Abstract
A strong natural selection for microbial antibiotic resistance has resulted from the extensive use and misuse of antibiotics. Though multiple factors are responsible for this crisis, the most significant factor – widespread prescription of broad-spectrum antibiotics – is largely driven by the fact that the standard process for determining antibiotic susceptibility includes a 1–2-day culture period, resulting in 48–72 h from patient sample to final determination. Clearly, disruptive approaches, rather than small incremental gains, are needed to address this issue. The field of microfluidics promises several advantages over existing macro-scale methods, including: faster assays, increased multiplexing, smaller volumes, increased portability for potential point-of-care use, higher sensitivity, and rapid detection methods. This Perspective will cover the advances made in the field of microfluidic, phenotypic antibiotic susceptibility testing (AST) over the past two years. Sections are organized based on the functionality of the chip – from simple microscopy platforms, to gradient generators, to antibody-based capture devices. Microfluidic AST methods that monitor growth as well as those that are not based on growth are presented. Finally, we will give our perspective on the major hurdles still facing the field, including the need for rapid sample preparation and affordable detection technologies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
1.
Introduction
-
1.1.
Antibiotic resistance: A global health crisis
-
1.2.
Need for innovative AST methodologies
-
1.3.
Microfluidics and AST
-
1.1.
-
2.
Microfluidic AST methods based on bacterial growth
-
2.1.
Incubator and/or microscopy platform
-
2.1.1.
Chip alone
-
2.1.2.
Hydrogel used
-
2.1.1.
-
2.2.
Gradient generator
-
2.2.1.
Chip alone
-
2.2.2.
Hydrogel used
-
2.2.1.
-
2.3.
Identification + AST
-
2.1.
-
3.
Microfluidic AST methods based on bacterial death
-
4.
Future outlook
-
4.1.
Major hurdle of turn-around-time: Growth steps, particularly from uncultured blood
-
4.2.
Major hurdle of affordability: Expensive detection technologies
-
4.3.
Conclusion
-
4.1.
1 Introduction
1.1 Antibiotic resistance: a global health crisis
The extensive use and misuse of antibiotics has resulted in a strong natural selection for microbial antibiotic resistance so that we now face the risk of entering a post-antibiotic era (Cars et al. 2011). The Centers for Disease Control and Prevention have identified 18 pathogens that pose the largest threat to human health in the US, ranging from “urgent” and “serious” to “concerning” (CDC 2013). Each of these pathogens (with the exception of Clostridium difficile) has developed resistance to at least one of our first-line antibiotics (Table 1), resulting in the current crisis in which more than two million people are sickened by antibiotic-resistant infections in the US each year, leading to more than 23,000 deaths (CDC 2013).
The developing consensus is that multiple factors are contributing to the rise in antibiotic resistance, including the inappropriate prescription of antibiotics (in both developed and developing countries), the lack of antibiotic stewardship programs in developing countries, and worldwide patient non-compliance to antibiotic regimens. The most significant factor – widespread prescription of broad-spectrum antibiotics – is largely driven by the fact that the standard process for determining antibiotic susceptibility, from patient sample to final result, includes a 1–2-day culture period and takes 48–72 h (Lu et al. 2013).
1.2 Need for innovative antibiotic susceptibility test (AST) methodologies
A survey of the antimicrobial susceptibility test (AST) methods available demonstrates a need for new approaches that would enable rapid, inexpensive, and sensitive tests that can quickly provide physicians with antibiotic susceptibility profiles (Jorgensen et al. 2009). The more traditional culture-based methods are accurate and inexpensive, but require strict adherence to standard protocols (Henry 2001) and significant operator and assay time (18–24 h with additional time needed for culture and subculture of patient samples). Semi-automated susceptibility systems (i.e., VITEK and MicroScan) decrease the turn-around-time and operator touch-time (culture and colony isolation are still required), but can add significant cost to the tests. With the fastest test requiring 9 h to complete, these semi-automated systems do not provide information in time to influence initial treatment decisions (Mittman et al. 2009; Chatzigeorgiou et al. 2011).
Molecular methods (e.g., PCR) can be useful in outbreaks, but are not appropriate for broad-spectrum diagnosis because 1) genetic markers have not been identified for all antibiotic-resistant bacterial strains and 2) susceptibility is not always correlated with genetic markers (Tato et al. 2010). Additionally, molecular approaches are susceptible to failure caused by the high frequency of genetic mutation under selective pressure (Stamper et al. 2011). Hence, functional or phenotypic assays more accurately determine antibiotic susceptibility.
To enable physicians to prescribe appropriate antimicrobial therapy, new, rapid AST methods must be developed that can deliver phenotypic antibiotic resistance information in time for initial drug therapy decisions. To facilitate this goal, these new ASTs must enable a massive reduction in the overall time to results by testing clinical samples directly and eliminating the need for culture. This, in turn, means that the test methods must be sensitive enough to achieve categorical agreement (S, I, or R) greater than 90 % of the time (Thornsberry 1985) with a limited initial inoculum (~100 CFU), especially in cases of bacteremia where concentrations range from 0.1–10 CFU/mL in blood.
Several organizations have recognized the urgent need for rapid antibiotic susceptibility testing. The £10 M Longitude Prize offered by the UK government has the aggressive goal to go from sample to result in less than thirty minutes. This prize also demands that the technology be affordable, easy-to-use—requiring only minimal training of health personnel—scalable to industrial manufacturing methods, safe, and of course, accurate. The upcoming $20 M Point-of-Care Diagnostic Challenge Prize offered by the US government will likely have a similar target. These initiatives aim to stimulate the development of disruptive approaches, rather than small incremental gains, to truly impact clinical practice.
1.3 Microfluidics and AST
Because conventional methods use turbidity as a measure of growth (with a limited sensitivity of 107 CFU/mL), bacterial populations must grow 16–20 h before reaching a detectable level (Dalgaard et al. 1994). Thus, methods with much lower limits of detection are needed to accelerate ASTs. The field of microfluidics promises several advantages over existing macro-scale methods (Sackmann et al. 2014). Increased multiplexing means that many tests can be run in parallel on a single sample. Automated assays require less training for operators and improve reproducibility. The use of smaller volumes means that precious reagents are conserved and costs are reduced. A smaller footprint also increases portability and potential point-of-care use. Finally, and most importantly, shorter diffusion distances and sensitive detection methods allow for faster assay times. In addition to being highly beneficial in developed countries, these features could also aid in the deployment of rapid ASTs to low - resource settings where overuse of antibiotics is rampant.
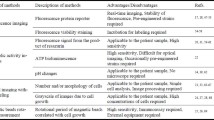
This Perspective highlights the advances made in the field of phenotypic, microfluidic AST methods over the past two years (summarized in Table 2). Because of this timeframe, some major areas of microfluidic AST research are not discussed, including plug-based screening methods (Boedicker et al. 2008; Funfak et al. 2009; Cao et al. 2012; Churski et al. 2012), bacterial growth within gas-permeable devices (Cira et al. 2012; Lu et al. 2013), and the measurement of bacterial growth as a function of bead rotation (AMBR) (Kinnunen et al. 2011; Sinn et al. 2011; Kinnunen et al. 2012).
2 Microfluidic AST methods based on bacterial growth
To accelerate the measurement of bacterial growth in the presence of antibiotics, microfluidic platforms have been developed that confine the microbes. In each of the cases presented here, bacteria are confined to a small volume (wells, channels or chambers), captured with antibodies (coated beads or membranes), or encapsulated in agarose. Confining the microbes accomplishes various purposes, which include increasing sensitivity by reducing diffusion distances and allowing for the microscopic tracking of individual bacteria. We have organized the various microfluidic platforms (summarized in Table 2) to highlight the differences in chip functionality. Some chips function as microscopy platforms (dilutions and incubations are performed off-chip) while others are almost entirely autonomous (all reagent manipulations and incubations are conducted on-chip). Still others incorporate both microbial identification and AST into a single platform. As hydrogels are an important recent innovation to the microfluidic AST field, we have separated each section into chips that utilize hydrogels and those that do not.
2.1 Incubator and/or microscopy platform
Researchers have developed microfluidic AST methods that vary widely in their approach and complexity. The simplest chips provide a platform for mixing, incubation and microscopy. Because reagent dilutions must be made off-chip before loading them onto the devices, set-up complexity is equal to the corresponding microbroth dilution methods.
2.1.1 Chip alone
Mohan et al. have reported on a microfluidic AST device that utilizes negative pressure to fill channels that lead into chambers (Mohan et al. 2015). Each set of twelve chambers has an antibiotic channel and a cell channel. Once both sides are filled, a mixing valve is actuated to obtain homogeneous mixtures within the 3-nL chambers. Their platform relies on the fluorescence detection of individual bacteria for precise quantification of bacterial numbers. This system, and the use of GFP-expressing bacteria, allowed them to study the interactions of polymicrobial mixtures in the presence of antibiotics over time. Fluorescence images were acquired every 30 min over the course of the assay (16 h). With a previous version of their platform, the researchers used GFP-expressing Escherichia coli to test the effects of ampicillin, cefalexin, chloramphenicol, and tetracycline alone and in combination (Mohan et al. 2013). Using their device, the antibiotic efficacy against fluorescent mutants could be determined in 2–4 h. A labeling method for wildtype strains has not yet been reported but use of cell-permeant fluorescent dyes is underway. The authors emphasize the advantages of their system, including enhanced detection sensitivity, reduced reagent volumes, and increased combinatorial capabilities. However, ease of portability is tempered by the fact that valve actuation requires a vacuum pump, incubation occurs at 35 °C, and bacterial detection is performed by an inverted fluorescence microscope.
Matsumoto et al. recently reported on a microfluidic platform in which bacteria are loaded into channels containing pre-loaded, dried antibiotic (Matsumoto et al. 2016). Three concentrations of five antibiotics (plus controls) can be tested on a single chip, giving a susceptible or resistant result. Following on-chip incubation (3 h), the four closely spaced channels are observed simultaneously by phase contrast microscopy. Images are acquired near the outlets where oxygenation, and thus bacterial growth, is highest. They found that the solution phase bacteria can settle in the microfluidic channels and, in some cases, sink more rapidly due to morphological changes (i.e., elongation). The authors tested their method using 101 clinical isolates of Pseudomonas aeruginosa (at starting concentrations of ca. 107 CFU/mL) against amikacin, ciprofloxacin, meropenem, ceftazidime, and piperacillin. Agreement rates were ≥90 % for each agent tested. Although the assay is simple and does not require expensive instrumentation, different susceptibility criteria need to be defined for each drug and programmed into dedicated software.
2.1.2 Hydrogel used
Other groups have developed chips that act as incubators and microscopy platforms, which utilize agarose as a means to immobilize the bacteria or define their growth chamber. In each case, the diffusive properties of the agarose (to both chemicals and gases) are critical.
Choi et al. have utilized the diffusion of antibiotics into agarose as a means to measure the MICs of encapsulated bacteria (Choi et al. 2013). Warm agarose was mixed with the bacterial strain of interest (200 μL of 5 × 108 CFU/mL) before being introduced into a central inlet and spreading into six radiating channels. Once solidified, antibiotics at different concentrations were then introduced in the side-branched channels, and diffused into the agarose. The growth of individual bacteria was then monitored over time at the interface of the two channels using bright field microscopy, and processed images were used to determine MICs within 3–4 h.
A year later, the same group disclosed improvements to their system (Choi et al. 2014). They increased the throughput of their device by fabricating a microfluidic chip that molds bacteria-mixed agarose (ca. 107 CFU/mL) into thin, flat slabs surrounding liquid sample wells in a 96-well plate format (Fig. 1a). They also improved the accuracy of their image analysis by including morphological changes in their characterization. They used their new system to test four CLSI strains and 189 clinical isolates, including extended-spectrum beta-lactamase–positive E. coli and Klebsiella pneumoniae, imipenem-resistant P. aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant Enterococci from hospitals. Including morphological changes in their analysis reduced their major error rates from 12.8 to 0.9 % for E. coli and from 48.1 to 13.7 % for P. aeruginosa. Accurate MICs can be determined from imaging just 10–20 bacteria for 3–4 h; however, high initial bacterial concentrations are still required and an auto-pipetting system is needed to load bacteria and pre-made antibiotic solutions into the chip.
The researchers have since extended their work to include on-chip susceptibility testing of Mycobacterium tuberculosis (TB) colonies (ca. 108 CFU) (Choi et al. 2016). This extension required a redesign of their chip that increased the volumes of both agarose and media to allow for long-term culturing. MICs were determined for susceptible (PanS), multi-drug-resistant (MDR) and extensively drug-resistant (XDR) TB against isoniazid, rifampin, ethambutol, and streptomycin in just nine days (as opposed to 4–6 weeks). Testing of 28 clinical isolates gave an agreement rate of 96.4 %, with errors only occurring in the XDR strains. We note that in each of these applications the agarose must be mixed with the bacteria prior to loading it on the chip, potentially increasing exposure to the pathogen.
A recent, novel approach utilizes hydrophilic phaseguides to direct the passive and autonomous capillary priming of hydrogel into a microfluidic chip (Puchberger-Enengl et al. 2015). The hydrogel forms a diffusive barrier that defines the growth chamber and allows for the diffusion of oxygen, antibiotics, and other reagents (Fig. 1b). Interestingly, when the outer chamber is filled with media, the device can also operate in anaerobic mode. The researchers tested the growth of E. coli, Bacillus amyloliquefaciens, and Enterococcus faecalis in growth chambers that were surrounded with agarose that contained ampicillin or gentamicin at concentrations varying between 0 to 128 μg/mL. Following a 3-h incubation with the antibiotics, fluorescent reagents (Syto 9 and hexidium iodide) were added to determine the number of bacteria, their phenotype, and their Gram type. The researchers also showed that their device supports enzyme assays and continuous shear-free culturing (Saccharomyces cerevisiae). Though the device operation is relatively simple, because the agarose must be loaded onto the chip immediately preceding the assay, the set-up complexity is significantly increased.
2.2 Gradient generator
Some groups have developed microfluidic AST platforms that include the additional functionality of on-chip gradient generation. These devices can utilize channels, microfluidic traps, or hydrogel slabs to generate either discrete or continuous gradients. Because the antibiotic dilutions are made on-chip, these methods have the advantage of simplified off-chip assay preparation.
2.2.1 Chip alone
Dai et al. have reported on a microfluidic AST device that measured the EC50 values of antibiotics against GFP-expressing P. aeruginosa in a zero-flow microfluidic chip (Dai et al. 2015). Each of the 14 chambers has an antibiotic metering channel, for concentration gradient formation, and a cell channel (3.5 × 108 CFU/mL). Once both sides are filled, mixing valves are actuated to obtain homogeneous mixtures within the 8-nL chambers. In keeping with standard AST methods, fluorescence images are acquired at 16, 20, and 24 h. The researchers used GFP-expressing P. aeruginosa to test the effects of gentamicin and ciprofloxacin. A labeling method for wildtype strains has not yet been reported. Although the system uses reduced volumes for precious reagents and automatically generates precise concentration gradients, the PDMS chip must be incubated in a humidity chamber to minimize evaporation and bacterial detection requires an inverted fluorescence microscope.
Kim et al. have developed a concentration gradient-forming microfluidic AST platform that tracks the number of bacteria within eight growth chambers (Kim et al. 2015). Bacteria (5 × 105 CFU/mL) mixed with an antibiotic of interest and with buffer are injected into the two input ports, and a concentration gradient is generated via automatic or manual pressure (Fig. 2a). The number of bacteria in each 30-nL chamber is then monitored over time using standard phase contrast microscopy. The researchers used their platform to test the responses of a model E. coli strain against ampicillin and streptomycin, and were able to determine their MICs within 3 h. Though their platform is simple, a humidified incubator is required for their assay and further experimentation is needed to generalize the cell counting method.
Examples of gradient-generating microfluidic AST devices; (a) Kim et al. use varying channel lengths to generate a concentration gradient on-chip; Bacteria are included in both the reagent and diluent; (b) Derzsi et al. use metering traps to deliver a nanoliter-sized bacterial sample to the storage well, followed by diluted reagent; The sequential merging of the diluent and the reagent in the metering traps forms a reagent plug that is approximately half as concentrated as the previous one; Panel a modified from (Kim et al. 2015); Panel b modified and reprinted with permission (Derzsi et al. 2016)
Another gradient-forming microfluidic platform was recently reported by Derzsi et al. (Derzsi et al. 2016). Their chip utilizes the passive capillary action of hydrodynamic traps to meter, merge, route, and store nanoliter-sized samples. The geometry and layout of their biphasic chip allows them to load bacteria and generate an 11-point dilution series in just five pipetting steps (Fig. 2b). The researchers used the reduction of resazurin as a read-out for viable bacteria, and measured fluorescence using a gel imager after 4 h of incubation at 37 °C. For proof of principle, ampicillin was diluted on chip to generate concentrations between 47 and 0.3 μg/mL, and was tested against a model strain of E. coli (at a starting concentration of 5 × 105 CFU/mL). The MIC obtained was in agreement with those reported in the literature. The chip was designed to give a dilution ratio of two, but actually diluted the sample by 1.68-fold. The researchers acknowledge that if other dilution ratios were required for an assay, the geometry of the channels and traps would need to be engineered accordingly.
2.2.2 Hydrogel used
Several groups have capitalized on the diffusive and immobilizing properties of agarose to accomplish gradient generation on-chip. These approaches generate continuous rather than discrete gradients, with antibiotic concentration corresponding to distance. The need to generate fresh agarose slabs (with or without bacteria) at the beginning of each experiment increases the set-up complexity.
Hou et al. recently reported on a platform that tracks the growth of bacteria immobilized within a linear concentration gradient of antibiotic to provide growth curves as functions of time and antibiotic concentration (Hou et al. 2014). They encapsulated bacteria (5 × 106 CFU) in an agarose gel within a commercially available microfluidic chamber and used phase contrast time-lapse photography to acquire (average grey scale) data for 2.5–4 h. The researchers used their method to analyze the responses of E. coli, S. aureus and Salmonella typhimurium to five different classes of antibiotic, obtaining MIC values and bacterial growth rates at sub-MIC concentrations. One advantage of this system is that it avoids the need to pre-label the bacteria for detection. Additionally, measuring the growth inhibition of antibiotics over a continuous gradient (rather than in discrete two-fold increments) can give more finely-tuned MIC values and makes the method impervious to changes in CLSI standards.
To track the growth of single bacteria exposed to various concentrations of antibiotic, Li et al. developed a three-layer microfluidic device (Li et al. 2014). Bacteria (3 μL of ca. 4 × 107 CFU/mL) are sandwiched between a glass slide and thin agarose membrane while two parallel channels in the top PDMS layer (source and sink) generate a linear concentration gradient across the device. The researchers tracked the morphological changes of single E. coli in the presence of a gradient of amoxicillin for 5 h to quantitatively measure antibiotic inhibition over time (Fig. 3a). They also demonstrated the ability of their device to culture slow growing bacteria over a number of days. Using their device, they were able to determine the effects of amoxicillin against Nitrosomonas europaea in four days (rather than the weeks it takes in culture). One can imagine adaptation of this system to monitor susceptibility of the notoriously slow-growing human pathogen M. tuberculosis. All tests were performed at room temperature, eliminating the need for bulky microscope heaters and making the assay more amenable to point-of-care applications.
Examples of microscopic monitoring of bacterial growth (a) or death (b); All scale bars: 10 μm; (a) Bright field images of a monolayer of E. coli during the first 5 h of growth on-chip; Licensed Material modified from (Li et al. 2014); (b) Phase contrast (i–ii) and fluorescence (iii–iv) images for a representative methicillin-sensitive S. aureus strain within an antibiotic-containing microchannel at the start (t = 1 min; i and iii) and the end of the assay (t = 60 min; ii and iv); Modified and reproduced with permission (Kalashnikov et al. 2014). http://pubs.acs.org/page/policy/authorchoice_ccby_termsofuse.html
2.3 Identification + AST
Still other microfluidic platforms include pathogen identification (ID) functionality along with AST. These approaches provide additional information that is critical for infection control and patient care. However, their workflows are complicated and, in the two cases reported here, their coverage is limited by antibody reactivity.
One of these dual functionality platforms was developed by He et al. (He et al. 2014). The chip utilizes antibody-coated glass beads to first capture E. coli O157 for ID (with ca. 90 % capture efficiency) and then tests its susceptibility to antibiotics. The device contains integrated concentration gradient generators to simplify AST, and was designed to align the beads in a monolayer for optimized fluorescence excitation and increased signal strength. The researchers showed that their platform could detect E. coli O157 at a cell density range of 104–108 CFU/mL within 30 min with quantitative determination of bacterial concentration. It can then simultaneously test the effects of three antibiotics within 4–8 h. While this platform can accomplish both ID and AST, its use of a single antibody limits its clinical utility by reducing the capture capability to only one strain of a single bacterial species.
Last year, Dong and Zhao reported on a microfluidic platform that captures and encapsulates the most common causative agents of urinary tract infections (UTIs) to accomplish both rapid ID and AST (Dong and Zhao 2015). Target microbes in the urine sample are captured by a set of 13 antibodies on a fiberglass membrane inside the device and are then encapsulated by alginate. Once captured, a subset of the wells is subjected to an immunosorbent ATP bioluminescence assay for immediate ID of the pathogen. Following ID, AST of eight antibiotics can be run in duplicate on the remaining wells (3–6 h). The researchers used their device to identify UTI pathogens spiked into 5 mL of artificial urine starting at concentrations of 1 × 103–1 × 105 CFU/mL, well within the range of clinical UTIs. Immunocapture and testing directly from urine greatly simplifies sample handling; however, antibodies are expensive and can lead to false negatives when a pathogen outside of the antibody set is responsible for the infection.
3 AST methods based on bacterial death
All of the aforementioned AST methods are based on the ability of the bacteria to proliferate in the presence of antibiotics. However, we believe that to develop a truly rapid susceptibility test, one must circumvent the need for growth. Disruptive technologies often require redefinitions. Hence, an alternative approach to measuring the growth of resistant strains in the presence of high concentrations of antibiotic is to monitor the death of susceptible strains under the same conditions.
We have explored the hypothesis that stress potentiates the action of antibiotics, reducing the time required to observe bacterial antibiotic susceptibility (Kalashnikov et al. 2014). To do so, we built a multi-channel microfluidic device capable of interrogating multiple bacterial strains and multiple antibiotics simultaneously. Bacterial cells are injected into the device (40 μL of 106 CFU/mL) and immobilized on an epoxide-coated glass slide on the floor of the microfluidic channel. The cells are exposed to shear stress by fluid flow (containing media, a chemical stressor, and a fluorescent dead cell stain) in the presence (experiment) or absence (control) of antibiotic. The percent of dead cells in each channel (the number of dead bacteria divided by the total number of bacteria) is monitored for 60 min via phase contrast and fluorescence microscopy (Fig. 3b). The percent of dead cells in the control channel is then subtracted from the percent in the experiment channel, giving a measure of bacterial cell death caused by antibiotic alone. We have shown that the method can distinguish between MRSA and methicillin-sensitive S. aureus in less than 30 min of applied stress, correctly assigning the susceptibility to methicillin of 18 strains tested in a blinded study (Kalashnikov et al. 2012). We have shown that our phenotypic AST is rapid, circumventing the need to wait for bacterial growth in the presence of antibiotic. Current drawbacks include the need for a fluorescence microscope, syringe pumps, and large volumes of antibiotic-containing media (ca. 60 mL per channel).
4 Future outlook
Despite the substantial advances made in the field, taking the Longitude Prize goals as the benchmark, the field still faces significant challenges. Technologies must be able to drive total turn-around-time down to less than thirty minutes while being affordable.
4.1 Major hurdle of turn-around-time: growth steps, particularly from uncultured blood
While the novel technologies described above represent considerable innovation in the field of microfluidic ASTs, they still require relatively high concentrations of input bacteria. With respect to assay time, although these microfluidic ASTs are rapid, the time required for susceptibility testing only accounts for half of the 48–72-h delay. Another 1–2 days are required to culture patient samples to increase the number of microbes present. Sample preparation (especially in blood-borne infections, where bacterial concentrations are so low) is therefore a current bottleneck for realizing the full potential of microfluidics-based biodetection (Mariella 2008), particularly accelerated, phenotypic, microfluidic ASTs.
To be truly rapid, workflows must circumvent the need for blood culture, purified colonies, and overnight subcultures, and test uncultured clinical samples directly. To do this, methods must be developed that eliminate the majority of blood cells and proteins while maintaining the integrity of the infective microbe. Approaches have included selective lysis followed by filtration (Farmer and Komorowski 1972; Sullivan et al. 1975), centrifugation (Boardman et al. 2015), or spin column purification (Loonen et al. 2013), and centrifugal gradients followed by filtration (Herlich et al. 1982; Lamberg et al. 1983; Bernhardt et al. 1991).
An inertial microfluidic device was recently published that can separate bacteria from the majority of blood components at a rate of 20 min/mL of whole blood (Hou et al. 2015). Recoveries of E. coli, P. aeruginosa, S. aureus and E. faecalis were ~65 % at 100 CFU/mL (alone and in combination). Following centrifugation of the bacterial output from the device and lysis, NanoString technology was employed for pathogen ID. Using biotinylated and fluorescently-tagged probes for species-specific rRNA sequences, the researchers showed that they were able to distinguish between three species of bacteria. Using this approach, they could identify bacteria directly from whole blood in ~8 h. They also showed that they could detect ciprofloxacin-responsive mRNA transcripts from sensitive E. coli by subjecting them to the antibiotic for 30 min prior to lysis. Unfortunately, due to limitations of the NanoString technology, they were only able to obtain susceptibility data on samples with >105 CFU/mL E. coli (or blood samples with 1 CFU/mL that had been cultured for 7.5 h).
4.2 Major hurdle of affordability: expensive detection technologies
Regrettably, the costs of detection and the amount of sample available are often diametrically opposed. The cheapest method of detection has historically been growth of large macroscopic colonies on an agar plate. But, as discussed, arriving at the point where the naked eye can make accurate AST assignments is far too time consuming. Several technologies described here, and in recent years, take the shortcut of microscopically monitoring the growth of single bacteria. However, these approaches can require expensive optics for visualization. Advances in optics for cheaper detection and alternative detection systems that eliminate optics altogether are sorely needed.
4.3 Conclusion
As bacterial populations become more resistant to available antibiotics, it becomes more critical that physicians move to targeted narrow-spectrum antibiotic therapy. This can only be accomplished with new AST methodologies that provide results in a fraction of the time of current protocols. Expertise from a variety of fields will be required to achieve these goals, and cross-disciplinary collaborations will need to be established in order to develop disruptive technologies that will improve patient outcomes and safeguard our antibiotics.
We believe that, with further development, the state-of-the-art AST methods described here could provide new tools to clinicians that would enable targeted and specific antibiotic therapy to be prescribed much earlier than is currently possible. We also note that, for the microfluidic platforms described here, no work has been reported on the “urgent” threats identified by the CDC (Table 1), while reports on “serious” pathogens are limited. For the successful advancement of these technologies, researchers will need to engineer solutions that require fewer input bacteria, and focus their efforts on the antibiotic-resistant pathogens that most threaten human health.
References
M. Bernhardt, D. R. Pennell, L. S. Almer, R. F. Schell, J. Clin. Microbiol. 29, 422 (1991)
A. Boardman, J. Campbell, H. Wirz, A. Sharon, A. F. Sauer-Budge, PLoS One 10, e0116837 (2015)
J. Q. Boedicker, L. Li, T. R. Kline, R. F. Ismagilov, Lab Chip 8, 1265 (2008)
J. Cao, D. Kursten, S. Schneider, A. Knauer, P. M. Gunther, J. M. Kohler, Lab Chip 12, 474 (2012)
O. Cars, A. Hedin, A. Heddini, Drug Resist. Updat. 14, 68 (2011)
CDC (2013) Antibiotic Resistance Threats in the United States, 2013. In: Services UDoHaH (ed), p 114
K. S. Chatzigeorgiou, T. N. Sergentanis, S. Tsiodras, S. J. Hamodrakas, P. G. Bagos, J. Clin. Microbiol. 49, 3284 (2011)
J. Choi, Y. G. Jung, J. Kim, S. Kim, Y. Jung, H. Na, S. Kwon, Lab Chip 13, 280 (2013)
J. Choi et al., Sci. Transl. Med. 6, 267ra174 (2014)
J. Choi et al., Appl. Microbiol. Biotechnol. 100, 2355 (2016)
K. Churski, T. S. Kaminski, S. Jakiela, W. Kamysz, W. Baranska-Rybak, D. B. Weibel, P. Garstecki, Lab Chip 12, 1629 (2012)
N. J. Cira, J. Y. Ho, M. E. Dueck, D. B. Weibel, Lab Chip 12, 1052 (2012)
J. Dai, S. J. Suh, M. Hamon, J. W. Hong, Biotechnol. J. 10, 1783 (2015)
P. Dalgaard, T. Ross, L. Kamperman, K. Neumeyer, T. A. McMeekin, Int. J. Food Microbiol. 23, 391 (1994)
L. Derzsi, T. S. Kaminski, P. Garstecki, Lab Chip 16, 893 (2016)
T. Dong, X. Zhao, Anal. Chem. 87, 2410 (2015)
S. G. Farmer, R. A. Komorowski Appl. Microbiol. 23, 500 (1972)
A. Funfak, J. Cao, O. S. Wolfbeis, K. Martin, J. M. Kohler, Microchim. Acta 164, 279 (2009)
J. He, X. Mu, Z. Guo, H. Hao, C. Zhang, Z. Zhao, Q. Wang, Eur. J. Clin. Microbiol. Infect. Dis. 33, 2223 (2014)
J. B. Henry (ed.), Clinical diagnosis and management by laboratory methods, 20th edn. (Philadelphia, Saunders, 2001)
M. B. Herlich, R. F. Schell, M. Francisco, J. L. LeFrock, J. Clin. Microbiol. 16, 99 (1982)
Z. Hou, Y. An, K. Hjort, K. Hjort, L. Sandegren, Z. Wu Lab Chip 14, 3409 (2014)
H. W. Hou, R. P. Bhattacharyya, D. T. Hung, J. Han, Lab Chip 15, 2297 (2015)
J. H. Jorgensen, M. J. Ferraro, Clin. Infect. Dis. 49, 1749 (2009)
M. Kalashnikov, J. C. Lee, J. Campbell, A. Sharon, A. F. Sauer-Budge, Lab Chip 12, 4523 (2012)
M. Kalashnikov, J. Campbell, J. C. Lee, A. Sharon, A. F. Sauer-Budge, J. Vis. Exp. e50828 (2014)
S. C. Kim, S. Cestellos-Blanco, K. Inoue, R. N. Zare, Antibiotics 4, 455 (2015)
P. Kinnunen, I. Sinn, B. H. McNaughton, D. W. Newton, M. A. Burns, R. Kopelman, Biosens. Bioelectron. 26, 2751 (2011)
P. Kinnunen, B. H. McNaughton, T. Albertson, I. Sinn, S. Mofakham, R. Elbez, D. W. Newton, A. Hunt, R. Kopelman, Small 8, 2477 (2012)
R. E. Lamberg, R. F. Schell, J. L. LeFrock, J. Clin. Microbiol. 17, 856 (1983)
B. Li, Y. Qiu, A. Glidle, D. McIlvenna, Q. Luo, J. Cooper, H. C. Shi, H. Yin, Anal. Chem. 86, 3131 (2014)
A. J. Loonen et al., PLoS One 8, e72349 (2013)
Y. Lu, J. Gao, D. D. Zhang, V. Gau, J. C. Liao, P. K. Wong, Anal. Chem. 85, 3971 (2013)
R. Mariella Jr, Biomed. Microdevices 10, 777 (2008)
Y. Matsumoto, S. Sakakihara, A. Grushnikov, K. Kikuchi, H. Noji, A. Yamaguchi, R. Iino, Y. Yagi, K. Nishino, PLoS One 11, e0148797 (2016)
S. A. Mittman, R. C. Huard, P. Della-Latta, S. Whittier, J. Clin. Microbiol. 47, 3557 (2009)
R. Mohan, A. Mukherjee, S. E. Sevgen, C. Sanpitakseree, J. Lee, C. M. Schroeder, P. J. Kenis, Biosens. Bioelectron. 49, 118 (2013)
R. Mohan, C. Sanpitakseree, A. V. Desai, S. E. Sevgen, C. M. Schroeder, P. J. A. Kenis, RSC Adv. 5, 35211 (2015)
D. Puchberger-Enengl, S. van den Driesche, C. Krutzler, F. Keplinger, M. J. Vellekoop, Biomicrofluidics 9, 014127 (2015)
E. K. Sackmann, A. L. Fulton, D. J. Beebe, Nature 507, 181 (2014)
I. Sinn, P. Kinnunen, T. Albertson, B. H. McNaughton, D. W. Newton, M. A. Burns, R. Kopelman, Lab Chip 11, 2604 (2011)
P. D. Stamper, L. Louie, H. Wong, A. E. Simor, J. E. Farley, K. C. Carroll, J. Clin. Microbiol. 49, 1240 (2011)
N. M. Sullivan, V. L. Sutter, S. M. Finegold, J. Clin. Microbiol. 1, 30 (1975)
M. Tato, M. Morosini, L. Garcia, S. Alberti, M. T. Coque, R. Canton, J. Clin. Microbiol. 48, 4089 (2010)
C. Thornsberry, in Manual of clinical microbiology, 4th edn., ed by E. Lennette, A. Balows, W. Hausler, H. Shadomy. Automated procedures for antimicrobial susceptibility tests (American Society for Microbiology, Washington, DC, 1985), p. 1015
Acknowledgments
Funding was provided in part by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (1R01AI101446).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Campbell, J., McBeth, C., Kalashnikov, M. et al. Microfluidic advances in phenotypic antibiotic susceptibility testing. Biomed Microdevices 18, 103 (2016). https://doi.org/10.1007/s10544-016-0121-8
Published:
DOI: https://doi.org/10.1007/s10544-016-0121-8