Abstract
Purpose
Only 50–65% of patients return to their previous sporting level after ACL rupture. The literature reports a reduced rate of graft rupture when an anterolateral ligament reconstruction (ALLR) is associated with ACL reconstruction.
ACL reconstruction combined with ALL allows a higher return to sport at pre-injury level than isolated reconstruction in patients playing pivot-contact sports.
Methods
A retrospective, single-centre study between 2012 and 2020 comparing reconstruction by hamstring tendon technique, isolated ACLR vs ACL with ALLR. An isokinetic test was performed at 6 months post-operatively and patients were re-contacted at a minimum 2-year follow-up to assess their level and delay to return to sport, graft rupture rate and functional evaluation.
Results
83 patients were included, 42 in ACLR group and 41 in ACL + ALLR group. Four patients were lost to follow-up and 79 patients were analysed. No significant difference was found on the level of return to sport (28.2% vs. 42.5%; p = 0.18), return to competition (43% vs. 60%; p = 0.18), delay to sports return, isokinetic assessment, functional scores, but a significant difference was found on graft rupture rate in favour of ALLR (12.8% vs. 0%; p = 0.02).
Conclusion
In our study, the addition of an ALL to ACL reconstruction did not improve pre-injury sports recovery or return to competition.
Study design
Cohort study, level of evidence 4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the anterior cruciate ligament (ACL) is a frequent injury, accounting for more than 50% of injuries following intra-articular knee trauma in pivot sport patients [18].
Despite good clinical and functional results after ACL reconstruction (ACLR), it has been reported that only 50–65% of patients return to their pre-rupture sporting level, and only one in two return to competitive sport [1, 5].
Several studies have compared reconstruction techniques using bone-patellar tendon versus hamstring tendon, without demonstrating the superiority of any one technique [5, 8], particularly with regard to return to sport at the same level.
The work of Claes [3] in 2013, followed by numerous anatomical and biomechanical studies, found that the anterolateral ligament (ALL) is a secondary stabilizer of the knee joint, limiting internal rotation between 30° and 90° of flexion and preventing anterolateral subluxation of the tibia on the femur [3, 15, 24]. Thus, ACLR associated with an ALL reconstruction (ALLR) provides better pivot control and a lower rate of graft rupture, thanks to the protective role of the ALL and a reduction in the load exerted on the ACL, with functional results similar to an isolated reconstruction [7, 14, 19, 21]. However, in these studies, the level and time to return to sport were secondary criteria or were not systematically evaluated.
We hypothesized that ACLR combined with ALLR would result in a higher rate of return to pre-injury sport than isolated reconstruction in pivot-contact patients.
The secondary objectives of our study were to evaluate the delay to return to sport, muscle recovery using isokinetic testing at 6 months, functional results, and the graft rupture rate at a minimum 2-year follow-up.
Methods
Subjects
A retrospective, single-centre, single-operator study in patients with ACL rupture playing pivot-contact sports such as team sports and martial arts, in competition or not, was conducted. The inclusion period was from 2012 to 2020 and included patients with symptomatic ACL rupture, confirmed by MRI, undergoing ACLR using the hamstring tendons technique with or without ALLR.
Exclusion criteria were iterative rupture or post-operative follow-up of less than 2 years.
Patients managed from 2012 to 2017 underwent isolated ACLR, then those managed from 2017 onwards underwent ACL with ALLR. The date of 2017 corresponds to the period when we systematically began the ALL technique for pivot-contact athletes. Two groups were thus formed: ACLR group and ACL + ALLR, regardless of associated lesions (meniscus or cartilage).
Surgical technique
The first part of ACL with ALLR consists of a conventional hamstring tendon reconstruction technique. However, the semitendinosus tendon is left pedicled, while the gracilis muscle tendon is used as a reinforcement on the semitendinosus to obtain 3 or 4 strands intra-articularly and 1 strand extra-articularly, the semitendinosus also being used to perform the ALLR (Fig. 1).
The lateral extra-articular tenodesis involves anatomical reconstruction of the anterolateral ligament, with a proximal femoral tunnel opposite the lateral femoral condyle. The transplant is then routed deep into the bony contact and under the iliotibial band to its posterior insertion at Gerdy’s tubercle (Fig. 2). The transplant is secured by an interference screw in a 2nd tibial tunnel, with the knee at 30° flexion and in neutral rotation (Fig. 3).
Post-operative check radiographs of the knee in front and in profile were taken to assess correct positioning of the tunnels. Weight-bearing was allowed from the day after surgery, with an extension splint until quadriceps locking was achieved. Rehabilitation began with recovery of passive joint mobility and quadriceps locking, followed by active mobility from 6 weeks and muscle strengthening.
Clinical evaluations
Preoperatively, each patient’s epidemiological parameters, injuries associated with ACL rupture, complementary reconstruction procedures, level of sport (recreational or competitive) and sport practised were collected. The Tegner activity scale was also used to determine the level of activity prior to injury and at assessment[22].
All patients received a consultation with radiographic follow-up at 6 weeks, 3 months, 6 months and 1 year. As part of the follow-up, a self-administered questionnaire was sent to them, with a minimum follow-up of 2 years after surgery, to collect the level of return to sport, return to competitive sport, delay of return to sport in training and competition, sprain recurrence, transplant rupture or new surgery, long-term complications, as well as the ACL-rsi (Anterior Cruciate Ligament-Return to Sport after) score [2] and functional scores: IKDC (International Knee Documentation Committee) [11] and Lysholm [17].
Muscular recovery was assessed by a rehabilitation physician, who performed an isokinetic test at 6 months post-operatively, calculating deficits for each muscle group, followed by flexor/extensor ratios (concentric at 60°/s) and finally the mixed or functional ratio. A functional ratio between 1 and 1.2 was considered protective and was sought, as was a flexor/extensor ratio between 0.5 and 0.6. All tests were performed on the Biodex dynamometer.
Following the results, the rehabilitation physician subjectively assessed the test in 4 stages: very satisfactory, satisfactory, moderately satisfactory or unsatisfactory.
The main purpose of these tests was to identify muscular imbalance, in order to guide rehabilitation and authorize or not the resumption of a pivot sport. In the event of an unsatisfactory result, patients were invited to undergo a test at 8 months post-operatively.
Statistical methods
The various variables studied were compared between the isolated ACLR and ACL + ALLR groups using Fisher’s exact test for qualitative variables and the Mann–Whitney test for numerical variables. A multivariate analysis was then performed, taking into account the various confounding factors identified in the univariate analysis.
Tests were considered significant when p was less than 0.05.
Data were collected via the Easymedstat website, and analyses were performed using R software version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria, 2021).
Results
Population
Eighty-three patients were included (67 men and 16 women, mean age 24 ± 7.2 years), 4 patients were lost to follow-up and 79 completed the questionnaire and were analysed at final follow-up (39 ACLR group and 40 ACL + ALLR group). Forty-seven patients underwent isokinetic evaluation at 6 months post-operatively and were analysed (21 ACLR group and 26 ACL + ALLR group).
The average time between trauma and surgery was 11 months in both groups, the average follow-up was 54 months. There was a significant difference in the time between surgery and assessment (75.4 ± 25.5 in ACLR vs 33.4 ± 11.3 in ACL + ALLR; p < 0,01), and in the management of meniscal lesions (14,6% meniscus suture in ACLR vs 41,5% in ACL + ALLR; p < 0,005). The two groups were comparable in all other respects (gender, BMI, Tegner score, sport type and level…), in particular, in term of associated lesions (meniscus, ligament and cartilage lesions) detected on imaging and also intraoperatively.
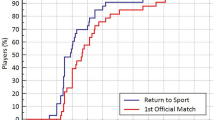
Return to play and return to competitive sport
The return to sport at the same level (28.2% vs. 42.5%), the return to competitive sport (43% vs. 60%) and the postoperative Tegner score were higher in the ACL + ALLR group, although the results were not significant (Table 1).
The multivariate analysis looked at the evaluation of the return to sport according to the following confounding factors, identified in the univariate analysis: ALLR, age, gender, time to return to sport and functional scores.
These analyses showed that the performance of a ALLR was not correlated with the level of return to sport, that there was a correlation between a return to the same level and a shorter time to return to sport with higher functional scores, and that a higher age at the time of the operation was a risk factor for not returning to competitive level (Table 2).
Delay to return to sport
No significant difference was found either in the time taken to return to training or competition, or in the time taken to return to work (Table 1).
Isokinetic evaluation
No significant differences were observed for: the deficits of each muscle group in the different modes of contraction, the flexor/extensor ratios (0.6 ± 0.1 vs. 0.6 ± 0.2; p = 0.5), the functional ratios (1.1 ± 0.5 vs. 1.1 ± 0.3; p = 0.4) and the observer’s subjective analysis.
Authorisation to resume pivot-contact sport at 6 months was 54.2% in the ACL + ALLR group compared with 25% in the ACLR group (p = 0.1).
Functional evaluation
The Lysholm, IKDC and ACLrsi scores were comparable between the 2 groups (Table 3). However, a significant difference in the rate of graft rupture in favour of ALLR was observed (0% (0) vs. 12.8% (5); p = 0.02).
In the multivariate analysis, only the association of ALLR or a lower preoperative Tegner score was correlated with a lower rate of graft rupture (Table 2).
Finally, no major complications or septic complications were found in either group.
Discussion
Combining ALL with ACL reconstruction in pivot-contact patients does not improve the level of return to pre-injury sport or the return to a competitive level, compared with isolated reconstruction.
However, the ALLR technique has been shown to be effective in reducing the rate of graft rupture compared with isolated reconstruction [9, 12, 21]. Some of these studies have also evaluated the time or level of return to sport but, to our knowledge, our study is the first comparative series to have taken this data as the main criterion.
Return to sport
Return to sport has been evaluated in several studies as a secondary endpoint and from these studies, a recent meta-analysis, published by Hurley et al. in 2021, compared return to sport after ACLR with or without extra-articular augmentation (EA) [13]. This meta-analysis concluded that patients managed for first-line ACLR, with or without EA, reported similar levels of return to sport.
Although not reaching the significance threshold, return to sport at pre-trauma level appeared higher in the ALLR group (28.2% vs. 42.5%; p = 0.18), as did return to competitive level (60% vs. 43%; p = 0.21).
Patients who returned to sport at the pre-trauma level were the quickest to return, with an average difference of 3 months, and had better functional scores. These results were corroborated by the multivariate analysis, which also showed that younger patients were more likely to return to competitive sport. This suggests a profile of patients who are young and highly motivated to return to competition, which very probably influences the level and time taken to return to sport, as well as functional recovery.
Ten comparative studies evaluating isolated ACLR versus ACLR with EA as first-line treatment were found in the literature, 8 of which evaluated the level of return to sport at the same level as a secondary endpoint [6, 9, 10, 20, 21, 23, 25, 26]. Of these studies, only 2 showed a difference in favour of ALLR, with Sonnery-Cottet et al. [21] finding a better pre-injury sport recovery in the combined hamstring + ALL reconstruction group compared with the isolated hamstring reconstruction group, with an odds ratio of 1.9, which contrasts with the results of our study. However, no difference was found between isolated patellar tendon reconstruction and combined reconstruction (hamstring graft + ALL).
Delay to return to sport
There was no difference between the two groups in terms of time to return to training or competition. However, the authorisation to return to sport by the rehabilitation physician at 6 months was higher in the ACL + ALLR group (54% vs. 25%; p = 0.07), although in the end this had to be confirmed by the surgeon based on clinical results and isokinetic tests, giving us a standardised return to sport for most patients in both groups.
The data in the literature, in particular the study by Hurley et al. [13], seems to be more in favour of EA. In fact, according to this meta-analysis, 3 studies evaluated the delay to return to sport, 2 of which showed a faster return after ALLR with a difference of 1 month.
Graft rupture and functional results
With regard to the reconstruction failure rate, our results are in line with those found in recent years, with a clear reduction in the graft rupture rate at 2 years, with 12.8% of ruptures in the ACLR group compared with 0% in the ACL + ALLR group (p = 0.02). The reduction in the failure rate after ALLR has already been demonstrated, notably in the Stability study by Getgood et al. [9] in 2020, and then confirmed by various meta-analyses [7, 16].
However, we did not observe any difference in the re-intervention rate, as the majority of patients in the ACLR group were re-intervened for a graft rupture, whereas patients in the ALLR group were re-intervened for meniscal surgery, which is linked to changes in practice that now clearly favour suturing.
There was no difference in the various functional scores, nor in the ACLrsi score, which assesses the psychological impact of returning to sport. Here again, our results are in line with various published series, with comparable functional results between isolated and combined plasty [9, 20].
The comparable results found in the isokinetic tests at 6 months lead us to conclude that the combined reconstruction does not cause greater muscle imbalance than an isolated reconstruction. This result was expected, because although differences have been observed between bone-patellar tendon autograft and hamstring tendon autograft, with a greater flexion deficit in the latter [4], all patients in our study benefited from the same hamstring transplant.
Limits
Our study has several limitations. ALLR combined with ACLR began in 2017, so the two groups underwent surgery at two different times. Thus, due to the retrospective nature of this study, the time between surgery and assessment was significantly longer in the ACLR group (75.4 months vs 33.4 months; p < 0.01). This delay may lead to memory bias and imprecision in their response. However, some patients stated that they had not resumed sporting activity because of lifestyle changes or lack of time, rather than because of a functional deficit caused by ACL rupture and reconstruction. For these patients, the trauma and the surgery mark a turning point in their sporting activities, and their decision not to return to activity will be based on personal rather than functional choices, regardless of the type of reconstruction we are able to offer them.
In addition, the experience of the surgeon was greater in the ACL + ALLR group, which could lead to better results in this group, although no significant difference was found between the two groups. The two groups were also not totally homogeneous in terms of sport level (athlete or not) because the design of our study made it difficult to further select patients with limited sample sizes. Finally, the relatively small size of our samples and the retrospective nature of our analysis limit the significance of our results.
Conclusion
ACL reconstruction combined with ALL reconstruction does not provide a better return to pre-injury sport than isolated reconstruction. However, it does reduce the graft rupture rate, while producing clinical and functional results comparable to isolated reconstruction, with no specific complications.
As a result, it seems entirely appropriate to systematically offer ALLR to pivot-contact athletes at risk of re-rupture.
Data availability
Patient consent was obtained for data analysis and publication.
References
Ardern CL, Taylor NF, Feller JA, Webster KE (2014) Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 48:1543–1552. https://doi.org/10.1136/bjsports-2013-093398
Bohu Y, Klouche S, Lefevre N, Webster K, Herman S (2015) Translation, cross-cultural adaptation and validation of the French version of the anterior cruciate ligament-return to sport after injury (ACL-RSI) scale. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 23:1192–1196. https://doi.org/10.1007/s00167-014-2942-4
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328. https://doi.org/10.1111/joa.12087
Dauty M, Tortellier L, Rochcongar P (2005) Isokinetic and anterior cruciate ligament reconstruction with hamstrings or patella tendon graft: analysis of literature. Int J Sports Med 26:599–606. https://doi.org/10.1055/s-2004-821342
DeFazio MW, Curry EJ, Gustin MJ, Sing DC, Abdul-Rassoul H, Ma R, Fu F, Li X (2020) Return to sport after ACL reconstruction with a BTB versus hamstring tendon autograft: a systematic review and meta-analysis. Orthop J Sports Med 8:2325967120964919. https://doi.org/10.1177/2325967120964919
Dejour D, Vanconcelos W, Bonin N, Saggin PRF (2013) Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop 37:193–199. https://doi.org/10.1007/s00264-012-1718-z
Delaloye J-R, Murar J, Gonzalez M, Amaral T, Kakatkar V, Sonnery-Cottet B (2018) Clinical outcomes after combined anterior cruciate ligament and anterolateral ligament reconstruction. Tech Orthop 33:225–231. https://doi.org/10.1097/BTO.0000000000000326
Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL (2016) Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med 44:1069–1079. https://doi.org/10.1177/0363546515584043
Getgood AMJ, Bryant DM, Litchfield R, Heard M, McCormack RG, Rezansoff A, Peterson D, Bardana D, MacDonald PB, Verdonk PCM, Spalding T, Willits K, Birmingham T, Hewison C, Wanlin S, Firth A, Pinto R, Martindale A, O’Neill L, Jennings M, Daniluk M, Boyer D, Zomar M, Moon K, Pritchett R, Payne K, Fan B, Mohan B, Buchko GM, Hiemstra LA, Kerslake S, Tynedal J, Stranges G, Mcrae S, Gullett L, Brown H, Legary A, Longo A, Christian M, Ferguson C, Mohtadi N, Barber R, Chan D, Campbell C, Garven A, Pulsifer K, Mayer M, Simunovic N, Duong A, Robinson D, Levy D, Skelly M, Shanmugaraj A, Howells F, Tough M, Spalding T, Thompson P, Metcalfe A, Asplin L, Dube A, Clarkson L, Brown J, Bolsover A, Bradshaw C, Belgrove L, Millan F, Turner S, Verdugo S, Lowe J, Dunne D, McGowan K, Suddens C-M, Declercq G, Vuylsteke K, Van Haver M (2020) Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the stability study randomized clinical trial. Am J Sports Med 48:285–297. https://doi.org/10.1177/0363546519896333
Goncharov EN, Koval OA, Dubrov VE, Bezuglov EN, Filimonova AM, Goncharov NG (2019) Clinical experience with combined reconstruction of the anterior cruciate and anterolateral ligaments of the knee in sportsmen. Int Orthop 43:2781–2788. https://doi.org/10.1007/s00264-019-04409-8
Hefti F, Müller W, Jakob RP, Stäubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 1:226–234. https://doi.org/10.1007/BF01560215
Helito CP, Camargo DB, Sobrado MF, Bonadio MB, Giglio PN, Pécora JR, Camanho GL, Demange MK (2018) Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 26:3652–3659. https://doi.org/10.1007/s00167-018-4934-2
Hurley ET, Manjunath AK, Strauss EJ, Jazrawi LM, Alaia MJ (2021) Return to play after anterior cruciate ligament reconstruction with extra-articular augmentation: a systematic review. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 37:381–387. https://doi.org/10.1016/j.arthro.2020.06.007
Ibrahim SA, Shohdy EM, Marwan Y, Ramadan SA, Almisfer AK, Mohammad MW, Abdulsattar WS, Khirat S (2017) Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament: a randomized clinical trial. Am J Sports Med 45:1558–1566. https://doi.org/10.1177/0363546517691517
Kennedy MI, Claes S, Fuso FAF, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF (2015) The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med 43:1606–1615. https://doi.org/10.1177/0363546515578253
Littlefield CP, Belk JW, Houck DA, Kraeutler MJ, LaPrade RF, Chahla J, McCarty EC (2020) The anterolateral ligament of the knee: an updated systematic review of anatomy, biomechanics, and clinical outcomes. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. https://doi.org/10.1016/j.arthro.2020.12.190
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154. https://doi.org/10.1177/036354658201000306
Majewski M, Susanne H, Klaus S (2006) Epidemiology of athletic knee injuries: a 10-year study. Knee 13:184–188. https://doi.org/10.1016/j.knee.2006.01.005
Rosenstiel N, Praz C, Ouanezar H, Saithna A, Fournier Y, Hager J-P, Thaunat M, Sonnery-Cottet B (2019) Combined anterior cruciate and anterolateral ligament reconstruction in the professional athlete: clinical outcomes from the scientific anterior cruciate ligament network international study group in a series of 70 patients with a minimum follow-up of 2 years. Arthrosc J Arthrosc Relat Surg 35:885–892. https://doi.org/10.1016/j.arthro.2018.09.020
Rowan FE, Huq SS, Haddad FS (2019) Lateral extra-articular tenodesis with ACL reconstruction demonstrates better patient-reported outcomes compared to ACL reconstruction alone at 2 years minimum follow-up. Arch Orthop Trauma Surg 139:1425–1433. https://doi.org/10.1007/s00402-019-03218-3
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M (2017) Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med 45:1547–1557. https://doi.org/10.1177/0363546516686057
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop 198:43–49
Trichine F, Chouteau J, Moyen B, Bouzitouna M, Maza R (2014) Patellar tendon autograft reconstruction of the anterior cruciate ligament with and without lateral plasty in advanced-stage chronic laxity. A clinical, prospective, randomized, single-blind study using passive dynamic X-rays. The Knee 21(1):58–65
Van der Watt L, Khan M, Rothrauff BB, Ayeni OR, Musahl V, Getgood A, Peterson D (2015) The structure and function of the anterolateral ligament of the knee: a systematic review. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 31:569-582.e3. https://doi.org/10.1016/j.arthro.2014.12.015
Zaffagnini S, Bruni D, Russo A, Takazawa Y, Presti ML, Giordano G, Marcacci M (2008) ST/G ACL reconstruction: double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports 18:573–581. https://doi.org/10.1111/j.1600-0838.2007.00697.x
Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP (2006) Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc 14:1060–1069. https://doi.org/10.1007/s00167-006-0130-x
Funding
Emmanuel Baulot contributed to Contracts for Company Serf, Aston and XNOV. Consulting fees for company Serf, Aston and XNOV. Pierre Martz contributed to Consulting fees for company Serf and XNOV. The other authors declare that they have no financial interest. No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonnachon, A., Labattut, L., Abdoul Carime, N. et al. Does combined anterior cruciate ligament and anterolateral ligament reconstruction improve return to sport?. Eur J Orthop Surg Traumatol 34, 981–987 (2024). https://doi.org/10.1007/s00590-023-03744-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03744-2