Abstract
The present study aimed to investigate the long-term quality of life (QoL) in a large sample of pediatric obsessive–compulsive disorder (OCD) patients. The study included 220 pediatric OCD patients from the Nordic Long-term OCD Treatment Study (NordLOTS) who were evaluated at seven time points before, during, and after stepped-care treatment over a 3-year follow-up period. Data from three symptom severity trajectory classes formed the basis of the QoL evaluation: acute (n = 127, N = 147), slow (n = 46, N = 63), and limited responders (n = 47, N = 59). Patients’ QoL was assessed using parent and child ratings of the revised Questionnaire for Measuring Health-related Quality of Life in Children and Adolescents (KINDL-R). QoL was analyzed by trajectory class using a random mixed effects model. The association between pre-treatment factors and long-term QoL was investigated across classes in a multivariate model. Three years after treatment, the acute responder class had reached QoL levels from a general population, whereas the limited responder class had not. The slow responder class reached norm levels for the child-rated QoL only. Higher levels of co-occurring externalizing symptoms before treatment were associated with lower parent-rated QoL during follow-up, while adolescence and higher levels of co-occurring internalizing symptoms were associated with lower child-rated QoL during follow-up. For some patients, residual OCD symptoms in the years after treatment, even at levels below assumed clinical significance, are associated with compromised QoL. Co-occurring symptoms could be part of the explanation. Assessing QoL after OCD treatment, beyond the clinician-rated symptom severity, could detect patients in need of further treatment and/or assessment. Trial registry: Nordic Long-term Obsessive–Compulsive Disorder (OCD) Treatment Study; www.controlled-trials.com; ISRCTN66385119.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality of life (QoL) has increasingly been acknowledged as a crucial measure of treatment outcome for a range of diseases, including obsessive–compulsive disorder (OCD), with the recognition that reductions in functional impairment and subjective well-being are important markers of treatment gains [1]. Symptom reductions should translate into better functioning and well-being for the patient. In this regard, generic questionnaires are considered important because they enable comparisons between clinical groups and general population groups [2, 3]. The definition of QoL varies and three perspectives dominate QoL research: health-related QoL (HRQoL), social indicators (e.g., wealth, infant mortality in a country, college-attendance), and subjective well-being (e.g., happiness, satisfaction with life, self-actualization) [4]. Of these, the former is the most prominent but does not represent a concept with a clear definition. However, HRQoL relies on the definition of health by the WHO, who identify it as, “a state of complete physical, mental and social well-being and not merely absence of disease or infirmity” [5]. HRQoL usually assesses areas like physical, mental/cognitive, and social functioning [6] and is by definition rated by the individual [4]. Given the various conceptualizations of QoL, comparisons between studies require awareness of definitions. In the present study, we apply an HRQoL approach in accordance with operationalization of the revised Questionnaire for Measuring Health-related Quality of Life in Children and Adolescents (KINDL-R), which is a subjective evaluation (as well as a parent proxy rating) of well-being in the areas of physical, emotional, self-esteem, family, friends, and school [7]. In previous studies, child and parent ratings of child QoL have not been strongly correlated [8, 9], and so it is important to consider both. By definition, children’s self-reports should be regarded as central [10], yet questions have been raised regarding the validity of younger children’s ratings [11]. Overall, in non-clinical samples parents seem to rate their children’s QoL higher than the children themselves, whereas the opposite is true for clinical samples [12].
OCD is characterized by recurrent obsessions and compulsions [13] and affects around 0.5–2% of children and adolescents [14, 15], causing considerable impairment for the children and their families [16]. Compared with the general population, QoL is reduced in adult OCD patients [17], especially for those with comorbid conditions that can be even more constraining on QoL than OCD symptoms alone [17,18,19,20,21]. This especially pertains to depressive symptoms, which have been suggested to be a mediating factor for QoL in OCD [22]. Although not as thoroughly investigated, children and adolescents with OCD also show reduced QoL compared with children with no psychiatric disorders [3, 23]. Like in adults, comorbid psychiatric disorders [3] as well as co-occurring symptoms, especially internalizing symptoms [23, 24], seem to reduce the childrens' QoL even further.
In adults with OCD, QoL increases in treatment responders after cognitive behavioral therapy (CBT) or medical treatment [17], yet QoL is still compromised in some of these patients compared with control groups [21, 25]. Only a few studies have investigated QoL in pediatric OCD after treatment [26,27,28,29]. This research corroborates findings from adult studies suggesting increasing QoL after CBT, yet for one study this was only the case for parent ratings [28]. Overall, the literature suggests that QoL and the severity of psychopathology are separate (yet, overlapping) constructs, both conceptually and empirically [2, 30, 31].
The long-term perspective of QoL in pediatric OCD (as well as other childhood mental and behavioral disorders) has been even less investigated [2]. Palermo and colleagues [32] interviewed 36 adults (> 16 years of age) diagnosed with OCD in childhood and found that remitters in adulthood (Y-BOCS < 8) showed higher QoL than non-remitters, especially regarding interpersonal relationships and work. Predictors of lower QoL in adulthood were primary hoarding symptoms in childhood, whereas forbidden thoughts symptoms in childhood predicted higher QoL in adulthood. Studies with larger samples and better follow-up procedures are needed to confirm these results. For pediatric clinical samples in general, factors associated with poorer QoL over time are pre-treatment chronic physical disease, low self-esteem, poor social skills, stressful life events, and poor family functioning [31, 33]. In the general population, family functioning has been found to mediate the longitudinal association between higher internalizing and externalizing symptoms at baseline and lower QoL after six months in 10–16 year-olds [34].
Since symptom severity ratings are more common for post-treatment assessment than QoL, it is important to investigate how QoL changes over time according to different symptom severity trajectories. This could provide valuable knowledge regarding the potential impact and significance of OC symptom severity in patients taking different paths. In a recent study on the present sample, three distinct trajectory classes were identified using latent class growth analysis on the Children’s Yale-Brown Obsessive–Compulsive Scale (CY-BOCS), with symptom severity ratings assessed during and up to 3 years after stepped-care treatment [35]. The acute, sustainable responder class (n = 147; below referred to as acute responders) showed acute treatment response with sustained low levels of symptom severity during the 3 years of follow-up. The slow, continued responder class (n = 63; below referred to as slow responders) did not meet the response criteria after initial treatment, but after about half of the patients received further treatment the mean trajectory of this class improved to the levels of the acute responder class at the 3-year end-point. The limited, long-term responder class (n = 59; below referred to as limited responders) had a mean trajectory reaching below the pre-defined cut-off for treatment response, but with no further improvement during follow-up. Almost a third of the patients in this trajectory class received further treatment. For more information about the three classes, please see the work of Jensen and colleagues [35].
The primary objective of the present study was to evaluate pediatric OCD patients’ long-term QoL (a composited score in the areas of physical, emotional, self-esteem, family, friends, and school well-being; below simply referred to as QoL) and subscale scores separately in relation to symptom severity trajectory classes. The specific aims concerning this objective were for each trajectory class to: (1) describe QoL and subscale scores during stepped-care treatment and up to 3 years of follow-up; (2) evaluate the differences in QoL from pre- to post-first-line CBT and from post-first-line CBT to the 3-year follow-up; (3) compare QoL and subscale scores with scores from a comparable general population at the 3-year follow-up; and (4) evaluate associations between QoL and symptom severity. For differences between the classes, the aim was to (5) evaluate QoL at all time points and the subscales at 3-year follow-up. The secondary objective was across trajectory classes to identify pre-treatment factor associations to QoL during the follow-up. We hypothesized that QoL would be associated with symptom severity, and we expected OCD symptom factor scores and co-occurring symptoms to be associated with QoL during follow-up.
Methods
Participants
The study included 220 out of 269 pediatric OCD patients aged 7–17 from the Nordic Long-term OCD Treatment Study (NordLOTS). As the QoL assessments were introduced during the study period due to time-consuming translations to all Scandinavian languages as well as approval processes, not all patients were given the QoL questionnaire at pre-treatment. The NordLOTS inclusion criteria were a DSM-IV OCD diagnosis and a CY-BOCS severity score above 15. Comorbid disorders were allowed if they were not of higher treatment priority than OCD. The NordLOTS study sample has been described in more detail elsewhere [36, 37]. Participants for the present study were included if they had either a child-rated or a parent-rated QoL assessment for at least one of seven study assessment points. The gender distribution was equal, with 50.9% females (51.3% in the full NordLOTS sample).
Treatment and procedures
All patients were assessed by independent evaluators at baseline. Treatment was conducted following a stepped-care design starting with 14 weekly sessions of manualized CBT for all patients (Step 1) [36, 37]. In Step 1, non-responders (CY-BOCS > 15; n = 50) were randomized to either a selective serotonin reuptake inhibitor (SSRI) for 16 weeks (n = 22) or an additional 10 sessions of CBT (n = 28) in Step 2 [38]. In Step 2, CBT non-responders were offered SSRIs [39]. During the first year of follow-up, up to four booster sessions were offered to patients on request. Relapse (CY-BOCS > 15) during this time period activated a total of 10 CBT sessions (including the boosters) followed by SSRI treatment in cases of continued non-response. The 2- and 3-year follow-ups were conducted naturalistically with no specified intervention procedures.
Assessment by independent evaluators as well as a comprehensive questionnaire battery were completed before treatment, mid-treatment during Step 1, at the end of Step 1, and 6, 12, 24, and 36 months after the end of Step 1.
Instruments
Questionnaire for Measuring Health-related Quality of Life in Children and Adolescents, revised version, KINDL-R is a generic questionnaire used to assess multidimensional health-related QoL in children and adolescents [40]. Both the self-report questionnaire for children and adolescents and the parent proxy report version were used in the present study. Six subscales with four items in each make up the questionnaire. The subscales reflected well-being related to the following areas: physical, emotional, self-esteem, family, friends, and school, representing the child’s experiences during the past week. Each item is rated on a five-point Likert scale (1 = never, 5 = always), and all scores are transformed to a scale ranging from 0 to 100, with higher scores indicating better QoL. All subscale scores are added together to form a total score that is also transformed to a 0–100 scale. In addition, the questionnaire provides a disorder-related subscale that reflects the child’s experience of OCD-related burden and is not part of the total score. The psychometric testing of the KINDL-R has proven good scale utilization with only the family subscale showing ceiling effects of 17% [7]. For all subscales, the scale fit was 85% or above, and the internal consistencies for subscales reached alpha-values from 0.54 (friends and school) to 0.73 (family) and 0.82 for the total score [7]. In the current sample, Cronbach´s alpha for the subscales at the 3-year follow-up point reached from 0.64 (school) to 0.86 (self-esteem) for the parent ratings and from 0.50 (school well-being) to 0.79 (self-esteem) for the child ratings. The disorder subscale reached alpha values at the 3-year follow-up of 0.71 and 0.54 for the parent and child ratings, respectively. For total scores at the 3-year follow-up point, Cronbach´s alpha was 0.80 for the parent ratings and 0.82 for the child ratings. For the present study, KINDL-R norm data were derived from a general population group (N = 1821, 8–16 years) consisting of children and adolescents from Sør-Trøndelag county in Norway, which is an area with both urban and rural establishments, making it demographically comparable with the present study sample [41]. More information about the comparison group can be found in studies by Jozefiak and colleagues [41, 42].
Children's Yale-Brown Obsessive–Compulsive Scale (CY-BOCS) is a semi-structured interview conducted by a clinician assessing the patient’s (children and adolescents aged 6–17) OCD symptom content and severity (0–40) [43]. The CY-BOCS has proven reasonable reliability and validity as well as good internal consistency [44]. Højgaard and colleagues (2017) conducted a factor analysis on the CY-BOCS symptom checklist and found three symptom dimensions (harm/sexual, symmetry/hoarding, and contamination/cleaning [45]), all of which were used in the present study.
Kiddie Schedule for Affective Disorders and Schizophrenia—Present and Lifetime Version (K-SADS-PL) is a semi-structured interview that detects a wide range of DSM-IV pediatric mental disorders [46]. The scale showed good convergent and divergent validity in the present sample [47].
Clinical Global Impression-Severity (CGI-S) is a widely used clinical rating of general OCD severity (seven levels from normal to extreme) [48].
Child Behavior Checklist (CBCL) is a 113-item questionnaire for 6–18-year-old children, assessing behavioral and emotional problems [49]. The scale comprises several subscales among which the parent-rated overall symptom scales: internalizing (score range 0–64) and externalizing (score range 0–70) raw scores were used in the present study. Internal consistency ranges from α = 0.78 to α = 0.97 [49].
Child Obsessive–Compulsive Impact Scale-Revised (COIS-R) is a child- and parent-rated questionnaire with 33 items assessing the impact of obsessive–compulsive symptoms on the child’s functioning and a total score ranging from 0 to 99 [16].
Children’s Global Assessment Scale (CGAS) is a clinical rating of the patient’s global functional level on a scale from one to 100 [50, 51].
Screen for Child Anxiety–Related Emotional Disorders (SCARED) is a child- and parent-rated questionnaire assessing DSM-IV anxiety symptoms [52].
Mood and Feelings Questionnaire (MFQ) assesses parent- and child-rated DSM-III-R depressive symptoms in 8–18 year-olds [53, 54].
Family Accommodation Scale (FAS) assesses the extent to which the family accommodates the child’s OCD symptoms in a 12-item clinical interview of parent(s) with a total score ranging from 0 to 48 [55].
Socioeconomic Status (SES) was categorized using Hollingshead’s two-factor index of social position [56] with a combination of parental occupation (1–9) and education (1–7) ratings. Occupation and education were given respective weights of 5 and 3 to generate a summary score (8–66).
Data analysis
Missing data
Consistent with the KINDL-R manual’s recommendations, a maximum of 30% missing was accepted of the subscale items. The number of KINDL-R ratings at different time points can be derived from Table 1. The difference in the number of patients receiving the KINDL-R at the beginning of the study due to the late introduction of the scale was considered random by definition. Percentages of at least one KINDL-R rating at any of the assessment points in the classes were 86.39% for the acute responders, 73.02% for the slow responders, and 79.66% for the limited responders, with a p-value regarding the difference between the classes of 0.063.
The number of study dropouts after treatment (i.e., no data from the 6-month assessment and onwards in the follow-up period) was n = 87 for the child-rated KINDL and n = 90 for the parent-rated KINDL. For both measures, the dropout group had higher pre-treatment age, higher CY-BOCS severity, later OCD onset, higher scores in the harm/sexual symptom dimension, higher scores on COIS-P and COIS-C, and a higher percentage of Step 1 non-responders compared with the non-dropout group. For the child-rated KINDL scores, the dropout group also had higher pre-treatment scores on CGI-S, CBCL internalizing and externalizing subscales, and MFQ-P. Not all of these variables were included in the analyses, however, as we were concerned they would obscure the actual results. Yet, the mentioned factors should be taken into account when interpreting the results.
Missing KINDL-R data were handled with maximum likelihood estimation as part of the linear mixed model. Missing data in pre-treatment variables used for testing associations to KINDL-R follow-up scores were handled with multiple imputations by chained equations. One hundred generated imputed datasets were combined using Rubin’s rules [57].
Analyses of QoL and subscales
Child- and parent-rated KINDL-R total scores, as well as the subscale scores, were analyzed by class using a random mixed effects model including all available data from the seven assessment points. The model included parent- and child-rated KINDL-R, class, time, and age group (7–11 vs. 12–17 years) with interactions between class and time as well as between an indicator of parent-/child-rating and time. Wald’s test was used to compare norm level means with QoL and subscale scores at the 3-year follow-up.
Associations between QoL and symptom severity
Total parent- and child-rated KINDL-R scores, as well as CY-BOCS scores from all time points, were converted to z-scores and plotted for comparison in each class. In addition, the associations between available KINDL-R scores and CY-BOCS severity scores were analyzed using Spearman’s correlation coefficient with 95% bootstrapped bias-corrected and accelerated confidence intervals (CI BCa).
Pre-treatment variables’ associations to QoL during follow-up across classes
The pre-treatment variables’ possible association to parent- and child-rated KINDL-R total scores during follow-up were analyzed using a mixed effects model including demographics (age, gender, and SES), OCD-related factors (symptom factor scores, severity scores for obsessions and compulsions separately, and duration of OCD), functional levels (COIS-P, FAS, and CGAS), and comorbid variables (KSADS tic disorder, CBCL internalizing symptoms, and CBCL externalizing symptoms). The pre-treatment variables were analyzed separately for parent and child KINDL-R follow-up ratings across classes to be able to include a wide range of variables, which were chosen to generate broad coverage while avoiding overlapping content.
Results
Quality of life in pediatric symptom severity trajectory classes
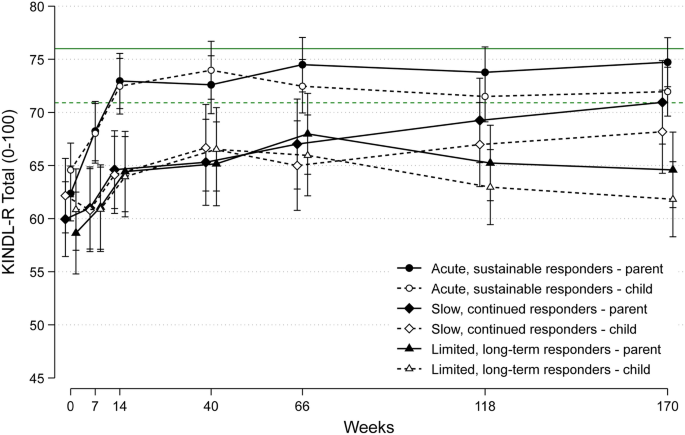
Parent- and child-rated KINDL-R-scores are plotted according to class membership along with norm scores in Fig. 1. The mean scores and number of ratings in the classes are listed in Table 1. Subscale scores (physical, emotional, self-esteem, family, friends, school, and disorder) and relevant norm scores are plotted in Supplementary Fig. 1a, b, which can be derived from the online appendix.
Parent- and child-rated KINDL-R total scores for three treatment responder classes during and after stepped-care treatment. Scores are adjusted for age. The solid green line represents mean parent scores of a representative norm group whereas the dashed green line represents mean child scores from the same group
Mean differences in KINDL-R over time for each class can be derived from Table 2. For both the parent and child ratings in the acute responder class, KINDL-R-scores increased during Step 1, and were sustained between the end of Step 1 and the 3-year follow-up. For the slow responder class, parent- but not child-rated KINDL-R-scores increased during Step 1, which also pertained to the period from the end of Step 1 and up to the 3-year follow-up point. Parent-rated KINDL-R-scores in the limited responder class increased during Step 1, but not the child ratings, and there were no changes from the end of Step 1 to the 3-year follow-up for either parent- or child-rated KINDL-R-scores. For the period from pre-treatment to the 3-year follow-up, the only total KINDL-R ratings that did not significantly increase were the child ratings in the limited responder class.
Three-year follow-up: comparisons with the general population for QoL and subscales
Comparisons with norm levels for KINDL-R total scores can be found in Table 2. Parent- and child-rated subscale scores, as well as scores from a general population, are listed in Table 3. Regarding KINDL-R total scores at the 3-year follow-up, both the parent and child ratings of the acute responder class had reached the levels of the norm group. The slow responder class reached norm levels at the 3-year follow-up for the child ratings, but not for the parent ratings. Both the parent and child ratings in the limited responder class were below norm levels at the 3-year follow-up. Regarding parent-rated subscale scores at the 3-year follow-up, the acute responder class was below norm levels for physical well-being and self-esteem, whereas this was the case for the slow responder class in self-esteem and for the limited responder class in physical, emotional, self-esteem, friends, and school well-being. For child-rated subscale scores at the 3-year follow-up, the acute responder class did not score below norm levels at any of the subscales and was above self-esteem norm levels. The slow responder class scored below norm levels on school well-being. The limited responder class scored below norm levels at the physical, emotional, family, friends, and school subscales.
Associations between QoL and symptom severity
The KINDL-R and CY-BOCS z-scores are for comparisons plotted in Supplementary Fig. 2, which is available in the online appendix. There was a significant negative association between KINDL-R and CY-BOCS scores for all of the three classes. The associations did not differ significantly (acute responders: r = − 0.357, CI = − 0.291 to − 0.411; slow responders: r = − 0.354, CI = − 0.249 to − 0.443; and limited responders: r = − 0.417, CI = − 0.339 to − 0.503).
Differences in QoL between trajectory classes
The statistical model implied equal differences in parent and child ratings for the three classes. As can be seen in Table 4, there were no differences between the classes in pre-treatment QoL total score. For the slow responder class, KINDL-R-scores were significantly lower than the acute responder class at all other time points, except for the 3-year follow-up. The limited responder class scored lower on the KINDL-R than the acute responder class at all time points except for pre-treatment. There were no significant differences between the slow and the limited responder classes except for the 3-year follow-up, where the slow responder class scored higher. Regarding the disorder subscale scores (Table 3), the child ratings of the acute responder class were significantly higher than the two other classes (which had similar scores) at the 3-year follow-up. In terms of parent-rated disorder well-being, the slow responder class scored significantly lower than the acute responder class, whereas the limited responder class scored significantly lower than the two other classes.
Across classes: pre-treatment associations to long-term QoL
Pre-treatment variable associations with KINDL-R scores during follow-up (parent- and child rated) can be found in Table 5. Lower parent-rated KINDL-R total scores during follow-up were associated with higher pre-treatment CBCL externalizing scores (β = 0.282, p = 0.026). Lower child-rated KINDL-R total scores during follow-up were associated with pre-treatment adolescence (β = 3.575, p = 0.035) and higher CBCL internalizing scores (β = 0.229, p = 0.040).
Discussion
In the present study, we investigated the QoL in 220 pediatric OCD patients from Denmark, Norway, and Sweden during stepped-care treatment and up to 3 years after treatment. We evaluated the QoL according to three distinct symptom severity trajectory classes in order to investigate QoL changes overtime related to patients’ level of symptom severity. In addition, we wanted to evaluate the symptom severity trajectories in terms of QoL as an important aspect of treatment outcome while comparing the follow-up scores to a comparable norm population.
Considering changes in each symptom severity trajectory class over time together with the differences between the classes, the picture was overall as expected, albeit with some findings deserving extra attention. At pre-treatment, there were no differences in the patients’ QoL when evaluated according to their 3-year symptom severity trajectories. However, after initial CBT the acute responder class, characterized by a quick response pattern, had significantly higher levels of QoL compared with the other classes. This is in line with other research showing that treatment response has a positive effect on patient QoL [23, 26]. The QoL in the acute responder class increased significantly during first-line CBT and was sustained during follow-up. For both the slow and the limited responder classes, the parents rated small but significant improvements in QoL during Step 1, while the children did not. This could indicate that a certain amount of symptom reduction is needed for the child to experience improved QoL as all three classes did improve according to symptom severity during Step 1, yet at different levels and paces. It also questions the definition of treatment response and suggests further symptom reductions and/or QoL assessments to be considered in treatment response definitions [58].
In the follow-up period, both the children and the parents rated improved QoL in the slow responder class, whereas this was only the case for the parent ratings in the limited responder class. The mean symptom severity trajectory of the slow responder class showed significant improvements in terms of symptom severity, probably as a result of further treatment for almost half of the patients in this class, so the QoL improvements are apparently following these changes in symptom severity. The fact that the child-ratings in the limited responder class did not show any improvements from pre-treatment to the 3-year follow-up point, despite their improvements in Step 1 according to symptom severity, is worrying and emphasizes the vulnerability and need for monitoring and/or further diagnosing of these patients. The mean trajectory for the limited responder class in the follow-up period was below the CY-BOCS cut-off of 16 for treatment response, which means that these patients on a group level would be regarded as responders to treatment. Yet, QoL assessments suggest that this symptom reduction did not have an actual impact on the child-rated QoL. Findings might indicate that QoL assessments after treatment could detect more patients in need of further treatment (for their OCD or other symptoms) than a narrow focus on symptom severity assessment alone. Overall, longitudinal QoL in children and adolescents is sparsely studied, yet it has been suggested that QoL generally decreases over a period of 3 years in children 8–18 years of age, especially for children with (deteriorating) mental disorders [59]. In the present study, none of the classes decreased in QoL levels over the 3-year period, except for a possible tendency in the limited responder class despite their low to moderate symptom severity. This may suggest that this class could still be considered a group of patients with a mental disorder(s) requiring further assessment and/or treatment. It is not possible to state causality from this study, but it could be speculated if aspects of QoL hinder treatment success. Since there were no pre-treatment differences in QoL between the patient groups, there could instead be a bi-directional relationship between symptom reductions and QoL where symptom reductions increase QoL, which again fosters further symptom reductions and so forth. A similar relationship between depressive symptoms and QoL has been suggested in Jacoby and colleagues [60].
Focusing on comparisons to norm levels at the 3-year endpoint, the acute responder class was in the range of norm levels according to both child- and parent-rated QoL. Yet, at a subscale level, this class was below norm levels on the parent ratings of the physical and school subscales, indicating remaining problem areas despite their positive outcomes regarding OCD symptom severity. This suggests that children and adolescents treated for OCD, even with excellent symptom severity reductions, could be considered more vulnerable than peers and may suggest general heightened attention towards children who have once been treated for OCD. The slow responder class reached norm QoL levels for the child ratings at the 3-year follow-up, but not for the parent ratings. This is interesting as this class had low OCD symptom severity at this time according to their mean symptom severity trajectory. As this class presented with higher levels of co-occurring symptoms than the acute responder class at pre-treatment [35], this could explain their compromised QoL levels at follow-up. Indeed, comorbid diagnoses have been associated with lower levels of QoL at pre-treatment in a subgroup of the present sample [3]. Analysis of subscale scores showed that the remaining problem areas concerned child-rated school well-being and parent-rated self-esteem for the slow responder class. In addition, this class presented with the highest drop-out rate during follow-up, which could indicate even more compromised QoL levels since dropouts were associated with non-response to CBT, lower functional levels, and co-occurring symptoms possibly associated with poorer QoL during follow-up. The limited responder class showed reduced QoL levels at the 3-year endpoint on all subscales with the exception of the parent-rated family subscale and child-rated self-esteem. This highlights that at the 3-year endpoint, either the remaining OCD symptoms have an impact on the patients’ QoL or these patients have co-occurring symptoms and/or other problem areas that affect their QoL negatively.
Interestingly, for the disorder subscale both the parent and child ratings of the slow and limited responder classes scored below the acute responder class despite the mean symptom severity trajectory of the slow responder class being aligned with the acute responder class at this point. Even though the disorder well-being subscale is not a rating of OCD symptoms as such, it still may indicate incongruence between a clinical rating and a patient rating of disorder severity. Recent research on adult OCD patients suggests that self-reporting of symptom severity is more aligned with the patients’ QoL than clinicians’ severity ratings [61], and emphasizes the added value of including a self-report (e.g., a QoL measure) as a treatment outcome [1, 2]. It has been suggested elsewhere that adult patients who only experience symptom reduction, but limited QoL improvements, are in need of further treatment to prevent symptom severity relapse [62] and to reach QoL norm levels [22]. Our findings add to this discussion and highlight the need for QoL assessments as part of treatment evaluation. In addition, this is supported by the findings of a negative, though not absolute, association between symptom severity and QoL, also found elsewhere [23, 28], suggesting QoL is a related but still separate construct from symptom severity. The difference in the association between classes was non-significant, yet with the seemingly highest association for the limited responder class. Even though there were no significant differences in the present sample, the tendency raises the question of whether patients could differ in their experience of symptom impact. For example, two patients may present with the same levels of symptom severity but have starkly different interpretations of the invalidating nature of their symptoms.
Pre-treatment higher externalizing symptoms were associated with lower parent-rated QoL during follow-up, whereas higher internalizing symptoms and adolescence were associated with lower child-rated QoL during follow-up. This was in line with our hypotheses regarding co-occurring symptoms being associated with long-term QoL in both children [23] and adults with OCD [21, 63]. The finding emphasizes the need to take a broader perspective in treating patients and to assess them thoroughly. Elsewhere it has been shown that family functioning could mediate the longitudinal association between QoL and internalizing and externalizing symptoms in typically developing adolescents [34], and also that individual competencies could mediate the association between emotional problems and QoL in adolescents with ADHD [64]. These mechanisms may influence adolescents with OCD as well and could be relevant focus points during treatment to influence internalizing and externalizing symptoms and thereby the patients’ QoL. We did not find any clear associations between symptom dimensions and QoL at follow-up. This is discordant with studies indicating hoarding symptoms to be associated with lower QoL [32, 65]. The discrepancy can be explained by the fact that hoarding symptoms were not analyzed separately in the present study, but rather as a part of a larger symptom category. Further research is warranted in order to clarify potential differences between symptom dimensions in their associations to QoL and factors which could act as moderators or mediators in such correlations.
Strengths and limitations
This study was conducted on a large pediatric OCD treatment sample including a long follow-up period with fixed assessment points. The study thereby adds to a gap in the literature regarding long-term QoL outcomes in children and adolescents with mental health problems generally, as well as OCD specifically. As in most follow-up studies, ours is limited by attrition. This was handled with maximum likelihood equations as part of the mixed-effects models, yet the pre-treatment differences between dropouts at 1-year follow-up for QoL ratings and non-dropouts need to be taken into consideration when evaluating study findings. Consequently, the estimated levels of QoL during follow-up may be optimistic, especially for the slow and limited responder classes that encompassed the most strained patients. Further, while the internal consistency of the total KINDL score is good, the results of the subscales should be interpreted more cautiously because of varying alpha levels.
Conclusion
This is the first study to evaluate long-term QoL related to symptom severity trajectories in a large sample of pediatric OCD patients. Findings suggest that for some patients, QoL is still compromised compared with norm levels from a comparable general population 3 years after initial treatment despite apparent sufficient treatment response according to symptom severity levels. Adolescence and co-occurring internalizing and externalizing symptoms at pre-treatment were associated with reduced long-term QoL and should also be considered central in treatment. The findings support QoL measures to be part of standard pediatric OCD treatment outcome evaluation as this may identify patients who are in need of further interventions and/or assessment despite apparent treatment response.
References
Krause KR, Bear HA, Edbrooke-Childs J, Wolpert M (2019) Review: What outcomes count? Outcomes measured for adolescent depression between 2007 and 2017. J Am Acad Child Adolesc Psychiatry 58:61–71. https://doi.org/10.1016/j.jaac.2018.07.893
Jonsson U, Alaie I, Löfgren Wilteus A et al (2017) Annual research review: quality of life and childhood mental and behavioural disorders—a critical review of the research. J Child Psychol Psychiatry 58:439–469. https://doi.org/10.1111/jcpp.12645
Weidle B, Jozefiak T, Ivarsson T, Thomsen PH (2014) Quality of life in children with OCD with and without comorbidity. Health Qual Life Outcomes 12:152. https://doi.org/10.1186/s12955-014-0152-x
Wallander JL, Koot HM (2016) Quality of life in children: a critical examination of concepts, approaches, issues, and future directions. Clin Psychol Rev 45:131–143. https://doi.org/10.1016/j.cpr.2015.11.007
World Health Organisation (1947) The constitution of the world health organisation. WHO Chronicle 1:29
Moons P, Budts W, De Geest S (2006) Critique on the conceptualisation of quality of life: a review and evaluation of different conceptual approaches. Int J Nurs Stud 43:891–901. https://doi.org/10.1016/j.ijnurstu.2006.03.015
Bullinger M, Brütt AL, Erhart M, Ravens-Sieberer U (2008) Psychometric properties of the KINDL-R questionnaire: results of the BELLA study. Eur Child Adolesc Psychiatry 17:125–132. https://doi.org/10.1007/s00787-008-1014-z
Theunissen NCM, Vogels TGC, Koopman HM et al (1998) The proxy problem: child report versus parent report in health-related quality of life research. Qual Life Res 7:387–397. https://doi.org/10.1023/A:1008801802877
Eiser C, Morse R (2001) Can parents rate their child’s health-related quality of life? Results of a systematic review. Qual Life Res 10:347–357. https://doi.org/10.1023/a:1012253723272
Matza LS, Rentz AM, Secnik K et al (2004) The link between health-related quality of life and clinical symptoms among children with attention-deficit hyperactivity disorder. J Dev Behav Pediatr 25:166–174. https://doi.org/10.1097/00004703-200406000-00005
Coghill D, Danckaerts M, Sonuga-Barke E, Sergeant J (2009) Practitioner review: quality of life in child mental health—conceptual challenges and practical choices. J Child Psychol Psychiatry 50:544–561. https://doi.org/10.1111/j.1469-7610.2009.02008.x
Upton P, Lawford J, Eiser C (2008) Parent–child agreement across child health-related quality of life instruments: a review of the literature. Qual Life Res 17:895–913. https://doi.org/10.1007/s11136-008-9350-5
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington, DC
Heyman I, Fombonne E, Simmons H et al (2001) Prevalence of obsessive–compulsive disorder in the British nationwide survey of child mental health. Br J Psychiatry 179:324–329. https://doi.org/10.1192/bjp.179.4.324
Canals J, Hernández-Martínez C, Cosi S, Voltas N (2012) The epidemiology of obsessive-compulsive disorder in Spanish school children. J Anxiety Disord 26:746–752. https://doi.org/10.1016/j.janxdis.2012.06.003
Piacentini J, Peris TS, Bergman RL et al (2007) BRIEF REPORT: functional impairment in childhood OCD: development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale-Revised (COIS-R). J Clin Child Adolesc Psychol 36:645–653. https://doi.org/10.1080/15374410701662790
Macy AS, Theo JN, Kaufmann SCV et al (2013) Quality of life in obsessive compulsive disorder. CNS Spectr 18:21–33. https://doi.org/10.1017/S1092852912000697
Eisen JL, Mancebo MA, Pinto A et al (2006) Impact of obsessive-compulsive disorder on quality of life. Compr Psychiatry 47:270–275. https://doi.org/10.1016/j.comppsych.2005.11.006
Koran LM (2000) Quality of life in obsessive compulsive disorder. Psychiatr Clin North Am 23:509–517. https://doi.org/10.1017/S1092852912000697
Cassin SE, Richter MA, Zhang KA, Rector NA (2009) Quality of life in treatment-seeking patients with obsessive-compulsive disorder with and without major depressive disorder. Can J Psychiatry 54:460–467. https://doi.org/10.1177/070674370905400707
Moritz S, Rufer M, Fricke S et al (2005) Quality of life in obsessive-compulsive disorder before and after treatment. Compr Psychiatry 46:453–459. https://doi.org/10.1016/j.comppsych.2005.04.002
Hertenstein E, Thiel N, Herbst N et al (2013) Quality of life changes following inpatient and outpatient treatment in obsessive-compulsive disorder: a study with 12 months follow-up. Ann Gen Psychiatry 12:4. https://doi.org/10.1186/1744-859X-12-4
Lack CW, Storch EA, Keeley ML et al (2009) Quality of life in children and adolescents with obsessive-compulsive disorder: base rates, parent–child agreement, and clinical correlates. Soc Psychiatry Psychiatr Epidemiol 44:935–942. https://doi.org/10.1007/s00127-009-0013-9
de Vivan AS, Rodrigues L, Wendt G et al (2013) Quality of life in adolescents with obsessive-compulsive disorder. Rev Bras Psiquiatr 35:369–374. https://doi.org/10.1590/1516-4446-2013-1135
Diefenbach GJ, Abramowitz JS, Norberg MM, Tolin DF (2007) Changes in quality of life following cognitive-behavioral therapy for obsessive-compulsive disorder. Behav Res Ther 45:3060–3068. https://doi.org/10.1016/j.brat.2007.04.014
Weidle B, Ivarsson T, Thomsen PH et al (2015) Quality of life in children with OCD before and after treatment. Eur Child Adolesc Psychiatry 24:1061–1074. https://doi.org/10.1007/s00787-014-0659-z
Wellen B, Skriner LC, Freeman J et al (2017) Examining the psychometric properties of the pediatric quality of life enjoyment and satisfaction questionnaire in two samples of youth with OCD. Child Psychiatry Hum Dev 48:180–188. https://doi.org/10.1007/s10578-016-0662-3
Storch EA, Small BJ, McGuire JF et al (2018) Quality of life in children and youth with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 28:104–110. https://doi.org/10.1089/cap.2017.0091
Conelea CA, Selles RR, Benito KG et al (2017) Secondary outcomes from the pediatric obsessive compulsive disorder treatment study II. J Psychiatr Res 92:94–100. https://doi.org/10.1016/j.jpsychires.2017.04.001
Bastiaansen D, Koot HM, Ferdinand RF (2005) Psychopathology in children: improvement of quality of life without psychiatric symptom reduction? Eur Child Adolesc Psychiatry 14:364–370. https://doi.org/10.1007/s00787-005-0481-8
Bastiaansen D, Ferdinand RF, Koot HM (2020) Predictors of quality of life in children and adolescents with psychiatric disorders. Child Psychiatry Hum Dev 51:104–113. https://doi.org/10.1007/s10578-019-00914-4
Palermo SD, Bloch MH, Craiglow B et al (2011) Predictors of early adulthood quality of life in children with obsessive-compulsive disorder. Soc Psychiatry Psychiatr Epidemiol 46:291–297. https://doi.org/10.1007/s00127-010-0194-2
Jozefiak T, Greger HK, Koot HM et al (2019) The role of family functioning and self-esteem in the quality of life of adolescents referred for psychiatric services: a 3-year follow-up. Qual Life Res 28:2443–2452. https://doi.org/10.1007/s11136-019-02197-7
Jozefiak T, Wallander JL (2016) Perceived family functioning, adolescent psychopathology and quality of life in the general population: a 6-month follow-up study. Qual Life Res 25:959–967. https://doi.org/10.1007/s11136-015-1138-9
Jensen S, Højgaard DRMA, Hybel KA et al (2020) Distinct trajectories of long-term symptom severity in pediatric obsessive–compulsive disorder during and after stepped-care treatment. J Child Psychol Psychiatry 61:969–978. https://doi.org/10.1111/jcpp.13155
Thomsen PH, Torp NC, Dahl K et al (2013) The Nordic long-term OCD treatment study (NordLOTS): rationale, design, and methods. Child Adolesc Psychiatry Ment Health 7:41. https://doi.org/10.1186/1753-2000-7-41
Torp NC, Dahl K, Skarphedinsson G et al (2015) Effectiveness of cognitive behavior treatment for pediatric obsessive-compulsive disorder: acute outcomes from the Nordic Long-term OCD Treatment Study (NordLOTS). Behav Res Ther 64:15–23. https://doi.org/10.1016/j.brat.2014.11.005
Skarphedinsson G, Weidle B, Thomsen PH et al (2015) Continued cognitive-behavior therapy versus sertraline for children and adolescents with obsessive-compulsive disorder that were non-responders to cognitive-behavior therapy: a randomized controlled trial. Eur Child Adolesc Psychiatry 24:591–602. https://doi.org/10.1007/s00787-014-0613-0
Skarphedinsson G, Weidle B, Ivarsson T (2015) Sertraline treatment of nonresponders to extended cognitive-behavior therapy in pediatric obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 25:574–579. https://doi.org/10.1089/cap.2015.0041
Ravens-Sieberer U, Bullinger M (2000) KINDL-R. Questionnaire for measuring health-related quality of life in children and adolescents—Revised version 2000
Jozefiak T, Larsson B, Wichstrøm L (2009) Changes in quality of life among Norwegian school children: a six-month follow-up study. Health Qual Life Outcomes 7:7. https://doi.org/10.1186/1477-7525-7-7
Jozefiak T, Larsson B, Wichstrøm L et al (2008) Quality of Life as reported by school children and their parents: a cross-sectional survey. Health Qual Life Outcomes 6:34. https://doi.org/10.1186/1477-7525-6-34
Scahill L, Riddle MA, McSwiggin-Hardin M et al (1997) Children’s yale-brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852. https://doi.org/10.1097/00004583-199706000-00023
Storch EA, Murphy TK, Geffken GR et al (2004) Psychometric evaluation of the children’s yale-brown obsessive-compulsive scale. Psychiatry Res 129:91–98. https://doi.org/10.1016/j.psychres.2004.06.009
Højgaard DRMA, Mortensen EL, Ivarsson T et al (2017) Structure and clinical correlates of obsessive–compulsive symptoms in a large sample of children and adolescents: a factor analytic study across five nations. Eur Child Adolesc Psychiatry 26:281–291. https://doi.org/10.1007/s00787-016-0887-5
Kaufman J, Birmaher B, Brent D et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988. https://doi.org/10.1097/00004583-199707000-00021
Kragh K, Husby M, Melin K et al (2019) Convergent and divergent validity of the schedule for affective disorders and schizophrenia for school-age children—present and lifetime version diagnoses in a sample of children and adolescents with obsessive–compulsive disorder. Nord J Psychiatry 73:111–117. https://doi.org/10.1080/08039488.2019.1571628
Guy W (1976) Clinical global impressions. In: Guy W (ed) ECDEU assessment manual for psychopharmacology. Rockville, MD, National Institute of Mental Health, pp 218–222
Achenbach TM (1994) Child behavior checklist and related instruments. In: Maruish MEE (ed) The use of psychological testing for treatment planning and outcome assessment. Lawrence Erlbaum Associates, Hillsdale, NJ, pp 517–549
Green B, Shirk S, Hanze D, Wanstrath J (1994) The children’s global assessment scale in clinical practice: an empirical evaluation. J Am Acad Child Adolesc Psychiatry 33:1158–1164. https://doi.org/10.1097/00004583-199410000-00011
Shaffer D, Gould MS, Brasic J et al (1983) A children’s global assessment scale (CGAS). Arch Gen Psychiatry 40:1228. https://doi.org/10.1001/archpsyc.1983.01790100074010
Birmaher B, Khetarpal S, Brent D et al (1997) The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 36:545–553. https://doi.org/10.1097/00004583-199704000-00018
Angold A, Weissman MM, John K et al (1987) Parent and child reports of depressive symptoms in children at low and high risk of depression. J Child Psychol Psychiatry 28:901–915
Messer S, Angold A, Costello E, Loeber R (1995) Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: factor composition and structure across development. Int J Methods Psychiatr Res 5:251–262
Calvocoressi L, Mazure CM, Kasl SV et al (1999) Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Ment Dis 187:636–642. https://doi.org/10.1097/00005053-199910000-00008
Hollingshead AB (1957) Two factor index of social position. Yale University Press, New Haven, CT
Rubin DB (1987) Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons Inc, Hoboken, NJ, USA
Farris SG, McLean CP, Van Meter PE et al (2013) Treatment response, symptom remission, and wellness in obsessive-compulsive disorder. J Clin Psychiatry 74:685–690. https://doi.org/10.4088/jcp.12m07789
Rajmil L, Palacio-Vieira JA, Herdman M et al (2009) Effect on health-related quality of life of changes in mental health in children and adolescents. Health Qual Life Outcomes 7:103. https://doi.org/10.1186/1477-7525-7-103
Jacoby RJ, Leonard RC, Riemann BC, Abramowitz JS (2014) Predictors of quality of life and functional impairment in obsessive–compulsive disorder. Compr Psychiatry 55:1195–1202. https://doi.org/10.1016/j.comppsych.2014.03.011
Asnaani A, Kaczkurkin AN, Alpert E et al (2017) The effect of treatment on quality of life and functioning in OCD. Compr Psychiatry 73:7–14. https://doi.org/10.1016/j.comppsych.2016.10.004
Norberg MM, Calamari JE, Cohen RJ, Riemann BC (2008) Quality of life in obsessive-compulsive disorder: an evaluation of impairment and a preliminary analysis of the ameliorating effects of treatment. Depress Anxiety 25:248–259. https://doi.org/10.1002/da.20298
Albert U, Maina G, Bogetto F et al (2010) Clinical predictors of health-related quality of life in obsessive-compulsive disorder. Compr Psychiatry 51:193–200. https://doi.org/10.1016/j.comppsych.2009.03.004
Schei J, Nøvik TS, Thomsen PH et al (2015) Improved quality of life among adolescents with attention-deficit/hyperactivity disorder is mediated by protective factors: a cross sectional survey. BMC Psychiatry 15:108. https://doi.org/10.1186/s12888-015-0491-0
Fontenelle IS, Fontenelle LF, Borges MC et al (2010) Quality of life and symptom dimensions of patients with obsessive–compulsive disorder. Psychiatry Res 179:198–203. https://doi.org/10.1016/j.psychres.2009.04.005
Acknowledgements
Thomas Jozefiak has kindly contributed to the project with norm data from his study on students from the general population.
Funding
TrygFonden and Aarhus University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Tord Ivarsson has served on the speaker’s bureau of Shire Sweden. The remaining authors declare that they have no conflicts of interest.
Ethical approval
The study has been approved by the National Ethical Committees and data authorities in Denmark, Norway, and Sweden, and patients and parents provided written consent.
Supplementary Information
Below is the link to the electronic supplementary material. I have provided the Supplementary Files in pdf format - please refer to the attached files
Rights and permissions
About this article
Cite this article
Jensen, S., Hybel, K.A., Højgaard, D.R.M.A. et al. Quality of life in pediatric patients with obsessive–compulsive disorder during and 3 years after stepped-care treatment. Eur Child Adolesc Psychiatry 31, 1377–1389 (2022). https://doi.org/10.1007/s00787-021-01775-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01775-w