Abstract
Male breast cancer is rare, accounting for 1% of all breast cancer diagnoses in the USA. Because of its rarity, most major breast cancer trials have included only female patients. This has resulted in limited prospective data to guide the clinical management of men with breast cancer. As a result, treatment decisions are typically extrapolated from data generated in female patients. This approach may be suboptimal, particularly considering the differing hormonal milieus between men and women with respect to both breast cancer development and treatment. Herein, we summarize current knowledge of the biology and clinicopathology of male breast cancer and review current approaches to locoregional and systemic management of this rare disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
While great strides have been made over recent years in screening, diagnosis, and treatment strategies for female breast cancer, we know little about the optimal management for male patients. The relative rarity of male breast cancer is an obstacle to prospective evaluation, and the resulting paucity of data is compounded by the frequent exclusion of male patients from clinical trials.
Due to the lack of prospective data and guidelines focused on male breast cancer, most of the treatment approaches recommended by clinicians are extrapolated from data generated in female patients, or based on lower levels of evidence (e.g., case reports/series or small retrospective cohorts). However, mirroring the management of female breast cancer may be suboptimal in some instances. For example, differences in the hormonal milieu between men and women could impact the efficacy of treatments, particularly those aimed at manipulating hormone receptor signaling.
In this review, we aim to summarize and highlight some of the key biological similarities and differences between male and female breast cancer, and review current approaches to managing this rare disease.
2 Epidemiology and risk factors
Male breast cancer is rare, accounting for < 1% of all breast cancer diagnoses in the USA and < 0.1% of cancer-related deaths in men. In 2017, it is estimated that 2470 men will be diagnosed with breast cancer in the USA, and 460 will die from the disease; in contrast, there will be an estimated 252,710 new diagnoses, and 40,610 deaths, in women [1]. For the last three decades, however, the incidence of male breast cancer appears to be slowly rising [2]. Risk factors for breast cancer in men are summarized in Table 1.
Men tend to be diagnosed with breast cancer at a later age than women, with median ages at diagnosis of 67 years and 61 years, respectively [3]. Male breast cancer is more common among black men, who have an incidence of 1.8 per 100,000, compared to 1.1 per 100,000 in white men. In black men, as in black women, breast cancer has worse prognostic features, including more advanced stage at diagnosis and higher tumor grade [4].
As in women, certain germline mutations predispose men to developing breast and other cancers. Overall, 15–20% of men with breast cancer report a family history of breast or ovarian cancer [3], and approximately 10% carry a known hereditary breast cancer predisposition gene mutation, with BRCA2 being the most clearly associated abnormality [5,6,7,8,9,10,11]. Men with deleterious BRCA2 mutations have an estimated lifetime risk of breast cancer of 1 to 6%, compared with 0.1% in the general male population [11,12,13]. Put into perspective, the lifetime risk of breast cancer for the general female population is estimated around 12% [2]. The risk of breast cancer among male BRCA1 mutation carriers is lower (lifetime risk of 1%) [13,14,15]. Other genes reported to be associated with male breast cancer include PALB2, PTEN, TP53, and CHEK2 [11, 16,17,18]. In addition, 3–7.5% of men with breast cancer have Klinefelter syndrome (XXY) [19, 20]. Given these data, genetic counseling and testing should be considered for men with breast cancer. The National Comprehensive Cancer Network recommends that men who carry deleterious BRCA mutations perform regular breast self-examinations and undergo annual clinical breast examinations starting at age 35 [21]. A prior recommendation for annual mammography was dropped in 2015 due to insufficient supportive evidence. However, the Spanish Society of Medical Oncology recommends that male deleterious mutation carriers have annual breast examinations and annual mammography starting at age 40 [22]. There are no data to guide us regarding risk-reducing bilateral prophylactic or contralateral prophylactic mastectomy for affected males. These are generally discouraged because of the low absolute risk of breast cancer. With regard to other cancers, the National Comprehensive Cancer Network recommends prostate cancer screening starting at age 45, and to consider melanoma screening with full-body skin and eye exam for men with BRCA2 mutations [21].
3 Clinicopathological features
The most reliable and up-to-date data on clinicopathological features of male breast cancer come from the retrospective portion of the EORTC 10085/TBCRC/BIG/NABCG International Male Breast Cancer Program [23, 24]. This large international joint analysis of clinical and biological data evaluated a retrospective cohort of male breast cancer patients diagnosed between 1990 and 2010. Further, 1483 tumors underwent central pathology review, improving our understanding of male breast cancer histopathology. Below, we summarize the key findings from this important analysis.
3.1 Clinical presentation and stage at diagnosis
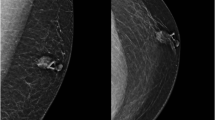
Most male breast cancers present as a subareolar painless mass [25]. Nipple retraction or ulceration can also be seen. Nipple discharge or bleeding is rare. Studies consistently show that breast cancer in men is generally diagnosed at a more advanced stage than in women (Fig. 1) [3]. This is likely related to the lack of mammographic screening in men, and possibly due to lack of awareness that men can develop breast cancer.
Breast cancer stage distribution by sex. Generated from SEER incidence cases between 2006 and 2015, including all ages and races. SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Beta Version. Surveillance Research Program, National Cancer Institute. [Cited 2017 Apr 14]. Available from https://seer.cancer.gov/explorer/
In the EORTC 10085/TBCRC/BIG/NABCG study, tumor stage was T1 in 49%, T2 in 38%, T3 in 2%, and T4 in 11%. Pathologic nodal stage was N0 in 59%, N1 in 32%, N2 in 5%, and N3 in 3%. Four percent had de novo metastatic disease (missing data on M status at diagnosis in 25%). For those with metastatic disease, the most common sites were bone (22%), lung (13%), and distant lymph nodes (7%). Other studies have found a similar distribution of tumor size, but a lower proportion with node-negative disease and lower rates of distant metastatic disease [26].
3.2 Histologic subtypes
The most common histological subtype was ductal carcinoma not otherwise specified (87%), consistent with previous studies [27,28,29]. In contrast, ductal carcinoma only accounts for 74% of all cases of female breast cancer [30]. Other histologic subtypes were extremely uncommon in men (invasive lobular 1.4%; mixed ductal and lobular features 5.9%; papillary 3%; mucinous 1.3%; cribriform, tubular, metaplastic, adenoid cystic, and others < 1% each).
3.3 Grade and mitotic activity
While histologic grade is prognostic in women [with higher grade associated with worse relapse-free survival (RFS) and overall survival (OS)] [31], and the grade distribution observed in the EORTC 10085/TBCRC/BIG/NABCG study was similar to what has been reported in women, this study surprisingly did not identify an association between grade and prognosis in men. However, patients with higher number of mitoses had worse RFS [hazard ratio (HR) 1.41; 95% confidence interval (CI) 1.03–1.94, p = 0.024 for those with > 7 mitoses] and OS (HR 1.39; 95% CI 1.07–1.82, p = 0.023 for those with > 7). In addition, the presence of a fibrotic focus (32% of cases), was also associated with worse RFS (HR 1.67, 95% CI 1.29–2.18) and OS (HR 1.29, 95% CI 1.11–1.74, p = 0.004).
3.4 Molecular subtypes (gene expression profiling)
Gene expression profiling has emerged as a method to identify and categorize intrinsic tumor subtypes. In female breast cancer, four distinct subtypes of breast cancer have been identified (Luminal A, Luminal B, HER2-enriched, and basal-like). However, few male breast cancers were included in these studies. In the landmark comprehensive genomic characterization of breast cancer performed by The Human Cancer Genome Atlas, only 6 of the 507 (1%) tumors sequenced were from men [32].
An early study that evaluated sex-specific gene expression profiles retrospectively compared 37 estrogen receptor (ER)-positive archived male breast cancer specimens to 53 ER-positive archived female specimens. Tissue microarray identified 1273 differentially expressed transcripts corresponding to 920 annotated genes using a stringent false discovery rate of 1%. A broad spectrum of cellular processes was differentially expressed in male breast cancer, including immune system response, cell metabolism, cell motility, and steroid response [33]. In an additional study, tissue microarray including 66 male breast cancer tumors identified two unique intrinsic subtypes, distinct from female breast cancer, categorized as luminal M1 and luminal M2. Despite a high rate of ER positivity, luminal M1 tumors had a comparatively lower estrogen-related signaling profiles, suggesting that alternate pathways driving tumor growth may be involved [34]. A separate analysis of 59 male breast cancer tumors suggested that while the repertoire of somatic alterations identified was similar to ER-positive/HER2-negative female breast cancers, male tumors less frequently harbored PIK3CA and TP53 mutations or 16q losses, while they were significantly enriched for mutations in DNA repair-related genes [35].
In the EORTC 10085/TBCRC/BIG/NABCG International Male Breast Cancer Program, most tumors were luminal-like (based on immunohistochemistry), with 42% of tumors being luminal A-like, 49% luminal B-like/HER2-negative, and 8% luminal B-like/HER2-positive. Non-luminal HER2-positive and basal subtypes were extremely rare (0.1 and 1%, respectively, Fig. 2) [23].
The aforementioned differences in gene expression profiling between male and female breast cancers may limit the use of clinically available gene expression tests (such as Oncotype DX or Mammaprint) used to estimate recurrence risk and degree of benefit of adjuvant chemotherapy, as these have primarily been developed and validated in female breast cancer (see section “Use of gene expression profiles for risk-stratification” later in this manuscript).
3.5 Tumor-infiltrating lymphocytes
The presence of high levels of tumor-infiltrating lymphocytes (TILs), a surrogate for adaptive immune system activation, is emerging as an important prognostic and predictive risk factor in female breast cancer, particularly in triple-negative and HER2-positive disease. In multiple studies, high TIL levels were associated with improved outcomes for patients with these disease subtypes. In the neoadjuvant setting, high TILs are associated with increased rates of pathologic complete response [36,37,38,39,40]; in the adjuvant setting, high TILs are associated with longer disease-free survival (DFS) and improved OS, independent of other known prognostic factors [41,42,43,44]. Interestingly, an inverse prognostic role of TILs is apparent in ER+/HER2- female breast cancer, with higher TIL levels found to be detrimental [45].
In the EORTC 10085/TBCRC/BIG/NABCG cohort, most patients had low levels of TILs (categorized as minimal in 25% and mild in 60% and of cases), while the remainder had moderate or high levels. Akin to what has been observed in female breast cancer, the presence of HER2-positive disease was associated with higher levels of TILs [41]. Similarly, patients with any disease subtype and a minimal TIL density had the worst RFS and OS when compared to those with higher levels. The number of patients with TNBC/basal subtypes was too small to draw conclusions for this subtype (n = 13). While this is the largest analysis of TILs performed in male breast cancer patients, conclusions are limited by the methodology used [46], which was not in accordance with the TIL Working Group recommendations for the evaluation of TILs in breast cancer [47], published after the EORTC 10085/TBCRC/BIG/NABCG study initiated. Future analyses in accordance with these guidelines are warranted.
4 Treatment for early-stage disease
A suggested algorithm for the management of male breast cancer is illustrated in Fig. 3.
Suggested algorithm for the management of male breast cancer. 1Staging evaluation as per female breast cancer guidelines. Consider testing for hereditary breast cancer predisposition genetic syndromes. 2If germline BRCA mutation identified, potential role for PARP inhibitors. 3ALND recommended if SLNB positive. 4PMRT as per FBC guidelines. 5Consider genomic profiling to assist decision regarding adjuvant chemotherapy. 6With tamoxifen after completion of chemotherapy if HR(+). 7visceral crisis, bulky/symptomatic disease, rapidly progressive disease. 8Sequential single-agent chemotherapy preferred. Combination may be considered if rapid response needed. AI aromatase inhibitor, ALND axillary lymph node dissection, FBC female breast cancer, GnRHa gonadotropin-releasing hormone agonist, HR hormone receptor, PMRT post-mastectomy radiation, SLNB sentinel lymph node biopsy, TNBC triple-negative breast cancer
4.1 Breast surgery
For male breast cancer, conventional treatment has been mastectomy with either axillary dissection for clinically node-positive patients or sentinel lymph node (SLN) surgery with selective axillary dissection based on pathologic status of the SLN [24, 26, 48,49,50,51,52,53,54]. Limited data suggest that breast conservation therapy is a safe approach for selected and motivated male patients [26, 53, 55]. However, many male breast cancers are centrally located and exhibit nipple involvement at presentation, thereby necessitating removal of the nipple-areolar complex, which may limit the potential cosmetic benefit of breast preservation. Similar to women, breast-conserving surgery for invasive breast cancer in men should be followed by adjuvant radiotherapy. The option for reconstruction after mastectomy with skin flap or skin and nipple-areolar preservation or later nipple reconstruction also exists, but there are no published data on the safety and efficacy of this approach for males with breast cancer.
While there are no data of the role of neoadjuvant chemotherapy in male breast cancer patients, this approach could be considered for patients where downsizing of the breast tumor is desired (e.g., patients with large tumors where achieving negative margins would be difficult, or when breast conserving surgery is desired), or for clinically node-positive patients, as neoadjuvant therapy may downstage the axilla and allow more limited axillary surgery with potentially less morbidity. This may be considered particularly for non-luminal or luminal B-like tumors, which are more likely to respond to cytotoxic chemotherapy. The role of neoadjuvant endocrine therapy is unknown in males, and not recommended.
4.2 Management of the axillary nodes
Recent reports suggest that SLN surgery is under-utilized in males, although it appears to be as safe and efficacious as for female breast cancer patients [24, 56, 57]. While approximately half of patients are node-negative at presentation [23, 26, 27, 58], only 18 to 25% of male breast cancer patients undergo SLN surgery alone or prior to axillary dissection [24, 52]. While SLN biopsy appears feasible in clinically node-negative men based on small case series [56, 57, 59,60,61,62,63,64], males with breast cancer have higher rates of both SLN and non-SLN positivity than females [55, 56, 65]. Further, the oncologic safety of omitting axillary lymph node dissection in men with low-volume axillary disease is unknown. Nomograms useful for predicting non-SLN positivity for female breast cancer do not perform as well for male breast cancer patients [52]. As such, the threshold for axillary lymph node dissection for SLN-positive disease might reasonably be lower in men than women. That said, in men with low-volume SLN metastases with indications for adjuvant radiotherapy, such as following breast-conserving surgery, axillary lymph node dissection may reasonably be omitted after multidisciplinary discussion [66,67,68].
4.3 Adjuvant radiation therapy
Data on adjuvant radiation therapy in men are also limited. Recently, a retrospective population analysis evaluated the impact of post-mastectomy radiotherapy (PMRT) after modified radical mastectomy in 1933 male breast cancer patients included in the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database. As expected, there was no significant difference in 5-year OS between those who received PMRT and those who did not due to differences in risk factors for those selected to receive PMRT. However, in a case-matched analysis, PMRT was associated with improved OS in the subset of patients with 1–3 positive nodes (5-year OS 79 vs 72%, p = 0.05) and those with 4+ positive nodes (5-year OS 73 vs 53%, p < 0.001) [69]. A small study of 31 male breast cancer patients found that relapses were infrequent (1 out of 31 patients) when PMRT criteria for women were applied to men [70]. In addition, in other small studies, receipt of adjuvant radiation therapy has been independently associated with longer DFS [71, 72]. Differences in OS were not demonstrated, perhaps due to low power for these analyses. These data are supportive of the efficacy of adjuvant PMRT for men with breast cancer and the practice that treatment recommendations should generally be based on evidence-based guidelines established for women with the disease [68, 73].
As in women, PMRT is recommended in men with four or more positive axillary lymph nodes and patients with involved internal mammary, infraclavicular, or supraclavicular nodes. In addition, tumors with direct extension to the chest wall or skin and inflammatory carcinoma are indications for PMRT. The decision to recommend PMRT for patients with one to three positive lymph nodes or for node-negative patients with tumors > 5 cm is more complex. These men should be strongly considered for PMRT, with other factors such as young age, high tumor grade, lymphovascular invasion, multiple involved nodes, extranodal extension, and positive surgical margins weighing more heavily in favor of radiation therapy administration [74, 75]. The management of clinically node-positive breast cancer treated with neoadjuvant chemotherapy which becomes pathologically node negative at surgery is an active area of investigation [76, 77]. Outside of clinical trials, treatment recommendations should be based on the most advanced of the clinical or pathologic stage [73, 74]. When PMRT is administered, 50 Gy in 25 fractions is routinely delivered to the chest wall and regional lymph nodes with consideration of a boost to the chest wall in some practices.
In men who undergo breast-conserving surgery, post-operative whole breast radiotherapy is the standard of care. A SEER analysis showed no significant difference in cause-specific survival in men with localized breast cancer treated with breast-conserving surgery plus adjuvant radiotherapy compared with mastectomy, supporting the oncologic safety of this approach in carefully selected patients [26]. Based on randomized controlled trials of “hypofractionated” radiotherapy after lumpectomy in women with breast cancer, whole breast radiotherapy should be administered to men in 40–42.5 Gy in 15–16 fractions with an optional boost to the lumpectomy cavity, depending on pathologic risk factors [78,79,80].
Omission of adjuvant radiation therapy in older women with a biologically favorable breast cancer (node-negative, ER-positive, tumor size ≤ 2 cm) treated with lumpectomy and endocrine therapy, does not impact OS [81, 82]. This approach has not been studied in men but is an appropriate consideration in comparable age (70 years and older) male patients. Accelerated partial breast irradiation has emerged as a standard treatment option in women with favorable early-stage breast cancer [83,84,85]. This modality is unlikely to provide as much breast sparing in men due to the smaller breast size, but may still reduce the dose to the heart and lungs compared with whole breast irradiation, and should be investigated in future studies. Indeed, long-term follow-up of women treated with older techniques has resulted in a greater appreciation for the importance of minimizing exposure to the heart and lungs [86, 87]. These studies highlight the necessity of careful attention to normal tissue constraints during treatment planning. Furthermore, they suggest that emerging technological advances that reduce normal tissue exposure such as deep-inspiration breath hold and proton therapy may further enhance the therapeutic ratio in men and women with breast cancer [88,89,90].
4.4 Systemic therapy for early-stage disease
4.4.1 Endocrine therapy
Given that the vast majority of male breast cancers are hormone receptor-positive, endocrine therapy is the mainstay of systemic treatment. Several retrospective (non-randomized) studies indicated that adjuvant endocrine therapy (tamoxifen being the most commonly used) may improve RFS and OS in male breast cancer patients, particularly for node-positive disease [58, 91,92,93,94,95]. Therefore, tamoxifen is the recommended standard adjuvant endocrine therapy in men (unless contraindicated) [3]. It is unknown if extended tamoxifen provides benefit in male patients as it does in select female patients [96, 97], but this longer course is reasonable for patients who are at high risk of recurrence.
Other hormonal therapies that are sometimes used in the adjuvant treatment of male breast cancer patients include gonadotropin-releasing hormone analogs (GNRHa), orchiectomy, estrogens, and progestins. While aromatase inhibitors have documented efficacy in postmenopausal women (and in premenopausal women undergoing concomitant ovarian function suppression), and have been used occasionally in men, there are sex differences in the endocrine environment that raise concerns about aromatase inhibitors stimulating androgen production in men (see “Endocrine therapy” under the “Treatment for advanced disease” section). Therefore, some recommend concurrent GNRHa whenever an aromatase inhibitor is used in males.
The toxicity of endocrine therapy is understudied in men, but small studies suggest that hot flashes and sexual dysfunction are common in men on tamoxifen, and as many as one in four men prematurely discontinue adjuvant endocrine therapy due to side effects [98,99,100,101].
4.4.2 Chemotherapy
Most adjuvant chemotherapy trials in breast cancer have excluded male patients. Adjuvant chemotherapy should be considered for men with intermediate or high-risk early-stage disease, particularly those with hormone receptor-negative disease, large tumors, nodal involvement, and/or younger age at diagnosis [3]. There are no studies specifically evaluating neoadjuvant therapy in men. If chemotherapy is indicated, a neoadjuvant approach may be considered, particularly for patients with larger tumors that would be otherwise be challenging to resect, and for patients with axillary nodal involvement, as neoadjuvant chemotherapy may lead to axillary downstaging, and offer the opportunity for a more limited axillary surgery.
Although most data come from small and non-randomized clinical studies, it appears that adjuvant chemotherapy decreases the risk of recurrence and mortality in male breast cancer [58, 91, 102,103,104,105]. In a study of 135 men with breast cancer [91], 62% received adjuvant chemotherapy (either alone or with endocrine therapy), which was associated with a trend towards lower mortality (HR: 0.78; 95% CI, 0.39–1.55) for node-positive patients. An older, small, prospective study assessed the use of adjuvant cyclophosphamide, methotrexate, and 5-fluorouracil (CMF), in 24 men with node-positive breast cancer [102]. In this cohort, although 71% had ER-positive disease, only 13% received adjuvant tamoxifen. The 5-year OS rate of 80% was higher than historical controls. A subsequent analysis with longer follow-up reported a 10-year OS of 64.5%, higher than that of male patients with node-positive breast cancer included in the SEER database (42.5%) [103]. While these findings suggest a benefit of adjuvant chemotherapy, higher OS rates after chemotherapy may be attributable to selection bias (because otherwise healthy men are more likely to have enrolled on a chemotherapy trial).
4.4.3 Use of gene expression profiles for risk-stratification
Genomic risk-stratification (such as Oncotype DX or Mammaprint) is routinely used in women with hormone receptor-positive breast cancer to assist clinicians with estimating the likelihood of recurrence and as a tool to identify those who may benefit from adjuvant. The utility of these tools in men is understudied.
A study presented in 2009 reported the findings of Oncotype DX analysis in 347 male breast cancer patients [106]. While there was a wide variation in gene expression, the distribution of risk categories was similar to that seen in women [low-risk (recurrence score < 18%) 54%, intermediate-risk (18–30) 35%, and high-risk (≥ 31) 11%)]. However, the mean expression of proliferation genes was higher in males. Similarly, other studies have found comparable distributions of low-, intermediate-, and high-risk recurrence scores between men and women [107, 108]. In a National Cancer Database study focusing on patients with node-positive disease, Oncotype Dx testing for patients with 1–3 positive lymph nodes was used less frequently in men (13.6%) than in women (20.6%, p < 0.001). Men with Oncotype Dx testing were less likely to be recommended to have adjuvant chemotherapy than those without testing (47.1 vs 75.5%, p < 0.001) [108]. Outcome data for male breast cancer are needed to ensure that it is appropriate to use Oncotype DX results to guide treatment decision-making. In the absence of data, it is reasonable to use these tools in practice, recognizing the limitations of such an approach in men.
4.4.4 HER2-directed therapies
The efficacy of adjuvant HER2-directed therapies is uncertain in men. However, given the substantial benefit seen with adjuvant HER2-directed therapy in women [109,110,111,112], and the absence of a biological rationale for differences in response by sex, the current recommendation is to use the same approach to treatment for HER2-positive breast cancer in women.
5 Treatment for advanced disease
A greater proportion of men with breast cancer have metastatic disease at the time of diagnosis compared to women [23]. Given that most men with breast cancer have ER-positive disease, chemotherapy is generally reserved for endocrine-resistant disease or bulky disease compromising vital organ function, where a rapid response is perceived to be necessary. Similar to the approach in women, when chemotherapy is used, sequential, single-agent regimens are usually preferred over combination regimens. In women, this strategy has been shown to result in similar survival outcomes with less toxicity [113].
5.1 Endocrine therapy
Historically, bilateral orchiectomy yielded objective responses ranging from 31 to 67% that lasted on average between 17 and 30 months [114,115,116,117]. Other endocrine ablative strategies such as adrenalectomy and hypophysectomy were also used as second-line therapy, with suggestions of improved outcomes. These treatments resulted in significant toxicity, and were largely abandoned once androgens, anti-androgens, corticosteroids, and, ultimately, tamoxifen became available.
Tamoxifen is the most extensively studied endocrine therapy in male patients with breast cancer and is the preferred initial treatment [118,119,120]. Similar to female breast cancer, ER positivity predicts benefit from tamoxifen [120]. Although there are no prospective randomized data evaluating tamoxifen in metastatic male breast cancer, biological insights support its use as first-line therapy. It appears that tamoxifen is less well-tolerated in males compared to females [121]; however, it is much better tolerated than other historical forms of treatment such as orchiectomy and adrenalectomy.
The role of aromatase inhibitors in male breast cancer is unclear, with data only available from case reports and case series [122,123,124,125,126]. In a study of 15 men with metastatic breast cancer treated with aromatase inhibitors, 53% had an objective response or stable disease [125]. Differences in estrogen production physiology between men and women raise concerns about efficacy of aromatase inhibitor monotherapy in male breast cancer [127,128,129]. A significant proportion of male estrogen is generated by the peripheral conversion of circulating androgens via the aromatase enzyme. In addition, approximately 20% of circulating estrogen in men is directly secreted by the testicles. There is evidence that the activity of the aromatase enzyme in men increases with age, and that estradiol levels are higher in older men compared to postmenopausal women. While aromatase inhibitors suppress the main source of estrogen in men (peripheral conversion), they do not affect the testicular production of estrogen. Furthermore, a feedback loop leading to increased levels of follicle-stimulating hormone, luteinizing hormone, and testosterone could theoretically provide additional substrate for peripheral conversion by the aromatase enzyme. For this reason, if aromatase inhibitors are being considered for the treatment of men with tamoxifen-resistant breast cancer, it may be wise to combine them with surgical or medical orchiectomy (using a GNRHa).
The role of fulvestrant in male breast cancer also remains unclear with low-level evidence suggesting activity. In a pooled analysis examining the efficacy of fulvestrant in 23 patients with male breast cancer [130], fulvestrant was given as first- or second-line therapy in 40% of patients, and as third line or beyond in 60%. Nearly 80% had visceral metastasis. A partial response was achieved in 26%, while 48% had stable disease (clinical benefit rate 74%). The median PFS was 5 months.
5.2 CDK4/6 inhibitors
The use of the CDK4/6 inhibitors palbociclib, ribociclib, and abemaciclib along with endocrine therapy has been established as the preferred first-line regimen for female metastatic breast cancer. Trials evaluating these agents have shown a doubling in progression-free survival compared to endocrine therapy alone [131,132,133,134,135]. In addition, abemaciclib is also FDA approved as monotherapy after progression on endocrine therapy and chemotherapy [136]. However, no male patients have been included in these trials. The only data available in men is from a single case report; a male patient with metastatic ER-positive, HER2-negative breast cancer received letrozole plus palbociclib as a fourth line of therapy and exhibited stable disease at 4 months on treatment [137]. The patient previously received paclitaxel, liposomal doxorubicin, and fulvestrant in the metastatic setting, and tamoxifen (5 years), followed by letrozole (2.5 years) in the adjuvant setting. Additional details, such as concomitant use of GNRHa were not included in the report.
5.3 mTOR inhibitors
mTOR inhibitors have been shown in clinical trials to reverse endocrine resistance in female breast cancer [138, 139]. There are two case reports of heavily pretreated male patients with metastatic breast cancer who had a favorable response to therapy, although one of the patients had to stop treatment after 4 months due to the development of stomatitis [140, 141].
5.4 Chemotherapy
In the metastatic setting, cytotoxic chemotherapy is often reserved for the endocrine-resistant or ER-negative settings, or for when there is impending visceral crisis and a rapid response to therapy is needed. There are no data demonstrating superiority of one agent over another, and as such, recommendations mirror those for female breast cancer. In a retrospective, multicenter case series including 23 heavily pretreated metastatic male breast cancer patients, treatment with eribulin was associated with a clinical response in 48% of patients. Eribulin was overall well tolerated and administered for a median of 6 cycles (range, 3–15) [142]. Single-agent activity has also been described with 5-fluorouracil, cyclophosphamide, methotrexate, and older drugs such as melphalan, chlorambucil, and thiotepa [143].
5.5 HER2-directed therapies
HER2 amplification is rare in male breast cancer, and the use of HER2-blockade in men with metastatic disease is limited to case reports [144,145,146]. Similar to the adjuvant setting, HER2-directed therapies in men with metastatic breast cancer are used in the same fashion as for women. This approach is based on the substantial benefit seen in women with HER2-positive metastatic disease, and no biological rationale for differences in response by sex.
5.6 Targeting the androgen receptor
Targeting the androgen receptor (AR) axis in male breast cancer has been an area of interest since the 1940s, when a case series demonstrated that bilateral orchiectomy was effective for treating skeletal metastases [147]. In the study by Cardoso et al., AR was highly positive in 87% of male breast cancer specimens, which is consistent with previous studies [148]. In a gene expression profiling study comparing male and female breast cancer, 1000 differentially expressed genes were identified, including a significantly higher number of AR-related genes, suggesting AR activation [33]. In the untreated male breast cancer population, androgens have been theorized to directly exert a tumorigenic effect by stimulating growth of AR-expressing breast cancer cells [149]. With anti-hormonal therapy, particularly aromatase inhibitors, androgen levels increase, potentially acting as a mechanism of resistance to anti-estrogen therapy. In 1993, Lopez et al. presented 11 cases of men with metastatic breast cancer treated with cyproterone acetate (an anti-androgen) combined with buserelin (GNRHa). In this series, seven men (64%) had an objective response to treatment [150]. The same group released additional data in 2014 that demonstrated an overall response rate of 53% in 36 men with metastatic breast cancer treated with cyproterone acetate ± GnRHa [151]. However, it is uncertain if the anti-androgen contributed efficacy beyond what would have been seen with a GnRH analog alone.
The precise actions of the AR in breast tissue are complex with multiple feedback loops. AR activation may be dependent on the hormonal milieu (i.e., relative tissue concentrations of androgens vs estrogens), presence or absence of co-expression of the ER, and on other concurrent active signaling pathways. Concordant (ER+/AR+ or ER−/AR−) or discordant (ER+/AR− or ER−/AR+) AR and ER expression may have differential effects on cell proliferation and on patient outcomes. In ER+/AR+ cell lines, activation of the AR has been reported to lead to apoptosis [152], whereas in ER−/AR+ cell lines, AR appears to induce proliferation [153]. Consistent with this, it has been reported that patients with discordant ER and AR expression appear to have a worse prognosis than those with concordant ER and AR expression [154]. Interestingly, after treatment with adjuvant tamoxifen, a higher ratio of AR to ER expression by IHC appears to be associated with shorter DFS, suggesting that AR expression may contribute to endocrine therapy resistance in ER+ tumors [155]. In a retrospective analysis of 43 men with breast cancer, AR expression was associated with a shorter median OS (37 months for AR+ vs 58 months AR−) [156].
While these studies suggest that AR targeting is a promising and logical treatment option for male breast cancer, these studies are small, often single center, and retrospective. Most extended across broad timespans and utilized multiple therapies, further limiting interpretation of the results. Even among the largest retrospective pooled analysis of AR systemic therapy (60 patients), no definitive conclusions have been drawn [157]. Newer, more potent anti-androgens, such as enzalutamide, have not been studied in male breast cancer, and randomized data comparing anti-androgens to other standard therapies are lacking. With more proficient androgen deprivation, the clinical benefit rate may improve, as is seen in prostate cancer. Several ongoing clinical studies (including both men and women) evaluating single-agent or combination anti-androgen therapy strategies are highlighted in Table 2.
5.7 PARP inhibitors
Agents that inhibit the poly(adenosine diphosphate-ribose) polymerase (PARP) enzyme have recently shown significant clinical activity in germline BRCA-associated breast [158, 159], ovarian [160,161,162] and prostate cancer [163], and are being evaluated for BRCA-associated pancreatic cancer. Two oral PARP inhibitors (olaparib and talazoparib) have been studied in phase 3 clinical trials among patients with germline BRCA mutations and HER2-negative metastatic breast cancer [158, 159]. In this setting, treatment with olaparib or talazoparib led to a significant improvement in the median PFS when compared with treatment of physician’s choice (TPC, which included various single-agent cytotoxic drugs, but no platinums). Both agents led to virtually identical improvements in overall response rates (TPC 29% vs olaparib 60%; TPC 22% vs talazoparib 63%) and PFS [TPC 4.2 months vs olaparib 7.0 months (HR 0.58, p < 0.001); TPC 5.6 months vs talazoparib 8.6 months (HR 0.54, p < 0.0001)]. Toxicity profiles and quality of life measures also favored the PARP inhibitors over TPC. In the phase 3 olaparib trial, seven men were enrolled, with five assigned to receive olaparib, and two assigned to TPC. Data on responses on these patients has not been reported.
Olaparib is currently approved by the FDA for use in patients with metastatic HER2-negative breast cancer and deleterious germline BRCA mutations. PARP inhibitors are also being explored in the setting of other DNA-damaging repair germline and/or somatic genetic alterations. Given the relative frequency of genetic predisposition gene mutations in men with breast cancer, there may be an expanding role for PARP inhibitors in these patients.
6 Survivorship
6.1 Endocrine therapy toxicities
Approaches to mitigate endocrine therapy side effects, such as vasomotor symptoms, currently mirror those taken in women. No specific treatment guidelines for men with breast cancer exist because no symptom intervention study has yet focused on the male breast cancer population. Similarly, treatment of sexual dysfunction is based on general guidelines for treating male sexual dysfunction secondary to low androgen states (minus hormone supplementation), without specific interventions having been developed for male breast cancer survivors. Given that men have high rates of premature endocrine therapy discontinuation, close monitoring and treatment of these symptoms is an essential part of survivorship care [164].
6.2 Fertility preservation
Chemotherapy can impair male fertility. In addition, preclinical data suggest that CDK4/6 inhibitor may lead to sperm damage (palbociclib FDA label). Men who desire future fertility should be counseled at the time of diagnosis about this risk and on considering sperm cryopreservation, particularly if they are being considered for chemotherapy [165].
6.3 Follow-up and surveillance
Because male breast cancer is rare, it is unclear whether survivors benefit from contralateral screening with breast imaging after mastectomy. While males with prior breast cancer have a 30-fold higher relative risk of a contralateral primary compared to the general population, the absolute risk remains small (0.1%/year) [166, 167]. Screening mammography might be most beneficial for male breast cancer survivors who have additional risk factors, such as BRCA mutations [168, 169]. Otherwise, breast self-examination and clinical examination are recommended.
6.4 Emotional support
Men who are diagnosed with breast cancer may feel stigmatized and isolated because this disease is much more common in women. Raising awareness of male breast cancer and connecting male breast cancer patients with others who have had similar experiences may be helpful. Support groups for male patients specifically are rare [170], and research is needed to assess how novel tools for virtual connectedness can be used to support men during and after treatment for breast cancer.
7 Conclusions
Male breast cancer is an uncommon disease that has been understudied. Although many characteristics are shared with female breast cancer, there are several important biologic differences to consider when extrapolating from the abundant female breast cancer literature for clinical decision-making. Preclinical studies focused on improving our understanding of the unique biology of male breast cancer are also needed. Establishment of male breast cancer cell lines, mouse models, and patient-derived xenograft models may facilitate this. There is a critical need for data on the activity and safety of novel agents such as CDK 4/6 inhibitors, mTOR inhibitors, PARP inhibitors, and other targeted therapies in men, and also for data on the efficacy of well-established treatments such as aromatase inhibitors and fulvestrant. Clinical investigators should be encouraged to allow the enrollment of male breast cancer patients in modern clinical trials, absent a strong biological rationale to justify their exclusion.
References
Siegel, R. L., Miller, K. D., & Jemal, A. (2017). Cancer statistics, 2017. CA: a Cancer Journal for Clinicians, 67(1), 7–30. https://doi.org/10.3322/caac.21387.
Howlader, N., Noone, A., Krapcho, M., Miller, D., Bishop, K., Kosary, C., et al. (2017). SEER Cancer statistics review, 1975-2014, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site. Accessed 8/7/2017 2017.
Korde, L. A., Zujewski, J. A., Kamin, L., Giordano, S., Domchek, S., Anderson, W. F., et al. (2010). Multidisciplinary meeting on male breast cancer: summary and research recommendations. Journal of Clinical Oncology, 28(12), 2114–2122. https://doi.org/10.1200/JCO.2009.25.5729.
Anderson, W. F., Althuis, M. D., Brinton, L. A., & Devesa, S. S. (2004). Is male breast cancer similar or different than female breast cancer? Breast Cancer Research and Treatment, 83(1), 77–86. https://doi.org/10.1023/B:BREA.0000010701.08825.2d.
Couch, F. J., Farid, L. M., DeShano, M. L., Tavtigian, S. V., Calzone, K., Campeau, L., et al. (1996). BRCA2 germline mutations in male breast cancer cases and breast cancer families. Nature Genetics, 13(1), 123–125. https://doi.org/10.1038/ng0596-123.
Syrjakoski, K., Kuukasjarvi, T., Waltering, K., Haraldsson, K., Auvinen, A., Borg, A., et al. (2004). BRCA2 mutations in 154 finnish male breast cancer patients. Neoplasia, 6(5), 541–545. https://doi.org/10.1593/neo.04193.
Haraldsson, K., Loman, N., Zhang, Q. X., Johannsson, O., Olsson, H., & Borg, A. (1998). BRCA2 germ-line mutations are frequent in male breast cancer patients without a family history of the disease. Cancer Research, 58(7), 1367–1371.
Thorlacius, S., Tryggvadottir, L., Olafsdottir, G. H., Jonasson, J. G., Ogmundsdottir, H. M., Tulinius, H., et al. (1995). Linkage to BRCA2 region in hereditary male breast cancer. Lancet, 346(8974), 544–545.
Wooster, R., Bignell, G., Lancaster, J., Swift, S., Seal, S., Mangion, J., et al. (1995). Identification of the breast cancer susceptibility gene BRCA2. Nature, 378(6559), 789–792. https://doi.org/10.1038/378789a0.
Gargiulo, P., Pensabene, M., Milano, M., Arpino, G., Giuliano, M., Forestieri, V., et al. (2016). Long-term survival and BRCA status in male breast cancer: a retrospective single-center analysis. BMC Cancer, 16(1), 375.
Pritzlaff, M., Summerour, P., McFarland, R., Li, S., Reineke, P., Dolinsky, J. S., et al. (2017). Male breast cancer in a multi-gene panel testing cohort: insights and unexpected results. Breast Cancer Research and Treatment, 161(3), 575–586.
Breast Cancer Linkage, C. (1999). Cancer risks in BRCA2 mutation carriers. Journal of the National Cancer Institute, 91(15), 1310–1316.
Tai, Y. C., Domchek, S., Parmigiani, G., & Chen, S. (2007). Breast cancer risk among male BRCA1 and BRCA2 mutation carriers. Journal of the National Cancer Institute, 99(23), 1811–1814. https://doi.org/10.1093/jnci/djm203.
Brose, M. S., Rebbeck, T. R., Calzone, K. A., Stopfer, J. E., Nathanson, K. L., & Weber, B. L. (2002). Cancer risk estimates for BRCA1 mutation carriers identified in a risk evaluation program. Journal of the National Cancer Institute, 94(18), 1365–1372.
Chodick, G., Struewing, J. P., Ron, E., Rutter, J. L., & Iscovich, J. (2008). Similar prevalence of founder BRCA1 and BRCA2 mutations among Ashkenazi and non-Ashkenazi men with breast cancer: evidence from 261 cases in Israel, 1976-1999. European Journal of Medical Genetics, 51(2), 141–147. https://doi.org/10.1016/j.ejmg.2007.11.001.
Fackenthal, J. D., Marsh, D. J., Richardson, A. L., Cummings, S. A., Eng, C., Robinson, B. G., et al. (2001). Male breast cancer in Cowden syndrome patients with germline PTEN mutations. Journal of Medical Genetics, 38(3), 159–164.
Anelli, A., Anelli, T. F., Youngson, B., Rosen, P. P., & Borgen, P. I. (1995). Mutations of the p53 gene in male breast cancer. Cancer, 75(9), 2233–2238.
Meijers-Heijboer, H., van den Ouweland, A., Klijn, J., Wasielewski, M., de Snoo, A., Oldenburg, R., et al. (2002). Low-penetrance susceptibility to breast cancer due to CHEK2(*)1100delC in noncarriers of BRCA1 or BRCA2 mutations. Nature Genetics, 31(1), 55–59. https://doi.org/10.1038/ng879.
Evans, D. B., & Crichlow, R. W. (1987). Carcinoma of the male breast and Klinefelter’s syndrome: is there an association? CA: a Cancer Journal for Clinicians, 37(4), 246–251.
Hultborn, R., Hanson, C., Kopf, I., Verbiene, I., Warnhammar, E., & Weimarck, A. (1997). Prevalence of Klinefelter’s syndrome in male breast cancer patients. Anticancer Research, 17(6D), 4293–4297.
Network, N. C. C. Genetic/familial high-risk assessment: Breast and ovarian (Version 1.2018). genetic/familial high-risk assessment 1.2018. Accessed November 10, 2017.
Llort, G., Chirivella, I., Morales, R., Serrano, R., Sanchez, A. B., Teulé, A., et al. (2015). SEOM clinical guidelines in hereditary breast and ovarian cancer. Clinical and Translational Oncology, 17(12), 956–961.
Vermeulen, M. A., Slaets, L., Cardoso, F., Giordano, S. H., Tryfonidis, K., van Diest, P. J., et al. (2017). Pathological characterisation of male breast cancer: results of the EORTC 10085/TBCRC/BIG/NABCG international male breast Cancer program. European Journal of Cancer, 82, 219–227. https://doi.org/10.1016/j.ejca.2017.01.034.
Cardoso, F., Bartlett, J. M. S., Slaets, L., van Deurzen, C. H. M., van Leeuwen-Stok, E., Porter, P., et al. (2017). Characterization of male breast cancer: results of the EORTC 10085/TBCRC/BIG/NABCG international male breast cancer program. Annals of oncology, mdx651-mdx651, doi:https://doi.org/10.1093/annonc/mdx651.
Culell, P., Solernou, L., Tarazona, J., Roma, J., Martí, E., Miguel, A., et al. (2007). Male breast cancer: a multicentric study. The Breast Journal, 13(2), 213–215.
Fields, E. C., DeWitt, P., Fisher, C. M., & Rabinovitch, R. (2013). Management of male breast cancer in the United States: a surveillance, epidemiology and end results analysis. International Journal of Radiation Oncology* Biology* Physics, 87(4), 747–752.
Giordano, S. H., Cohen, D. S., Buzdar, A. U., Perkins, G., & Hortobagyi, G. N. (2004). Breast carcinoma in men: a population-based study. Cancer, 101(1), 51–57. https://doi.org/10.1002/cncr.20312.
Shaaban, A. M., Ball, G. R., Brannan, R. A., Cserni, G., Di Benedetto, A., Dent, J., et al. (2012). A comparative biomarker study of 514 matched cases of male and female breast cancer reveals gender-specific biological differences. Breast Cancer Research and Treatment, 133(3), 949–958. https://doi.org/10.1007/s10549-011-1856-9.
Burga, A. M., Fadare, O., Lininger, R. A., & Tavassoli, F. A. (2006). Invasive carcinomas of the male breast: a morphologic study of the distribution of histologic subtypes and metastatic patterns in 778 cases. Virchows Archiv, 449(5), 507–512. https://doi.org/10.1007/s00428-006-0305-3.
Weigelt, B., Geyer, F. C., & Reis-Filho, J. S. (2010). Histological types of breast cancer: how special are they? Molecular Oncology, 4(3), 192–208. https://doi.org/10.1016/j.molonc.2010.04.004.
Rakha, E. A., Reis-Filho, J. S., Baehner, F., Dabbs, D. J., Decker, T., Eusebi, V., et al. (2010). Breast cancer prognostic classification in the molecular era: the role of histological grade. Breast Cancer Research, 12(4), 207. https://doi.org/10.1186/bcr2607.
Network, C. G. A. (2012). Comprehensive molecular portraits of human breast tumours. Nature, 490(7418), 61–70.
Callari, M., Cappelletti, V., De Cecco, L., Musella, V., Miodini, P., Veneroni, S., et al. (2011). Gene expression analysis reveals a different transcriptomic landscape in female and male breast cancer. Breast Cancer Research and Treatment, 127(3), 601–610.
Johansson, I., Nilsson, C., Berglund, P., Lauss, M., Ringnér, M., Olsson, H., et al. (2012). Gene expression profiling of primary male breast cancers reveals two unique subgroups and identifies N-acetyltransferase-1 (NAT1) as a novel prognostic biomarker. Breast Cancer Research, 14(1), R31.
Piscuoglio, S., Ng, C. K., Murray, M. P., Guerini-Rocco, E., Martelotto, L. G., Geyer, F. C., et al. (2016). The genomic landscape of male breast cancers. Clinical Cancer Research, 22(16), 4045–4056.
Denkert, C., von Minckwitz, G., Darb-Esfahani, S., Ingold Heppner, B., Klauschen, F., Furlanetto, J., et al. (2017). Abstract S1-09: Evaluation of tumor-infiltrating lymphocytes (TILs) as predictive and prognostic biomarker in different subtypes of breast cancer treated with neoadjuvant therapy - a metaanalysis of 3771 patients. Cancer research, 77(4 Supplement), S1-09-S01-09, doi:https://doi.org/10.1158/1538-7445.sabcs16-s1-09.
Denkert, C., Loibl, S., Noske, A., Roller, M., Muller, B. M., Komor, M., et al. (2010). Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. Journal of Clinical Oncology, 28(1), 105–113. https://doi.org/10.1200/JCO.2009.23.7370.
Yamaguchi, R., Tanaka, M., Yano, A., Tse, G. M., Yamaguchi, M., Koura, K., et al. (2012). Tumor-infiltrating lymphocytes are important pathologic predictors for neoadjuvant chemotherapy in patients with breast cancer. Human Pathology, 43(10), 1688–1694. https://doi.org/10.1016/j.humpath.2011.12.013.
West, N. R., Milne, K., Truong, P. T., Macpherson, N., Nelson, B. H., & Watson, P. H. (2011). Tumor-infiltrating lymphocytes predict response to anthracycline-based chemotherapy in estrogen receptor-negative breast cancer. Breast Cancer Research, 13(6), R126. https://doi.org/10.1186/bcr3072.
Ono, M., Tsuda, H., Shimizu, C., Yamamoto, S., Shibata, T., Yamamoto, H., et al. (2012). Tumor-infiltrating lymphocytes are correlated with response to neoadjuvant chemotherapy in triple-negative breast cancer. Breast Cancer Research and Treatment, 132(3), 793–805. https://doi.org/10.1007/s10549-011-1554-7.
Loi, S., Sirtaine, N., Piette, F., Salgado, R., Viale, G., Van Eenoo, F., et al. (2013). Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 31(7), 860–867. https://doi.org/10.1200/JCO.2011.41.0902.
Loi, S., Michiels, S., Salgado, R., Sirtaine, N., Jose, V., Fumagalli, D., et al. (2014). Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Annals of Oncology, 25(8), 1544–1550. https://doi.org/10.1093/annonc/mdu112.
Adams, S., Gray, R. J., Demaria, S., Goldstein, L., Perez, E. A., Shulman, L. N., et al. (2014). Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. Journal of Clinical Oncology, 32(27), 2959–2966. https://doi.org/10.1200/JCO.2013.55.0491.
Pruneri, G., Vingiani, A., Bagnardi, V., Rotmensz, N., De Rose, A., Palazzo, A., et al. (2016). Clinical validity of tumor-infiltrating lymphocytes analysis in patients with triple-negative breast cancer. Annals of Oncology : Official Journal of the European Society for Medical Oncology / ESMO, 27(2), 249–256. https://doi.org/10.1093/annonc/mdv571.
Montagna, E., Vingiani, A., Maisonneuve, P., Cancello, G., Contaldo, F., Pruneri, G., et al. (2017). Unfavorable prognostic role of tumor-infiltrating lymphocytes in hormone-receptor positive, HER2 negative metastatic breast cancer treated with metronomic chemotherapy. Breast, 34, 83–88. https://doi.org/10.1016/j.breast.2017.05.009.
Lee, A. H., Gillett, C. E., Ryder, K., Fentiman, I. S., Miles, D. W., & Millis, R. R. (2006). Different patterns of inflammation and prognosis in invasive carcinoma of the breast. Histopathology, 48(6), 692–701. https://doi.org/10.1111/j.1365-2559.2006.02410.x.
Salgado, R., Denkert, C., Demaria, S., Sirtaine, N., Klauschen, F., Pruneri, G., et al. (2015). The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Annals of Oncology : Official Journal of the European Society for Medical Oncology / ESMO, 26(2), 259–271. https://doi.org/10.1093/annonc/mdu450.
Zhou, F. F., Xia, L. P., Guo, G. F., Wang, X., Yuan, Z. Y., Zhang, B., et al. (2010). Changes in therapeutic strategies in Chinese male patients with breast cancer: 40 years of experience in a single institute. Breast, 19(6), 450–455. https://doi.org/10.1016/j.breast.2010.04.007.
Schaub, N. P., Maloney, N., Schneider, H., Feliberti, E., & Perry, R. (2008). Changes in male breast cancer over a 30-year period. The American Surgeon, 74(8), 707–711 discussion 711-702.
Scott-Conner, C. E., Jochimsen, P. R., Menck, H. R., & Winchester, D. J. (1999). An analysis of male and female breast cancer treatment and survival among demographically identical pairs of patients. Surgery, 126(4), 775–780 discussion 780-771.
Sousa, B., Moser, E., & Cardoso, F. (2013). An update on male breast cancer and future directions for research and treatment. European Journal of Pharmacology, 717(1–3), 71–83. https://doi.org/10.1016/j.ejphar.2013.03.037.
Vaysse, C., Sroussi, J., Mallon, P., Feron, J., Rivain, A., Ngo, C., et al. (2012). Prediction of axillary lymph node status in male breast carcinoma. Annals of Oncology, 24(2), 370–376.
Leone, J. P., Leone, J., Zwenger, A. O., Iturbe, J., Vallejo, C. T., & Leone, B. A. (2015). Prognostic significance of tumor subtypes in male breast cancer: a population-based study. Breast Cancer Research and Treatment, 152(3), 601–609.
Gargiulo, P., Pensabene, M., Milano, M., Arpino, G., Giuliano, M., Forestieri, V., et al. (2016). Long-term survival and BRCA status in male breast cancer: a retrospective single-center analysis. BMC Cancer, 16, 375–375.
Golshan, M., Rusby, J., Dominguez, F., & Smith, B. L. (2007). Breast conservation for male breast carcinoma. The Breast, 16(6), 653–656.
Boughey, J. C., Bedrosian, I., Meric-Bernstam, F., Ross, M. I., Kuerer, H. M., Akins, J. S., et al. (2006). Comparative analysis of sentinel lymph node operation in male and female breast cancer patients. Journal of the American College of Surgeons, 203(4), 475–480. https://doi.org/10.1016/j.jamcollsurg.2006.06.014.
Cimmino, V. M., Degnim, A. C., Sabel, M. S., Diehl, K. M., Newman, L. A., & Chang, A. E. (2004). Efficacy of sentinel lymph node biopsy in male breast cancer. Journal of Surgical Oncology, 86(2), 74–77. https://doi.org/10.1002/jso.20045.
Cutuli, B., Le-Nir, C. C., Serin, D., Kirova, Y., Gaci, Z., Lemanski, C., et al. (2010). Male breast cancer. Evolution of treatment and prognostic factors. Analysis of 489 cases. Critical Reviews in Oncology/Hematology, 73(3), 246–254. https://doi.org/10.1016/j.critrevonc.2009.04.002.
Gentilini, O., Chagas, E., Zurrida, S., Intra, M., De Cicco, C., Gatti, G., et al. (2007). Sentinel lymph node biopsy in male patients with early breast cancer. Oncologist, 12(5), 512–515. https://doi.org/10.1634/theoncologist.12-5-512.
Flynn, L. W., Park, J., Patil, S. M., Cody 3rd, H. S., & Port, E. R. (2008). Sentinel lymph node biopsy is successful and accurate in male breast carcinoma. Journal of the American College of Surgeons, 206(4), 616–621. https://doi.org/10.1016/j.jamcollsurg.2007.11.005.
Albo, D., Ames, F. C., Hunt, K. K., Ross, M. I., Singletary, S. E., & Kuerer, H. M. (2003). Evaluation of lymph node status in male breast cancer patients: a role for sentinel lymph node biopsy. Breast Cancer Research and Treatment, 77(1), 9–14.
Goyal, A., Horgan, K., Kissin, M., Yiangou, C., Sibbering, M., Lansdown, M., et al. (2004). Sentinel lymph node biopsy in male breast cancer patients. European Journal of Surgical Oncology, 30(5), 480–483. https://doi.org/10.1016/j.ejso.2004.02.006.
Port, E. R., Fey, J. V., Cody 3rd, H. S., & Borgen, P. I. (2001). Sentinel lymph node biopsy in patients with male breast carcinoma. Cancer, 91(2), 319–323.
De Cicco, C., Baio, S. M., Veronesi, P., Trifiro, G., Ciprian, A., Vento, A., et al. (2004). Sentinel node biopsy in male breast cancer. Nuclear Medicine Communications, 25(2), 139–143.
Rusby, J. E., Smith, B. L., Dominguez, F. J., & Golshan, M. (2006). Sentinel lymph node biopsy in men with breast cancer: a report of 31 consecutive procedures and review of the literature. Clinical Breast Cancer, 7(5), 406–410.
Giuliano, A. E., Ballman, K. V., McCall, L., Beitsch, P. D., Brennan, M. B., Kelemen, P. R., et al. (2017). Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. Jama, 318(10), 918–926.
Donker, M., van Tienhoven, G., Straver, M. E., Meijnen, P., van de Velde, C. J., Mansel, R. E., et al. (2014). Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. The Lancet Oncology, 15(12), 1303–1310.
Bratman, S. V., Kapp, D. S., & Horst, K. C. (2012). Evolving trends in the initial locoregional management of male breast cancer. The Breast, 21(3), 296–302.
Abrams, M. J., Koffer, P. P., Wazer, D. E., & Hepel, J. T. (2017). Postmastectomy radiation therapy is associated with improved survival in node-positive male breast cancer: a population analysis. International Journal of Radiation Oncology* Biology* Physics, 98(2), 384–391.
Stranzl, H., Mayer, R., Quehenberger, F., Prettenhofer, U., Willfurth, P., Stoger, H., et al. (1999). Adjuvant radiotherapy in male breast cancer. Radiotherapy and Oncology, 53(1), 29–35.
Atalay, C., Kanlioz, M., & Altinok, M. (2003). Prognostic factors affecting survival in male breast cancer. Journal of Experimental & Clinical Cancer Research, 22(1), 29–33.
Yu, E., Suzuki, H., Younus, J., Elfiki, T., Stitt, L., Yau, G., et al. (2012). The impact of post-mastectomy radiation therapy on male breast cancer patients--a case series. International Journal of Radiation Oncology, Biology, Physics, 82(2), 696–700. https://doi.org/10.1016/j.ijrobp.2011.01.010.
Gradishar, W. J., Anderson, B. O., Balassanian, R., Blair, S. L., Burstein, H. J., Cyr, A., et al. (2017). NCCN guidelines insights: breast cancer, version 1.2017. Journal of the National Comprehensive Cancer Network, 15(4), 433–451.
Recht, A., Comen, E. A., Fine, R. E., Fleming, G. F., Hardenbergh, P. H., Ho, A. Y., et al. (2016). Postmastectomy radiotherapy: an american society of clinical oncology, american society for radiation oncology, and society of surgical oncology focused guideline update. Practical Radiation Oncology, 6(6), e219–e234.
McGale, P., Taylor, C., Correa, C., Cutter, D., Duane, F., Ewertz, M., et al. (2014). Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Elsevier.
Marks, L. B., & Prosnitz, L. R. (2013). Reducing local therapy in patients responding to preoperative systemic therapy: are we outsmarting ourselves? Journal of Clinical Oncology, 32(6), 491–493.
White, J., & Mamounas, E. (2013). Locoregional radiotherapy in patients with breast cancer responding to neoadjuvant chemotherapy: a paradigm for treatment individualization. Journal of Clinical Oncology, 32(6), 494–495.
Haviland, J. S., Owen, J. R., Dewar, J. A., Agrawal, R. K., Barrett, J., Barrett-Lee, P. J., et al. (2013). The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. The Lancet Oncology, 14(11), 1086–1094.
Whelan, T. J., Pignol, J.-P., Levine, M. N., Julian, J. A., MacKenzie, R., Parpia, S., et al. (2010). Long-term results of hypofractionated radiation therapy for breast cancer. New England Journal of Medicine, 362(6), 513–520.
Bartelink, H., Maingon, P., Poortmans, P., Weltens, C., Fourquet, A., Jager, J., et al. (2015). Whole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trial. The Lancet Oncology, 16(1), 47–56.
Kunkler, I. H., Williams, L. J., Jack, W. J., Cameron, D. A., Dixon, J. M., & Investigators, P. I. (2015). Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. The Lancet Oncology, 16(3), 266–273. https://doi.org/10.1016/S1470-2045(14)71221-5.
Hughes, K. S., Schnaper, L. A., Bellon, J. R., Cirrincione, C. T., Berry, D. A., McCormick, B., et al. (2013). Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. Journal of Clinical Oncology, 31(19), 2382–2387.
Coles, C. E., Griffin, C. L., Kirby, A. M., Titley, J., Agrawal, R. K., Alhasso, A., et al. (2017). Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. The Lancet, 390(10099), 1048–1060.
Strnad, V., Ott, O. J., Hildebrandt, G., Kauer-Dorner, D., Knauerhase, H., Major, T., et al. (2016). 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. The Lancet, 387(10015), 229–238.
Hieken, T. J., Mutter, R. W., Jakub, J. W., Boughey, J. C., Degnim, A. C., Sukov, W. R., et al. (2016). A novel treatment schedule for rapid completion of surgery and radiation in early-stage breast cancer. Annals of Surgical Oncology, 23(10), 3297–3303.
Darby, S. C., Ewertz, M., McGale, P., Bennet, A. M., Blom-Goldman, U., Brønnum, D., et al. (2013). Risk of ischemic heart disease in women after radiotherapy for breast cancer. New England Journal of Medicine, 368(11), 987–998.
Taylor, C., Correa, C., Duane, F. K., Aznar, M. C., Anderson, S. J., Bergh, J., et al. (2017). Estimating the risks of breast cancer radiotherapy: evidence from modern radiation doses to the lungs and heart and from previous randomized trials. Journal of Clinical Oncology, 35(15), 1641–1649.
Beck, R. E., Kim, L., Yue, N. J., Haffty, B. G., Khan, A. J., & Goyal, S. (2014). Treatment techniques to reduce cardiac irradiation for breast cancer patients treated with breast-conserving surgery and radiation therapy: a review. Frontiers in oncology, 4.
MacDonald, S. M., Patel, S. A., Hickey, S., Specht, M., Isakoff, S. J., Gadd, M., et al. (2013). Proton therapy for breast cancer after mastectomy: early outcomes of a prospective clinical trial. International Journal of Radiation Oncology* Biology* Physics, 86(3), 484–490.
Mutter, R. W., Remmes, N. B., Kahila, M. M., Hoeft, K. A., Pafundi, D. H., Zhang, Y., et al. (2017). Initial clinical experience of postmastectomy intensity modulated proton therapy in patients with breast expanders with metallic ports. Practical Radiation Oncology, 7(4), e243–e252.
Giordano, S. H., Perkins, G. H., Broglio, K., Garcia, S. G., Middleton, L. P., Buzdar, A. U., et al. (2005). Adjuvant systemic therapy for male breast carcinoma. Cancer, 104(11), 2359–2364. https://doi.org/10.1002/cncr.21526.
Ribeiro, G., & Swindell, R. (1992). Adjuvant tamoxifen for male breast cancer (MBC). British Journal of Cancer, 65(2), 252–254.
Goss, P. E., Reid, C., Pintilie, M., Lim, R., & Miller, N. (1999). Male breast carcinoma: a review of 229 patients who presented to the Princess Margaret Hospital during 40 years: 1955-1996. Cancer, 85(3), 629–639.
Ribeiro, G. (1985). Male breast carcinoma--a review of 301 cases from the Christie Hospital & Holt Radium Institute, Manchester. British Journal of Cancer, 51(1), 115–119.
Eggemann, H., Ignatov, A., Smith, B. J., Altmann, U., von Minckwitz, G., Rohl, F. W., et al. (2013). Adjuvant therapy with tamoxifen compared to aromatase inhibitors for 257 male breast cancer patients. Breast Cancer Research and Treatment, 137(2), 465–470. https://doi.org/10.1007/s10549-012-2355-3.
Davies, C., Pan, H., Godwin, J., Gray, R., Arriagada, R., Raina, V., et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. The Lancet, 381(9869), 805–816. https://doi.org/10.1016/S0140-6736(12)61963-1.
Gray, R. G., Rea, D., Handley, K., Bowden, S. J., Perry, P., Earl, H. M., et al. (2013). aTTom: long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. American Society of Clinical Oncology.
Pemmaraju, N., Munsell, M., Hortobagyi, G., & Giordano, S. (2011). Retrospective review of male breast cancer patients: analysis of tamoxifen-related side-effects. Annals of Oncology, 23(6), 1471–1474.
Visram, H., Kanji, F., & Dent, S. (2010). Endocrine therapy for male breast cancer: rates of toxicity and adherence. Current Oncology, 17(5), 17.
Moredo Anelli, T. F., Anelli, A., Tran, K. N., Lebwohl, D. E., & Borgen, P. I. (1994). Tamoxifen adminstration is associated with a high rate of treatment-limiting symptoms in male breast cancer patients. Cancer, 74(1), 74–77.
Ruddy, K. J., Giobbie-Hurder, A., Giordano, S. H., Goldfarb, S., Kereakoglow, S., Winer, E. P., et al. (2013). Quality of life and symptoms in male breast cancer survivors. The Breast, 22(2), 197–199.
Bagley, C. S., Wesley, M. N., Young, R. C., & Lippman, M. E. (1987). Adjuvant chemotherapy in males with cancer of the breast. American Journal of Clinical Oncology, 10(1), 55–60.
Walshe, J. M., Berman, A. W., Vatas, U., Steinberg, S. M., Anderson, W. F., Lippman, M. E., et al. (2007). A prospective study of adjuvant CMF in males with node positive breast cancer: 20-year follow-up. Breast Cancer Research and Treatment, 103(2), 177–183. https://doi.org/10.1007/s10549-006-9363-0.
Yildirim, E., & Berberoglu, U. (1998). Male breast cancer: a 22-year experience. European Journal of Surgical Oncology, 24(6), 548–552.
Patel 2nd, H. Z., Buzdar, A. U., & Hortobagyi, G. N. (1989). Role of adjuvant chemotherapy in male breast cancer. Cancer, 64(8), 1583–1585.
Shak, S., Palmer, G., Baehner, F. L., Millward, C., Watson, D., & Sledge Jr., G. W. (2009). Molecular characterization of male breast cancer by standardized quantitative RT-PCR analysis: First large genomic study of 347 male breast cancers compared to 82,434 female breast cancers. Journal of Clinical Oncology, 27(15_suppl), 549–549. https://doi.org/10.1200/jco.2009.27.15_suppl.549.
Grenader, T., Yerushalmi, R., Tokar, M., Fried, G., Kaufman, B., Peretz, T., et al. (2014). The 21-gene recurrence score assay (Oncotype DX™) in estrogen receptor-positive male breast cancer: experience in an Israeli cohort. Oncology, 87(1), 1–6.
Peethambaram, P. P., Hoskin, T. L., Day, C. N., Goetz, M. P., Habermann, E. B., & Boughey, J. C. (2017). Use of 21-gene recurrence score assay to individualize adjuvant chemotherapy recommendations in ER+/HER2− node positive breast cancer—a National Cancer Database study. NPJ breast cancer, 3, 41.
Gianni, L., Pienkowski, T., Im, Y. H., Roman, L., Tseng, L. M., Liu, M. C., et al. (2012). Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. The Lancet Oncology, 13(1), 25–32. https://doi.org/10.1016/S1470-2045(11)70336-9.
Baselga, J., Bradbury, I., Eidtmann, H., Di Cosimo, S., de Azambuja, E., Aura, C., et al. (2012). Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet, 379(9816), 633–640. https://doi.org/10.1016/S0140-6736(11)61847-3.
von Minckwitz, G., Procter, M., de Azambuja, E., Zardavas, D., Benyunes, M., Viale, G., et al. (2017). Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. The New England Journal of Medicine, 377(2), 122–131. https://doi.org/10.1056/NEJMoa1703643.
Chan, A., Delaloge, S., Holmes, F. A., Moy, B., Iwata, H., Harvey, V. J., et al. (2016). Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet Oncology, 17(3), 367–377. https://doi.org/10.1016/S1470-2045(15)00551-3.
Dear, R. F., McGeechan, K., Jenkins, M. C., Barratt, A., Tattersall, M. H., & Wilcken, N. (2013). Combination versus sequential single agent chemotherapy for metastatic breast cancer. Cochrane Database of Systematic Reviews, 12, CD008792. https://doi.org/10.1002/14651858.CD008792.pub2.
Treves, N. (1959). The treatment of cancer, especially inoperable cancer, of the male breast by ablative surgery (orchiectomy, adrenalec tomy, and hypophysectomy) and hormone therapy (estrogens and corticosteroids); an analysis of 42 patients. Cancer, 12(4), 820–832.
Neifeld, J. P., Meyskens, F., Tormey, D. C., & Javadpour, N. (1976). The role of orchiectomy in the management of advanced male breast cancer. Cancer, 37(2), 992–995.
Kraybill, W. G., Kaufman, R., & Kinne, D. (1981). Treatment of advanced male breast cancer. Cancer, 47(9), 2185–2189.
Kantarjian, H., Yap, H. Y., Hortobagyi, G., Buzdar, A., & Blumenschein, G. (1983). Hormonal therapy for metastatic male breast cancer. Archives of Internal Medicine, 143(2), 237–240.
Izquierdo, M. A., Alonso, C., De Andres, L., & Ojeda, B. (1994). Male breast cancer. Report of a series of 50 cases. Acta Oncologica, 33(7), 767–771.
Patterson, J. S., Battersby, L. A., & Bach, B. K. (1980). Use of tamoxifen in advanced male breast cancer. Cancer Treatment Reports, 64(6–7), 801–804.
Jaiyesimi, I. A., Buzdar, A. U., Sahin, A. A., & Ross, M. A. (1992). Carcinoma of the male breast. Annals of Internal Medicine, 117(9), 771–777.
Pemmaraju, N., Munsell, M. F., Hortobagyi, G. N., & Giordano, S. H. (2012). Retrospective review of male breast cancer patients: analysis of tamoxifen-related side-effects. Annals of Oncology, 23(6), 1471–1474. https://doi.org/10.1093/annonc/mdr459.
Giordano, S. H., Valero, V., Buzdar, A. U., & Hortobagyi, G. N. (2002). Efficacy of anastrozole in male breast cancer. American Journal of Clinical Oncology, 25(3), 235–237.
Italiano, A., Largillier, R., Marcy, P. Y., Foa, C., Ferrero, J. M., Hartmann, M. T., et al. (2004). Complete remission obtained with letrozole in a man with metastatic breast cancer. La Revue de Médecine Interne, 25(4), 323–324. https://doi.org/10.1016/j.revmed.2003.12.006.
Zabolotny, B. P., Zalai, C. V., & Meterissian, S. H. (2005). Successful use of letrozole in male breast cancer: a case report and review of hormonal therapy for male breast cancer. Journal of Surgical Oncology, 90(1), 26–30. https://doi.org/10.1002/jso.20233.
Doyen, J., Italiano, A., Largillier, R., Ferrero, J. M., Fontana, X., & Thyss, A. (2010). Aromatase inhibition in male breast cancer patients: biological and clinical implications. Annals of Oncology, 21(6), 1243–1245. https://doi.org/10.1093/annonc/mdp450.
Giordano, S. H., & Hortobagyi, G. N. (2006). Leuprolide acetate plus aromatase inhibition for male breast cancer. Journal of Clinical Oncology, 24(21), e42–e43. https://doi.org/10.1200/JCO.2006.07.2397.
Hemsell, D. L., Grodin, J. M., Brenner, P. F., Siiteri, P. K., & MacDonald, P. C. (1974). Plasma precursors of estrogen. II. Correlation of the extent of conversion of plasma androstenedione to estrone with age. J Clin Endocrinol Metab, 38(3), 476–479. https://doi.org/10.1210/jcem-38-3-476.
Nordman, I. C., & Dalley, D. N. (2008). Breast cancer in men: should aromatase inhibitors become first-line hormonal treatment? The Breast Journal, 14(6), 562–569. https://doi.org/10.1111/j.1524-4741.2008.00648.x.
Mauras, N., O'Brien, K. O., Klein, K. O., & Hayes, V. (2000). Estrogen suppression in males: metabolic effects. The Journal of Clinical Endocrinology and Metabolism, 85(7), 2370–2377. https://doi.org/10.1210/jcem.85.7.6676.
Zagouri, F., Sergentanis, T. N., Chrysikos, D., Dimopoulos, M. A., & Psaltopoulou, T. (2015). Fulvestrant and male breast cancer: a pooled analysis. Breast Cancer Research and Treatment, 149(1), 269–275. https://doi.org/10.1007/s10549-014-3240-z.
Finn, R. S., Crown, J. P., Lang, I., Boer, K., Bondarenko, I. M., Kulyk, S. O., et al. (2015). The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. The Lancet Oncology, 16(1), 25–35. https://doi.org/10.1016/S1470-2045(14)71159-3.
Finn, R. S., Martin, M., Rugo, H. S., Jones, S., Im, S. A., Gelmon, K., et al. (2016). Palbociclib and letrozole in advanced breast Cancer. The New England Journal of Medicine, 375(20), 1925–1936. https://doi.org/10.1056/NEJMoa1607303.
Turner, N. C., Ro, J., Andre, F., Loi, S., Verma, S., Iwata, H., et al. (2015). Palbociclib in hormone-receptor-positive advanced breast Cancer. The New England Journal of Medicine, 373(3), 209–219. https://doi.org/10.1056/NEJMoa1505270.
Hortobagyi, G. N., Stemmer, S. M., Burris, H. A., Yap, Y. S., Sonke, G. S., Paluch-Shimon, S., et al. (2016). Ribociclib as first-line therapy for HR-positive, advanced breast Cancer. The New England Journal of Medicine, 375(18), 1738–1748. https://doi.org/10.1056/NEJMoa1609709.
Goetz, M. P., Toi, M., Campone, M., Sohn, J., Paluch-Shimon, S., Huober, J., et al. (2017). MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. Journal of Clinical Oncology, JCO. 2017.2075. 6155.
Dickler, M. N., Tolaney, S. M., Rugo, H. S., Cortes, J., Diéras, V., Patt, D. A., et al. (2016). MONARCH1: Results from a phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as monotherapy, in patients with HR+/HER2-breast cancer, after chemotherapy for advanced disease. American Society of Clinical Oncology.
Sorscher, S. (2016). A first case of male breast Cancer responding to combined aromatase inhibitor/palbociclib therapy. International Journal of Cancer and Clinical Research, 3(7).
Baselga, J., Campone, M., Piccart, M., Burris 3rd, H. A., Rugo, H. S., Sahmoud, T., et al. (2012). Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. The New England Journal of Medicine, 366(6), 520–529. https://doi.org/10.1056/NEJMoa1109653.
Bachelot, T., Bourgier, C., Cropet, C., Ray-Coquard, I., Ferrero, J. M., Freyer, G., et al. (2012). Randomized phase II trial of everolimus in combination with tamoxifen in patients with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer with prior exposure to aromatase inhibitors: a GINECO study. Journal of Clinical Oncology, 30(22), 2718–2724. https://doi.org/10.1200/JCO.2011.39.0708.
Ballatore, Z., Pistelli, M., Battelli, N., Pagliacci, A., De Lisa, M., Berardi, R., et al. (2016). Everolimus and exemestane in long survival hormone receptor positive male breast cancer: case report. BMC Research Notes, 9(1), 497. https://doi.org/10.1186/s13104-016-2301-2.
Kattan, J., & Kourie, H. R. (2014). The use of everolimus to reverse tamoxifen resistance in men with metastatic breast cancer: a case report. Investigational New Drugs, 32(5), 1046–1047. https://doi.org/10.1007/s10637-014-0133-2.
Giotta, F., Acito, L., Candeloro, G., Del Medico, P., Gadaleta-Caldarola, G., Giordano, G., et al. (2016). Eribulin in male patients with breast cancer: the first report of clinical outcomes. The Oncologist, 21(11), 1298–1305.
Yap, H.-Y., Tashima, C. K., Blumenschein, G. R., Hortobagyi, G. N., & Eckles, N. (1980). Chemotherapy for advanced male breast cancer. Jama, 243(17), 1739–1741.
Rudlowski, C., Rath, W., Becker, A. J., Wiestler, O. D., & Buttner, R. (2001). Trastuzumab and breast cancer. The New England Journal of Medicine, 345(13), 997–998.
Carmona-Bayonas, A. (2007). Potential benefit of maintenance trastuzumab and anastrozole therapy in male advanced breast cancer. Breast, 16(3), 323–325. https://doi.org/10.1016/j.breast.2006.12.010.
Hayashi, H., Kimura, M., Yoshimoto, N., Tsuzuki, M., Tsunoda, N., Fujita, T., et al. (2009). A case of HER2-positive male breast cancer with lung metastases showing a good response to trastuzumab and paclitaxel treatment. Breast Cancer, 16(2), 136–140. https://doi.org/10.1007/s12282-008-0060-1.
Farrow, J. H., & Adair, F. E. (1942). Effect of orchidectomy on skeletal metastases from cancer of the male breast. Science (New York, NY), 95(2478), 654.
Kidwai, N., Gong, Y., Sun, X., Deshpande, C. G., Yeldandi, A. V., Rao, M. S., et al. (2003). Expression of androgen receptor and prostate-specific antigen in male breast carcinoma. Breast Cancer Research, 6(1), R18.
Di Lauro, L., Barba, M., Pizzuti, L., Vici, P., Sergi, D., Di Benedetto, A., et al. (2015). Androgen receptor and antiandrogen therapy in male breast cancer. Cancer Letters, 368(1), 20–25.
Lopez, M., Natali, M., Lauro, L. D., Vici, P., Pignatti, F., & Carpano, S. (1993). Combined treatment with buserelin and cyproterone acetate in metastatic male breast cancer. Cancer, 72(2), 502–505.
Di Lauro, L., Vici, P., Barba, M., Pizzuti, L., Sergi, D., Rinaldi, M., et al. (2014). Antiandrogen therapy in metastatic male breast cancer: results from an updated analysis in an expanded case series. Breast Cancer Research and Treatment, 148(1), 73–80.
Panet-Raymond, V., Gottlieb, B., Beitel, L. K., Pinsky, L., & Trifiro, M. A. (2000). Interactions between androgen and estrogen receptors and the effects on their transactivational properties. Molecular and Cellular Endocrinology, 167(1–2), 139–150.
Robinson, J. L., Macarthur, S., Ross-Innes, C. S., Tilley, W. D., Neal, D. E., Mills, I. G., et al. (2011). Androgen receptor driven transcription in molecular apocrine breast cancer is mediated by FoxA1. The EMBO Journal, 30(15), 3019–3027. https://doi.org/10.1038/emboj.2011.216.
Elebro, K., Borgquist, S., Simonsson, M., Markkula, A., Jirstrom, K., Ingvar, C., et al. (2015). Combined androgen and estrogen receptor status in breast cancer: treatment prediction and prognosis in a population-based prospective cohort. Clinical Cancer Research, 21(16), 3640–3650. https://doi.org/10.1158/1078-0432.CCR-14-2564.
Cochrane, D. R., Bernales, S., Jacobsen, B. M., Cittelly, D. M., Howe, E. N., D'Amato, N. C., et al. (2014). Role of the androgen receptor in breast cancer and preclinical analysis of enzalutamide. Breast Cancer Research, 16(1), R7. https://doi.org/10.1186/bcr3599.
Kwiatkowska, E., Teresiak, M., Filas, V., Karczewska, A., Breborowicz, D., & Mackiewicz, A. (2003). BRCA2 mutations and androgen receptor expression as independent predictors of outcome of male breast cancer patients. Clinical Cancer Research, 9(12), 4452–4459.
Di Lauro, L., Pizzuti, L., Barba, M., Sergi, D., Sperduti, I., Mottolese, M., et al. (2015). Role of gonadotropin-releasing hormone analogues in metastatic male breast cancer: results from a pooled analysis. Journal of Hematology & Oncology, 8(1), 53.
Robson, M., Im, S.-A., Senkus, E., Xu, B., Domchek, S. M., Masuda, N., et al. (2017). Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. New England Journal of Medicine.
Litton, J., Rugo, H. S., Hurvitz, S., Gonçalves, A., Lee, K.-H., Fehrenbacher, L., et al. EMBRACA: a phase 3 trial comparing talazoparib, an oral PARP inhibitor, to physician’s choice of therapy in patients with advanced breast cancer and a germline BRCA mutation. In San Antonio Breast Cancer Symposium, San Antonio, TX, 2017 (Vol. Oral Session: General Session 6).
Pujade-Lauraine, E., Ledermann, J. A., Selle, F., Gebski, V., Penson, R. T., Oza, A. M., et al. (2017). Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. The Lancet Oncology, 18(9), 1274–1284.
Swisher, E. M., Lin, K. K., Oza, A. M., Scott, C. L., Giordano, H., Sun, J., et al. (2017). Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 part 1): an international, multicentre, open-label, phase 2 trial. The Lancet Oncology, 18(1), 75–87.
Mirza, M. R., Monk, B. J., Herrstedt, J., Oza, A. M., Mahner, S., Redondo, A., et al. (2016). Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. New England Journal of Medicine, 375(22), 2154–2164.
Mateo, J., Carreira, S., Sandhu, S., Miranda, S., Mossop, H., Perez-Lopez, R., et al. (2015). DNA-repair defects and olaparib in metastatic prostate cancer. The New England Journal of Medicine, 2015(373), 1697–1708.
Ferzoco, R. M., & Ruddy, K. J. (2015). Optimal delivery of male breast cancer follow-up care: improving outcomes. Breast Cancer: Targets and Therapy, 7, 371.
Loren, A. W., Mangu, P. B., Beck, L. N., Brennan, L., Magdalinski, A. J., Partridge, A. H., et al. (2013). Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology, 31(19), 2500–2510.
Grenader, T., Goldberg, A., & Shavit, L. (2008). Second cancers in patients with male breast cancer: a literature review. Journal of Cancer Survivorship, 2(2), 73–78.
Auvinen, A., Curtis, R. E., & Ron, E. (2002). Risk of subsequent cancer following breast cancer in men. Journal of the National Cancer Institute, 94(17), 1330–1332.
Giordano, S. H., Buzdar, A. U., & Hortobagyi, G. N. (2002). Breast cancer in men. Annals of Internal Medicine, 137(8), 678–687.
Estala, S. M. (2006). Proposed screening recommendations for male breast cancer. The Nurse Practitioner, 31(2), 62–63.
Farrell, E., Borstelmann, N., Meyer, F., Partridge, A., Winer, E., & Ruddy, K. (2014). Male breast cancer networking and telephone support group: A model for supporting a unique population. Psycho-Oncology, 23(8), 956–958.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leon-Ferre, R.A., Giridhar, K.V., Hieken, T.J. et al. A contemporary review of male breast cancer: current evidence and unanswered questions. Cancer Metastasis Rev 37, 599–614 (2018). https://doi.org/10.1007/s10555-018-9761-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-018-9761-x