Summary
Osteoporosis is a frequent disease in postmenopausal women. Despite the fact that fragility fractures cause many problems, osteoporosis is still underdiagnosed and undertreated. This manuscript outlines the topics diagnosis of osteoporosis, fracture risk prevention, and therapy after fracture. Regular physical activities, a sufficient intake of calcium, and a normal vitamin D level are important for bone health. Depending on the personal fracture risk, the patient may also be prescribed bone-specific medication to prevent fragility fractures. In case of a prevalent osteoporotic fracture, the initiation or adaptation of bone-specific therapy is indispensable. Since most osteoporotic fractures occur during a fall, fall risk reduction is an important measure to inhibit a new fracture. Rehabilitation of patients with fragility fractures varies with different localizations of the fracture and should be performed by a multidisciplinary team.
Zusammenfassung
Osteoporose ist eine häufige Erkrankung bei Personen fortgeschrittenen Alters, speziell bei postmenopausalen Frauen. Trotz der Häufigkeit und Probleme, die Fragilitätsfrakturen verursachen, bleibt die Erkrankung oft unerkannt und Betroffene werden nicht therapiert. Dieses Manuskript beschäftigt sich mit der Diagnose der Osteoporose, mit Frakturprävention und Therapien nach einer Fraktur. Regelmäßige körperliche Aktivitäten, eine ausreichende Kalziumzufuhr und normale Vitamin D Spiegel sind für einen gesunden Knochen wichtig. In Abhängigkeit vom Frakturrisiko können dem Patienten auch knochenspezifische Medikamente verschrieben werden. Im Falle einer Fragilitätsfraktur muss unbedingt die entsprechende Therapie begonnen oder eine laufende Therapie optimiert werden. Da es zu den meisten osteoporotischen Frakturen im Rahmen eines Sturzes kommt, ist die Sturzrisikoreduktion ein wesentlicher Bestandteil der primären und sekundären Frakturprävention. Die spezifische Rehabilitation ist von der Lokalisation der Fraktur abhängig und wird am besten von einem multidisziplinären Team durchgeführt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is defined as a “systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture” [1]. The clinical manifestation of osteoporosis is the occurrence of fractures. One in three women and one in five men over the age of 50 years are predicted to suffer a fracture [2] leading to limitations in quality of life [3]—to pain, morbidity, and increased mortality. The probability of fracture varies between countries [4, 5], but because of the growing elderly population, osteoporotic fractures are a worldwide problem, and the economic burden increases exponentially.
A clinician’s aim is to inhibit fragility fractures and associated problems. Unfortunately, osteoporosis is often underdiagnosed, and sometimes even patients with fragility fractures have not been treated with a disease-specific medication. Up to half of the women reporting a previous hip or spine fracture did not receive disease-specific treatment [6]. The first step to prevent fragility fractures is to increase the percentage of diagnosed osteoporotic patients.
Diagnosis of osteoporosis and fracture risk assessment
A detailed history may help to identify risk factors for osteoporosis. Potential causes for secondary osteoporosis are endocrine disorders, hypogonadism, inflammatory disease, bone marrow disorders, immobilization, malabsorption, low body weight, defective synthesis of connective tissue, or regular intake of drugs with negative effect on bone metabolism (Fig. 1). A clinical examination is indispensable. It may reveal an abnormal high decrease of height compared to young age, an increased kyphosis with fir tree phenomenon, or the typical “osteoporosis-tummy”; all are indicators of possible vertebral fractures.
Diagnosis is verified by bone mineral density (BMD) measurement. Measuring areal BMD by dual energy X-ray absorptiometry (DXA) is the method of choice for diagnosis of osteoporosis. The amount of mineralized bone mass is expressed as a T-score, and the cut-off point for osteoporosis is a T-score of 2.5 standard deviations (SDs) below the mean BMD at the spine or at the hip of a healthy female population aged 30 years [7]. At least two intact vertebral bodies are necessary to give clear information on the lumbar spine. Concerning the hip, three areas—“femoral neck”, “trochanter”, or “total”—may be chosen. X-ray images are usually taken to identify morphological changes of the skeleton as well as calcified vessels or lymph nodes to enhance the diagnostic accuracy of the DXA measurement. Volumetric BMD measurement with quantitative computed tomography (QCT) has the advantage of giving information on trabecular and cortical bone and not being falsified by calcified vessels or other tissue nearby. Since vertebral fractures do not necessarily hurt, X-ray images are crucial for detection of vertebral fractures. Quantitative assessment of bone mass has been proven to be a strong predictor of fragility fractures, but macro- and microarchitecture of bone, material properties, microdamage, and bone turnover are also essential.
Analysis of biochemical parameters ascertains the etiology of the disease—the differentiation between primary and secondary osteoporosis. Bone turnover markers (BTMs) are circulating components of bone metabolism and give a hint concerning the individual’s fracture risk. Evaluation of BTMs when initiating bone-specific therapy is helpful in deciding which kind of treatment regimen should be started. Analysis of BTMs, especially during the early phase of treatment, may be useful for treatment monitoring [8]. Biomarkers of bone formation are bone alkaline phosphatase (BALP), osteocalcin, and the N-terminal propeptide of type I collage (P1NP). Biomarkers of bone resorption are C-terminal cross-linked collagen type I peptide (CTX) and tartrate-resistant acid phosphatase (TRAP) 5b. Cathepsin K as well as receptor activator of nuclear factor kappa-B (RANK), RANK ligand (RANKL), and its decoy receptor osteoprotegerin are only used for scientific purposes.
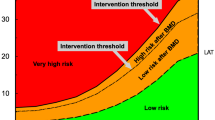
In addition to BMD measurement and analysis of BTMs, web-based tools may also be helpful in fracture risk prediction for individual patients. Very popular is the World Health Organization (WHO)-sponsored tool FRAX (http://www.shef.ac.uk/FRAX/). It is a country-specific calculator [9] which includes 12 different risk factors and can also be used without knowledge of BMD. The individual’s risk of an osteoporotic or a hip fracture within the following 10 years is calculated.
Prevention of fragility fractures
Up to the age of 20–30 years, bone mass increases. After reaching the peak bone mass, bone adapts to biomechanical demands and depends on calcium homeostasis as well as hormonal factors, diseases, and medical therapies affecting bone turnover. Since osteoporosis is a multifactorial disease, osteoporosis therapy and fracture prevention also have to be multifactorial.
Prevention starts already at a very young age. During childhood the main goal is to increase bone mass. Since bone surfaces are covered with a greater proportion of active osteoblasts during growth than after skeletal maturity [10], exercise is especially effective during childhood. We know that exercise has long-lasting effects on bone integrity because a high physical fitness level in young adulthood reduces the risk of fractures later in life [11]. A 10 % increase in peak bone mass cuts the future risk of osteoporotic fractures in half [12]. Along with regular physical activities, a sufficient calcium intake with nutrition which should increase with increasing age is recommended.
Even though exercise has less effect on bone mass when grown up, small but probably important increases may be reached [13]. The higher the exercises’ impact on bone, the more effective they are. A 16-weeks-lasting jump training, for instance, improved hip BMD in premenopausal women [14]. A meta-analysis showed that even walking as a singular exercise therapy performed for more than 6 months has positive effects on femoral neck BMD in peri- and postmenopausal women [15]. A multimodal exercise program, which aimed to ameliorate muscle strength, BMD, and balance, proved to be especially reasonable in elderly subjects [16]. Regular bone loading also has a benefit on bone geometry [17] and, thus, reduces the risk of fragility fractures.
Aside from regular physical activities, daily intake of milk products and a sufficient vitamin D level are modifiable lifestyle factors which have a protective effect on bone health. If a sufficient intake with nutrition is not possible or sun exposure not enough, there is the option to substitute calcium as well as vitamin D. For maintenance of musculoskeletal integrity, the European Society for Clinical Aspects of Osteoporosis and Osteoarthritis (ESCEO) recommends postmenopausal women a daily dietary protein intake of 1.0–1.2 g per kilogram bodyweight, the intake of 800 IU vitamin D, and 1000 mg calcium as well as regular physical activities three to five times a week [18]. Caffeine, nicotine, and a high intake of ethanol should be avoided.
An important point in fracture prevention is the prevention of falls because above the age of 65 years, about 30 % of self-dependent elderly and half of those living in residential care facilities or nursing homes fall at least once a year; the percentage increases further with increasing age, and about half of the fallers are recurrent fallers [19]. Most falls are of multifactorial origin, endogenous and exogenous risk factors being responsible for the fall. Except for most of the vertebral fractures, the nature of an accidental fall is an essential part concerning the risk of a fragility fracture. A fracture occurs if the applied load during the impact of the fall is higher than the structural capacity of the bone (Fig. 1). According to the American Geriatrics Society, persons over the age of 65 years should be screened for falls or risk for falling. The algorithm is shown on the Internet page www.americangeriatrics.org.
Prevention of fragility fractures |
|---|
Regular physical activities/exercise |
Sufficient calcium intake and vitamin D level, possibly substitution |
Bone-specific medication (depending on fracture risk) |
Rehabilitation of fragility fractures
Rehabilitation after vertebral fractures
Acute vertebral fractures may cause rest pain and an even higher pain during movement. If that is the case, pain reduction is the primary aim of rehabilitation. Because of potential side effects, pharmaceuticals should be used at a low dose and as short as possible. Electrotherapy is another option of pain management reducing the need of analgesics [20] and keeping the patient independent and mobile. Osteoporosis-related kyphosis leads to many problems including balance abnormalities [21] and consequently an increased risk of falling. That may be counteracted by strengthening the back muscles [22, 23]. Additionally, progressive back-strengthening exercise increases back extensor strength and BMD while reducing the incidence of further vertebral fractures [24]. A multicomponent exercise program that includes resistance and balance training, emphasizing a daily training of spinal extensors, is recommended for individuals with osteoporosis; of course, impairments, fracture risk, and activity history have to be taken into consideration [25]. Wearing a functional orthosis for a 6-month period seems to reduce pain and to increase trunk muscle strength [26]. In case of persisting pain after vertebral fracture despite pain management, vertebro- or kyphoplasty may be a therapeutic option. A meta-analysis showed that compared to conservative treatment, surgical treatment is more effective in decreasing pain in the short, mid and long term, but a significant difference in physical function and quality of life is not observed [27]. In a patient with prevalent fragility fracture, an osteoporosis-specific medication has to be initiated. We distinguish antiresorptive from anabolic therapy and from medication with a dual mode of action (Table 1). Oral bisphosphonates are the first-line treatment option for postmenopausal osteoporosis. They reduce the risk of vertebral and hip fracture by about half [28]. The parenteral bisphosphonate zoledronic acid reduces the cumulative incidence of hip fractures by 41 %, the clinical vertebral fractures by 77 %, and the non-vertebral fractures by 25 % compared to placebo within 3 years [29]. Selective estrogen receptor modulators reduce the risk of vertebral fractures by about 30 % [30]. The human monoclonal antibody to the RANKL denosumab reduces the risk of vertebral (relative decrease of 68 %), non-vertebral (relative decrease of 29 %), and hip fractures (relative decrease of 40 %) in postmenopausal osteoporotic women [31]. An advantage of denosumab is that it is a treatment option in patients with chronic kidney disease. The only anabolic therapy is the daily injection of 20 μg parathyroid hormone (PTH). It increases intracortical remodelling and endocortical bone mass. After the 2-years-lasting PTH therapy, a consolidating therapy with an antiresorptive agent is necessary. Vertebral (RR 0.35) and non-vertebral fractures (RR 0.47) are reduced after a median treatment period of 21 months [32]. Even after cessation of PTH therapy, fracture rate reduction is continued. The efficacy of strontium ranelate has also been shown [33]. However, according to the European Medicines Agency’s Committee for Medical Products for Human Use, because of an increased risk of myocardial infarction, strontium ranelate should only be used to treat severe osteoporosis in postmenopausal women and men at high risk of fracture for whom treatment with other medicinal products approved for the treatment of osteoporosis is not possible. It must not be used in patients with ischaemic cardiac disease, peripheral arterial obstruction disease, cerebrovascular disease, or uncontrolled hypertension. Of course, all medications’ contraindications and adverse effects have to be checked before initiating bone-specific medication. Especially because of potential negative side effects of long-term bisphosphonate therapy, concerns on optimal treatment duration have been raised. In general, a 3–5-years-lasting therapy is suggested, and continuation of bone-specific therapy is only indicated in patients with persisting high risk of fragility fractures [34].
Rehabilitation of vertebral fractures |
|---|
Pain management |
Strength training |
Functional orthosis |
Kyphoplasty/vertebroplasty |
Bone-specific medication |
Rehabilitation after hip fracture
Fractures of the hip region have to be operated on as soon as possible. Since nourishment is often not balanced in elderly subjects, it is important to pay attention to a high-protein diet, enriched with minerals and vitamins [35]. After surgery, rehabilitation should start more or less immediately. Early mobilization (within 24 h) may prevent complications such as deep vein thrombosis. The best strategies for enhancing mobility after hip surgery are not known [36], but strengthening exercises of the knee extensors—started as soon as 2.5 days after surgery—have been shown to be feasible and effective, increasing knee extensor strength [37]. After progressive strength training—initiated 3 weeks after hip fracture surgery—improvements in functional outcome like the “timed up and go” and 6-min walk test were observed [38].
Since 90 % of all hip fractures occur during a fall, fall risk reduction is a very important part of rehabilitation in these patients. According to a systematic review [39], group and home-based exercise programs as well as home safety modification reduce the rate of falls and risk of falling. Multifactorial interventions directed towards the individual’s risk reduce the rate of falls. Supplementation with vitamin D is only effective in subjects with a low vitamin D level. Exercise programmes designed to prevent falls in older adults also seem to prevent injuries caused by falls, including fractures [40]. After hip surgery, multidisciplinary care in a geriatric ward significantly reduces the rate of falls. In care facilities, vitamin D supplementation and multifactorial interventions are beneficial; exercise only lessens falls in people who have a relatively low demand of care [41].
The aim of hip protectors is to decrease the risk of hip fracture despite a sideways fall. While hitting the ground, the impact on bone is supposed to be reduced. However, studies in which randomization was performed on an individual basis did not reveal an efficacy of hip protectors in preventing hip fractures [42]. The reason for failure may be that these protectors were often not worn while falling.
Of course, a patient who has had a hip fracture needs a bone-specific medication. If he/she has already been on such a therapy, the regimen has to be adapted/optimized. It is important to treat patients on an individual basis taking into account the patient’s risk of fracture [43].
Rehabilitation after hip fracture |
|---|
Postoperative mobilization |
Fall risk reduction, including exercise |
Hip protector |
Bone-specific medication |
Conclusion
Osteoporosis is a systemic skeletal disease associated with an increased risk of fragility fracture leading to pain, morbidity, and risk of mortality. Thus, prevention of the first fragility fracture or subsequent osteoporotic fracture is the clinician’s primary aim. Despite the fact that peak bone mass is to a high amount genetically determined, lifestyle factors also have an important effect on bone health. Parents should have their children’s sufficient intake of milk products and regular physical activities in mind. In adults, besides a calcium intake of 1000 mg per day and an adequate vitamin D level, regular bone loading is recommended. In case of the occurrence of fragility fractures, a specific rehabilitation has to be initiated. After vertebral fracture maintenance of mobility—if necessary with use of pain killers—strengthening of back muscles in order to ameliorate postural stability and reduce the risk of falling, probably the use of orthoses and, of course, the initiation or adaptation of bone-specific medication are in the foreground. Hip fractures are the most-affecting osteoporotic fractures. After surgery, patients have to be mobilized as soon as possible. The aim is to regain the general state of health as soon as possible. Fall risk reduction and initiation of bone-specific therapy are indispensable. The best way of rehabilitation is the rehabilitation performed by a multiprofessional team.
Conflict of interest
The author declares that there are no actual or potential conflicts of interest in relation to this article.
References
Consensus development conference. prophylaxis and treatment of osteoporosis. Am J Med. 1991;90:107–10.
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl 2):S3–7.
Kerschan-Schindl K, Patsch J, Kudlacek S, Gleiss A, Pietschmann P. Measuring quality of life with the German Osteoporosis Quality of Life Questionnaire in women with osteoporosis. Wien Klin Wochenschr. 2012;124:532–7.
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probably of fracture worldwide. Osteoporos Int. 2012;23:2239–56.
Borgström F, Lekander I, Ivergard M, Ström O, Svedborn A, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Kallikorm R, Lesnyak O, McCloskey E, Nassonov E, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson AN, Jönsson B, Kanis JA. The international costs and utilities related to osteoporotic fractures study (ICUROS)-quality of life during the first 4 months after fracture. Osteoporos Int. 2013;24:811–23.
Díez-Pérez A, Hooven FH, Adachi JD, Adami S, Anderson FA, Boonen S, et al. Regional differences in treatment for osteoporosis. The Global Longitudinal Study of Osteoporosis in Women (GLOW). Bone. 2011;49:493–8.
Kanis JA, Melton J III, Christiansen C, et al. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–41. (Perspective)
Bieglmayer C, Dimai HP, Gasser RW, et al. Biomarkers of bone turnover in diagnosis and therapy of osteoporosis: a consensus advice from an Austrian working group. Wien Med Wochenschr. 2012;162:464–77.
Kanis JA, Oden A, Johnell O, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–46.
Seeman E. Pathogenesis of bone fragility in women and men. Lancet. 2002;359:1841–50.
Nordström P, Sievänen H, Gustafson Y, Pedersen NL, Nordström A. High physical fitness in young adulthood reduces the risk of fractures later in life in men: a nationwide cohort study. J Bone Miner Res. 2013;28:1061–7.
Bonjour JP, Chevalley T, Rizzoli R, Ferrari S. Gene-environment interactions in the skeletal response to nutrition and exercise during growth. Med Sport Sci. 2007;51:64–80.
Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011; CD000333.
Tucker LA, Strong JE, LeCheminant JD, et al. Effect of two jumping programs on hip bone mineral density in premenopausal women: a randomized controlled trial. Am J Health Promot. 2015;29:158–64.
Ma D, Wu L, He Z. Effects of walking on the preservation of bone mienral density in perimenopausal and postmenopausal women: a systematic review and meta-analysis. Menopause. 2013;20:1216–26.
Gianoudis J, Bailey CA, Ebeling PR, et al. Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Miner Res. 2014;29:182–91.
Wilks DC, Winwood K, Gilliver SF, Kwiet A, Chatfield M, Michaelis I, Sun LW, Ferretti JL, Sargeant AJ, Felsenberg D, Rittweger J. Bone mass and geometry of the tibia and the radius of master sprinters, middle and long distance runners, race-walkers and sedentary control participants: A pQCT study. Bone. 2009, 91–97.
Rizzoli R, Stevenson JC, Bauer JM, et al. The role of dietary protein and vitamin D in maintaining musculoskeletal health in postmenopausal women: a consensus statement from the European Society for Clinical and economic aspects of Osteoporosis and Osteoarthritis (ESCEO). Maturitas. 2014;79:122–32.
Kannus P, Palvanen M, Jarvinen T, Pakkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366:1885–93.
Zambito A, Bianchini D, Gatti D, Rossini M, Adami S, Viapiana O. Interferential and horizontal therapies in chronic low back pain due to multiple vertebral fractures: a randomized, double blind, clinical study. Osteoporos Int. 2007;18:1541–5.
Sinaki M, Breay RH, Hughes CA, Larson DR, Kaufman KR. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporos Int. 2005;16:1004–10.
Itoi E, Sinaki M. Effect of back-stengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69:1054–9.
Lynn SG, Sinaki M, Westerlind KC. Balance characteristics of persons with osteoporosis. Arch Phys Med Rehabil. 1997;78:273–7.
Sinaki M, Itoi E, Ahner HW, Wollan P, Gelzcer R, Mullan BP, Collins DA, Hodgson SF. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002;30:836–41.
Giangregorio LM, McGill S, Wark JD, Laprade J, Heinonen A, Ashe MC, MacIntyre NJ, Cheung AM, Shipp K, Keller H, Jain R, Papaioannou A. Too fit to fracture: outcomes of a Delphi consensus process on physical activity and exercise recommendations for adults with osteoporosis with or without vertebral fractures. Osteoporos Int. 2015;26:891–910.
Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthesis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83:177–86.
Guo JB, Chen BL, Xie B, Zhang WY, Yang YJ, Wang XQ. Surgical versus non-surgical treatment for vertebral compression fracture with osteopenia: a systematic review and meta-analysis. PLoS One. 2015;10:e0127145.
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR, Fracture Intervention Trial. Fracture risk reduction with alendronate in women with osteoporosis: the fracture intervention trial. J Clin Endocrinol Metab. 2000;85:4118–24.
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR; HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–22.
Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–45.
Cummings SR, Martin JS, Mc Clung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65.
Neer R, Arnaud CD, Zanchettta JR, et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41.
Meunier PJ, Roux C, Seeman E, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350:459–68.
Kerschan-Schindl HJ, Obermayer-Pietsch B, Gasser RW, Dimai HP, Fahrleitner-Pammer A, Dobnig H, Roschger P, Preisinger E, Klaushofer K, Resch H, Pietschmann P. How long should women with postmenopausal osteoporosis be treated with a bisphosphonate? Horm Metab Res. 2013;45:621–8.
Pfeifer M, Minne H. Musculoskeletal rehabilitation after hip fracture: a review. Arch Osteoporos. 2010;5:49–59.
Handoll HH, Sherrington C, Mak JC. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev. 2011;16(3):CD001704.
Kronborg L, Bandholm T, Palm H, Kehlet H, Kristensen MT. Feasibility of progressive strength training implemented in the acute ward after hip fracture surgery. PLoS One. 2014;9:e93332.
Overgaard J, Kristen MT. Feasibility of progressive strength training shortly after hip fracture surgery. World J Orthop. 2013;18:248–58.
Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;12:CD007146.
El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f6234.
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions in preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465.
Gillespie WJ, Gillespie LD, Parker MJ. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev. 2010;6(10):CD001255.
Kerschan-Schindl K, Mikosch P, Obermayer-Pietsch B, Gasser RW, Dimai HP, Fahrleitner-Pammer A, Dobnig H, Roschger P, Preisinger E, Klaushofer K, Resch H, Pietschmann P. Current controversies in clinical management of postmenopausal osteoporosis. Exp Clin Endocrinol Diabetes. 2014;122:437–44.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kerschan-Schindl, K. Prevention and rehabilitation of osteoporosis. Wien Med Wochenschr 166, 22–27 (2016). https://doi.org/10.1007/s10354-015-0417-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-015-0417-y