Abstract
Purpose
Pediatric laparoscopic herniorrhaphy has rare complications, but recurrence might occur. The purpose of this manuscript is to evaluate the efficacy of linear suture technique of laparoscopic pediatric herniorrhaphy in reducing recurrences.
Methods
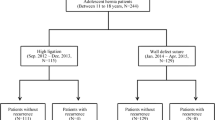
Laparoscopic surgery was performed on 2223 pediatric patients (under 10 years old) from September 2012 to December 2014 in Damsoyu Hospital, Seoul, Republic of Korea. The causes of recurrence were investigated case by case. The patients were categorized into two groups according to the suture method used in closing the hernia orifice: Group 1 (purse-string suture, 1009 patients) and Group 2 (linear suture, 1214 patients).
Results
There were 1413 (63.6%) male and 810 (36.4%) female patients. Mean age was 30.5 ± 29.2 months. A significantly higher proportion of male patients, contralateral patent processus vaginalis, and less proportion of recurrence were observed in Group 2. There were ten cases of recurrence in Group 1 because the internal ring suture could not endure the tension. One recurrence occurred in Group 2. The suture technique and age were found to be a significant risk factor for recurrence. Linear suture technique had a lower recurrence rate (odds ratio = 0.07, with 95% confidence interval 0.01–0.53, and p = 0.004).
Conclusions
Purse-string suture technique causes significantly higher occurrence of hernia recurrences than linear suture technique. Linear suture technique can reduce recurrence by increasing the endurance to tension around the internal ring by distributing pressure to a wider area along the linear suture line. Linear suture technique can effectively reduce recurrence in pediatric inguinal herniorrhaphy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is the most common disease for children who require surgical correction. High ligation of the internal ring has been performed effectively for over 100 years by open method for pediatric inguinal hernia (open herniorrhaphy, OH). Recently, laparoscopic surgery has been expanded to the area of pediatric surgery [1]. In both OH and LH, high ligation is used to close the internal ring. Many centers have reported better surgical outcomes of laparoscopic inguinal herniorrhaphy (LH) than those of OH [2, 3]. Although pediatric herniorrhaphy has rare complications, recurrence might occur. The advantages of LH in comparison to OH include the prevention of metachronous contralateral inguinal hernia (MCIH) and minimal scar formation [4].
There have been various surgical techniques to perform herniorrhaphy in LH [5–10]. The aim of this study is to assess the differences in recurrence rates between the purse-string suture (PSS) and intracorporeal linear suture (ILS) in laparoscopic pediatric inguinal herniorrhaphy and to determine which offers more effective and safer results. Specifically, we present a new technique for hernia repair and compare it with a prior technique of laparoscopic hernia repair for recurrence. The recurrence rate has been reported as 0.8–3.8% in OH [4]. Despite the advantages of LH, other studies have reported that the recurrence of hernia after LH still exists at about 0–5% [11–13]. We focus on the clinical characteristics of recurrence after herniorrhaphy and analyze the risk factors for recurrence. Eventually, we report the proper surgical technique that can effectively reduce recurrence in pediatric herniorrhaphy.
Materials and methods
From September 2012 to December 2014, 2223 pediatric inguinal hernia patients underwent laparoscopic herniorrhaphy in Damsoyu Hospital, Seoul, Republic of Korea. From September 2012 to December 2013, 1009 children underwent LH with the PSS (Group 1). From January 2014 to December 2014, 1214 children underwent LH with the ILS (Group 2). All operations were performed by a highly experienced surgeon (Lee SR, over 1000 laparoscopic operations per year) with 10 years of experience. Patient characteristics, operative findings and outcomes were archived from medical records retrospectively. The following patient data were collected: age, sex, symptoms, location of hernia, bilaterality, types of the herniated organ, operative methods, and operation time. The clinical characteristics and the recurrence of the LH in the PSS group (Group 1) were compared with the LH with the ILS group (Group 2). Patients who required high ligation of contralateral patent processus vaginalis (cPPV) were excluded from the “bilaterality” of hernia, and only symptomatic patients under 10 years old were included in the “bilaterality” of hernia. Therefore, 1009 patients (958 patients with unilateral hernia, and 51 patients with bilateral hernia) with 1060 surgical procedures were included in Group 1. 1214 patients (1153 patients with unilateral hernia, and 61 patients with bilateral hernia) with 1275 surgical procedures were included in Group 2. For the cases that developed recurrence, the cause of recurrence was also investigated.
Surgical procedure
The procedures were performed under general anesthesia in the supine position. For the laparoscopic system, a 2.9 mm camera and 2.7 mm instruments were used. A transumbilical 3 mm incision (by No. 15 scalpel) was used for creation of the pneumoperitoneum via a 3 mm trocar. CO2 pneumoperitoneum was maintained at 4–8 mmHg. Two other 2.7 mm instruments were inserted through separate stab incisions in the lateral abdomen without trocars (Fig. 1).
The suture needle was inserted directly through the lower abdominal area. The internal ring was closed using suture with a non-absorbable multifilament (3.0–4.0 silk). In the PSS group, purse-string suture was placed in the peritoneum at the level of the internal inguinal ring by carefully lifting the peritoneum using an atraumatic 3 mm grasper to prevent injury to the vas deferens and testicular vessels. The knot was tied intracorporeally. On the other hand, the focus of this study is the new high ligation suture method, which we call the “linear suture technique”, because of the linear suture line. We describe the steps in the linear suture technique as follows (Fig. 2). For males, we start suturing by tying around the vas deferens and the cord vessels. We continue to suture to the upper boundary of the internal ring parallel to the inferior epigastric vessel, and continuously without any intermediate tying. Then, we change the direction and suture continuously in the opposite direction until we come back down and tie at the initial knot. For females, initially we tie including the round ligament, and the rest of the suturing both ways is done continuously in the same manner as in males. The knot is tied intracorporeally. The post-suture appearance of the PSS in LH was very similar to that of OH, while the ILS in LH was different from PSS (Fig. 3). After the high ligation, the contralateral processus vaginalis was examined for patency, and if it were open we performed suture at the same time.
Suture procedure of the high ligation of the internal ring. a Purse-string suture. b Linear suture in a male patient. Initially, we tied around the vas deferens and cord vessels. We sutured the upper boundary of the internal ring parallel to the inferior epigastric vessel continuously, and then sutured continuously in the opposite direction until we came back down and tied at the initial knot. c Linear suture in a female patient. Initially, we tied including the round ligament and the rest of the suture and both ways were done continuously in the same way as in males
The dermal bond was used to cover the scar, and therefore no dressing was required after discharge. Food intake was resumed 1 h after the operation, and patients were discharged on the same day.
Telephone follow-ups were performed to check postoperative status such as pain, wound state, possible symptoms of recurrence and complications on day 2, day 7, 3 months afterward and the subsequent year(s). For the cases that developed recurrence, the risk factors for recurrence were carefully investigated.
Statistical methods
All statistical analyses were performed using the SPSS software, version 23.0 for Windows (SPSS Inc; Chicago, Illinois, USA). Continuous variables were presented by mean and standard deviation (SD). Categorical variables were presented by frequency and percentage. The Shapiro–Wilk’s test was used to test for the normality of the continuous variables. Because not all continuous variables were normally distributed, our choice of statistical test of continuous variables was the Mann–Whitney U test. For categorical variables, the Fisher’s exact test or χ 2 test was used. The odds ratios were calculated using the logistic regression. A p value threshold of 0.05 was chosen; any univariate p value below or equal to 0.05 was considered statistically significant.
Results
Clinical characteristics of the patients and comparison between the PSS (Group 1) and ILS (Group 2)
A total of 2223 children with inguinal hernia were operated laparoscopically. The clinical characteristics of these patients are shown in Table 1. There were 1413 (63.6%) male and 810 (36.4%) female patients. The mean age was 30.5 ± 29.2 months. Bilateral symptomatic inguinal hernia excluding cPPV was found in 112 patients (5.0%), and cPPV was observed in 1406 patients (63.2%). Postoperative complication occurred in six patients consistent with a rate of 0.3% as follows: wound hematoma (n = 3), wound seroma (n = 2) and wound infection (n = 1) There was no conversion to open surgery.
Table 2 shows the clinical differences between Group 1 and Group 2. The number of infants under the age of 1 year was 431 (40.7%) in Group 1 and 509 (39.9%) in Group 2; the proportion of infants was statistically similar in the two groups. Patients over the age of 1 year comprised the majority, at about 60%, for both groups (29.0 ± 28.8 vs 31.2 ± 29.5 months, p = 0.735). There were 633 males (60%) and 427 females (40%) in Group 1, and 842 males (66%) and 433 females (34%) in Group 2 (p = 0.002). In Group 1, 51 (5%) patients had bilateral symptoms, 564 (53.2%) had right hernia and 496 (46.8%) had left hernia. In Group 2, 61 (5%) patients had bilateral symptom, 709 (55.6%) had right hernia and 566 (44.4%) had left hernia. The proportions of the bilateral, right, and left hernias did not show significant differences between the two groups. The proportion of the patients who had cPPV was statistically different between the two groups: 57.0% in Group 1 vs. 63.5% in Group 2.
The herniated organs were bowel, omentum, and ovary, and the proportions did not show significant differences between the two groups (p = 0.140). The herniation of the bowel and omentum represented similar proportions around 45%, while the herniation of the ovary accounted for only about 10%, understandably since only female patients are subject to ovary hernia.
The mean operation time was significantly reduced and more consistent in Group 2 (16.1 ± 5.3 vs 12.6 ± 3.7 min, p < 0.001). Recurrence occurred more frequently in Group 1 (n = 10) than Group 2 (n = 1) (p = 0.004). MCIH developed in three patients of Group 1.
Recurrence after LH: comparison between PSS (Group 1) and ILS (Group 2)
The clinical characteristics of patients who had recurrence are shown in Table 3. In Group 1, 10 (8 males and 2 females) of 1060 cases had recurrences (0.94%). The mean recurrence time interval from the date of operation to recurrence was 9.1 ± 4.8 (4–19) months. Most recurrences occurred within 12 months after surgery, although two recurrences occurred at 15 and 19 months, respectively. In Group 2, recurrence occurred in 1 male patient out of 1275 cases (0.08%), and the time interval from the date of operation to recurrence for this patient was 8 months.
The cause of recurrence was investigated carefully for each patient, and in all cases it was due to the tension on the suture line (Fig. 4). In Group 2, one male patient had a recurrence due to the same cause.
Logistic regression test indicated that sex, bilaterality, type of organ, and incarceration were not associated with recurrence. On the other hand, the suture technique and age were found to be a significant risk factor for recurrence. The adjusted odds ratio of linear suture for recurrence was calculated to be 0.07 (p = 0.004). The adjusted odds ratio of infants older than 1 year was 0.20 (p = 0.034) (Table 4).
Discussion
In pediatric herniorrhaphy, high ligation is used for closing the internal ring in open as well as in laparoscopic surgery. The benefit of LH over OH is still controversial, and Alzahem has claimed that he was not able to identify any clear benefit of LH over OH apart from reduction in MCIH development and shorter operative time for bilateral cases [16]. However, the advantages of laparoscopic inguinal herniorrhaphy such as superior cosmetic appearance, low MCIH rate, low injury of vas deferens and cord vessels, and decreased operation time have been reported by many authors [14, 15]. Lee and Liang reported a low recurrence of 0.88% after performing micro-laparoscopic high ligation in 450 patients [15]. Marte et al. also found that the incision of the peritoneum lateral to the internal inguinal ring along with a W-shaped suture, compared to the W-shaped suture alone, is safe and effective in preventing hernia recurrence [17].
While recurrences still occur in OH and LH [18, 19], LH has a low recurrence rate and a low MCIH rate compared to OH [20, 21].This is because the presence of a hernia sac can be monitored thoroughly via the laparoscopic camera. The suture methods of laparoscopic high ligation are intracorporeal suture and percutaneous needle-assisted repair [22, 23].
Various causes of recurrence have been reported; surgeon’s experience, patient’s sex and age, and loosening of the knot are all factors that affect the recurrence rate [23–25]. In our study, under 1 year of age was a significant risk factor for recurrence. Similarly, Treef et al. found that younger children up to the age of 2 years had the highest risk of recurrence [18]. The reason for this may be given as follows. Children under 12 months showed high stretchiness around the internal ring. Purse-string suture restricts the area and, as a result, the tension leads to occasional recurrences. On the other hand, children over 12 months have less flexibility in tissue, and the internal ring is sutured including the transversalis fascia sling medially and the transversalis fascia laterally. Hence, the tissues can hold up much better and the recurrence rate appears to be no different depending on the suture method. In the current study, bowel was the most common organ to be herniated in male infants less than 1-year-old and ovary was the most common organ in female infants less than 1-year-old. Eight of ten patients with recurrence in group 1 had herniated bowels or ovaries. Internal ring stretchiness was seen in recurrence cases and more commonly in patients with prolonged symptoms. Stretchiness seems to be closely related with the long interval between the operation and disease manifestation, and the type of herniated organs. Therefore, high stretchiness in young infants might be the potential reason for the prolonged symptoms resulting in recurrences in infants.
There was a statistically significant difference in gender proportions between Group 1 and Group 2. Male patients tend to have recurrence more frequently than female patients in Group 1 (8 out of 10 patients), although it was not statistically significant in the logistic regression test. However, the more the patients enrolled, the less is the discrepancy of gender distributions expected, generally. However, because this study was conducted based on a retrospective design and enrolled all of the patients who visited one clinic. Gender discrepancy between the two periods could not be explained clearly, and this limitation is inevitable in the retrospective design.
The proportion of cPPV was significantly higher in Group 2. After having the first three MCIH cases in Group 1, to prevent MCIH, a more strict definition of cPPV was applied. At first, if an open tunnel was clearly detected after checking the peritoneal veil covering the internal ring, cPPV was diagnosed and ligated. However, in Group 2, a modified and broadened definition of cPPV was applied including both open tunnels and concave shapes, suggesting the possibility of cPPV. This modified definition seems to be the possible explanation for increased cPPV and decreased MCIH rate in Group 2 compared to Group 1.
In the current study, the suture method was a significant risk factor to affect recurrence. Although many factors can cause recurrence, we hypothesized that one of the causes of recurrence was the tension of the internal ring. In the operative field, the appearances of open herniorrhaphy and laparoscopic herniorrhaphy with PSS are similar as shown in Fig. 3. Based on the appearances, we hypothesized that recurrence was due to the increased tension on the suture line. To disperse the tension, we came up with ILS. The PSS has a point suture tie that receives and concentrates all the pressure, while the linear suture has a long line of suture area. The pressure is distributed along the suture line.
The mean operation time was approximately 16.1 ± 5.3 min in Group 1 and 12.6 ± 3.7 min in Group 2. This reduction in the operation time of 3 min on average was significant (p < 0.001), and the standard deviation in the operation length was also lower for Group 2, meaning that the surgeries using the linear suture method were not only shorter on average but also less variable in length. Because of the surgeon’s enough experience in our study, the recurrence rate was not affected by a surgeon’s learning curve, and that the distinction in operation time clearly reflects the time consumed between two different surgical techniques. The difference in operation time did not affect the recurrence rate according to the logistic regression test.
It should be noted that the follow-up period is different for the two groups in this study, and therefore the patients who underwent surgeries more recently need to be observed for longer periods of time to observe the “true” recurrence rate. However, considering most of the recurrence occurred within 12 months, the follow-up period of the last patient in Group 2 was 15 months at the time of this writing, suggesting that the follow-up period of Group 2 was enough. The effect of the difference in the follow-up period is expected to be minimal.
In conclusion, based on our findings, intracorporeal linear suture technique for internal ring high ligation has shown to significantly reduce the recurrence rate. We addressed the cause of recurrence using the prior suture method and provided a rationale why changing the suture method can reduce the recurrence rate. The linear suture technique does not have any added risk. When performed by an experienced surgeon, the intracorporeal linear suture method is safe and feasible, and could be an optimal and practical choice of treatment for pediatric inguinal hernia.
References
Schier F (2006) Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg 41:1081–1084. doi:10.1016/j.jpedsurg.2006.02.028
Chan KL, Hui WC, Tam PK (2005) Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc 19:927–932. doi:10.1007/s00464-004-8224-3
Wang KS, Committee on F, Newborn AAoP, Section on Surgery AAoP (2012) Assessment and management of inguinal hernia in infants. Pediatrics 130:768–773. doi:10.1542/peds.2012-2008
Schier F, Montupet P, Esposito C (2002) Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg 37:395–397
Boo YJ, Han HJ, Ji WB, Lee JS (2012) Laparoscopic hernia sac transection and intracorporeal ligation show very low recurrence rate in pediatric inguinal hernia. J Laparoendosc Adv Surg Tech A 22:720–723. doi:10.1089/lap.2012.0040
Abraham MK, Nasir AA, Puzhankara R, Abdur-Rahman LO, Viswanath N, Kedari P, Sudarshan B (2012) Laparoscopic inguinal hernia repair in children: a single-centre experience over 7 years. Afr J Paediatr Surg 9:137–139. doi:10.4103/0189-6725.99400
Chang YT, Lin JY, Lee JY, Tsai CJ, Chiu WC, Chiu CS (2012) Comparative mid-term results between inguinal herniotomy and single-port laparoscopic herniorrhaphy for pediatric inguinal hernia. Surg Laparosc Endosc Percutan Tech 22:526–531. doi:10.1097/SLE.0b013e3182680842
Guner YS, Emami CN, Chokshi NK, Wang K, Shin CE (2010) Inversion herniotomy: a laparoscopic technique for female inguinal hernia repair. J Laparoendosc Adv Surg Tech A 20:481–484. doi:10.1089/lap.2009.0169
Molina Vazquez ME, Sanchez Abuin A, Aguilar Cuesta R (2012) Laparoscopic assisted percutaneous treatment of inguinal hernia in infants. Cir Pediatr 25:4–8
Lee DY, Baik YH, Kwak BS, Oh MG, Choi WY (2015) A purse-string suture at the level of internal inguinal ring, taking only the peritoneum leaving the distal sac: is it enough for inguinal hernia in pediatric patients? Hernia 19:607–610. doi:10.1007/s10029-015-1348-7
Crankson SJ, Al Tawil K, Al Namshan M, Al Jadaan S, Baylon BJ, Gieballa M, Ahmed IH (2015) Management of inguinal hernia in premature infants: 10-year experience. J Indian Assoc Pediatr Surg 20:21–24. doi:10.4103/0971-9261.145440
Sulkowski JP, Cooper JN, Duggan EM, Balci O, Anandalwar SP, Blakely ML, Heiss K, Rangel S, Minneci PC, Deans KJ (2015) Does timing of neonatal inguinal hernia repair affect outcomes? J Pediatr Surg 50:171–176. doi:10.1016/j.jpedsurg.2014.10.035
Clarke S (2010) Pediatric inguinal hernia and hydrocele: an evidence-based review in the era of minimal access surgery. J Laparoendosc Adv Surg Tech A 20:305–309. doi:10.1089/lap.2010.9997
Alzahem A (2011) Laparoscopic versus open inguinal herniotomy in infants and children: a meta-analysis. Pediatr Surg Int 27:605–612. doi:10.1007/s00383-010-2840-x
Saranga Bharathi R, Arora M, Baskaran V (2008) Pediatric inguinal hernia: laparoscopic versus open surgery. JSLS 12:277–281
Lee Y, Liang J (2002) Experience with 450 cases of micro-laparoscopic herniotomy in infants and children. Pediatric Endosurgery Innov Tech 6:25–28
Marte A, Sabatino MD, Borrelli M, Parmeggiani P (2009) Decreased recurrence rate in the laparoscopic herniorraphy in children: comparison between two techniques. J Laparoendosc Adv Surg Tech A 19:259–262. doi:10.1089/lap.2008.0292
Treef W, Schier F (2009) Characteristics of laparoscopic inguinal hernia recurrences. Pediatr Surg Int 25:149–152. doi:10.1007/s00383-008-2305-7
Postlethwait RW (1985) Recurrent inguinal hernia. Ann Surg 202:777–779
Yang C, Zhang H, Pu J, Mei H, Zheng L, Tong Q (2011) Laparoscopic vs open herniorrhaphy in the management of pediatric inguinal hernia: a systemic review and meta-analysis. J Pediatr Surg 46:1824–1834. doi:10.1016/j.jpedsurg.2011.04.001
Shalaby R, Ibrahem R, Shahin M, Yehya A, Abdalrazek M, Alsayaad I, Shouker MA (2012) Laparoscopic hernia repair versus open herniotomy in children: a controlled randomized study. Minim Invasive Surg 2012:484135. doi:10.1155/2012/484135
McClain L, Streck C, Lesher A, Cina R, Hebra A (2015) Laparoscopic needle-assisted inguinal hernia repair in 495 children. Surg Endosc 29:781–786. doi:10.1007/s00464-014-3739-8
Wolak PK, Patkowski D (2014) Laparoscopic inguinal hernia repair in children using the percutaneous internal ring suturing technique—own experience. Wideochir Inne Tech Maloinwazyjne 9:53–58. doi:10.5114/wiitm.2014.40389
Shalaby R, Ismail M, Samaha A, Yehya A, Ibrahem R, Gouda S, Helal A, Alsamahy O (2014) Laparoscopic inguinal hernia repair; experience with 874 children. J Pediatr Surg 49:460–464. doi:10.1016/j.jpedsurg.2013.10.019
Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, Farley DR (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg 254:502–509. doi:10.1097/SLA.0b013e31822c6994 (discussion 509-511)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest and source of funding
Authors Choi SB, Lee SR declare that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study (retrospective observational study), formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, S.R., Choi, S.B. The efficacy of laparoscopic intracorporeal linear suture technique as a strategy for reducing recurrences in pediatric inguinal hernia. Hernia 21, 425–433 (2017). https://doi.org/10.1007/s10029-016-1546-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1546-y