Abstract
Purpose
Cervical disc arthroplasty (CDA) was developed to treat cervical degenerated disc diseases with the advantages of preserving the kinematics of the functional spinal unit. However, the safety and reliability of multi-level CDA are still controverted when comparing to the single-level CDA. It has shown unclear benefits in terms of clinical results, functional recovery, heterotopic ossification, and the need for secondary surgical procedures. The purpose of this study is to estimate the effectiveness of multi-level cervical arthroplasty over single-level CDA for the treatment of cervical spondylosis and disc diseases.
Methods
To compare the studies of multi-level CDA versus single-level CDA in patients with cervical spondylosis that reported at least one of the following outcomes: functionality, neck pain, arm pain, quality of life, reoperation and incidence of heterotopic ossification, electronic databases (Medline, Embase, Pubmed, Cochrane library, and Cochrane Central Register of Controlled Trials) were searched. No language restrictions were used. Two authors independently assessed the methodological quality of included studies and extracted the relevant data.
Results
Out of Eight cohorts that were included in the study, four were prospective cohorts and the other four were retrospective. The results of the meta-analysis indicated that there was no significant difference in neck disability index scores, neck visual analog scale (VAS), arm VAS, morbidity of reoperation, heterotopic ossification, and parameters of living quality when comparing multi-level CDA with single-level CDA at 1 and 2 years follow-up postoperatively (p > 0.05).
Conclusions
The meta-analysis revealed that the outcomes and functional recovery of patients performed with multi-level CDA are equivalent to those with single-level CDA, which suggests the multi-level CDA is as effective and safe as single-level invention for the treatment of cervical spondylosis. Nonetheless, more well-designed studies with large groups of patients are needed to provide further evidence for the benefit and reliability of multi-level CDA in the treatment of cervical disc diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical spondylosis and disc diseases are the most common cause of radiculopathy and myelopathy resulting in significant disability [1]. For decades, anterior cervical discectomy with fusion (ACDF) has been regarded as the “gold standard” of surgical intervention in treating cervical disc diseases, achieving neural decompression, segmental stabilization, and excellent clinical outcomes [2–4]. However, in recent years, cervical disc arthroplasty (CDA) has become an emerging option, which is designed to preserve segmental motion and theoretically prevent adjacent segment disease (ASD) [5, 6]. CDA has been increasingly regarded as an acceptable surgical intervention to treat cervical disc diseases.
To date, the legitimacy of CDA has been demonstrated by an accumulation of short- and intermediate-term follow-up studies [7] and a few long-term studies [8, 9]. Following anterior cervical decompression and artificial disc replacement, the motion patterns and disc height are preserved and the subsequent degeneration at adjacent levels can retard or reduce, resulting in excellent outcomes and clinical recovery [10–13]. However, cervical arthroplasty may also be companied with complications, such as increased flexibility of the adjacent disc, erosion of the prosthesis and heterotopic ossification. Most studies have compared single-level disc replacement with ACDF. Although the multi-level disc replacement has also been advocated and performed by some authors for the treatment of multi-level cervical disc diseases instead of extensive fusion techniques, the clinical effect and safety of multi-level CDA are still disputed [14, 15].
Previous meta-analysis reviews focus on the comparison between single-level CDA and fusion, however, the outcomes and benefit of multi-level CDA compared with single-level CDA are less clear. The purpose of this study was to compare outcomes after multi-level CDA with those after single-level CDA to evaluate whether favorable single-level CDA outcomes and reliability extend to multilevel surgery.
Materials and methods
Search strategy
To search all of the relevant literature, we conducted a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)-compliant search of Medline, Embase, Pubmed, Cochrane library, and Cochrane Central Register of Controlled Trials (CENTRAL) by using combinations of the following keywords: “cervical arthroplasty”, “cervical artificial disc replacement”, cervical prosthesis, cervical total replacement “single-level”, “multi-level or two-levels or three-levels”. We searched for randomized controlled trails (RCTs), prospective cohort and retrospective cohort published between January 1990 and November 2014 that compared single-level cervical arthroplasty with multi-level cervical arthroplasty. We placed no restrictions on the language of the publication. References cited in the relevant articles were also reviewed. All researches were carefully estimated to identify repeated data. Criteria used to define duplicate data included study centers, treatment information, and any additional inclusion criteria.
Inclusion and exclusion criteria
Researches that conformed to the following criteria were eligible for inclusion in this study: (1) original researches; (2) studies that include multi-level CDA compared with single-level CDA; (3) studies with follow-up more than 1 year. We excluded studies in the thoracic or lumbar spine, articles that were duplicate reports of an earlier trial, reviews, and case-reports.
Data extraction
Two of the authors extracted the data from eligible studies independently, discussed discrepancies, and reached conformity for all items. The indispensable information extracted from all primary researches included the titles, author names, year of publication, original country, study design, sample size, type of arthroplasty prosthesis, duration of follow-up, and outcome parameters. The corresponding author of each study was contacted to obtain any missing information if it was required. The extracted data were rechecked for accuracy or against the inclusion criteria by the corresponding author.
Outcomes
The following outcomes were extracted from the included publications.
-
1.
Disability was assessed postoperatively using the neck disability index (NDI).
-
2.
Pain was assessed using the arm and neck visual analog scale (VAS).
-
3.
Complications included the following severe events related to surgical procedures or implants: numbness or paresthesia, dural tear, cerebrospinal spinal fluid leakage, hematoma formation, dysphagia, dysphonia, and deep infections.
-
4.
Heterotopic ossification (HO) rate after cervical total disc replacement.
-
5.
Incidence of reoperation. Secondary procedures occurred in cases of continued neck and shoulder pain, prosthesis flexibility, or adjacent-level degeneration, and when implants or pros-theses needed to be removed for infection.
-
6.
Success rate. Outcomes in some studies were graded based on the Odom classification [16]. The SF-36 quality of life score was also used in some studies to assess the recovery of patients [17].
Quality assessment
The quality of the studies was independently assessed by the authors according to the Newcastle-Ottawa Scale (NOS). The manual was downloaded from Ottawa Hospital Research Institute online. The NOS uses a pentagram symbol “☆” rating system (a pentagram symbol stands for one score), to judge quality of cohorts based on three aspects of the cohort studies: selection, comparability and outcomes. Scores were ranged from 0 to 9. Studies with a score ≥7 were regarded to be of high-quality.
Statistical analysis
We performed all meta-analyses with the STATA 12.0 (StataCorp LP, College Station, TX, USA). For continuous outcomes, means and standard deviations were pooled to generate a mean difference (MD), and 95 % confidence intervals (CI) were generated. For dichotomous outcomes, the risk ratio (RR) or the odds ratio (OR) and 95 % CI were assessed. A probability of p < 0.05 was considered to be statistically significant. Assessment for statistical heterogeneity was calculated using the I-square tests, which described the proportion of the total variation in meta-analysis assessments from 0 to 100 % [18]. The random effects model was used for the analysis when an obvious heterogeneity was observed among the included studies (I 2 > 50 %). The fixed-effects model was used when there was no significant heterogeneity between the included studies (I 2 ≤ 50 %) [19]. The possibility of publishing bias was not evaluated because there were <10 studies assessed.
Results
Study characteristics
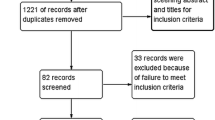
By searching in PubMed, Embase, Medline, Cochrane library, and Cochrane Central Register of Controlled Trials (CENTRAL), 156 studies were initially identified. Eighty-seven studies were excluded because they did not meet the inclusion criteria. A flow diagram of the selection process for relative articles is shown in Fig. 1. Finally, eight studies were included into our meta-analysis and the characteristics are presented in Table 1. Out of the eight studies, four are designed as prospective cohort and the other four are retrospective cohort. Totally, 506 patients were undergone single-level CDA and 240 patients were instrumented by 532 levels of CDA in multi-level group.
Quality assessment
Assessment of the study specific quality scores from NOS system is shown in Table 2. The median score of included studies was 7.375, with a range from 6 to 8. Seven of the eight studies were identified as relatively high-quality.
Outcomes analysis
Comparison between multi-level and single-level cervical arthroplasty was based on usual clinical outcomes, including NDI, VAS, reoperation rate, heterotopic ossification, and quality of life satisfaction (success rate and SF-36 quality of life score) [20]. The mean NDI, radicular VAS and cervical VAS were comparable pre-operatively between both groups (p > 0.05 for the three comparisons), and they decreased significantly at all post-operative time points compared to pre-operative values, by the same extent. At 24 months post-operation, there was no significant difference between both groups in the NDI score (single-level, 27.3 ± 1.8 versus multi-level 29.2 ± 2.9, p = 0.713), the radicular VAS score (single-level, 24.4 ± 2.1 versus multi-level 26.7 ± 3.9, p = 0.790), and the cervical VAS score (single-level, 23.5 ± 1.7 versus multi-level 23.9 ± 3.2, p = 0.593). The SF-36 quality of life score also showed a strong improvement in both groups compared to pre-operative baseline during the follow-up period, without remarkable difference between the two groups. And the success rate, taking into account both functional improvement and absence of revision surgery, was 69 and 66 % in the single- and the multi-level groups, respectively (p = 0.727). Regarding complications and re-operations, the number of patients meeting at least one complication/re-operation did not differ significantly between both groups (p = 0.109). Consistent with this, Kim et al. [21] reported that the double- and single-level Bryan arthroplasty showed similar NDI and VAS score at 1 year follow-up. Moreover, Wu et al. [22] reported that the clinical outcomes measured by VAS neck, VAS arm, and NDI, were all significantly improved after surgery compared with the pre-operative status in both groups. Notably, there was no significant difference between the single- and multilevel groups at each time point of evaluation (i.e., pre-operation, and 12 and 24 month post-operation).
However, in another study [14] of 140 patients that underwent cervical arthroplasty with PCM prostheses (229 segments), the mean improvement in the NDI for the single cases was 37.6 % versus the multilevel cases mean improvement in NDI of 52.6 % (p = 0.021). The difference between the two groups was statistically significant. The mean improvement in the VAS showed the same association: single-level mean improvement 58.4 % versus multilevel mean VAS improvement 65.9 %. Only the reoperation rates and serious adverse events were similar between single-level and multilevel arthroplasty. These findings demonstrate that clinic recovery of multi-level cervical arthroplasty is superior to single-level arthroplasty, which is not supported by the other three cohorts. This diversity may be due to the difference between the properties of PCM prostheses and Bryan and other prostheses (discussed in “Discussion”). Notably, after the relevant data were pooled from the eight included studies and investigated by meta-analysis, the overall difference of clinical outcomes between single- and multi-level CDA was not significant.
NDI
Four studies reported a postoperative NDI score of single-level and multi-level CDA. All of the four cohorts completed 1-year follow-up, three of them observed 2-year follow-up. The meta-analysis showed that the between-study heterogeneity existed (1 year follow-up, I 2 = 93.9 %; 2 year follow-up, I 2 = 88.9 %), so the random effects model was used to calculate the summary risk ratio with corresponding 95 % CI. In forest plots, the overall effect estimate was shown by a diamond for total or subtotal 95 % CI. When the diamond overlapped the vertical line of no effect, it indicated no statistically significant difference in NDI score between the two treatment groups. The SMD was 0.024 for the NDI (95 % CI −0.171 to 0.218; z = 0.24, p = 0.811) in 1 year follow-up. The SMD was 0.009 for the NDI (95 % CI −0.605 to 0.621; z = 0.03, p = 0.979) in 2-year follow-up (Fig. 2).
Forest plot of the meta-analysis of the NDI score comparing single-level with multi-level CDA. Diamonds stand for the overall effect estimate. When the diamonds overlap the vertical line of no effect (null line), it indicates that there is no statistically significant difference in NDI score between the two treatment groups in 1- and 2-year follow-up
Neck pain
Four studies reported neck VAS score postoperatively in 1-year follow-up and three studies reported 2 years follow-up. The random effects model was used in the analysis of 1 year follow-up because of the heterogeneity (I 2 = 73.5 %). In the meta-analysis of 2 years follow-up the fixed model was used because the heterogeneity was not significant (I 2 = 0.0 %). The results showed no significant difference in neck VAS score between single-level and multi-level CDA groups. The SMD was 0.179 for the neck VAS (95 % CI −0.213 to 0.571; z = 0.90, p = 0.370) in 1 year follow-up (Fig. 3a). The SMD was 0.039 for the neck VAS (95 % CI −0.159 to 0.237; z = 0.39, p = 0.700) in 2-year follow-up (Fig. 3b).
Forest plot of the meta-analysis of the neck VAS scores of single-level CDA versus multi-level CDA. a 1 year follow-up; b 2 years follow-up. The diamond of overall effect estimate overlaps the line of no effect, indicating there is no significant difference in neck VAS score between the two treatment groups
Arm pain
The arm VAS score in four cohorts were reported in 1-year follow-up and three studies reported 2 years follow-up. The random effects model was used because of the heterogeneity (1 year follow-up, I 2 = 73.9 %; 2 year follow-up, I 2 = 65.2 %). The results showed no significant difference in arm VAS score between single-level and multi-level CDA groups. The SMD was 0.199 for the neck VAS (95 % CI −0.197 to 0.594; z = 0.98, p = 0.325) in 1 year follow-up. The SMD was 0.039 for the neck VAS (95 % CI −0.363 to 0.324; z = 0.11, p = 0.910) in 2-year follow-up (Fig. 4).
Adverse events
Reoperation
Three studies reported the morbidity of reoperation. There was no significant difference in incidence of reoperation between the multi-level and single-level CDA (RR = 0.715, 95 % CI 0.271–1.890; z = 0.68, p = 0.499) with very low heterogeneity (I 2 = 0.0 %) (Fig. 5).
Heterotopic ossification
Five studies reported the incidence of heterotopic ossification (HO) postoperatively. Grading of HO was defined by the classification proposed by McAfee et al. [23]. The meta-analysis of the incidence of HO from McAfee Grade I to IV showed there was no significant difference between single-level and multi-level CDA groups (RR = 0.648, 95 % CI 0.295–1.427; I 2 = 80.3 %, z = 1.08, p = 0.282) (Fig. 6a). The meta-analysis of the severe complication, HO of Grade IV in three studies, was also been performed. The difference was not significant between the two groups (RR = 1.246, 95 % CI 0.608–2.554; z = 0.60, p = 0.547) with moderate heterogeneity (I 2 = 27.5 %) (Fig. 6b).
Forest plot of the meta-analysis of the incidence of heterotopic ossification (HO) postoperatively comparing single-level with multi-level CDA. a The morbidity of HO from Grade I to IV was pooled; b only the data of severe HO of Grade IV was pooled. No statistically significant difference between the two groups when the diamond touches the null line
Quality of life
Success rate
Clinical outcomes were assessed using the Odom outcome classification [16]. Clinical success was defined as patient report of “excellent” or “good” in the Odom rating system. Three cohorts reported the success rate of multi-level and single-level CDA. The difference was not significant between the two groups (RR = 1.470, 95 % CI 0.768–2.815; I 2 = 91.5 %, z = 1.16, p = 0.245) (Fig. 7).
SF-36 quality of life score
The SF-36 physical component score (PCS) and mental component score (MCS) were reported in two studies. Pooled analysis shows that the PCS of multi-level CDA had no significant difference compared with single-level CDA. As shown in Fig. 8a, at 1-year follow-up, SMD (95 % CI) = 0.075 (−0.201 to 0.350), I 2 = 0.0 %, z = 0.53, p = 0.595. At 2-year follow-up, SMD (95 % CI) = 0.070 (−0.641 to 0.501), I 2 = 59.9 %, z = 0.24, p = 0.810 (Fig. 8b). The difference of the MCS between the two groups was not significant. At 1-year follow-up, SMD (95 % CI) = 0.146 (−0.130 to 0.421), I 2 = 0.0 %, z = 1.03, p = 0.301; at 2-year follow-up, SMD (95 % CI) = 0.002 (−0.273 to 0.278), I 2 = 59.9 %, z = 0.02, p = 0.986 (Fig. 8c).
Forest plot of the meta-analysis of SF-36 quality of life score postoperatively between single-level with multi-level CDA. a Physical component score (PCS) at 1 year follow-up; b PCS at 2 years follow-up; c Mental component score (MCS) at 1 and 2 years follow-up. No statistically significant difference between the two groups when the diamond touches the null line
Discussion
Cervical disc arthroplasty is used increasingly to treat degenerative cervical diseases in recent years. A number of studies reported the comparison between single-level CDA and ACDF. Previous meta-analysis reported that the clinical outcomes of cervical arthroplasty are equivalent to or superior to the outcomes of ACDF for the treatment of single-level cervical diseases [24, 25]. Single-level CDA is commonly accepted for its satisfying outcomes as ACDF. However, the outcomes and reliability of multi-level CDA remain debated.
In our previous study, we designed a prospective random control trial to compare the clinical outcomes between two-level ACDF and CDA [26]. The evaluation of the total 65 patients indicated that Bryan artificial cervical disc replacement seemed reliable and safe in the treatment of patients with two-level cervical disc disease. Also in a cadaveric study [27], Phillips showed that a two-level CDA allowed a near-normal mobility at index and adjacent levels. In another in vitro study [28], Laxer showed that adjacent discs experience substantially lower pressure after two-level disc replacement when compared to two-level anterior fusion (ACDF). Nonetheless, to date, the amount of studies comparing the outcomes of multi-level CDA with ACDF is far lacked to be pooled by meta-analysis. To investigate whether the outcomes and reliability of multi-level CDA are superior or inferior to single-level CDA, we focused on the studies comparing the two methods of surgery when we searched the literature. Only eight cohorts met the including criteria of our meta-analysis, four were prospective cohorts and the others retrospective. No RCT comparing multi-level CDA with single-level CDA was obtained. The methodological quality assessed by NOS system showed that seven of the cohorts were identified as relatively high-quality and one was moderate. Clinical heterogeneity was induced by the biomechanical properties, different intention of surgery, different cervical prostheses, and the biophysical environment in the included studies. As a result, these methodological quality deficits should be considered when interpreting the findings of this meta-analysis. Besides, the possibility of publication bias was not assessed because of the small number of included studies.
In our meta-analysis, the multi-level arthroplasty group was equally beneficial to the NDI in the single-level CDA group. The heterogeneity was generated from the study of PCM prostheses reported by Pimenta [14], which showed the overall mean improvement in the NDI for the single cases was 37.6 % versus the multilevel cases (52.6 %) with statistically significant difference (p = 0.021). Whereas Huppert [20] reported that there was no significant difference between both groups regarding the NDI score at 1 and 2 years postoperatively. And the retrospective cohort of Wu [22] measured the clinical outcomes by VAS neck, VAS arm, and NDI. Also, there were no significant differences of these parameters between the single- and multi-level groups at 1 or 2 years follow-up. Finally, we pooled the studies reporting the NDI of the two groups by using random effect model in the meta-analysis because of the high heterogeneity. The data of neck VAS, arm VAS and quality of life were also analyzed and our results showed that multi-level CDA was as effective as single-level CDA to improve the outcomes and functional recovery of patients. The diversity of outcomes between different studies may be contributed to various prostheses. The cervical prostheses are mainly divided into three types, minimally-constrained/unconstrained (Bryan, Mobi-C), semi-constrained (PCM, Prestig-LP), and constrained (Prodisc-C). Sung Bae Park [29] reported that four types of prostheses (Bryan, Mobi-C, PCM, and Prestige-LP) provided the preservation of sagittal range of motion (ROM) and increased superior adjacent segment kinematics, regardless of prosthesis design. Patients who received the unconstrained prostheses Bryan and Mobi-C showed increased ROM at the index level and a high incidence of adjacent segment degeneration (ASD) compared with patients who received the semi-constrained prostheses (PCM and Prestig-LP). Most of the CDA studied in this meta-analysis were Bryan prosthesis. A long-term follow-up of Bryan CDA [8] reported that at 4 and 6 years postoperatively, the clinical outcomes appear consistent with the previous results at 1 and 2 years postoperatively. The mean angular motion results at 4 and 6 years postoperatively for single-level patients were 7.3° and 7.7°, respectively. Two-level patients had slightly less motion at 4 and 6 years postoperatively with mean caudad values of 5.7° (4 years) and 6.0° (6 years), and cephalad values of 4.2° (4 years) and 6.2° (6 years), respectively, suggesting a reliable preserve of cervical ROM was provided by two-level CDA in long-term follow-up. Because the ROM improvement was reported by inconsistent criteria detecting the total cervical spine or different implanted level, respectively, we did not investigate the pooled ROM results by meta-analysis.
Data on adverse events were not consistent in the studies included. We reviewed postoperative complications, reoperation rate and heterotopic ossification in multi-level and single-level CDA. The reoperation rate was reported in three studies and the analysis showed that multi-level group had a similar rate of reoperation to the single-level CDA. Meanwhile, the incidence rates of HO after cervical arthroplasty showed a huge discrepancy in previous literatures. The formation of HO has been reported from none to more than two-thirds in a variety of cervical artificial discs. For Bryan disc, the reported rate of HO has varied from 48.1 % in 52 levels, to 29 % in 59 levels, to 17.8 % in 90 levels [30–32]. However, more than 60 % of high rates of HO have been reported for other kinds of artificial discs [33–35]. The discrepancy of the reported incidence rates might be attributed to types of artificial discs and the difference of HO determination and the level of scrutiny. Grading of HO was defined by the classification proposed by McAfee et al. [23]. Class 0 means no HO present and Class IV represents severe HO causing inadvertent arthrodesis, bony ankylosis, bridging trabecular bone continuous between adjacent endplates and <3° of motion of lateral flexion–extension radiographs. Five studies reported the incidence of HO (Grade I to Grade IV) and three of them reported the data of HO of Grade IV. The data of severe (Grade IV) HO and the total incidence of HO were pooled respectively. The meta-analysis showed no significant difference of HO (severe or total) incidence between multi-level and single-level CDA.
There are several strengths and limitations of this study. The strengths include a rigorous search strategy, no language limitations, article screening, and methodological assessments performed in duplicate, abstracted data verified by a second reviewer and utilization of the NOS system to judge the quality of the evidence. In addition, this is the first meta-analysis on this topic to compare the difference between multi-level and single-level CDA. However, some limitations of this study should be acknowledged. First, there was no RCT comparing the outcomes between multi-level and single-level CDA. The studies included were composed of four prospective and four retrospective cohorts, the statistic quality of which was inferior to RCTs. Second, the statistical power could be improved in the future by including more studies. Due to the small number of included studies, some parameters could not be analyzed by subgroups to avoid a high heterogeneity which may exert instability on the consistency of the outcomes. Moreover, clinical heterogeneity might be caused by the different indications for surgery, the characteristics of the different prostheses and the surgical technologies used at different treatment centers.
In summary, this meta-analysis indicates that the parameters of outcomes and functional recovery of patients performed with multi-level CDA are equivalent to those with single-level CDA. Besides, more well-designed studies with large groups of patients are needed to provide further evidence of the effect and reliability of multi-level CDA in the treatment of cervical disc diseases.
References
Carette S, Fehlings MG (2005) Clinical practice. Cervical radiculopathy. N Engl J Med 353(4):392–399
Bohlman HH et al (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Jt Surg Am 75(9):1298–1307
Bose B (1998) Anterior cervical fusion using Caspar plating: analysis of results and review of the literature. Surg Neurol 49(1):25–31
Kaiser MG et al (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50(2):229–236 discussion 236–8
Pickett G, Rouleau JP, Duggal N (2005) Kinematic analysis of the cervical spine following implantation of an artificial cervical disc. Spine (Phila Pa 1976) 30(17):1949–1954
Sasso RC, Best NM (2008) Cervical kinematics after fusion and Bryan disc arthroplasty. J Spinal Disord Tech 21(1):19–22
Clements DH, O’Leary PF (1990) Anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 15(10):1023–1025
Goffin J et al (2010) A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine 12(3):261–269
Robertson JT, Metcalf NH (2004) Long-term outcome after implantation of the Prestige I disc in an end-stage indication: 4-year results from a pilot study. Neurosurg Focus 17(3):E10
Cummins BH, Robertson JT, Gill SS (1998) Surgical experience with an implanted artificial cervical joint. J Neurosurg 88(6):943–948
Goffin J et al (2003) Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level. Spine (Phila Pa 1976) 28(24):2673–2678
Mummaneni PV, Haid RW (2004) The future in the care of the cervical spine: interbody fusion and arthroplasty. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 1(2):155–159
Wigfield CC et al (2002) The new Frenchay artificial cervical joint: results from a 2-year pilot study. Spine (Phila Pa 1976) 27(22):2446–2452
Pimenta L et al (2007) Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine (Phila Pa 1976) 32(12):1337–1344
Wang Y et al (2006) Clinical report of cervical arthroplasty in management of spondylotic myelopathy in Chinese. J Orthop Surg Res 1:13
Odom GL, Finney W, Woodhall B (1958) Cervical disk lesions. J Am Med Assoc 166(1):23–28
McHorney CA et al (1994) The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 32(1):40–66
Higgins JP et al (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22(4):719–748
Huppert J et al (2011) Comparison between single- and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J 20(9):1417–1426
Kim SW et al (2009) Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J 18(2):218–231
Wu JC et al (2012) Multilevel arthroplasty for cervical spondylosis: more heterotopic ossification at 3 years of follow-up. Spine (Phila Pa 1976) 37(20):E1251–E1259
McAfee PC et al (2003) Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech 16(4):384–389
Xing D et al (2013) A meta-analysis of cervical arthroplasty compared to anterior cervical discectomy and fusion for single-level cervical disc disease. J Clin Neurosci 20(7):970–978
Fallah A et al (2012) Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLoS One 7(8):e43407
Cheng L et al (2009) Fusion versus Bryan Cervical Disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop 33(5):1347–1351
Phillips FM et al (2009) Effect of two-level total disc replacement on cervical spine kinematics. Spine (Phila Pa 1976) 34(22):E794–E799
Laxer E et al (2006) Adjacent segment disc pressures following two-level cervical disc replacement versus simulated anterior cervical fusion. Stud Health Technol Inform 123:488–492
Park SB et al (2013) X-ray based kinematic analysis of cervical spine according to prosthesis designs: analysis of the Mobi C, Bryan, PCM, and Prestige LP. J Spinal Disord Tech [Epub ahead of print]
Tu TH et al (2011) Heterotopic ossification after cervical total disc replacement: determination by CT and effects on clinical outcomes. J Neurosurg Spine 14(4):457–465
Leung C et al (2005) Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery 57(4):759–763 discussion 759–63
Heidecke V et al (2008) Intervertebral disc replacement for cervical degenerative disease—clinical results and functional outcome at 2 years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochir (Wien) 150(5):453–459 discussion 459
Mehren C et al (2006) Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 31(24):2802–2806
Suchomel P et al (2010) Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4-year follow-up. Eur Spine J 19(2):307–315
Beaurain J et al (2009) Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J 18(6):841–850
Coric D et al (2010) Prospective study of cervical arthroplasty in 98 patients involved in 1 of 3 separate investigational device exemption studies from a single investigational site with a minimum 2-year follow-up. J Neurosurg Spine 13(6):715–721
Kim HK et al (2009) Surgical outcome of cervical arthroplasty using bryan(r). J Korean Neurosurg Soc 46(6):532–537
Acknowledgments
This work was supported by the grant from Ph.D. Programs Foundation of Ministry of Education of China (20110131120079) and Shandong Provincial Natural Science Foundation, China (No. ZR2013HM095).
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Zhao and L. Cheng contributed equally to this study.
Rights and permissions
About this article
Cite this article
Zhao, H., Cheng, L., Hou, Y. et al. Multi-level cervical disc arthroplasty (CDA) versus single-level CDA for the treatment of cervical disc diseases: a meta-analysis. Eur Spine J 24, 101–112 (2015). https://doi.org/10.1007/s00586-014-3429-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3429-1