Abstract
Background
Open repair of recurrent paediatric inguinal hernias (IH) is difficult and there is definite risk of damaging the vas deferens and testicular vessels during dissection of the previous open herniotomy field. Laparoscopic repair (LR) has the benefit of avoiding the previous operative site.
Method
Records of patients with recurrent IH that had LR after open repair were reviewed and evaluated retrospectively. The results were compared with data from cases in which the LR method was used in the initial IH repair.
Results
From September 2002 to October 2005, four boys and one girl (mean age 58.8 months) were treated in our institution for recurrent IH after open repair. Operative time, success rate and complications did not show any statistically significant difference when compared with our previous prospectively collected data for primary repairs.
Conclusion
Laparoscopic repair is the preferred operation for recurrent childhood IH after open repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Repair of inguinal hernia (IH) is one of the most common operations in paediatric surgical practice [1]. The incidence of IH ranges from 0.8 to 4.4% in children of all ages. It is particularly common in the first year of life.
Open repair is still the most popular method of treatment for paediatric IH resulting from patent processus vaginalis only [2, 3]. There is no need to perform muscle strengthening procedures after division and ligation of the hernia sac. However, the recurrence rate remains high, ranging from 1.76 to 6.3% [4–6], and has been attributed to the operational setting, i.e. a general department where several surgeons and residents operate upon a limited number of paediatric patients [6]. Other suggested reasons include junior surgeons or surgeons without specific paediatric surgical training performing the operations.
In boys, re-operations are difficult and require tedious and careful dissection of the dense fibrous tissue resulting from the earlier surgery. There are definite risks of damaging the vas deferens and testicular vessels, which are situated in the midst of the dense fibrous tissue.
Our centre has reported a safe laparoscopic method for paediatric IH repair [7–9]. In cases of recurrent hernia after an open operation, the operative site is above the previous operative field. The laparoscopic method should thus have a lesser chance of damaging the vas deferens and testicular vessels.
The present study was designed to evaluate our laparoscopic repair (LR) for paediatric recurrent IH after open repair. The results were also compared with the data acculmulated from cases in which the same laparoscopic method was used in the first attempt at IH repair.
Materials and methods
The medical records of all paediatric patients who were treated laparoscopically in our institution for recurrent IH after open surgery were reviewed retrospectively. The following parameters of the patients were noted: sex, age, follow-up duration, operation time, success rate and complications. The data were compared with data from our previously reported IH patients who were treated laparoscopically as the first initial hernia operation [9].
Continuous data were expressed as mean ± standard deviation (SD) and statistical significance with two-tail t test or Mann–Whitney test. For proportional data, Chi-square or Fisher’s exact test was used. Statistical significance was set at P<0.05.
Surgical technique
The detailed technique has been reported elsewhere [7–9]. Briefly, after induction of general endotracheal anaesthesia, the patient is placed in the Trendelenburg position. A 5-mm port is then inserted through the umbilicus. Pneumoperitoneum with pressure between 8 and 10 mm Hg is created with carbon dioxide. The internal opening of the hernia is first confirmed and then the opposite side is inspected. Two more 3-mm ports are placed under telescopic vision via the abdominal wall medial to anterior superior iliac spine. Contents of the hernia, such as omentum or bowel loop, are gently dissected from the hernia sac (Fig. 1). For girls, 3/0 prolene stitches are placed into the peritoneal cavity through the abdominal wall with a 25 mm half circle round body needle. The entry point of the needle is placed under telescopic vision so that it is in the vicinity of the 3 o’clock position of the internal inguinal opening. A purse-string suture is placed around the internal hernia opening and tied using intraperitoneal knotting. The ends of the stitches are then cut after passing the needle out through the abdominal wall.
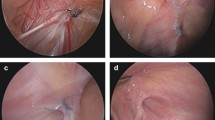
For boys, to separate the important structures of vas deferens and testicular vessels from the peritoneum, normal saline injection is introduced into the extraperitoneal space with an injector (6F, 155 mm, NM-3k injector, Olympus, Tokyo, Japan) guided by a metal cannula (Stryker, Santa Clara, CA) (Fig. 2a–d). The same size of stitches and needles are used as in girls. On placing the needle for the purse-string stitch, “Needle sign” was emphasised. “Needle sign” refers to the point at which the needle could be seen clearly underneath the peritoneum without the vas and the testicular vessel in between. Checking for this sign further protected these important structures from being included in the stitch.
a Appearance of the internal inguinal opening after a portion of omentum was dissected from the opening. There was not much fibrous tissue around the opening. b Extraperitoneal saline injection easily separated the testicular vessels and vas deferens from the peritoneum. c A purse string stitch was put around the internal inguinal opening. d An intracorporal knot tightly closed the internal inguinal opening
The stitch ends are pulled and tightened slightly before being tied together. A complete ring of peritoneum without the presence of any visible significant portion of raw stitch is noted as “Complete ring” sign. Only then are the ends tied and the opening closed completely. The “Complete ring” sign was used to prevent recurrence.
After release of pneumoperitoneum, the ports are removed. The umbilical wound is closed with absorbable stitches and the lateral wounds with sterile strips.
Results
From September 2002 to October 2005, four boys and one girl (mean age 58.8 months) were treated in our institution for recurrent IH following open operations (Table 1). One patient had bilateral hernias after an open operation on one side in another institution. Both hernias in this patient were treated laparoscopically in one operative setting.
All patients were treated successfully with our laparoscopic technique. No recurrence was detected in this group of patients with a mean follow-up period of 21 months. No testicular atrophy or other possible complications were detected during follow-up.
Comparison of the present data of operative time and complications from recurrent LR repairs following open operations with previous data from primary repairs by LR [9] revealed no statistically significant difference (Table 1). The recurrent repairs were as simple as primary repairs because both could be finished within similar operative times.
Discussion
After reviewing 71 recurrent IH after open repair in 62 children, Grosfeld et al. [10] suggested adequate high ligation at the internal ring, snugging of a large internal ring, avoidance of injury to the canal floor and closure of the internal ring in girls to prevent indirect hernia recurrence. From the above technical considerations, the laparoscopic method can theoretically avoid recurrence. However, the recurrence rate was reported to be 3.4% in data collected from three centres carrying out 933 repairs [11]. The main reason for the high recurrence rate may be the presence of testicular vessels and vas deferens in close proximity to the peritoneum at the expected site of closure near the internal ring (Fig. 1). Our technical refinement, which uses saline injection to separate these structures from the peritoneum (Fig. 2a–d), and the emphasis on the “Complete ring” sign during surgery, has reduced the recurrence rate to 1% [8].
As the first initial operation for IH, LR is also found to be superior to open operation with regard to postoperative pain, recovery and cosmesis. It can also allow detection of contralateral hernias and have them repaired at the same operation [9]. These findings were based on our prospective randomised single-blinded control study to compare the two forms of operation for paediatric IH.
For recurrent hernias after an open operation, re-operation with the open method requires going through the old operation site, which in boys almost always has the vas deferens and testicular vessels embedded in dense fibrous tissue. The operation is always tedious and there is the danger of damaging these important structures. From the present retrospective study, the laparoscopic method is the preferred operation for recurrent hernias after open hernia repair. In addition to all the advantages of the laparoscopic method, it also avoids the previous operation site, thus avoiding damage to the vas deferens and testicular vessels. Further, it is as simple as a fresh hernia repair because the time taken for LR of recurrent hernia was the same as for a fresh LR (Table 1). There were no added complications, and the operations were no less successful as compared with initial laparoscopic operations. There was no recurrence in the present group of patients after a mean follow-up of 21 months.
In conclusion, LR is the preferred operation for recurrent childhood IH following open operation. With refinements in the technique of LR, recurrence can be prevented even in this group of patients.
References
Cheung TT, Chan KL (2003) Laparoscopic inguinal hernia repair in children. Ann Coll Surg HK 7:94–96
Levitt MA, Ferraraccio D, Arbesman MC, Brisseau GF, Caty MG, Glick PL (2002) Variability of inguinal hernia surgical technique: a survey of North American pediatric surgeons. J Pediatr Surg 37:745–751
Antonoff MB, Kreykes NS, Saltzman DA, Acton RD (2005) American academy of pediatric section on surgery hernia survey revisited. J Pediatr Surg 40:1009–1014
Carneiro PM (1990) Inguinal herniotomy in children. East Afr Med J 67:359–364
Harvey MH, Johnstone MJ, Fossard DP (1985) Inguinal herniotomy in children: a five-year survey. Br J Surg 72:485–487
Nazir M, Saebo A (1996) Contralateral inguinal hernial development and ipsilateral recurrence following unilateral hernia repair in infants and children. Acta Chir Belg 96:28–30
Chan KL, Tam PK (2003) A safe laparoscopic technique for the repair of inguinal hernias in boys. J Am Coll Surg 196:987–989
Chan KL, Tam PK (2004) Technical refinements in laparoscopic repair of childhood inguinal hernias. Surg Endosc 18:957–960
Chan KL, Hui WC, Tam PK (2005) Prospective randomized single-center, single-blinded comparison of laparoscopic vs repair of pediatric inguinal hernia. Surg Endosc 19:927–932
Grosfeld JL, Minnick K, Shedd F, West KW, Rescorla FJ, Vane DW (1991) Inguinal hernia in children: factors affecting recurrence in 62 cases. J Pediatr Surg 26:283–287
Schier F, Montupet P, Espostito C (2002). Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg 37:395–397
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, K.L. Laparoscopic repair of recurrent childhood inguinal hernias after open herniotomy . Hernia 11, 37–40 (2007). https://doi.org/10.1007/s10029-006-0158-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-006-0158-3