Abstract
Purpose
Recurrence is a concerning area in pediatric inguinal hernia repair. Various laparoscopic repair methods are available to treat recurrent pediatric inguinal hernia. We analyzed previous laparoscopic hernia repairs and report the outcomes of laparoscopic inguinal hernia reoperations in patients with recurrent inguinal hernia.
Methods
Fifty-one patients who presented for recurrent inguinal hernia after laparoscopic hernia repair from September 2012 to May 2017 were retrospectively evaluated. Previous laparoscopic procedures were analyzed with respect to sac removal (removal vs. leaving in place), suture material (absorbable vs. nonabsorbable), and high ligation method (purse string vs. multiple stitches). We removed the hernia sac from all patients and performed suture repair of the muscular arch of the internal inguinal ring using nonabsorbable material.
Results
All patients (38 male, 13 female) had indirect inguinal hernias. No conversion to open surgery occurred. Forty-three (84.3%) patients developed recurrence within 1 year after the previous operation [mean 8.7 ± 6.9 (range 3–33) months]. Twenty patients had concurrent hydroceles (39.2%); 16 were cord hydroceles and 4 were canal of Nuck hydroceles. In the previous operations, the hernia sac was not removed in 100% (51/51) of patients, absorbable suture material was used in 58.8% (30/51), and purse string high ligation was performed in 88.2% (45/51). No re-recurrence developed during a mean follow-up of 25.0 ± 12.6 (range 13–54) months.
Conclusion
Laparoscopic reoperation with hernia sac removal and suture repair of the muscular arch of the internal inguinal ring with nonabsorbable material is an effective operation with few recurrences and complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical management of pediatric recurrent inguinal hernia (PRIH) is always challenging. Unlike recurrent inguinal hernia in adults, no general guidelines are available for reoperation of PRIH. In adults, the current guidelines recommend a laparoscopic operation using large-size mesh for the treatment of recurrent inguinal hernias originally repaired by a primary open approach, and an open approach for the treatment of recurrent adult inguinal hernias originally repaired by a primary laparoscopic operation [1,2,3,4]. Two standard methods are used: transabdominal preperitoneal patch plasty and total extraperitoneal patch plasty [5].
Many reports have described the results of primary laparoscopic surgery for pediatric inguinal hernia (PIH) [6,7,8] and successful treatment of recurrent hernias using laparoscopic procedures [9,10,11,12]; nevertheless, no general guidelines are available for the treatment of PRIH. The various techniques used to date have differences in the hernia sac removal technique, suture material, and high ligation method [7, 8, 13]. The recurrence rate after laparoscopic primary PIH repair reportedly ranges from 0.68 to 4.00% [14]. The re-recurrence rate after a laparoscopic reoperation reportedly ranges from 8 to 19% in adult inguinal hernias [2]. However, few data are available on the re-recurrence rate after laparoscopic reoperations in PRIH. The re-recurrence rate after a laparoscopic reoperation for PRIH is reportedly lower than that in adults [11, 12]. To the best of our knowledge, few reports have described the results of re-laparoscopic repair after primary laparoscopic PIH repair. In this study, we analyzed the technical details that could contribute to recurrence in previous operations. We evaluated a laparoscopic hernia reoperation technique involving hernia sac removal with multiple stitches using nonabsorbable suture material for treating patients with PRIH who had previously undergone laparoscopic hernia repair.
Methods
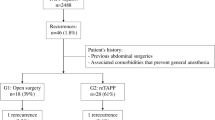
We retrospectively analyzed the case records of 51 patients who presented with PRIH from September 2012 to May 2017 at Damsoyu Hospital, Seoul, Republic of Korea. Patients who developed recurrence after surgery in another hospital and patients who developed recurrence after surgery in our hospital were included in the study. Each patient’s history and surgical method were confirmed by checking the medical records obtained from the facility at which the initial procedure had been performed. All data were retrospectively collected by a data manager working at the Damsoyu Hospital research center. The previous laparoscopic procedures were analyzed with respect to removal of the hernia sac (removal vs. leaving in place), suture material (absorbable vs. nonabsorbable) (Fig. 1a, b), and high ligation method (purse string vs. multiple stitches) (Fig. 1c, d).
Laparoscopic hernia repair technique
Laparoscopic PRIH repair was performed using a three-port technique with high ligation. The laparoscopy system included a 3.0-mm camera and 3.0-mm instruments. The operation was performed with the patient in the supine position under general anesthesia. A transumbilical 3.0-mm incision was made, and a 3.0-mm trocar was used to create carbon dioxide pneumoperitoneum that was maintained at 6–8 mmHg. The other 3.0-mm instruments were inserted through separate 3.0-mm stab incisions on the lateral abdomen.
Recurrence sites were observed with a laparoscopic camera. The loosened peritoneum (hernia sac) was incised at the lateral site of the entrance of the internal inguinal ring and entirely removed. When hydroceles of the spermatic cord or canal of Nuck were present, hydrocelectomy was performed simultaneously (Fig. 2). If a previous tie was present, it was removed (Fig. 3a, b). The vas deferens and gonadal vessels were preserved separately from the sac (Fig. 3c). The muscular arch suture technique using nonabsorbable 3–0 silk was previously reported [15], and the procedures are shown in Fig. 3. The first stitch was used to tie the lateral and medial muscular arch of the internal inguinal ring with a space for the vas deferens and gonadal vessels to pass through without compression (Fig. 3d, e). The first stitch was a suture of the iliopubic tract and the medial muscular arch of the internal inguinal ring, avoiding the triangle of pain and triangle of doom (Fig. 3f). After the first stitch, the muscular arch of the internal inguinal ring suture continued without contact with the iliopubic tract (Fig. 3g). Suture of the muscular arch was performed to prevent damage to the femoral branch of the genitofemoral nerve and to reduce tension. The peritoneum was then closed in the downward direction (Fig. 3h).
Reoperation of a right inguinal recurrent hernia. a Previous nonabsorbable suture material. b Removal of previous stitch. c Complete removal of hernia sac. Preservation of the vas deferens (white arrow) and gonadal vessels (black arrow). d First stitch of the iliopubic tract (white arrow). e Suturing of the medial side of the muscular arch of the internal inguinal ring (white arrow). f Sufficient space for the vas deferens (white arrow) and gonadal vessels (black arrow) before the first knot. Intact triangle of pain (white triangle) and triangle of doom (black triangle). g Complete repair of the muscular arch of the internal inguinal ring. h Closure of the peritoneum
Protocols and follow-up
Liquid ingestion and lactation were permitted after 2 h of observation. The protocol at our institution stipulates that the patient can be discharged if their condition remains stable and they feel comfortable while performing daily activities such as walking and eating. Routine outpatient follow-up included a physical examination after 1 week and 1 year. After 1 year, we conducted a telephone interview without follow-up and then conducted annual telephone follow-ups in December every year until June 2018. The follow-up period was 13–54 months. Telephone interviews were performed to obtain information on the postoperative status (such as pain and recurrence). Outpatient follow-up included routine questions apart from the information obtained from the retrospective chart review.
Statistical methods
All statistical analyses were performed using R software version 3.3.2 (R Development Core Team, Vienna, Austria, http://www.R-project.org). Continuous variables are presented as mean and standard deviation. Categorical variables are presented as frequency and percentage.
Results
Patient characteristics
The patients’ characteristics are shown in Table 1. All patients had previously undergone laparoscopic hernia repair. The total number of patients with PRIH was 51, and their mean age was 40.7 ± 33.0 (range 6–156) months. Thirty-eight patients were male and 13 were female. There were 30 right hernias, 20 left hernias, and 1 bilateral hernia. Of all 51 patients, 43 were undergoing their second operation, 5 were undergoing their third operation, and 3 were undergoing their fourth operation. All patients had an indirect inguinal hernia. Forty-three patients developed recurrence within 1 year after the previous operation, and the mean recurrence period was 8.7 ± 6.9 (range 3–33) months.
Details of previous laparoscopic operations
The detailed techniques of the previous laparoscopic operations are shown in Table 2. With respect to the hernia sac treatment method, the sac was removed in no patients (0%); it was left in place in all patients (100%). With regard to suture material, 30 (58.8%) patients were treated with absorbable suture material and 21 (41.2%) were treated with nonabsorbable suture material. In terms of the suture method, 45 (88.2%) patients were treated by purse string sutures and 6 (11.8%) were treated by multiple stitches.
Outcomes of laparoscopic reoperation
The outcomes of the laparoscopic reoperation are shown in Table 3. The mean operation time was 18.6 ± 8.6 (range 10–60) minutes. Twenty hernias were accompanied by hydroceles (39.2%); 16 were cord hydroceles and 4 were canal of Nuck hydroceles. The postoperative complications comprised two scrotal hematomas, one inguinal seroma, one umbilical port site infection, and one case of urinary retention, all of which subsided with conservative treatment. No re-recurrence was observed during a mean follow-up period of 25.0 ± 12.6 (range 13–54) months.
Discussion
Technical guidelines are available for treating recurrent adult inguinal hernia, and these guidelines recommend the use of large-size mesh [16]. In the treatment of adult recurrent inguinal hernia, a laparoscopic operation is recommended for hernias originally repaired by a primary open approach, and an open approach is recommended for those originally repaired by a primary laparoscopic operation [1,2,3,4]. However, few technical guidelines or recommended surgical procedures are available for the treatment of PRIH. Successful treatment of PRIH by a laparoscopic reoperation was recently reported [9,10,11,12]. Because laparoscopic PRIH reoperation has a limitation in mesh use, which differs from adult hernia repair, detailed techniques are important. Hernia sac disconnection and nonabsorbable suture material reportedly reduce the recurrence rate after primary PIH repair [6], and placement of multiple sutures is reportedly associated with a lower recurrence rate than the use of purse string sutures [7]. One study showed that closure of the muscular arch of the internal inguinal ring reduces recurrence in adolescent primary inguinal hernia repair [15]. During reoperation, closure of the muscular arch of the internal inguinal ring can reportedly reduce recurrence [11].
Laparoscopic PIH repair is usually performed by two methods: intracorporeal high ligation and percutaneous high ligation. The reported recurrence rates associated with these two methods are 0.4–3.7% and 0.0–15.5%, respectively [17,18,19]. Hernia sac treatment can be performed using various intracorporeal suture techniques: complete peritoneal disconnection surgery, surgical hernia sac removal, and high ligation without treatment of the hernia sac [20]. The reported recurrence rate associated with each method is 0.00% (0/80) [6], 0.53% (2/375) [21], and 2.60% (2/77) [6], respectively. The recurrence rate was low in previously reported sac disconnection or removal surgery. In the present study, the hernia sac was left in place in all previous laparoscopic operations. In terms of the suture method, the recurrence rate associated with purse string sutures is 0.94–2.40%, and that associated with multiple stitches is 0.08–3.76% [6, 7, 22]. In another study, the recurrence rate when using absorbable vs. nonabsorbable suture material was 5.0% and 3.8%, respectively [23, 24]. The reported rate of hydrocele occurrence after laparoscopic PIH repair is 19% [6, 25]. Leaving the hernia sac in place may cause hydrocele formation [26]. In this study, reoperation was performed with removal of the hernia sac. Although one seroma occurred, no hydroceles developed. The inguinal seroma was resolved by conservative treatment.
All cases of PRIH in this study were lateral (indirect), similar to the findings in other studies [9]. In one report, the recurrence rate was lower when performing hernia sac disconnection than when leaving the hernia sac intact [6]. There is a risk of injury to the vas deferens and gonadal vessels when removing the hernia sac [27, 28]. We encountered no intraoperative major bleeding or vas deferens injury due to removal of the peritoneum while pulling the vas deferens and gonadal vessels to the inferomedial side. Other studies have indicated that the use of nonabsorbable sutures [24], multiple stitches [7], and suture repair of the muscular arch of the internal inguinal ring [15] were associated with a lower recurrence rate than the use of absorbable sutures, purse string sutures, and high ligation, respectively.
Pain assessment is difficult in pediatric patients. In one study of adolescent patients with inguinal hernias, there was no difference in pain between the patients who did and did not undergo muscular arch suturing [15]. Surgery to suture the muscular arch to the iliopubic tract has also been reported, but there was no mention of pain [11]. The entry point of the femoral branch of the genitofemoral nerve was in the caudal location of the inguinal ligament in 84.0% of patients and in the medial direction in the anterior superior iliac spine in 5.2% [29].
In the present study, five patients underwent a third operation and three patients underwent a fourth operation. Unlike adult laparoscopic hernia repair, pediatric laparoscopic hernia repair does not involve the use of synthetic mesh. No mesh adhesion or anatomical transformation occurred when performing re-laparoscopic repair and no injury to important structures was encountered. All patients who underwent two or more surgeries were referred to our hospital after laparoscopic repair at another hospital, and the re-laparoscopic hernia repairs were not difficult to perform.
This study has several limitations, including its retrospective design. The patients underwent initial PIH repair in various hospitals. Because the follow-up period was not long, longer-term follow-up is required to ascertain the actual recurrence rate. Another limitation is that the telephone interview was performed 1 year after the operation because it is difficult to convince patients and their families to revisit the hospital in the long term after treatment of a benign disease.
Despite the relatively short-term observation period, patients with PRIH who previously underwent laparoscopic surgery encountered no difficulty in laparoscopic reoperation, and the recurrence rate was low. Therefore, an important finding of this study is that laparoscopic reoperation may be considered a priority in the treatment of PRIH after laparoscopic surgery.
In conclusion, this study focused on laparoscopic reoperation for the treatment of PRIH after previous laparoscopic PIH repair. Because of the limitation in the use of synthetic mesh in the treatment of PRIH, technical details are important. The laparoscopic reoperation was safe in patients with PRIH after having undergone a primary laparoscopic procedure. Laparoscopic reoperation for PRIH with hernia sac removal and suture repair of the muscular arch of the internal inguinal ring with nonabsorbable material is an effective operation with few recurrences and complications.
References
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Bisgaard T, Bay-Nielsen M, Kehlet H (2008) Re-recurrence after operation for recurrent inguinal hernia. A nationwide 8-year follow-up study on the role of type of repair. Ann Surg 247:707–711
Kockerling F, Jacob D, Wiegank W, Hukauf M, Schug-Pass C, Kuthe A, Bittner R (2016) Endoscopic repair of primary versus recurrent male unilateral inguinal hernias: are there differences in the outcome? Surg Endosc 30:1146–1155
Kockerling F, Bittner R, Kuthe A, Stechemesser B, Lorenz R, Koch A, Reinpold W, Niebuhr H, Hukauf M, Schug-Pass C (2017) Laparo-endoscopic versus open recurrent inguinal hernia repair: should we follow the guidelines? Surg Endosc 31:3168–3185
Varcus F, Duta C, Dobrescu A, Lazar F, Papurica M, Tarta C (2016) Laparoscopic repair of inguinal hernia TEP versus TAPP. Chirurgia (Bucur) 111:308–312
Abd-Alrazek M, Alsherbiny H, Mahfouz M, Alsamahy O, Shalaby R, Shams A, Elian A, Ashour Y (2017) Laparoscopic pediatric inguinal hernia repair: a controlled randomized study. J Pediatr Surg 52:1539–1544
Lee SR, Choi SB (2017) The efficacy of laparoscopic intracorporeal linear suture technique as a strategy for reducing recurrences in pediatric inguinal hernia. Hernia 21:425–433
Amano H, Tanaka Y, Kawashima H, Deie K, Fujiogi M, Suzuki K, Morita K, Iwanaka T, Uchida H (2017) Comparison of single-incision laparoscopic percutaneous extraperitoneal closure (SILPEC) and open repair for pediatric inguinal hernia: a single-center retrospective cohort study of 2028 cases. Surg Endosc 31:4988–4995
Koivusalo AI (2017) A review of the incidence, manifestation, predisposing factors, and management of recurrent pediatric inguinal hernia. Eur J Pediatr Surg 27:478–483
Shalaby R, Ismail M, Gouda S, Yehya AA, Gamaan I, Ibrahim R, Hassan S, Alazab A (2015) Laparoscopic management of recurrent inguinal hernia in childhood. J Pediatr Surg 50:1903–1908
Shehata SM, ElBatarny AM, Attia MA, El Attar AA, Shalaby AM (2015) Laparoscopic interrupted muscular arch repair in recurrent unilateral inguinal hernia among children. J Laparoendosc Adv Surg Tech A 25:675–680
Chan KL (2007) Laparoscopic repair of recurrent childhood inguinal hernias after open herniotomy. Hernia 11:37–40
Ibrahim MM (2015) Two ports laparoscopic inguinal hernia repair in children. Minim Invasive Surg 2015:821680
Steinau G, Treutner KH, Feeken G, Schumpelick V (1995) Recurrent inguinal hernias in infants and children. World J Surg 19:303–306
Lee SR (2018) Benefits of laparoscopic posterior wall suture repair in treating adolescent indirect inguinal hernias. Hernia 22:653–659
HerniaSurge G (2018) International guidelines for groin hernia management. Hernia 22:1–165
Chan KL, Chan HY, Tam PK (2007) Towards a near-zero recurrence rate in laparoscopic inguinal hernia repair for pediatric patients of all ages. J Pediatr Surg 42:1993–1997
Shehata SM, Attia MA, Attar AAE, Ebid AE, Shalaby MM, ElBatarny AM (2018) Algorithm of laparoscopic technique in pediatric inguinal hernia: results from experience of 10 years. J Laparoendosc Adv Surg Tech A 28:755–759
Chen Y, Wang F, Zhong H, Zhao J, Li Y, Shi Z (2017) A systematic review and meta-analysis concerning single-site laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia and hydrocele. Surg Endosc 31:4888–4901
Lukong CS (2012) Surgical techniques of laparoscopic inguinal hernia repair in childhood: a critical appraisal. J Surg Tech Case Rep 4:1–5
Garcia-Hernandez C, Carvajal-Figueroa L, Suarez-Gutierrez R, Landa-Juarez S (2012) Laparoscopic approach for inguinal hernia in children: resection without suture. J Pediatr Surg 47:2093–2095
Marte A, Sabatino MD, Borrelli M, Parmeggiani P (2009) Decreased recurrence rate in the laparoscopic herniorraphy in children: comparison between two techniques. J Laparoendosc Adv Surg Tech A 19:259–262
Ozgediz D, Roayaie K, Lee H, Nobuhara KK, Farmer DL, Bratton B, Harrison MR (2007) Subcutaneous endoscopically assisted ligation (SEAL) of the internal ring for repair of inguinal hernias in children: report of a new technique and early results. Surg Endosc 21:1327–1331
Grimsby GM, Keays MA, Villanueva C, Bush NC, Snodgrass WT, Gargollo PC, Jacobs MA (2015) Non-absorbable sutures are associated with lower recurrence rates in laparoscopic percutaneous inguinal hernia ligation. J Pediatr Urol 11:275.e1–275.e4
Ein SH, Nasr A, Wales P, Gerstle T (2009) The very large recurrent postoperative scrotal hydrocele after pediatric inguinal hernia repair: a rare problem. Pediatr Surg Int 25:239–241
Tsai YC, Wu CC, Yang SS (2007) Minilaparoscopic herniorrhaphy with hernia sac transection in children and young adults: a preliminary report. Surg Endosc 21:1623–1625
Chowbey PK, Pithawala M, Khullar R, Sharma A, Soni V, Baijal M (2006) Complications in groin hernia surgery and the way out. J Minim Access Surg 2:174–177
Bouchot O, Branchereau J, Perrouin-Verbe MA (2018) Influence of inguinal hernia repair on male fertility. J Visc Surg 155(Suppl 1):S37–S40
Reinpold W, Schroeder AD, Schroeder M, Berger C, Rohr M, Wehrenberg U (2015) Retroperitoneal anatomy of the iliohypogastric, ilioinguinal, genitofemoral, and lateral femoral cutaneous nerve: consequences for prevention and treatment of chronic inguinodynia. Hernia 19:539–548
Acknowledgements
We would like to express our gratitude to staff at the research center of Damsoyu Hospital. We also thank Angela Morben, DVM, ELS, from Edanz Group (http://www.edanzediting.com/ac), for editing a draft of this manuscript.
Funding
The authors have no financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
This study was approved by the Institutional Review Board of Damsoyu Hospital.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual patients or their parents/guardians.
Rights and permissions
About this article
Cite this article
Lee, S.R., Park, P.J. Laparoscopic reoperation for pediatric recurrent inguinal hernia after previous laparoscopic repair. Hernia 23, 663–669 (2019). https://doi.org/10.1007/s10029-018-1840-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1840-y