Abstract
Tuberculosis (TB) is a major global health problem, and multi-drug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) are spreading throughout the world. However, conventional drug susceptibility test (DST) methods, which rely on the detection of the colony formation on a solid medium, require 1–2 months to the result. A rapid and accurate DST is necessary to identify patients with drug-resistant TB and treat them with appropriate drugs. Here, we used microscopic imaging of Mycobacterium tuberculosis (MTB) immobilized in an agarose matrix for a rapid DST. The agarose matrix, which was molded in a microfluidic chip, was inoculated with MTB, and TB drugs in liquid culture medium diffused throughout the agarose to reach the MTB immobilized in the agarose matrix. After the responses of MTB to drugs were tracked with an automated microscopic system, an image-processing program automatically determined the susceptibility and resistance of MTB to specific doses of TB drugs. The automatic DST system was able to assess the drug susceptibility of various drug-resistant clinical TB strains within 9 days with an accuracy comparable to that of conventional method. Our rapid DST method based on microscopic time-lapse imaging greatly reduces the time required for a DST and can be used to rapidly and accurately treat TB patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) is a grave infectious disease that threatens the health of overall world’s population. Specifically, each year, approximately 1 % of the world’s population is newly infected with TB and 1.3 million people die of the disease despite the availability of anti-TB agents (WHO 2014). Moreover, the incidences of multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) are gradually increasing due to the poor management of suspected or confirmed TB patients (Gandhi et al. 2010). Recently, the first cases of totally drug-resistant TB (TDR-TB) developed in Iran (Velayati et al. 2009). To reduce the transmission of TB and improve outcomes for TB patients, a DST that facilitates rapid and accurate treatment is required. Identifying ineffective anti-TB agents to Mycobacterium tuberculosis (MTB) from patients is important to detect MDR-TB, XDR-TB, and TDR-TB and avoid treatment failure.
After sputum culture on solid or liquid media, the MTB stock was prepared from the MTB colony on the solid media or liquid media. The stock is inoculated on the test well with TB drugs (Chegou et al. 2011). Common DST methods are based on cell culture on solid and liquid media. For the solid medium culture method, a solid medium containing TB drug is inoculated with MTB, and macroscopic colony formation is monitored thereafter (Heifets and Cangelosi 1999). This conventional DST method takes at least 3–6 weeks because MTB grows very slowly (its cell dividing time is approximately 24 h) and requires to wait until enough growth of the cells for human naked-eye detection of the colony formation. The use of liquid media accelerates the growth of MTB to reduce the time required for the DST (Cheng et al. 1994). In fact, a representative commercial DST platform using liquid media, the MGIT 960 system, is available (Bemer et al. 2002). This system detects a florescent signal when MTB grows and consumes oxygen and determines the drug susceptibility (Siddiqi et al. 2012).
Alternatively, MTB can be directly screened using the microscopic observation drug susceptibility (MODS) method (Caviedes et al. 2000; Moore et al. 2006, 2004). In this method, injection-molded plates inoculated with 7H9 broth and decontaminated sputum is examined by inverted light microscope. Each well is then monitored daily to detect MTB growth (Moore et al. 2006), which yields DST results within 1 week.
Many lab-on-a-chip technologies have been developed to microscopically track bacterial cells (Lindstrom and Andersson-Svahn 2010; Love et al. 2013; Yin and Marshall 2012): an array of micro-scale wells, passive microfluidic trapping, an actively valved microfluidic system, and droplet microfluidics. In the array method using micro-scale wells and passive microfluidic trapping, the cells settle via gravity and are trapped in the wells by fluid flow (Jin et al. 2009). However, the difficulty associated with controlling the fluidic environment hinders multiplex assays for drug testing. To better control cell and drug loading, actively valved microfluidics employs a computer-controlled, pneumatically actuated trapping method to precisely control small quantities of liquids via multiple control elements. However, this approach relies on complex control, which is associated with high costs and operating efforts. Therefore, this method is not applicable for routine clinical drug testing. To test various concentrations of antibiotics in one device with high-resolution imaging, a microfluidic linear gradient 3D culture device was developed (Hou et al. 2014). Droplet microfluidics can generate a sufficiently chamber number for multiplexing drug tests (Guo et al. 2012). However, these methods do not ensure the immobilization of bacterial cells in the liquid, which is necessary for tracking specific cells.
In this study, an automated microscopic imaging system of bacteria immobilized in agarose matrix was used for a rapid DST. We have already developed a rapid antimicrobial susceptibility test (AST) platform for common bacteria (Choi et al. 2013, 2014) but could not perform the requisite long incubation for MTB DSTs. Golchin et al. developed a microfluidic based system using hydrogel for fixation of MTB for a rapid DST of mycobacteria (Golchin et al. 2012). However, the throughput of this test is limited by the syringe pump-based fluidic control and fluorescent imaging. To rapidly screen MTB for drug susceptibility, we developed a chamber consisting of a thin layer of agarose containing MTB cells. To immobilize the MTB, agarose was used as a cell-fixing material, which produced a 3D culture niche. The culture medium and drugs diffuse into the agarose matrix, and the MTB cells are tracked using time-lapse microscopic imaging. The side surface of the thin layer is exposed to allow liquid culture media and drugs to be supplied to the cells. The size of the culture medium reservoir is sufficient for dryness prevention during long-term incubation. An automated imaging instrument was employed to ensure high throughput, and the acquired images were automatically processed to produce quantitative digital information about MTB growth. Based on the data, the minimum inhibitory concentration (MIC) values of drugs were determined within only 9 days, whereas conventional DST systems on solid media require approximately 4–6 weeks to provide the same data (Fig. 1a, b). The clinical strain test indicated that the Disc Agarose Channel (DAC) system can be used to rapidly and accurately carry out DSTs.
Comparison of the conventional DST method and the rapid DST based on microscopic tracking of MTB cells in the agarose matrix. a The conventional DST method based on naked-eye detection. The method takes approximately 4–6 weeks to obtain DST results. b Rapid DST based on microscopic tracking in agarose matrix. This method requires 9 days to produce DST results. c 24-well poly(methyl methacrylate) (PMMA) chip and its top-view. Food dye was used for visualization of agarose loading
Materials and methods
Chemicals
Agarose (Seakem® LE agarose, Lonza, Rockland, ME, USA) was used as a fixing material in this research. The agarose solution was mixed with a stock solution of TB, which posed a risk of heat shock if a high-temperature agarose solution was used. To reduce this risk, an agarose concentration of 0.5 % was used because this concentration is sufficiently low to prevent solidification at 37 °C. The liquid state 0.5 % agarose is mixed with MTB stock solution as 3:1 in volume and the final 0.375 % agarose mixture is loaded into the chip. Additionally, lower concentrations of agarose enhance the diffusion of the culture medium and drug. The drugs used for the DST were purchased from Sigma-Aldrich. The liquid culture medium was Middlebrook 7H9 broth (BBL, BD Franklin Lakes, NJ, USA) supplemented with 10 % oleic albumin dextrose catalase (OADC) (BBL, BD Franklin Lakes, NJ, USA).
Strains
The standard strain, M. tuberculosis H37Rv, and clinical strains, Pan-susceptible, MDR, and XDR-TB, were obtained from the Korean Institute of Tuberculosis. The primary drug susceptibility pattern of the clinical strains was provided in Table S1∼S3. The MTB strains were pre-cultured on Löwenstein-Jensen (LJ) medium until there were several colonies for a DST process.
DST using LJ proportion method
The LJ proportion DST is used as a standard method. MTB stock of McFarland 1.0 was prepared from LJ media and was used to inoculate both the drug-free and drug-containing media. All tested DST were then incubated at 37 °C for 4∼8 weeks. After examination of colony formation by naked-eye detection, susceptibility was defined as the drug concentration on which 1 % proportion growth was found, while confluent growth was observed on the drug-free medium. Critical concentrations of the LJ proportion DST are 0.2 μg/ml for isoniazid, 40.0 μg/ml for rifampin, 2.0 μg/ml for ethambutol, and 4.0 μg/ml for streptomycin (Kam et al. 2010).
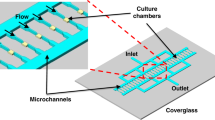
Design and fabrication of Disc Agarose Channel chip
For the microscopic time-lapse imaging of TB, a test chip was necessary to immobilize the TB in agarose to ensure the sufficient delivery of drugs and optical transparency. To satisfy these requirements, a new chip, the Disc Agarose Channel (DAC) chip, was designed and fabricated (Fig. 1c). The DAC chip consists of a disc-shaped channel, which was loaded with the agarose and TB mixture. The chip also features structures to enhance the diffusion of the culture medium and drugs, such as wells that contain culture medium or drug, open spaces, and holes. The depth of the disc-shaped channel (300 μm) was determined by the height of a spacer. The thickness of the disc-shaped channel is important because the diffusion lengths of culture media and drug are limited in a hydrogel. Based on a previous study, we determined that 300 μm is sufficiently thin to deliver culture media and drug to TB in agarose (Choi et al. 2014). TB DSTs require a long incubation time, which is limited by the supply of culture medium. However, the use of a syringe pump to supply medium is inconvenient and limits the throughput of the system. Therefore, the size of each well was the same as that of a single well in a 24-well plate. Specifically, the diameter of the well is 12.4 mm, and the height of the well is 12 mm. The wells contained approximately 0.5 ml of medium, which is suitable for more than 1 month of incubation. The fabrication of chips using PDMS limits the dimensions of the chip, and the manufacturing throughput is low. Therefore, injection molding was used to fabricate the DAC chip. After designing the chip using a 3D design tool (SolidWorks®, Dassault Systèes SolidWorks Corp.), the aluminum mold was machined. Poly(methyl methacrylate) (PMMA) was used to generate the chips. After the fabrication of chips, a polycarbonate film was bonded to the bottom of the chip using the pressurized solvent-bonding method (80 % of ethanol and 20 % of 1,2-dichloroethane in weight, Sigma-Aldrich, St. Louis, MO, USA). The chip was then subjected to O2 plasma treatment to ensure hydrophilicity. The chip was then treated with gamma rays for 5 h for sterilization.
DST process
TB stock solutions were prepared by collecting colonies from LJ medium using a sterilized loop. The aggregated colonies were dispersed in a U-shaped bottom tube by vortexing with 2-mm-diameter glass beads. Due to safety concerns, the vortexed tube was allowed to rest for 15 min. After stabilization, 7H9 medium containing 10 % OADC was added to the tube. By using spectrophotometer, we adjusted the MTB concentration of stock as McFarland Turbidity Standard No. 1.5–3.0 and there were approximately 107 CFU/ml of MTB. The 300 μl of stock solution was mixed with 900 μl of 0.5 % agarose at 37 °C by vortexing. Subsequently, a 40 μl of 0.375 % agarose mixture with TB stock was loaded into the inlet of DAC chip (Fig. 2a, b). The agarose was then allowed to solidify at room temperature for 1 min. A 0.5-ml aliquot of 7H9 containing 10 % OADC and TB drugs was then added to the DAC chip (Fig. 2c). The drug in the culture medium was then allowed to diffuse into the agarose. After this process, the DAC chip was then sealed by an air-permeable film to prevent the evaporation of the culture medium and incubated in a temperature-controlled culture chamber at 37 °C. The 0.375 % agarose matrix is stable during the incubation because the melting point of the agarose is higher than 70 °C. One area at the edge of the agarose was imaged with a ×20 lens on an inverted microscope every other day using the time-lapse method (Fig. 2d). These procedures were all carried out on biological safety cabinet.
Rapid DST experimental procedures using a DAC chip. a Empty DAC chip. b Loaded MTB cells mixed with liquid agarose at 37 °C. c Loaded liquid medium containing drug. d Diffusion of drug and culture medium. e Time-lapse imaging of standard strain, M. tuberculosis H37Rv, in 7H9 broth media. The scale bar represents 10 μm
Result
A 3D culture formation chip for the DST of MTB
In this study, agarose was used as a 3D culture matrix for the DST of MTB. A stable 3D culture matrix was necessary for the long-term incubation of MTB. To ensure a uniform supply of liquid culture medium and drug, the agarose matrix was properly formed in the mold. To visualize the formation of the agarose matrix, a 0.5 % agarose mixture containing food dye at a ratio of 3 (food dye):1 (agarose) by volume was loaded into the chip and imaged (Fig. 3a). The agarose matrix was well formed on the DAC chip. To verify the stability of the agarose matrix, the MTB cells were cultured in the agarose matrix, whose structure was maintained sufficiently to track specific cells for 13 days (Fig. 3b).
a Loading of agarose mixture on DAC chip. The scale bar represents 1 mm. b Long-term incubation of MTB on DAC chip. For 13 days of incubation, the MTB cells were well immobilized in an agarose matrix. The red rectangle represents the imaging region for the DST. The scale bar represents 0.1 mm. c Diffusion of antibiotics into agarose. After 1 μg/ml rhodamine B was loaded, fluorescent images a, b, c, and d in the region of the red rectangle in Fig 3a were taken 0, 10, 30, and 60 min in sequence. The exposure time was 0.1 s. The scale bar represents 1 mm
Diffusion characteristics in the DAC chip
Agarose was used to fix the MTB strains. The TB drugs were dissolved in a liquid medium, 7H9 broth, to be delivered to the MTB strains embedded in the agarose matrix. The diffusion characteristics of agarose have been previously reported (Fatin-Rouge et al. 2004; Liang et al. 2006a; Stickle et al. 1984). In this work, the concentration of drugs at the corner of the DAC chip (the imaging area) needed to be uniform to ensure accurate DST results. Using Fick’s law, the time (T) required for a molecule to diffuse to the imaging area (1200 μm from reservoir) was calculated.
D is the diffusion constant of a molecule in the media and d is the diffusion distance. The diffusion coefficient of penicillin (MW, 313 g/mol) in 2 % agarose at 37 °C is approximately 30,000 μm2/min. Drugs diffuse in the imaging area for approximately 12 min. Agarose (0.5 %) was mixed with liquid medium to a final concentration of 0.375 %, and drugs will diffuse faster in this matrix than in the 2 % agarose matrix. Oxygen gradient is generated in agarose matrix, and the oxygen concentration at 1 mm from the source was about 10 % of source in 2 % agarose (Oppegard and Eddington 2013). We used 0.5 % agarose before mixing with MTB stock solution, and the final concentration of agarose was 0.375 %. In that concentration, the oxygen concentration would be higher than 2 %. Also, due to the air-permeable film, oxygen can be solved in the liquid culture media and sufficient oxygen is supplied continuously. In case of culture media, there is protein substance with high molecular weight oleic acid (282.46 Da), bovine albumin (67 kDa), dextrose (180.16 Da), and catalase (250 kDa). Even in those cases, the total diffusion time is calculated less than 10 min (Liang et al. 2006b). Because the dividing time of MTB is approximately 20–24 h, the drug distribution in the agarose matrix is sufficient for the DST. Rhodamine B (molecular weight, 479.02 g/mol) was used to visualize the diffusion characteristics of the agarose matrix in the DAC chip because its molecular weight is similar to that of the TB drugs (isoniazid, 137.139; rifampicin, 822.94; and ethambutol, 204.31 g/mol). The chips were treated with 1 μg/ml of these molecules and imaged at 0, 10, 30, and 60 min to assess the uniformity of diffusion (Fig. 3d). The fluorescent signal became uniform within 60 min of loading the fluorescent dye, implying that this system is suitable for a DST (considering the cell division of MTB, which is approximately 20–24 h).
Microscopic tracking of MTB cells in the DAC chip
Conventional DST methods rely on the measurement of MTB growth via the macroscopic observation of colony formation on a solid medium or on indirect fluorescence-based detection methods that measure oxygen consumption in liquid medium (MGIT 960 system). In this study, MTB growth under various drug conditions was tracked using microscopic imaging by automated imaging device (×20 lens, QuantaMatrix Inc.). The MTB cells on the DAC chip were tracked every other day for 9 days (Fig. 2e). One imaging area (1126.4 μm × 594 μm) contained many different sizes of TB because the MTB cells were prepared from colonies (the big cluster form) on solid medium.
Structure and operation of experiment automation device
The automated microscopic system consists of an array rack that contains up to 24 plates, a barcode reader, a robot arm, a thermostat system for maintaining the chamber at 37 °C, and an imaging device, as shown in Fig. 4a, b. The robot arm unloads a plate from the array rack, and the barcode reader identifies the information, such as starting date of the DST experiment, the concentration profiles of drugs, and clinical samples. The plate is then loaded into an imaging device, which finds the focus marker to align the x-, y-, and z-axes. The design of the focus marker is shown in Fig. 4c and features a rectangle for x- and z-axis alignment. The alignment of the y- and y-axes is facilitated by an image-processing algorithm. The z-axis alignment position is detected when the focus marker is in focus. The focus marker alignment facilitates the alignment of time-lapse images with minimal error, typically within 2 μm. The plate is moved to the imaging location from focus maker aligned position, and images of growing cells are then captured. The robot arm returns the plate back to the array rack after imaging.
Structure of experiment automation device and auto-focusing process. a The automated microscopic system consists of an imaging device, a plate handler, a barcode reader, and a thermostat system. b The components of automated microscopic system. c Auto-focusing process. To track MTB in agarose, the same region on the chip needs to be imaged throughout the incubation. The x- and y-axis features are detected using an image-processing algorithm, and the z-axis is aligned by determining the position at which a focus marker comes into focus. The scale bar represents 0.3 mm
Image processing for automatic susceptibility determination
The conventional DST method on solid medium (LJ medium) relies on the macroscopic assessment of MTB growth by a trained experimenter. Thus, this method is subject to human error. In this study, automatic image processing was employed to determine the drug susceptibility of MTB and avoid human error. The microscopic time-lapse images obtained with a CCD camera were processed to digitalize the MTB growth in response to TB drugs. The image-processing flow consists of the image-processing step and the decision-making step (Fig S1 and S2). The image-processing step includes binarization, noise reduction, and object area calculation (Fig S3∼S18). The decision-making step includes the growth decision and susceptibility decision. The Niblack binarization algorithm is adopted as the binarization process owing to the shadow region on the background (Fig S19∼S22). The close morphology operation is adopted as the noise reduction process in other to remove the small noise areas and fill in the bacillus areas. Although not all black areas represent growing MTB cells because the boundaries of MTB colonies were not clear and the imaging area contained some debris, most black areas were due to the growth of MTB in the agarose matrix and consequently proportional to this parameter. The black area in the images was calculated by counting the pixel number. Using a sequential digital date, proportional growth rate of MTB was plotted as a function of time in Fig. 6. We compared this growth rate with the growth rate of the control to determine the susceptibility of TB strains to various concentrations of TB drugs.
MTB DST using the DAC system
MTB DSTs are based on the estimation of growth of a MTB strain in the presence of a single “critical concentration” of one drug. Typically, the critical concentration of an anti-TB drug indicates clinically relevant resistance if growth is observed, whereas susceptible MTB strains are inhibited at the critical concentration. In the DAC system, the 0.5 % pure agarose was used for only immobilization of MTB and 7H9 medium containing 10 % OADC was supplied as culture media as used in MGIT 960 system. Therefore, In the DAC system, the critical concentration of each anti-TB drug is determined by the critical concentration of the Middlebrook 7H9 broth because the DAC system is more similar to the liquid culture system than the solid culture system using LJ media. After determining the critical concentration of each anti-TB drug, DSTs were conducted using the DAC system at serial twofold concentrations near the critical concentration to determine susceptibility. When the MIC value was at or below the critical concentration, the strain was considered to be susceptible, whereas resistant strains were defined by MIC values that exceed the critical concentration. Specifically, the critical concentration of rifampin against a clinical strain of MTB is 1.0 μg/ml in the DAC system. The DST using the DAC system was performed at the 0 (control), 0.25, 0.5, 1.0, 2.0, and 4.0 μg/ml concentrations of rifampin. To determine the MIC value, images of growing MTB were obtained and processed at each rifampin concentration according to the incubation time (Fig. 5). The proportional growth rate curve was calculated and plotted after image processing (Eq. 1 and Fig. 6).
Time-lapse images and processed images of M. tuberculosis (PanS #2859) treated with rifampin. a Raw growth images of M. tuberculosis at 0, 0.25, 0.5, 1, 2, and 4 μg/ml concentrations of rifampin. b Processed images. In the processed images, the black area represents the area occupied by growing M. tuberculosis colonies
Quantification of growth dynamics of M. tuberculosis (PanS #2859) treated with rifampin. By measuring the growth areas of the M. tuberculosis in the images (Fig. 5), the proportional growth rate of MTB cells was plotted. Growth continued to increase at 0, 0.25, and 0.5 μg/ml, whereas growth was arrested at 1.0, 2.0, and 4.0 μg/ml. Therefore, the MIC value of rifampin against M. tuberculosis was determined to be 1.0 μg/ml in the DAC system
A t and A 0 are the areas of MTB in the image at time t and the initial state (0 h), respectively. At 0, 0.25, and 0.5 μg/ml, growth rate continued to increase, whereas growth was arrested at 1.0, 2.0, and 4.0 μg/ml. Therefore, the MIC value of rifampin against MTB was determined to be 1.0 μg/ml in the DAC system. The MIC value (1.0 μg/ml) was the same as the critical concentration of rifampin (1.0 μg/ml), indicating that this strain was susceptible (Fig. 6). For checking the reproducibility of the method, we performed quality control test three times with a standard strain, M. tuberculosis H37Ra, and a clinical strain, M. tuberculosis KIT 87190. In the three serial tests, the DST results were identical in terms of susceptibility in all four drugs (Table S4 and S5).
Clinical sample test of DAC system
Rapid DSTs are an urgent public health diagnostic need due to the increasing number of confirmed and suspected MDR, XDR, and TDR-TB patients worldwide. The DAC system provides an opportunity for rapid DST. To validate the use of the DAC system for rapid DST in a clinical setting, the susceptibilities of ten clinical PanS (all susceptible), nine MDR, and nine XDR-TB strains to several primary anti-TB drugs, such as isoniazid, rifampicin, streptomycin, and ethambutol, were determined. The critical concentrations of isoniazid, rifampicin, streptomycin, and ethambutol are 0.1, 1.0, 1.0, and 5.0 μg/ml, respectively. A conventional LJ culture DST was used as the gold standard, and it took 4–6 weeks to produce DST results. The DST results of the DAC system were compared with those of the LJ culture DST. In the DAC system, the images of all tested strains were taken at the same position every other day for 9 days using the time-lapse method. The images were processed, and the time-lapse data were plotted to determine the MIC values of the four anti-TB drugs, which were compared with results from the LJ culture-based DST (Tables 1 and 2). The corresponding error rates were then calculated. Specifically, the DAC system did not produce any error for the PanS and MDR-TB strains, whereas four discrepancies were noted for the XDR-TB strain, resulting in an error rate of 88.9 %. The total agreement rate for all strains was 96.4 % in the DAC system.
Furthermore, isoniazid and rifampin did not produce error in the DAC system, whereas streptomycin yielded an agreement rate of 88.9 % (specificity) and 90.0 % (sensitivity) between the DAC and conventional system for susceptible and resistant strains, respectively. The total agreement rate was 89.3 %. Therefore, 18.2 % of resistant cases may be susceptible to streptomycin. In this study, the drug susceptibility was determined based on the MIC value using the critical concentration used in Middlebrook 7H9 broth. We plan to improve the accuracy of our system by determining its specific critical concentration. For ethambutol, the DAC and conventional systems showed an agreement rate of 92.3 % (specificity) and 100.0 % (sensitivity) for susceptible and resistant strains, respectively. The total agreement was 96.4 %. Based on these results, the DAC system can reliably reduce the time to detection to 9 days and produce accurate results to diagnose susceptible and resistant cases of TB.
Discussion
To rapidly identify appropriate drugs for infectious disease, we have developed a rapid antimicrobial susceptibility test (RAST) system with fast-growing bacteria (Choi et al. 2013, 2014). However, the RAST system was not suitable for slow-growing bacteria because the liquid medium in the culture chamber evaporated within a few days, which destabilized the agarose matrix on the chip. Therefore, we needed to develop a new system for DST with slow-growing bacteria, namely the DAC system. The volume of liquid medium in the DAC chip is sufficient to ensure the stability of the agarose matrix for several weeks. Specifically, DAC system is a DST platform that tracks the growth of MTB in the agarose matrix using a microscope. This DST method is capable of reducing the time of DST. To track the growth of MTB cells under a microscope, the cells need to be immobilized and have access to a stable supply of cell culture medium. Agarose has been proven to be a biocompatible material that facilitates the diffusion of culture media. Therefore, this material was selected for 3D culture. The immobilized MTB cells proliferated in agarose, as observed under a microscope with time-lapse imaging.
We propose that the DAC system is similar to liquid medium culture systems due to the pure agarose for immobilization of MTB and liquid culture media, 7H9, with 10 % OADC. In the liquid culture system, the growth of MTB is accelerated (Moore et al. 2004). The MODS detects the growth of MTB using microscopic observation. However, individual cells cannot be easily tracked in the liquid culture system because the cells are not immobilized and of non-uniform distribution of MTB in liquid state, which requires to scan whole well and produces inevitable errors in the determined MTB growth. Therefore, we immobilized MTB cells with agarose for tracking the growth of MTB without compromising the growth rate in liquid media. The imaging time for one test well is less than 10 s, and there were no errors from the failure from tracking MTB.
In this study, the MTB cells in the agarose matrix were obtained from pre-cultured colonies on LJ medium. An automated liquid culture system, the BD MGIT 960, was used to culture the sputum of TB system because this type of culture requires only 2 weeks, whereas the LJ culture system usually takes 4 to 6 weeks. The MTB-positive samples from the MGIT 960 system can be used in the DAC DST system. If the DAC DST system is integrated with the MGIT culture system, DST results can be obtained from patient sputum within 2 or 3 weeks (1 or 2 weeks for MGIT culturing and 9 days for DST using the DAC system). Thus, this approach is much faster than the conventional system, which requires 4 to 12 weeks for sputum culture and DST (Fig. 7).
In this study, only primary drugs were tested. However, the DAC system can be easily expanded to examine primary and secondary drugs. The DAC system is currently being automated with an image-acquiring and image-processing program for use in clinical areas. This automated DAC system may facilitate the identification of effective drugs within 1 week, which will increase the cure rate. This rapid and accurate DST will increase the cure rate of TB and ultimately help to reduce the spread of resistant TB.
In summary, the growth tracking of MTB using a microscope in an agarose matrix rapidly produced DST results in 9 days. The agarose matrix provided a 3D culture environment that is suitable for MTB culture and obtaining DST results with a microscopic imaging method. The standard strains, including all susceptible, MDR, and XDR strains, were tested using a DAC platform, which produced data comparable to those obtained using conventional methods. Thus, the DAC system is a rapid and accurate DST platform that may help reduce global health problems related to MTB.
References
Bemer P, Palicova F, Rüsch-Gerdes S, Drugeon HB, Pfyffer GE (2002) Multicenter evaluation of fully automated BACTEC Mycobacteria Growth Indicator Tube 960 system for susceptibility testing of Mycobacterium tuberculosis. J Clin Microbiol 40:150–154. doi:10.1128/jcm.40.1.150-154.2002
Caviedes L, Lee TS, Gilman RH, Sheen P, Spellman E, Lee EH, Berg DE, Montenegro-James S (2000) Rapid, efficient detection and drug susceptibility testing of Mycobacterium tuberculosis in sputum by microscopic observation of broth cultures. The Tuberculosis Working Group in Peru. J Clin Microbiol 38:1203–1208
Chegou NN, Hoek KG, Kriel M, Warren RM, Victor TC, Walzl G (2011) Tuberculosis assays: past, present and future. Expert Rev Anti-Infect Ther 9(4):457–469. doi:10.1586/eri.11.23
Cheng A, Li M, Chan C, Chan C, Lyon D, Wise R, Lee J (1994) Evaluation of three culture media and their combinations for the isolation of Mycobacterium tuberculosis from pleural aspirates of patients with tuberculous pleurisy. J trop med and hyg 97:249–253
Choi J, Jung Y-G, Kim J, Kim S, Jung Y, Na H, Kwon S (2013) Rapid antibiotic susceptibility testing by tracking single cell growth in a microfluidic agarose channel system. Lab Chip 13:280–287
Choi J, Yoo J, Lee M, Kim E-G, Lee JS, Lee S, Joo S, Song SH, Kim E-C, Lee JC, Kim HC, Jung Y-G, Kwon S (2014) A rapid antimicrobial susceptibility test based on single-cell morphological analysis. Sci Transl Med 6:267ra174. doi:10.1126/scitranslmed.3009650
Fatin-Rouge N, Starchev K, Buffle J (2004) Size effects on diffusion processes within agarose gels. Biophys J 86:2710–2719
Gandhi NR, Nunn P, Dheda K, Schaaf HS, Zignol M, Van Soolingen D, Jensen P, Bayona J (2010) Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global control of tuberculosis. Lancet 375:1830–1843
Golchin SA, Stratford J, Curry RJ, McFadden J (2012) A microfluidic system for long-term time-lapse microscopy studies of mycobacteria. Tuberc 92:489–496. doi:10.1016/j.tube.2012.06.006
Guo MT, Rotem A, Heyman JA, Weitz DA (2012) Droplet microfluidics for high-throughput biological assays. Lab Chip 12:2146–2155
Heifets L, Cangelosi G (1999) Drug susceptibility testing of Mycobacterium tuberculosis: a neglected problem at the turn of the century State of the Art. Int J of Tuberc and Lung Dis 3:564–581
Hou Z, An Y, Hjort K, Hjort K, Sandegren L, Wu Z (2014) Time lapse investigation of antibiotic susceptibility using a microfluidic linear gradient 3D culture device. Lab Chip 14:3409–3418. doi:10.1039/C4LC00451E
Jin A, Ozawa T, Tajiri K, Obata T, Kondo S, Kinoshita K, Kadowaki S, Takahashi K, Sugiyama T, Kishi H, Muraguchi A (2009) A rapid and efficient single-cell manipulation method for screening antigen-specific antibody-secreting cells from human peripheral blood. Nat Med 15:1088–1092 doi:http://www.nature.com/nm/journal/v15/n9/suppinfo/nm.1966_S1.html
Kam KM, Sloutsky A, Yip CW, Bulled N, Seung KJ, Zignol M, Espinal M, Kim SJ (2010) Determination of critical concentrations of second-line anti-tuberculosis drugs with clinical and microbiological relevance. Int J Tuberc Lung Dis 14:282–288
Liang S, Xu J, Weng L, Dai H, Zhang X, Zhang L (2006a) Protein diffusion in agarose hydrogel in situ measured by improved refractive index method. J Control Release 115:189–196. doi:10.1016/j.jconrel.2006.08.006
Liang S, Xu J, Weng L, Dai H, Zhang X, Zhang L (2006b) Protein diffusion in agarose hydrogel in situ measured by improved refractive index method. J Control Release 115:189–196. doi:10.1016/j.jconrel.2006.08.006
Lindstrom S, Andersson-Svahn H (2010) Overview of single-cell analyses: microdevices and applications. Lab Chip 10:3363–3372. doi:10.1039/C0LC00150C
Love KR, Bagh S, Choi J, Love JC (2013) Microtools for single-cell analysis in biopharmaceutical development and manufacturing. Trends Biotechnol 31:280–286. doi:10.1016/j.tibtech.2013.03.001
Moore DA, Evans CA, Gilman RH, Caviedes L, Coronel J, Vivar A, Sanchez E, Pinedo Y, Saravia JC, Salazar C, Oberhelman R, Hollm-Delgado MG, LaChira D, Escombe AR, Friedland JS (2006) Microscopic-observation drug-susceptibility assay for the diagnosis of TB. N Engl J Med 355:1539–1550. doi:10.1056/NEJMoa055524
Moore DAJ, Mendoza D, Gilman RH, Evans CAW, Delgado MGH, Guerra J, Caviedes L, Vargas D, Ticona E, Ortiz J, Soto G, Serpa J, Tuberculosis Working Grp in P (2004) Microscopic observation drug susceptibility assay, a rapid, reliable diagnostic test for multidrug-resistant tuberculosis suitable for use in resource-poor settings. J Clin Microbiol 42:4432–4437. doi:10.1128/jcm.42.10.4432-4437.2004
Oppegard SC, Eddington DT (2013) A microfabricated platform for establishing oxygen gradients in 3-D constructs. Biomed Microdevices 15:407–414. doi:10.1007/s10544-013-9737-0
Siddiqi S, Ahmed A, Asif S, Behera D, Javaid M, Jani J, Jyoti A, Mahatre R, Mahto D, Richter E, Rodrigues C, Visalakshi P, Rusch-Gerdes S (2012) Direct drug susceptibility testing of Mycobacterium tuberculosis for rapid detection of multidrug resistance using the Bactec MGIT 960 system: a multicenter study. J Clin Microbiol 50:435–440. doi:10.1128/JCM.05188-11
Stickle DF, Lauffenburger DA, Zigmond SH (1984) Measurement of chemoattractant concentration profiles and diffusion coefficient in agarose. J Immunol Methods 70:65–74
Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, ZiaZarifi AH, Hoffner SE (2009) Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in Iran. Chest 136:420–425. doi:10.1378/chest.08-2427
WHO (2014) Global tuberculosis report. World Health Organization, Geneva, Switzerland
Yin H, Marshall D (2012) Microfluidics for single cell analysis. Curr Opin Biotechnol 23:110–119. doi:10.1016/j.copbio.2011.11.002
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding information
This work was supported by the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (grant numbers HI13C1468 and HI13C0866); the Institute for Basic Science (IBS) in Korea; the Pioneer Research Center Program through the NRF of Korea funded by the Ministry of Science, ICT & Future Planning (NRF-2012-0,009,555), an NRF grant funded by the Korean Government (2012M3A9B2030170); and the Nano Material Technology Development Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (2012M3A7A9671610).
Conflict of interest
J. Yoo, E.-G. Kim., K.O. Park, Y.-G. Jung, and S. Kwon at the submission of the paper were employed at QuantaMatrix Inc., which is commercializing the rapid DST technology. J. Yoo, E.-G. Kim., K.O. Park, Y.-G. Jung, and S. Kwon have equity interest in QuantaMatrix Inc.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Jungil Choi, Jungheon Yoo, and Ki-jung Kim contributed equally to this work
Electronic supplementary material
ESM 1
(PDF 865 kb)
Rights and permissions
About this article
Cite this article
Choi, J., Yoo, J., Kim, Kj. et al. Rapid drug susceptibility test of Mycobacterium tuberculosis using microscopic time-lapse imaging in an agarose matrix. Appl Microbiol Biotechnol 100, 2355–2365 (2016). https://doi.org/10.1007/s00253-015-7210-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-015-7210-0