al. 2000), such parenting difficulties have been postulated to be one mechanism by which maternal depression contributes to childhood psychopathology (Goodman and Gotlib 1999, 2002). The purpose of the present study was to further explore relations among maternal depression, parenting, and children’s adjustment by examining the relations among mothers’ depression history, current depressive symptoms, and behaviors while interacting with their children during a problem-solving task.
Maternal Negativity
Compared to nondepressed women, depressed mothers have been found to be more negative with their children from infancy through adolescence (e.g., Field 1984; Jacob and Johnson 1997). For example, depressed mothers made more guilt-inducing, critical, and harsh statements to their 8- to 16-year-old children during a conflict discussion (Hamilton et al. 1993) compared to healthy women. Offspring of parents who engaged in negative parenting behaviors were found to have greater levels of both internalizing and externalizing problems (Ge et al. 1996). Heller and Baker (2000) showed that pre-school children whose mothers were highly negative had the most severe externalizing problems during pre-school, first, and third grades.
Negative parenting by depressed mothers also has been characterized by either too much involvement (i.e., intrusive and controlling) or too little involvement with their children (i.e., neglectful or distant) (e.g., Garber et al. 1997; Lovejoy et al. 2000). For example, depressed mothers are less engaging, less vocal, and less skillful at getting and keeping their children’s attention (Sameroff et al. 1982), and they make more off-task, non-productive comments to their children than do nondepressed mothers (Hammen et al. 1987).
Maternal Positivity
Depressed mothers are not only more negative, but also are less positive during interactions with their children compared to nondepressed mothers (Jacob and Johnson 1997). For example, depressed mothers praised their children less frequently and provided less positive feedback of their children’s performance and competence (Hammen 1992). Positivity also can include the provision of support to children in the context of a problem-solving activity. Goldsmith and Rogoff (1995) showed that depressed mothers were less sensitive to their child’s level of understanding, appeared less comfortable in the teaching role, and did less teaching during structured tasks than did their nondepressed counterparts. In addition, depressed mothers used fewer questions, explanations, and suggestions during such tasks (Cox et al. 1987) and spent less time in jointly focused attention with their children (Goldsmith and Rogoff 1997). These behaviors contrast with teaching strategies such as praise, encouragement, use of Socratic methods, and providing enough support to prevent frustration, which are known to facilitate the development of children’s problem-solving skills (Murray et al. 2006).
The Present Study
The present study builds on the existing literature in three important ways. First, the majority of studies of parent–child interaction with depressed mothers have involved infants or pre-school children (e.g., Field 1984; Weinberg and Tronick 1998; although see Brennan et al. 2003; Gordon et al. 1989). Indeed, so few studies have investigated mother–child interactions with older children or adolescents that Lovejoy et al. (2000) were unable to draw conclusions regarding children older than age 6. Only seven of the 46 studies reviewed by Lovejoy et al. included children over age 6, and only four of the seven included children over 12 years old. The absence of interaction data for older children and adolescents is concerning because the rates of depression increase during adolescence (Angold and Costello 2001), and offspring of depressed mothers may be particularly vulnerable to their mother’s psychopathology during this age period (Goodman and Gotlib 2002). In addition, adolescence brings new challenges to parents who must alter their behaviors, for example, to encourage autonomy while preserving appropriate supervision and modify expectations in response to children’s emerging abstract thinking. As children develop, what they need from parents changes; the potential impact of depression on a parent’s ability to negotiate these developmental transitions is not well understood.
Second, this study observed maternal behaviors during a potentially positive and collaborative task. Most previous observational studies of older children have used an interaction task designed to provoke conflict between parent and child (e.g., Ge et al. 1996; Jacob and Johnson 1997). Conflict-laden tasks are more likely to elicit negative behaviors, whereas game-like tasks are more likely to elicit positive behaviors (Donenberg and Weisz 1997). It is important to study opportunities for positive parent–child interactions, as these interactions may foster children’s feelings of self-competence and self-esteem (Cole et al. 2007) and may protect against the development of conduct-related problems (Chronis et al. 2007). A central goal of this study was to investigate whether the behaviors typically associated with depressed parenting (i.e., high negative and low positive) would be evident during a task that pulled for more positive exchanges between mothers and children.
Third, the present study addressed an important limitation in the maternal depression literature. Although depression is a heterogeneous disorder that can vary in its severity, duration, and recurrence, few studies have addressed these aspects of maternal depression (Goodman and Gotlib 1999). Brennan et al. (2000) found that severity and chronicity of maternal depression were related to higher levels of behavior problems and lower vocabulary scores in children at age 5. Other studies examining the relation between the severity and course of mothers’ depression history and mother–child interactions have produced inconsistent results. Whereas Murray et al. (2006) reported that depression history was unrelated to mothers’ current behaviors, in another study (Campbell et al. 1995) mother’s history of chronic depression predicted maternal affect and interaction style. Thus, the extent to which mothers’ parenting behaviors and children’s adaptation are related to the chronicity and severity of the mother’s depression remains unclear.
Moreover, the relation between severity and chronicity of mothers’ depression history and their current level of depressive symptoms is not well-understood. It is possible that the impact of chronic past depressive episodes on parenting is only evident during times of current symptoms (e.g., an “activating hypothesis”). Alternatively, a mother with a history of chronic depression may experience more impairment in her parenting, relative to a woman with a comparable level of symptoms and no prior history of depressive disorder. This would be consistent with the notion that the experience of depression may “scar” the functioning of an individual (Pettit and Joiner 2006). It also is possible that a third variable, such as interpersonal deficits may be causally related to both chronic depression and impaired parenting.
A further complication is that previous research has been inconsistent in how “depression” was defined (Lovejoy et al. 2000). Whereas some studies have treated depression as a continuous variable in terms of the number of current symptoms reported on questionnaires (e.g., Field et al. 1984), others have used a current diagnosis of a depressive disorder (e.g., Weissman et al. 2006), and still others have included mothers with only a past history of a depressive disorder (e.g., Hammen et al. 1987). Thus, it is unclear whether the parenting behaviors associated with maternal depression are a function of current depressive symptoms or long-standing, entrenched behaviors that are present in women with a history of depression even when they are not currently symptomatic. To address these issues, the present study used a relatively large sample of women who varied with regard to the chronicity and severity of their histories of depressive disorders as well as their current levels of depressive symptoms.
In summary, this study examined the relations among mothers’ prior depressive disorders, current depressive symptoms, and behaviors while interacting with their children during a laboratory problem-solving task. We hypothesized that higher levels of current maternal depressive symptoms and greater chronicity/severity of prior maternal depression would be associated with more negative and less positive maternal behaviors. Current symptoms were expected to be more strongly associated with mothers’ behaviors than past depressive disorders. We further hypothesized that the relation between mothers’ history of mood disorders and her observed behavior would be mediated by her current level of depressive symptoms. Finally, we examined the extent to which maternal behaviors were related to children’s adjustment. In particular, we hypothesized that higher levels of maternal negativity and lower levels of positivity during the problem-solving interaction would each be associated with higher levels of externalizing and internalizing problems in the children; we further predicted that mothers’ observed behaviors during the problem-solving task would mediate the relation between maternal depression and children’s symptoms.
Method
Participants
Participants were 204 children (mean age = 11.86, SD = 0.55) and their mothers who were participating in a larger study of psychopathology in youth. The sample of children was 55.4% female, 82.8% Caucasian, 13.2% African-American, and 3.5% other (Hispanic, Asian, Native American). The families were predominantly working (e.g., nurses aid, sales clerk) and middle class (e.g., store manager, teacher) with a mean socioeconomic status (Hollingshead 1975) of 41.85 (SD = 13.28).
Parents of fifth grade children from metropolitan public schools were invited to participate in a study about parents and children. A brief health history questionnaire comprised of 24 medical conditions (e.g., heart disease, depression) and 34 medications (e.g., Prozac, Elavil) was sent with a letter describing the project to over 3,500 families. Of the 1,495 mothers who responded, the 587 who endorsed either a history of depressive symptoms, use of antidepressants, or no history of psychopathology were interviewed further by telephone. Based on screening calls of the 587 mothers, 349 met inclusion criteria. The 238 families not further screened were excluded because they did not meet criteria for a depressive disorder (38%), had other nondepressive psychiatric disorders (19%), had a serious medical condition (14%), were no longer interested (21%), the target child either was in the wrong grade or was in full-time special education (6%),Footnote 1 or the family had moved out of the area (2%). The Structured Clinical Interview for DSM diagnoses (SCID; Spitzer et al. 1990) then was conducted with the 349 mothers who met initial inclusion criteria; 109 families then were excluded because the interview revealed that they did not meet the inclusion criteria. The final sample of 240 families consisted of 185 mothers who had had a depressive disorder (i.e., 147 with Major Depressive Disorder, 38 with Dysthymia, Depression NOS, or Adjustment Disorder with Depressed Mood) and 55 mothers who were life-time free of psychopathology. Thirty-six of the 240 families were not included in the current study due to one of the following factors: (a) equipment failure during the video-taping of the mother–child interaction, (b) missing questionnaire data, (c) use of a different form of the problem-solving task, or (d) refusal to be videotaped. These 36 families did not differ significantly from the 204 families who participated in the interaction task with regard to demographics or psychopathology. The final sample of 204 families consisted of 157 mothers who had histories of depressive disorders and 47 mothers who were lifetime-free of psychiatric diagnoses.
The interaction task and child symptom data were collected when children were in the sixth grade. A research assistant who was unaware of mothers’ psychiatric history individually administered the questionnaires and conducted the interaction task with the mother–child dyad.
Measures
Mother’s History of Depressive Disorders
Maternal history of depression was assessed with the Structured Clinical Interview for DSM (SCID; Spitzer et al. 1990), a semi-structured diagnostic interview used to assess current and previous episodes of psychopathology according to DSM criteria (American Psychiatric Association 1994). Inter-rater reliability calculated on a random subset of 20% of these interviews indicated 94% agreement (kappa = 0.88) for diagnoses of depressive disorders.
Using the SCID, interviewers collected information regarding the duration, timing, and severity of each of the mothers’ depressive episodes that had occurred during the target child’s lifetime. Based on the work of Keller et al. (1986) and Sameroff et al. (1983), a chronicity/severity index was created. This index (see Horowitz and Garber 2003 for more details) reflected (a) the number of diagnosed depressive episodes the mother experienced during the child’s lifetime, (b) the length of time of each episode, summed to reflect the total amount of time during the child’s life that the mother had been depressed, and (c) the severity of each episode with regard to impairment, hospitalization, suicidality, and psychosis. Four chronicity/severity (CS) groups were formed. Mothers in the nondepressed group (n = 47) had no history of a psychiatric diagnosis. The mild group (n = 43) had experienced no more than two episodes of depression, had been depressed for no more than 1 year during the child’s life, and had not experienced hospitalization, suicidality, or psychosis. The moderate group (n = 70) had had between one and three depressive episodes that had lasted more than 1 year, but less than 4 years of their child’s life, or had experienced one depressive episode of less than 1 year that included hospitalization, a suicide attempt, or psychotic features. The chronic/severe group (n = 44) consisted of mothers who had been depressed for more than 4 years or who had had more than four depressive episodes during their child’s lifetime. There were no significant differences among the above groups with regard to mother’s age, race, or socio-economic status.
Mothers’ Current Depressive Symptoms
Mothers’ current symptoms were assessed with the Beck Depression Inventory (BDI; Beck et al. 1961), a 21-item self-report scale that measures affective, cognitive, behavioral, and somatic symptoms of depression. The BDI has good validity with both psychiatric (Beck et al. 1961) and community samples (Bumberry et al. 1978). Coefficient alpha in this sample was 0.91.
Children’s Externalizing and Internalizing Symptoms
The Child Behavior Checklist (CBCL: Achenbach 1991) is a parent-report instrument used to assess externalizing and internalizing symptoms in children and adolescents. The externalizing subscale includes symptoms of aggression and delinquency; the internalizing subscale measures symptoms of depression, anxiety, somatic complaints, and social withdrawal. Internal consistency in this sample was 0.93 for the externalizing subscale and 0.89 for the internalizing subscale.
Mother–Child Interaction Task
Mothers were asked to collaborate with their child on a set of game-like problem-solving tasks. A research assistant (RA) instructed the mother to “work with your child as you typically would work with him/her on a project or a school assignment.” The tasks consisted of a set of five mazes and a set of scrambled word games (anagrams) presented in increasing levels of difficulty. The mother–child dyads were given 5 min for mazes and 5 min for anagrams. The RA left the room during each task. At the end of the first 5 min, the RA collected the mazes, passed out the anagrams, and reviewed the instructions. The tasks were intended to provide an opportunity for mothers to work with their children on game-like tasks in which the mother could provide guidance and assistance. In contrast to the often used “reveal differences” task, which tends to elicit conflict, the problem-solving task used in the present study was selected to elicit a range of instructive and positive maternal behaviors.
Coding of Maternal Behaviors During the Interaction with their Child
The coding system used to rate maternal behavior was adapted from several existing coding systems (Hetherington and Clingempeel 1992; Holmbeck et al. 1995). Modifications were made to capture the positive and negative maternal behaviors that were expected given theory and previous research regarding behaviors of depressed mothers and the particular problem-solving task used in the current study.
Maternal behaviors were micro-coded on 14 specific positive and negative verbal and nonverbal behaviors (e.g., smiling, tries to take over task), scored according to the frequency with which they occurred during each 5-min task. In addition, seven positive and negative global maternal features (e.g., warmth, critical) were macro-coded using a 5-point Likert scale (1 = not at all, 2 = somewhat, 3 = moderately, 4 = very, 5 = extremely) based on the coder’s overall impression of the mother’s behaviors and affect during the tasks. Each task was coded separately, yielding scores for the mazes and the anagrams. For both the micro- and macro-coding systems, higher scores reflected more of the construct being observed.
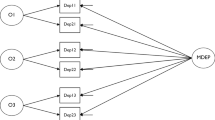
Reduction of Observational Data
Observational data were standardized using z scores and a factor analysis (Thompson 2004) was performed using principal components extraction with varimax rotation. A two factor solution reflecting maternal positivity and negativity was expected based on previous research (e.g., Dallaire et al. 2006) and strong support was found for a two factor solution. The eigenvalue for factor 1 (maternal positivity) was 7.75 and the eigenvalue for factor 2 (maternal negativity) was 4.65. Items that loaded 0.4 or higher on each factor were retained. Table 1 presents the final item composition of each factor and factor loadings. The final maternal positivity scale consisted of 14 items (alpha = 0.87) that measured such behaviors as smiling, laughing, use of praise, warmth, consistent interest and involvement, and providing constructive assistance. The final maternal negativity scale consisted of ten items (alpha = 0.79) including behaviors such as criticism, issuing orders about how to approach the task, trying to take control of the task away from the child, and displaying negative affect.
Inter-rater Reliability
The first author (CEF), who was unaware of mothers’ depression status, coded all tapes and a 20% randomly selected sample of tapes was independently coded by two trained research assistants to establish inter-rater reliability using Pearson r correlation coefficients. Inter-rater agreement averaged 0.78 across all items. Kappa coefficients were not calculated because of the frequency tally metric (Cohen 1960).
Results
Data Analyses
Table 2 presents the means, standard deviations, and correlations for observational data summary scores and predictor variables. Mothers reported a range of current depressive symptoms; 73% of women reported a BDI score within the normal range (Total score = 0–9); 20% reported mild to moderate symptoms (Total score = 10–16); and 7% reported moderate to severe symptoms (Total score = 20–42) (Beck et al. 1961). Mothers’ current depressive symptoms were significantly related to maternal depression history (r (200) = 0.45, p < 0.001); an analysis of variance indicated that each chronicity/severity group (Healthy group BDI mean = 1.41, SD = 1.92; Mild group Mean = 6.24, SD = 7.21; Moderate group Mean = 7.83, SD = 7.95; Severe group Mean = 12.02, SD = 8.04) differed from the other groups on level of current symptoms (F(3, 196) = 17.08, p < 0.001), except that the mild and moderate groups did not differ significantly from each other. Among the children, 10 and 12% fell within the clinical range (T score ≥ 65) for externalizing or internalizing problems, respectively.
Relation of Maternal Depression to Mothers’ Interaction Behaviors
Regression analyses were conducted to examine the relation between previous and current maternal depression and maternal interaction behaviors (observed positivity and negativity). Mothers’ current depressive symptoms (i.e., BDI) were significantly related to maternal positivity (Beta = −0.27, R 2 = 0.07, p < 0.001) and negativity during the interaction task (Beta = 0.19, R 2 = 0.03, p < 0.01). That is, higher levels of current depressive symptoms were associated with lower levels of positive affect and behavior and higher levels of negative affect and behavior in mothers during the interaction task. Chronicity/severity of mother’s depression history was significantly and negatively related to observed maternal positivity during the interaction (Beta = −0.21, R 2 = 0.04, p < 0.01), but not to observed maternal negativity. Analysis of Variance indicated a significant difference between the levels of positivity among mothers in the severe group (Mean = −3.17) and mothers in the healthy group (Mean = 2.72).
Next, we explored the relative contribution of chronicity/severity of maternal depression history and current depressive symptoms to mothers’ interaction behaviors by entering both variables simultaneously into the same regression analysis. Mothers’ current depressive symptoms were significantly associated with both positive (Beta = −0.21, p < 0.01) and negative (Beta = .18, p < 0.05) interaction behaviors over and above the variance explained by depression history (Beta = −0.12 ns and Beta = 0.01 ns, respectively).
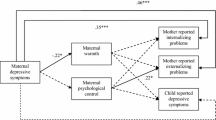
To test whether mothers’ current depressive symptoms mediated the relation between their depression history and their observed behavior, we followed established procedures for testing mediation (Baron and Kenny 1986). Significant relations were found between mother’s depression history and current depressive symptoms, and between current symptoms and observed positivity (see Fig. 1). Chronicity/severity of mother’s depression history was significantly and negatively related to maternal positivity (Beta −0.21, p < 0.01), and this relation was significantly reduced (Beta = −0.12 ns) when the hypothesized mediator (current depressive symptoms) was included in the model. Using equations suggested by Sobel (1988) and Holmbeck (2002), a z statistic can be computed based on unstandardized beta weights and standard errors, and then compared to a table of critical values. The z = −3.78 significantly exceeded the critical value of 1.96 required for p < 0.05, thus indicating that the amount of mediation was significantly different from zero. Using an equation recommended by MacKinnon and Dwyer (1993), we found that 48% of the variance in the relation between depression history and maternal positivity was accounted for by mothers’ current depressive symptoms.
Relation of Maternal Interaction Behaviors to Children’s Symptoms
Mothers’ levels of both positivity and negativity during the interaction significantly predicted children’s externalizing behaviors.Footnote 2 , Footnote 3 That is, higher levels of maternal positivity were associated with lower levels of offspring externalizing problems (Beta = −0.28, R 2 = 0.08, p < 0.001); higher levels of maternal negativity were associated with higher levels of offspring externalizing symptoms (Beta = 0.15, R 2 = 0.02, p < 0.05).Footnote 4 Neither maternal positivity nor negativity significantly predicted children’s internalizing symptoms.
Relations among Maternal Depression, Maternal Interaction Behaviors, and Children’s Symptoms
A series of regression analyses were conducted to examine whether maternal interaction behaviors mediated the relation between maternal depression and children’s symptoms. First, we tested whether the relation between mothers’ current depressive symptoms and children’s externalizing symptoms was mediated by maternal positivity and negativity, and second, whether the relation between mothers’ depression history and children’s externalizing symptoms was mediated by maternal positivity.
The association between mother’s current depressive symptoms and children’s externalizing behaviors was significant (Beta = 0.42, p < 0.001); and, as reported above, mother’s current depressive symptoms were significantly associated with her level of positivity during the interaction. When the hypothesized mediator of maternal positivity was added, the relation between mothers’ current depressive symptoms and children’s externalizing was reduced (Beta = 0.37, p < 0.001) (see Fig. 2). Although modest, this reduction was significantly different from zero (z = 2.904, p < 0.05), accounting for 10% of the variance (MacKinnon and Dwyer 1993) in the relation between mothers’ current depressive symptoms and children’s externalizing symptoms.
Regression models testing maternal negativity as a mediator between mother’s current depressive symptoms and children’s externalizing problems resulted in no significant reduction in the relation between maternal depression and children’s externalizing (which remained at Beta = 0.42, p < 0.001). Thus, both mothers’ depressive symptoms and observed negativity were significant and separate predictors of children’s externalizing behaviors.
Finally, the chronicity/severity of mother’s depression history significantly predicted children’s externalizing behaviors (Beta = 0.36, p < 0.001). Analysis of variance indicated that children of mothers in each chronicity/severity group differed significantly from children of never depressed mothers on level of externalizing symptoms. Maternal depression chronicity/severity also was significantly associated with levels of maternal positivity during the problem-solving tasks (Beta = −0.21, p < 0.01) (see Fig. 3). When the hypothesized mediator (observed maternal positivity) was added to this regression equation, there was a significant (z = 2.51, p < 0.05) reduction of the effect (Beta = 0.30, p < 0.001), accounting for 16.7% of the variance. Thus, the relation between the chronicity/severity of mothers’ depression history and children’s externalizing symptoms was partially mediated through mothers’ levels of positive behaviors during the interaction task.
Discussion
The purpose of the present study was to investigate relations among different aspects of maternal depression (i.e., chronicity/severity of depression history and current symptom levels), mothers’ behaviors during a laboratory interaction task with their children, and the children’s adjustment. As hypothesized, higher levels of current maternal depressive symptoms were associated with less positive and more negative maternal behaviors including lower levels of laughter, praise and support of their children’s efforts, fewer constructive and useful suggestions during the task, and more negative affect, criticism, and controlling behaviors. These results are consistent with other studies that have found that currently depressed women are more likely to display higher negativity and lower positivity toward their children, compared to nondepressed mothers (Lovejoy et al. 2000). The present study extends this literature by demonstrating these maternal behaviors during interactions with young adolescent offspring who have been studied far less than infants and toddlers (Goodman and Gotlib 1999; Lovejoy et al. 2000).
This study also expanded the literature by using a problem-solving task rather than a conflict-inducing interaction. Nevertheless, depressed mothers still engaged in more negative and less positive behaviors during a task that was intended to elicit parental behaviors such as helping and teaching. Clinically, this finding is concerning because it implies that currently depressed women may be less able to muster the energy to be positive with their children and may have difficulty concealing their irritability, even during family times that are meant to be instructive or enjoyable. In addition, depressed women may be less able to support their children through the challenging aspects of a task. Theories of child development (e.g., Vygotsky 1978) suggest that parents can further a child’s learning by allowing the child to grapple with challenges, while providing “scaffolding” that may include tangible assistance, and help with affect regulation and frustration-tolerance. These results showed that, at least in this context, depressed women may have found it difficult to provide this type of scaffolding for their children. Future research should investigate whether the maternal behaviors evident in this study would be similar across other “helping” tasks, such as when young adolescents seek guidance from parents about interpersonal problems, academic assignments, or other life challenges.
In addition, studies need to explore whether and how depressed mothers transfer knowledge about problem-solving to their children, and how this process impacts children’s development. For example, offspring of depressed women may have more poorly developed problem-solving or executive function skills because such organizing strategies have not been taught or modeled for them. Moreover, children whose mothers are intrusive or controlling may develop less self-confidence about their own abilities or may derive less satisfaction from their achievements. An important clinical implication is that mothers in treatment for depression might benefit from supplementary interventions that directly address their parenting skills.
The present study also examined the relative contribution of mothers’ current and past depression to their interaction behaviors and to their children’s symptoms. Whereas mothers’ current depressive symptoms were related to both how negative and positive she acted toward her child, a history of chronic/severe depressive episodes was linked with lower levels of positive, but not negative, current interaction behaviors. Weinberg and Tronick (1998) found that depressed women whose symptoms improved during treatment continued to behave less positively with their infants compared to nondepressed controls. The present findings suggest that previous depression may continue to impact mothers’ current functioning by affecting their positive parenting behaviors. Other studies (e.g., Murray et al. 2006), however, have not found a significant relation between mothers’ psychiatric history and maternal behavior. Such discrepant findings across studies might have been partially due to differences in the methods (e.g., tasks) and samples (e.g., child age, timing of mothers’ depression) used.
We found that mothers’ current levels of depressive symptoms had a stronger relation to their interaction behaviors than did the chronicity/severity of their depression histories, and partially mediated the relation between depression history and maternal interaction behaviors, accounting for 48% of the variance. That is, more chronic/severe histories of maternal depression predicted a greater likelihood of higher levels of current depressive symptoms, which in turn, predicted fewer positive maternal behaviors during the interaction task. Given the relapsing nature of mood disorders, these findings suggest that interventions should particularly target mothers with chronic/severe histories who are experiencing current depressive symptoms.
Partial support was found for the hypothesis that mothers’ interaction behaviors would be associated with their children’s symptoms. Higher levels of maternal negativity and lower levels of maternal positivity were significantly associated with higher levels of children’s externalizing problems, although not internalizing symptoms. These findings are consistent with a growing recognition that an absence of maternal positivity is related to children’s externalizing behaviors (Chronis et al. 2007). Ge et al. (1996) reported that mothers of children who later developed externalizing problems were lower in warmth than mothers of healthy children. Additionally, the importance of maternal positivity has been emphasized in treatment studies with young children (Eyberg and Boggs 1989) that have attempted to remediate children’s behavior problems by increasing positive parent–child interactions and teaching parents to praise and label children’s positive behaviors (Barkley 1997). These evidence-based treatment protocols highlight the need to increase parents’ positive interactions with their children in order to decrease the likelihood of children’s behavior problems.
Differences in the age of onset of internalizing versus externalizing problems may partially explain the current findings. Externalizing problems often begin earlier (between ages 6 and 10) than do internalizing problems, particularly depression, which tends to emerge about age 14 or 15 (Angold and Costello 2001). It is possible that relations between maternal interaction behaviors and children’s internalizing problems might not become apparent until these children move further into adolescence.
Tests of mediation models indicated that the relation between maternal depression (defined as either current symptoms or chronicity/severity of depression history) and children’s externalizing symptoms was partially mediated by mother’s level of positivity in interaction with her child, accounting for 10 and 17% of the variance, respectively. Maternal negativity, however, did not mediate the relation between maternal depression and children’s symptoms. Thus, the extent of mothers’ positive engagement with their children may be an important mechanism by which maternal depression impacts children’s behavior problems. It is important to note, however, that the amount of variance in the relation between maternal depression and children’s externalizing symptoms explained by maternal behaviors was relatively small. As other research studies suggest (e.g., Conduct Problems Prevention Research Group 1992), the development of disruptive behavior problems involves many risk factors, and maternal depression can affect children in different ways (Goodman and Gotlib 1999) (e.g., poor parenting, exposure to family discord, modeling of ineffective coping strategies). The current results suggest that one possible mechanism by which maternal depression may increase risk for behavior problems in offspring is through the absence of a positive mother–child relationship.
Limitations of the present study suggest directions for future research. First, the coding system only focused on maternal behavior and affect. As a result, we cannot draw conclusions about children’s behaviors during the interaction, or the ways in which children’s behaviors may have influenced maternal behaviors. The behaviors and characteristics of children (e.g., temperament, psychopathology) as well as the fit between parent and child can influence parenting styles, the quality of the parent–child relationship, and child outcomes (Anderson et al. 1986; Thomas and Chess 1977). Future research should examine children’s interaction behaviors and explore the sequential relations between mother and child behaviors.
Second, the data were basically cross-sectional, except for mothers’ history of depressive disorders. Mother’s current symptoms, interaction behaviors, and child adjustment were all measured at the same time point. A longitudinal examination of these relations is needed to address the temporal associations among these variables across time.
A third limitation was the use of mothers as informants about children’s symptoms. Although mothers’ perceptions of their children may influence how they act toward them, mothers’ report also may have been affected by their current depressive symptoms. Evidence has been mixed regarding the presence of a depressive bias in reporting about children’s behavior problems, with some studies showing that depressed women are negatively biased, and others showing that depressed women actually may be more accurate in perceiving their children (Ackerman and DeRubeis 1991; Richters 1992). Future research should include multiple informants to ascertain the extent to which children’s problems are similarly reported by another parent, teachers, or the children themselves, and whether these reports also are linked with maternal interaction behavior.
In summary, the present study examined the extent to which maternal depression was associated with maternal interaction behaviors and their children’s adjustment. Mothers’ current depressive symptoms and the chronicity/severity of their prior depressive disorders both were associated with how positively mothers behaved during a problem-solving interaction with their children, whereas only current symptoms were associated with maternal negativity. Maternal interaction behaviors, in turn, were associated with children’s externalizing symptoms. Finally, the relation of maternal depression to children’s externalizing behaviors was partially mediated by how positive mothers were during their interactions with their children. An important clinical implication of these results is that depressed mothers and their children may benefit from interventions that increase mothers’ positive parenting behaviors.
Notes
Students in full-time special education classes were excluded due to concerns about their being able to complete the battery of questionnaires, which required at least a fifth grade reading level.
Demographic variables investigated as potential control variables included SES, race, mother’s age, and mother’s marital status. Because inclusion of these variables did not alter the findings, and these variables were not hypothesized to affect the relation between maternal depression and mothers’ interaction behaviors, they were trimmed from the models.
Due to concerns about depressive bias in maternal reporting, these analyses were repeated using the Youth Self-Report version of the CBCL. Results were identical using the CBCL and YSR with the exception of the relation between maternal negativity and externalizing (YSR), which was a trend. We used the CBCL because parents’ report of externalizing behaviors tends to be more accurate than children’s report, and given the age of the sample, we expected more externalizing problems than internalizing problems.
Child gender was significantly correlated with CBCL internalizing and externalizing scores, so gender was initially used as a control variable. Because its inclusion did not alter the results and because gender differences were not hypothesized, gender was trimmed from the final model.
References
Achenbach, T. M. (1991). Manual for the youth-self-report and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry.
Ackerman, R., & DeRubeis, R. J. (1991). Is depressive realism real? Clinical Psychology Review, 11, 565–584.
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders ((4th.) ed.). Washington, D.C.: Author.
Anderson, K. E., Lytton, H., & Romney, D. M. (1986). Mothers’ interactions with normal and conduct disordered-boys: Who affects whom? Developmental Psychology, 22, 604–609.
Angold, A., & Costello, E. J. (2001). The epidemiology of depression in children and adolescents. In I. M. Goodyer (Ed.), Cambridge child and adolescent psychiatry. The depressed child and adolescent (2nd ed., pp. 143–178). Cambridge University Press.
Barkley, R. A. (1997). Defiant children. New York: Guilford.
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 61, 1173–1182.
Beck, A. T., Ward, C. F., Mendelson, M., Mock, J., & Erlbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 53–63.
Brennan, P., Hammen, C., Andersen, M. J., Bor, W., Najman, J. M., & Williams, G. M. (2000). Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology, 36, 759–766.
Brennan, P. A., LeBrocque, R., & Hammen, C. (2003). Maternal depression, parent–child relationships, and resilient outcomes in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1469–1477.
Bumberry, W., Oliver, J. M., & McClure, J. N. (1978). Validation of the Beck depression Inventory in a university population using psychiatric estimate as the criterion. Journal of Consulting and Clinical Psychology, 46, 150–155.
Campbell, S. B., Cohn, J. F., & Meyers, T. (1995). Depression in first-time mothers: Mother–infant interaction and depression chronicity. Developmental Psychology, 31, 349–357.
Chronis, A. M., Lahey, B. B., Pelham, W. E., Williams, S. H., Baumann, B., Kipp, H., et al. (2007). Maternal depression and early positive parenting predict future conduct problems in young children with attention deficit/hyperactivity disorder. Developmental Psychology, 43, 70–82.
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 10, 37–46.
Cole, D. A., Warren, D. E., Dallaire, D. H., Lagrange, B., Travis, R., & Ciesla, J. (2007). Early predictors of helpless thoughts and behaviors in children: Developmental precursors to depressive cognitions. Clinical Child Psychology and Psychiatry, 12, 295–305.
Conduct Problems Prevention Research Group (1992). A developmental and clinical model for the prevention of conduct disorder: The FAST Track Program. Development and Psychopathology, 4, 509–527.
Cox, A. D., Pickering, C., Pound, A., & Mills, M. (1987). The impact of maternal depression in young children. Journal of Child Psychology and Psychiatry, 28, 917–928.
Dallaire, D. H., Pineda, A. Q., Cole, D. A., Ciesla, J. A., Jacquez, F., LaGrange, B., et al. (2006). Relation of positive and negative parenting to children’s depressive symptoms. Journal of Clinical Child and Adolescent Psychology, 35, 313–322.
Donenberg, G. R., & Weisz, J. R. (1997). Experimental task and speaker effects on parent child interactions of aggressive and depressed/anxious children. Journal of Abnormal Child Psychology, 25, 367–387.
Eyberg, S. M., & Boggs, S. R. (1989). Parent training for oppositional-defiant pre-schoolers. In C. E. Schaeffer, & J. M. Briesmeister (Eds.) (pp. 105–132). New York: Wiley.
Field, T. (1984). Early interactions between infants and their post-partum depressed mothers. Infant Behavior and Development, 7, 527–532.
Garber, J., Robinson, N. S., & Valentiner, D. (1997). The relation between parenting and adolescent depression: Self-worth as a mediator. Journal of Adolescent Research, 12, 12–33.
Ge, X., Best, K. M., Conger, R. D., & Simons, R. L. (1996). Parenting behaviors and the occurrence and co-occurrence of adolescent depressive symptoms and conduct problems. Developmental Psychology, 32, 717–731.
Goldsmith, D. F., & Rogoff, B. (1995). Sensitivity and teaching by dysphoric and nondysphoric women in structured and nonstructured situations. Developmental Psychology, 31, 388–394.
Goldsmith, D. F., & Rogoff, B. (1997). Mothers’ and toddlers’ coordinated joint focus of attention: Variations with maternal dysphoric symptoms. Developmental Psychology, 33, 113–119.
Goodman, S. H., & Gotlib, I. H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490.
Goodman, S. H., & Gotlib, I. H. (Eds.), (2002). Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: APA.
Gordon, D., Burge, D., Hammen, C., & Adrian, C. (1989). Observations of interactions of depressed women with their children. American Journal of Psychiatry, 146, 50–55.
Hamilton, E. B., Jones, M., & Hammen, C. (1993). Maternal interaction style in affective disordered, physically ill, and normal women. Family Process, 32, 329–340.
Hammen, C. (1992). The family-environmental context of depression: A perspective on children’s risk. In D. Cicchetti, & S. L. Toth (Eds.) Rochester symposium on developmental psychopathology, Vol. IV. Developmental perspectives on depression (pp. 251–281). Rochester, NY: University of Rochester Press.
Hammen, C., Gordon, G., Burge, D., Adrian, C., Jaenicke, C., & Hiroto, G. (1987). Maternal affective disorders, illness, and stress: Risk for children’s psychopathology. American Journal of Psychiatry, 144, 736–741.
Heller, T. L., & Baker, B. L. (2000). Maternal negativity in children’s externalizing behavior. Early Education and Development, 11, 483–498.
Hetherington, E. M., & Clingempeel, W. G. (1992). Coping with marital transitions. Monographs of the Society for Research in Child development, 57(2–3, Serial No. 277), 1–242.
Hollingshead, A. B. (1975). Four factor index of social status. Yale University.
Holmbeck, G. N. (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27, 87–96.
Holmbeck, G. N., Belvedere, M., Gorey-Ferguson, L., & Schneider, J. (1995). Family Macro-Coding Manual.
Horowitz, J. L., & Garber, J. (2003). Relation of intelligence and religiosity to depressive disorders in offspring of depressed and nondepressed mothers. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 578–586.
Jacob, T., & Johnson, S. L. (1997). Parent child interaction among depressed fathers and mothers: impact on child functioning. Journal of Family Psychology, 11, 391–409.
Keller, M., Beardslee, W., Dorer, D., Lavori, P., Samuelson, H., & Klerman, G. (1986). Impact of severity and chronicity of parental affective illness on adaptive functioning and psychopathology in children. Archives of General Psychiatry, 43, 930–937.
Kim-Cohen, J., Moffit, T. E., Taylor, A., Pawlby, S. J., & Caspi, A. (2005). Maternal depression and children’s antisocial behavior: Nature and nurture effects. Archives of General Psychiatry, 62, 173–181.
Lovejoy, M. C., Graczyk, P. A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting: A meta-analytic review. Clinical Psychology Review, 20, 561–592.
MacKinnon, D. P., & Dwyer, J. H. (1993). Estimating mediated effects in prevention studies. Evaluation Review, 17, 141–158.
Murray, L., Woolgar, M., Martins, C., Christaki, A., Hipwell, A., & Cooper, P. (2006). Conversations around homework: Links to parental mental health, family characteristics and child psychological functioning. British Journal of Developmental Psychology, 24, 125–149.
Pettit, J. W., & Joiner, T. E. (2006). Chronic depression: Interpersonal sources, therapeutic solutions. Washington, DC: APA.
Richters, J. E. (1992). Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin, 112, 485–499.
Sameroff, A. J., Seifer, R., & Barocas, R. (1983). Impact of parental psychopathoplogy: Diagnosis, severity, or social status effects. Infant Mental Health Journal, 4, 236–249.
Sameroff, A. J., Seifer, R., & Zax, M. (1982). Early development of children at risk for emotional disorder. Monographs of the Society for Research in Child Development, Vol 47(7).
Sobel, M. E. (1988). Direct and indirect effect in linear structural equation models. In J. S. Long (Ed.) Common problems/proper solutions: Avoiding error in quantitative research (pp. 46–64). Beverly Hills, CA: Sage.
Spitzer, R. L., Williams, J. B. W., Gibbon, M., & First, M. B. (1990). The structured clinical interview for DSM-III-R (SCID) I: History, rationale, and description. Archives of General Psychiatry, 49, 624–628.
Thomas, A., & Chess, S. (1977). Temperament and development. New York: Bruner/Mazel.
Thompson, B. (2004). Exploratory and confirmatory factor analysis: Understanding concepts and applications. Washington, DC: APA.
Weinberg, M. K., & Tronick, E. (1998). The impact of maternal psychiatric illness on infant development. Journal of Clinical Psychiatry, 59, 53–61.
Weissman, M., Pilowsky, D. J., Wickramaratne, P. J., Talati, A., Wisniewski, S. R., Fava, M., et al. (2006). Remissions in maternal depression and child psychopathology: A STAR*D-Child report. Journal of the American Medical Association, 295, 1389–1398.
Wickramaratne, P. J., & Weissman, M. M. (1998). Onset of psychopathology in offspring by developmental phase and parental depression. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 933–942.
Vygotsky, L. S. (1978). Prehistory of written speech. Social Science, 17, 1–17.
Acknowledgement
The authors would like to acknowledge Children’s Hospitals and Clinics, Minneapolis-St. Paul and the University of Michigan for providing support to the first author during completion of this project. This work was supported in part by grants from the National Institute of Mental Health (MH4545801; MH57822), NICHD GrantP30HD15052, and the William T. Grant Foundation (173096) awarded to the second author. We would all like to thank the parents and children who participated in this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is derived from the first author’s dissertation, completed at Loyola University Chicago under the direction of the third author.
Rights and permissions
About this article
Cite this article
Ewell Foster, C.J., Garber, J. & Durlak, J.A. Current and Past Maternal Depression, Maternal Interaction Behaviors, and Children’s Externalizing and Internalizing Symptoms. J Abnorm Child Psychol 36, 527–537 (2008). https://doi.org/10.1007/s10802-007-9197-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-007-9197-1